Role of adeno-associated virus vectors in Modern Gene Therapy
SEP 19, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
AAV Vectors in Gene Therapy: Background and Objectives
Adeno-associated virus (AAV) vectors have emerged as one of the most promising delivery systems in the field of gene therapy over the past three decades. Initially discovered as contaminants in adenovirus preparations in the 1960s, AAVs are small, non-enveloped viruses belonging to the Parvoviridae family. Their natural inability to cause disease in humans, coupled with their capacity to infect both dividing and non-dividing cells, has positioned them as ideal candidates for therapeutic gene delivery.
The evolution of AAV technology has been marked by significant milestones. Early research in the 1980s and 1990s focused on understanding the basic biology of these viruses, while the 2000s witnessed the development of recombinant AAV vectors with enhanced transduction efficiency. Recent advancements have centered on engineering novel AAV capsids with improved tissue tropism and reduced immunogenicity, expanding their therapeutic potential.
The primary objective of AAV vector technology in modern gene therapy is to provide safe, efficient, and long-term gene expression in target tissues. Unlike other viral vectors, AAVs predominantly remain episomal rather than integrating into the host genome, significantly reducing the risk of insertional mutagenesis. This safety profile has been instrumental in gaining regulatory approvals for AAV-based therapies.
Current technical goals in the field include developing AAV vectors with increased packaging capacity beyond the traditional limit of approximately 4.7 kb, enhancing tissue-specific targeting capabilities, and overcoming pre-existing immunity challenges. Researchers are also focused on improving manufacturing processes to increase vector yield and purity, which remains critical for clinical applications.
The trajectory of AAV vector development is increasingly moving toward personalized medicine approaches. This includes the creation of designer AAVs tailored to specific disease conditions and patient populations. Computational and high-throughput screening methods are being employed to predict and optimize AAV capsid properties, representing a shift from traditional empirical approaches to more rational design strategies.
Another emerging trend is the application of AAV vectors in genome editing technologies, particularly CRISPR-Cas systems. The combination of these technologies offers unprecedented opportunities for precise genetic modifications, potentially revolutionizing the treatment of monogenic disorders and complex diseases alike.
As gene therapy transitions from experimental treatments to approved medical interventions, AAV vectors stand at the forefront of this therapeutic revolution. Their continued refinement and optimization will likely shape the future landscape of genetic medicine, potentially offering solutions for previously untreatable conditions and improving patient outcomes across a spectrum of diseases.
The evolution of AAV technology has been marked by significant milestones. Early research in the 1980s and 1990s focused on understanding the basic biology of these viruses, while the 2000s witnessed the development of recombinant AAV vectors with enhanced transduction efficiency. Recent advancements have centered on engineering novel AAV capsids with improved tissue tropism and reduced immunogenicity, expanding their therapeutic potential.
The primary objective of AAV vector technology in modern gene therapy is to provide safe, efficient, and long-term gene expression in target tissues. Unlike other viral vectors, AAVs predominantly remain episomal rather than integrating into the host genome, significantly reducing the risk of insertional mutagenesis. This safety profile has been instrumental in gaining regulatory approvals for AAV-based therapies.
Current technical goals in the field include developing AAV vectors with increased packaging capacity beyond the traditional limit of approximately 4.7 kb, enhancing tissue-specific targeting capabilities, and overcoming pre-existing immunity challenges. Researchers are also focused on improving manufacturing processes to increase vector yield and purity, which remains critical for clinical applications.
The trajectory of AAV vector development is increasingly moving toward personalized medicine approaches. This includes the creation of designer AAVs tailored to specific disease conditions and patient populations. Computational and high-throughput screening methods are being employed to predict and optimize AAV capsid properties, representing a shift from traditional empirical approaches to more rational design strategies.
Another emerging trend is the application of AAV vectors in genome editing technologies, particularly CRISPR-Cas systems. The combination of these technologies offers unprecedented opportunities for precise genetic modifications, potentially revolutionizing the treatment of monogenic disorders and complex diseases alike.
As gene therapy transitions from experimental treatments to approved medical interventions, AAV vectors stand at the forefront of this therapeutic revolution. Their continued refinement and optimization will likely shape the future landscape of genetic medicine, potentially offering solutions for previously untreatable conditions and improving patient outcomes across a spectrum of diseases.
Market Analysis of AAV-based Gene Therapy Demand
The global market for AAV-based gene therapy has experienced remarkable growth, with current valuations reaching approximately $7.6 billion in 2023 and projected to exceed $25 billion by 2030, representing a compound annual growth rate (CAGR) of 18.7%. This substantial market expansion is primarily driven by the increasing prevalence of genetic disorders, growing acceptance of gene therapy approaches, and significant advancements in AAV vector technology.
North America currently dominates the market landscape, accounting for nearly 48% of global revenue, followed by Europe at 30% and Asia-Pacific at 18%. This regional distribution reflects the concentration of research institutions, biotechnology companies, and favorable regulatory frameworks in these regions. The United States specifically leads in clinical trials and commercialization efforts, with over 200 active clinical studies utilizing AAV vectors.
From a therapeutic application perspective, neurological disorders represent the largest market segment (32%), followed by ophthalmologic conditions (28%), cardiovascular diseases (15%), and muscular disorders (12%). This distribution aligns with AAV's natural tropism for certain tissues and the clinical success demonstrated in these therapeutic areas. Notably, Luxturna for inherited retinal dystrophy and Zolgensma for spinal muscular atrophy have achieved significant commercial success, validating the market potential.
Patient demand continues to grow exponentially, particularly for rare genetic disorders where traditional treatments offer limited efficacy. Market research indicates that approximately 400 million people worldwide suffer from rare diseases, with 80% having genetic origins - representing a vast untapped market for AAV-based therapies. Patient advocacy groups have become increasingly influential in driving research funding and regulatory approvals.
Healthcare payers and insurance providers have demonstrated willingness to cover these high-cost therapies due to their potential long-term benefits and cost-effectiveness compared to lifetime management of chronic genetic conditions. However, pricing remains a significant market challenge, with current therapies ranging from $425,000 to $2.1 million per treatment.
Manufacturing capacity represents a critical bottleneck in meeting market demand, with current global production capabilities estimated at only 15% of projected requirements for 2025. This supply-demand gap has spurred significant investment in manufacturing technologies and facilities, with over $4.5 billion committed to expanding production infrastructure over the past three years.
Emerging markets in Asia, particularly China and India, are experiencing the fastest growth rates in AAV therapy development, driven by government initiatives, increasing healthcare expenditure, and growing biotechnology sectors. These regions are expected to contribute significantly to market expansion in the coming decade.
North America currently dominates the market landscape, accounting for nearly 48% of global revenue, followed by Europe at 30% and Asia-Pacific at 18%. This regional distribution reflects the concentration of research institutions, biotechnology companies, and favorable regulatory frameworks in these regions. The United States specifically leads in clinical trials and commercialization efforts, with over 200 active clinical studies utilizing AAV vectors.
From a therapeutic application perspective, neurological disorders represent the largest market segment (32%), followed by ophthalmologic conditions (28%), cardiovascular diseases (15%), and muscular disorders (12%). This distribution aligns with AAV's natural tropism for certain tissues and the clinical success demonstrated in these therapeutic areas. Notably, Luxturna for inherited retinal dystrophy and Zolgensma for spinal muscular atrophy have achieved significant commercial success, validating the market potential.
Patient demand continues to grow exponentially, particularly for rare genetic disorders where traditional treatments offer limited efficacy. Market research indicates that approximately 400 million people worldwide suffer from rare diseases, with 80% having genetic origins - representing a vast untapped market for AAV-based therapies. Patient advocacy groups have become increasingly influential in driving research funding and regulatory approvals.
Healthcare payers and insurance providers have demonstrated willingness to cover these high-cost therapies due to their potential long-term benefits and cost-effectiveness compared to lifetime management of chronic genetic conditions. However, pricing remains a significant market challenge, with current therapies ranging from $425,000 to $2.1 million per treatment.
Manufacturing capacity represents a critical bottleneck in meeting market demand, with current global production capabilities estimated at only 15% of projected requirements for 2025. This supply-demand gap has spurred significant investment in manufacturing technologies and facilities, with over $4.5 billion committed to expanding production infrastructure over the past three years.
Emerging markets in Asia, particularly China and India, are experiencing the fastest growth rates in AAV therapy development, driven by government initiatives, increasing healthcare expenditure, and growing biotechnology sectors. These regions are expected to contribute significantly to market expansion in the coming decade.
Current Status and Challenges in AAV Vector Technology
Adeno-associated virus (AAV) vectors have emerged as leading delivery vehicles for gene therapy applications globally. Currently, AAV technology has achieved significant milestones with several approved therapies including Luxturna for inherited retinal dystrophy, Zolgensma for spinal muscular atrophy, and Hemgenix for hemophilia B. These approvals demonstrate the clinical viability of AAV-based approaches across diverse genetic disorders.
Despite these successes, AAV vector technology faces several critical challenges. Manufacturing scalability remains a significant hurdle, with current production systems struggling to meet the demand for clinical-grade vectors at commercially viable scales. The cost of goods for AAV-based therapies remains prohibitively high, with treatments often priced in the hundreds of thousands to millions of dollars per patient, limiting accessibility and market penetration.
Immunogenicity presents another major obstacle, as pre-existing neutralizing antibodies against AAV capsids are prevalent in human populations, potentially excluding 30-50% of patients from certain AAV serotype treatments. Additionally, adaptive immune responses following vector administration can eliminate transduced cells, compromising therapeutic efficacy and preventing vector readministration.
Packaging capacity limitations restrict AAV vectors to accommodating transgenes of approximately 4.7 kb, excluding many therapeutic genes for disorders requiring larger genetic payloads. This size constraint has necessitated complex split-vector approaches or alternative delivery strategies for conditions like Duchenne muscular dystrophy.
Tissue tropism specificity remains suboptimal, with current AAV serotypes showing preferential targeting to liver, central nervous system, or muscle, but lacking precision for many other clinically relevant tissues. Off-target transduction can lead to safety concerns and reduced therapeutic index.
The durability of transgene expression represents another challenge, particularly in dividing cell populations where episomal AAV genomes are diluted through cell division. This necessitates strategies for genomic integration or repeat dosing protocols to maintain therapeutic effect.
Regulatory frameworks for AAV-based therapies continue to evolve, with inconsistent requirements across different regions creating complexity in global development programs. Recent safety signals, including hepatotoxicity and oncogenicity concerns with some AAV vectors, have prompted increased scrutiny from regulatory agencies.
Technological innovations addressing these challenges include engineered capsids with enhanced tissue specificity, reduced immunogenicity, and improved manufacturing characteristics. Novel production platforms utilizing suspension cell culture systems and continuous processing are being developed to improve scalability and reduce costs.
Despite these successes, AAV vector technology faces several critical challenges. Manufacturing scalability remains a significant hurdle, with current production systems struggling to meet the demand for clinical-grade vectors at commercially viable scales. The cost of goods for AAV-based therapies remains prohibitively high, with treatments often priced in the hundreds of thousands to millions of dollars per patient, limiting accessibility and market penetration.
Immunogenicity presents another major obstacle, as pre-existing neutralizing antibodies against AAV capsids are prevalent in human populations, potentially excluding 30-50% of patients from certain AAV serotype treatments. Additionally, adaptive immune responses following vector administration can eliminate transduced cells, compromising therapeutic efficacy and preventing vector readministration.
Packaging capacity limitations restrict AAV vectors to accommodating transgenes of approximately 4.7 kb, excluding many therapeutic genes for disorders requiring larger genetic payloads. This size constraint has necessitated complex split-vector approaches or alternative delivery strategies for conditions like Duchenne muscular dystrophy.
Tissue tropism specificity remains suboptimal, with current AAV serotypes showing preferential targeting to liver, central nervous system, or muscle, but lacking precision for many other clinically relevant tissues. Off-target transduction can lead to safety concerns and reduced therapeutic index.
The durability of transgene expression represents another challenge, particularly in dividing cell populations where episomal AAV genomes are diluted through cell division. This necessitates strategies for genomic integration or repeat dosing protocols to maintain therapeutic effect.
Regulatory frameworks for AAV-based therapies continue to evolve, with inconsistent requirements across different regions creating complexity in global development programs. Recent safety signals, including hepatotoxicity and oncogenicity concerns with some AAV vectors, have prompted increased scrutiny from regulatory agencies.
Technological innovations addressing these challenges include engineered capsids with enhanced tissue specificity, reduced immunogenicity, and improved manufacturing characteristics. Novel production platforms utilizing suspension cell culture systems and continuous processing are being developed to improve scalability and reduce costs.
Current AAV Vector Delivery Systems and Approaches
01 AAV vector design and engineering
Adeno-associated virus (AAV) vectors can be engineered to improve their efficiency as gene delivery vehicles. This includes modifications to the viral capsid structure to enhance tissue tropism, reduce immunogenicity, and increase transduction efficiency. Various serotypes of AAV vectors have been developed with different tissue specificities, allowing for targeted gene delivery to specific organs or cell types. Engineering approaches also focus on optimizing the vector genome to improve transgene expression and packaging capacity.- AAV vector design and engineering: Adeno-associated virus vectors can be engineered to improve their efficiency and specificity for gene therapy applications. This includes modifications to the viral capsid proteins to alter tissue tropism, enhance transduction efficiency, and evade immune responses. Various serotypes of AAV (AAV1-AAV9) have different natural tropisms that can be exploited for targeting specific tissues. Advanced engineering techniques include directed evolution, rational design, and chimeric capsid development to create novel vectors with desired properties.
- AAV production and purification methods: Methods for producing high-titer, clinical-grade AAV vectors are critical for therapeutic applications. This includes optimized cell culture systems, transfection protocols, and helper virus functions. Purification techniques such as density gradient ultracentrifugation, chromatography, and filtration are employed to obtain pure AAV preparations. Quality control measures ensure the removal of contaminants, empty capsids, and aggregates. Scalable manufacturing processes have been developed to meet the demands of clinical trials and commercial applications.
- Therapeutic applications of AAV vectors: AAV vectors are widely used in gene therapy for treating various genetic disorders and acquired diseases. They have shown promise in clinical trials for conditions such as hemophilia, spinal muscular atrophy, retinal disorders, and neurodegenerative diseases. The ability of AAV to provide long-term transgene expression in non-dividing cells makes them particularly suitable for treating chronic conditions. Different routes of administration, including systemic, intramuscular, intrathecal, and subretinal delivery, have been developed to target specific tissues and organs.
- Immune responses to AAV vectors: Pre-existing immunity to AAV capsids and immune responses generated after vector administration can limit the efficacy of AAV-mediated gene therapy. Strategies to overcome these challenges include immunomodulation protocols, capsid engineering to evade neutralizing antibodies, and alternative serotype selection. The development of empty capsid decoys, novel immunosuppressive regimens, and liver-directed expression to induce tolerance are approaches being explored to mitigate immune responses. Understanding the mechanisms of innate and adaptive immunity to AAV is crucial for improving vector design.
- Novel AAV vector delivery systems: Innovative delivery systems for AAV vectors aim to enhance targeting specificity, increase transduction efficiency, and reduce off-target effects. These include hybrid vectors combining AAV with other delivery platforms, nanoparticle formulations, and targeted delivery using cell-specific promoters or ligands. Controlled release systems, tissue-specific enhancers, and microRNA-regulated expression cassettes provide additional layers of specificity. Advanced delivery methods such as focused ultrasound-mediated blood-brain barrier opening and direct cerebrospinal fluid administration are being developed for central nervous system applications.
02 AAV production and purification methods
Various methods have been developed for the production and purification of adeno-associated virus vectors for gene therapy applications. These include cell culture systems for virus propagation, transfection protocols for vector packaging, and downstream processing techniques such as chromatography and ultracentrifugation for vector purification. Innovations in manufacturing processes aim to increase vector yield, purity, and stability while reducing production costs and ensuring consistent quality for clinical applications.Expand Specific Solutions03 Therapeutic applications of AAV vectors
Adeno-associated virus vectors are widely used in gene therapy for treating various diseases. They can deliver therapeutic genes to target tissues for the treatment of genetic disorders, neurodegenerative diseases, cardiovascular conditions, and certain cancers. AAV vectors have shown promise in clinical trials for conditions such as hemophilia, retinal disorders, muscular dystrophy, and central nervous system diseases. Their ability to provide long-term gene expression in non-dividing cells makes them particularly valuable for treating chronic conditions requiring sustained therapeutic protein production.Expand Specific Solutions04 Immune responses to AAV vectors
The immune response to adeno-associated virus vectors presents a significant challenge in gene therapy. Pre-existing immunity to wild-type AAV in humans can neutralize therapeutic vectors, reducing their efficacy. Additionally, immune responses against the vector capsid or transgene product can limit long-term expression and prevent re-administration. Strategies to overcome these challenges include immunomodulation protocols, capsid engineering to evade neutralizing antibodies, alternative administration routes, and vector dosing optimization to improve the safety and efficacy of AAV-based gene therapies.Expand Specific Solutions05 Novel AAV serotypes and variants
Research has led to the discovery and development of novel AAV serotypes and engineered variants with enhanced properties for gene therapy. These include naturally occurring serotypes with unique tissue tropisms and synthetic or evolved capsid variants with improved transduction efficiency, reduced immunogenicity, or altered tissue specificity. High-throughput screening and directed evolution approaches have generated AAV variants capable of crossing biological barriers, such as the blood-brain barrier, or targeting specific cell types with greater precision, expanding the therapeutic potential of AAV-based gene delivery systems.Expand Specific Solutions
Key Industry Players in AAV Vector Research
The adeno-associated virus (AAV) vector market in gene therapy is currently in a rapid growth phase, with an expanding market size projected to reach billions by 2027. The technology has matured significantly over the past decade, transitioning from experimental to clinical applications with several FDA-approved therapies. Leading pharmaceutical companies like Novartis and specialized biotechs such as Oxford Biomedica and uniQure have established strong positions in the field. Academic institutions including University of Florida, Scripps Research Institute, and Sichuan University continue to drive innovation through foundational research. The competitive landscape features a mix of established players and emerging companies, with increasing collaboration between research institutions and industry partners. Technical challenges in manufacturing scale-up and immune responses remain areas for competitive differentiation as the field advances toward broader therapeutic applications.
University of Florida
Technical Solution: University of Florida has pioneered AAV vector technology through their Gene Therapy Center, developing novel serotypes with enhanced tissue tropism and reduced immunogenicity. Their platform includes AAV vectors with modified capsid proteins that allow for improved transduction efficiency in specific tissues, particularly in neurological and ocular applications. They've engineered AAV vectors with reduced neutralizing antibody recognition, addressing one of the key challenges in gene therapy. Their research has led to the development of self-complementary AAV vectors that bypass the rate-limiting second-strand DNA synthesis step, resulting in more rapid and efficient transgene expression[1]. Additionally, they've established scalable manufacturing processes using insect cell-based systems that yield higher vector titers compared to traditional mammalian cell production methods[3].
Strengths: Extensive expertise in AAV vector engineering with multiple patented serotypes; established manufacturing platforms with superior yields; strong clinical translation record. Weaknesses: Some of their proprietary vectors face licensing restrictions; potential immunogenicity issues remain for repeat dosing applications; limited payload capacity compared to other viral vectors.
Novartis AG
Technical Solution: Novartis has developed a comprehensive AAV vector platform for gene therapy applications, centered around their Zolgensma® treatment for spinal muscular atrophy (SMA). Their technology utilizes AAV9 serotype vectors that can cross the blood-brain barrier, enabling effective targeting of motor neurons in the central nervous system. The company has implemented a proprietary manufacturing process using a triple transfection method in HEK293 cells, which has been scaled to commercial levels with consistent quality attributes. Their AAV vectors incorporate self-complementary DNA technology to enhance transgene expression and utilize specific promoters for tissue-selective expression[2]. Novartis has also developed analytical methods for vector characterization, including digital PCR for genome titration and cell-based potency assays that correlate with clinical outcomes[4]. Their platform includes strategies to manage immunogenicity through transient immunosuppression protocols during treatment.
Strengths: Established commercial manufacturing capability at scale; proven clinical efficacy with approved AAV-based therapies; robust analytical platform for product characterization. Weaknesses: High treatment costs limiting accessibility; pre-existing immunity to AAV9 excludes approximately 50% of potential patients; single-dose administration strategy without option for redosing due to immune responses.
Critical Patents and Innovations in AAV Vector Design
Adeno-associated virus gene therapy products and methods
PatentWO2024015794A3
Innovation
- Dual-function AAV gene therapy vectors that simultaneously express a therapeutic protein/RNA to treat genetic defects and an anti-inflammatory protein/peptide to address neuroinflammation.
- Use of self-cleaving peptides to create fusion proteins that can efficiently separate therapeutic and anti-inflammatory components after translation.
- Secretion of anti-inflammatory proteins from transduced cells to treat microglial activation in the surrounding environment, addressing the neuroinflammatory component of neurodegenerative diseases.
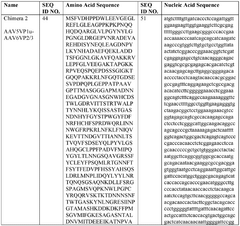
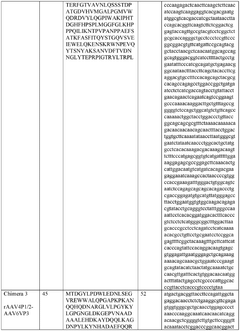
Modified adeno-associated viral vectors for use in genetic engineering
PatentWO2020142236A1
Innovation
- The development of modified AAV vectors that include specific amino acid substitutions in the AAP polypeptides, particularly in the helical regions of VP2 and VP3, enhance the production titer and infectivity of AAV particles, allowing for improved transgene delivery and targeting capabilities.
Safety and Immunogenicity Considerations for AAV Vectors
Safety considerations for AAV vectors remain paramount in the advancement of gene therapy applications. Despite their generally favorable safety profile compared to other viral vectors, AAV vectors still present several challenges that require careful assessment. Pre-existing immunity to AAV capsids represents a significant concern, as approximately 30-80% of the human population carries neutralizing antibodies against various AAV serotypes, particularly AAV2. This immune response can substantially reduce transduction efficiency and therapeutic efficacy, necessitating patient screening prior to treatment.
Capsid-directed CD8+ T cell responses constitute another critical immunological barrier. Following AAV vector administration, cellular immune responses against transduced cells can lead to clearance of these cells, potentially resulting in transient therapeutic effects and elevated liver enzymes in some patients. This phenomenon has been observed in clinical trials for hemophilia B and other disorders, highlighting the need for immunomodulatory strategies.
Vector dose-dependent toxicity presents additional safety concerns. High vector doses, often necessary to achieve therapeutic efficacy, may trigger innate immune responses characterized by cytokine release and complement activation. These responses can manifest as systemic inflammatory reactions ranging from mild to severe, with documented cases of severe adverse events in high-dose AAV clinical trials, including several fatalities reported between 2019-2022.
Manufacturing-related impurities further complicate the safety profile of AAV vectors. Empty capsids, host cell proteins, and residual DNA can contribute to immunogenicity and potentially reduce efficacy. Advanced purification methods are continuously being developed to address these challenges and improve vector quality.
Insertional mutagenesis risk, while lower than with retroviral vectors, remains a theoretical concern with AAV vectors. Although AAV predominantly exists episomally, integration events can occur at low frequencies, particularly at sites of DNA damage, necessitating long-term safety monitoring of treated patients.
To address these challenges, researchers are developing innovative strategies including engineered capsids with reduced immunogenicity, transient immunosuppression protocols, plasmapheresis to remove neutralizing antibodies, and empty capsid decoys. Alternative administration routes and improved manufacturing processes are also being explored to enhance safety profiles.
Regulatory frameworks continue to evolve in response to emerging safety data, with agencies implementing risk mitigation strategies and standardized assessment protocols for AAV-based therapies. The balance between achieving therapeutic efficacy and maintaining acceptable safety margins remains a central focus in the ongoing development of AAV vector technologies for gene therapy applications.
Capsid-directed CD8+ T cell responses constitute another critical immunological barrier. Following AAV vector administration, cellular immune responses against transduced cells can lead to clearance of these cells, potentially resulting in transient therapeutic effects and elevated liver enzymes in some patients. This phenomenon has been observed in clinical trials for hemophilia B and other disorders, highlighting the need for immunomodulatory strategies.
Vector dose-dependent toxicity presents additional safety concerns. High vector doses, often necessary to achieve therapeutic efficacy, may trigger innate immune responses characterized by cytokine release and complement activation. These responses can manifest as systemic inflammatory reactions ranging from mild to severe, with documented cases of severe adverse events in high-dose AAV clinical trials, including several fatalities reported between 2019-2022.
Manufacturing-related impurities further complicate the safety profile of AAV vectors. Empty capsids, host cell proteins, and residual DNA can contribute to immunogenicity and potentially reduce efficacy. Advanced purification methods are continuously being developed to address these challenges and improve vector quality.
Insertional mutagenesis risk, while lower than with retroviral vectors, remains a theoretical concern with AAV vectors. Although AAV predominantly exists episomally, integration events can occur at low frequencies, particularly at sites of DNA damage, necessitating long-term safety monitoring of treated patients.
To address these challenges, researchers are developing innovative strategies including engineered capsids with reduced immunogenicity, transient immunosuppression protocols, plasmapheresis to remove neutralizing antibodies, and empty capsid decoys. Alternative administration routes and improved manufacturing processes are also being explored to enhance safety profiles.
Regulatory frameworks continue to evolve in response to emerging safety data, with agencies implementing risk mitigation strategies and standardized assessment protocols for AAV-based therapies. The balance between achieving therapeutic efficacy and maintaining acceptable safety margins remains a central focus in the ongoing development of AAV vector technologies for gene therapy applications.
Regulatory Framework for AAV-mediated Gene Therapy
The regulatory landscape for AAV-mediated gene therapy has evolved significantly over the past two decades, reflecting both scientific advancements and growing clinical applications. The U.S. Food and Drug Administration (FDA) has established a comprehensive framework through its Center for Biologics Evaluation and Research (CBER), which oversees the approval pathway for gene therapy products, including those utilizing AAV vectors.
The European Medicines Agency (EMA) has developed parallel but distinct regulatory guidelines, implementing the Advanced Therapy Medicinal Products (ATMP) classification which specifically addresses gene therapy medicinal products (GTMPs). This framework provides specialized evaluation procedures while maintaining rigorous safety standards for AAV vector-based therapies.
Regulatory considerations for AAV-mediated gene therapies encompass several critical dimensions. Vector characterization requirements mandate detailed molecular profiling of AAV vectors, including capsid protein composition, genome integrity, and potential contaminants. Manufacturing consistency must be demonstrated through validated quality control measures that ensure batch-to-batch reproducibility.
Safety assessment protocols are particularly stringent, requiring comprehensive preclinical toxicology studies addressing biodistribution, persistence, and potential for germline transmission. Immunogenicity concerns receive special attention due to the prevalence of pre-existing neutralizing antibodies against AAV serotypes in human populations.
Long-term patient monitoring represents another regulatory cornerstone, with requirements for extended follow-up periods ranging from 5 to 15 years depending on the jurisdiction and indication. This reflects concerns about delayed adverse events and potential integration-related risks, despite AAV's predominantly episomal persistence.
Recent regulatory innovations include accelerated approval pathways for rare disease treatments, such as the FDA's Regenerative Medicine Advanced Therapy (RMAT) designation and the EMA's Priority Medicines (PRIME) scheme. These mechanisms facilitate expedited development while maintaining safety standards for promising AAV therapies addressing unmet medical needs.
Global harmonization efforts are underway through initiatives like the International Council for Harmonisation (ICH), which aims to standardize requirements across major regulatory bodies. However, significant regional variations persist in areas such as environmental risk assessment and patient eligibility criteria for clinical trials.
The regulatory framework continues to evolve in response to emerging challenges, including the development of novel AAV serotypes, redosing strategies, and manufacturing scalability concerns. Regulatory agencies increasingly engage in early dialogue with developers through programs like the FDA's INTERACT meetings to address these complex issues proactively.
The European Medicines Agency (EMA) has developed parallel but distinct regulatory guidelines, implementing the Advanced Therapy Medicinal Products (ATMP) classification which specifically addresses gene therapy medicinal products (GTMPs). This framework provides specialized evaluation procedures while maintaining rigorous safety standards for AAV vector-based therapies.
Regulatory considerations for AAV-mediated gene therapies encompass several critical dimensions. Vector characterization requirements mandate detailed molecular profiling of AAV vectors, including capsid protein composition, genome integrity, and potential contaminants. Manufacturing consistency must be demonstrated through validated quality control measures that ensure batch-to-batch reproducibility.
Safety assessment protocols are particularly stringent, requiring comprehensive preclinical toxicology studies addressing biodistribution, persistence, and potential for germline transmission. Immunogenicity concerns receive special attention due to the prevalence of pre-existing neutralizing antibodies against AAV serotypes in human populations.
Long-term patient monitoring represents another regulatory cornerstone, with requirements for extended follow-up periods ranging from 5 to 15 years depending on the jurisdiction and indication. This reflects concerns about delayed adverse events and potential integration-related risks, despite AAV's predominantly episomal persistence.
Recent regulatory innovations include accelerated approval pathways for rare disease treatments, such as the FDA's Regenerative Medicine Advanced Therapy (RMAT) designation and the EMA's Priority Medicines (PRIME) scheme. These mechanisms facilitate expedited development while maintaining safety standards for promising AAV therapies addressing unmet medical needs.
Global harmonization efforts are underway through initiatives like the International Council for Harmonisation (ICH), which aims to standardize requirements across major regulatory bodies. However, significant regional variations persist in areas such as environmental risk assessment and patient eligibility criteria for clinical trials.
The regulatory framework continues to evolve in response to emerging challenges, including the development of novel AAV serotypes, redosing strategies, and manufacturing scalability concerns. Regulatory agencies increasingly engage in early dialogue with developers through programs like the FDA's INTERACT meetings to address these complex issues proactively.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!