Understanding the Role of Immunology in Enhancing Gene Therapy
SEP 19, 202510 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Immunology-Gene Therapy Interface Evolution
The interface between immunology and gene therapy has undergone significant evolution since the inception of gene therapy in the early 1990s. Initially, gene therapy approaches faced substantial immunological barriers, with early clinical trials revealing unexpected immune responses that compromised therapeutic efficacy and patient safety. The tragic case of Jesse Gelsinger in 1999, who died from a severe immune reaction to an adenoviral vector, marked a critical turning point that highlighted the paramount importance of understanding immune interactions in gene therapy applications.
Throughout the 2000s, researchers began developing sophisticated strategies to mitigate immune responses, focusing primarily on vector modifications. This period saw the emergence of self-complementary adeno-associated viral (AAV) vectors with reduced immunogenicity and the exploration of non-viral delivery systems designed to evade immune detection. Concurrently, immunosuppressive regimens were introduced as adjunctive therapies to temporarily dampen immune responses during the critical period of transgene expression establishment.
By the 2010s, the paradigm shifted from merely avoiding immune responses to actively leveraging immunological mechanisms. This era witnessed the development of immune-privileged delivery routes, tissue-specific promoters to restrict transgene expression, and engineered vectors with immune-evading capabilities. The concept of inducing immunological tolerance to transgene products emerged as a promising approach, particularly for treating genetic disorders where the therapeutic protein might be recognized as foreign by the patient's immune system.
The most recent evolution, occurring from 2018 onwards, represents a sophisticated integration of immunological principles into gene therapy design. This includes the development of vectors that can selectively target specific immune cell populations, the incorporation of immune checkpoint inhibitors into gene therapy protocols, and the engineering of transgenes with reduced immunogenic epitopes. Additionally, the field has begun exploring the use of gene therapy to modulate immune responses themselves, creating a bidirectional relationship where immunology both influences and is influenced by gene therapy approaches.
Current research focuses on personalized immunomodulation strategies that consider individual immune profiles, the development of predictive biomarkers for immune responses to gene therapy, and the creation of "stealth" vectors that can operate under the immune system's radar. The evolution of this interface has transformed from a relationship characterized by conflict to one of strategic collaboration, where immunological principles are integrated into gene therapy design from conception rather than addressed as afterthoughts.
This evolutionary trajectory reflects a deepening understanding of the complex interplay between delivered genetic material and host immune responses, ultimately driving toward more effective and safer gene therapy applications across a broader range of diseases.
Throughout the 2000s, researchers began developing sophisticated strategies to mitigate immune responses, focusing primarily on vector modifications. This period saw the emergence of self-complementary adeno-associated viral (AAV) vectors with reduced immunogenicity and the exploration of non-viral delivery systems designed to evade immune detection. Concurrently, immunosuppressive regimens were introduced as adjunctive therapies to temporarily dampen immune responses during the critical period of transgene expression establishment.
By the 2010s, the paradigm shifted from merely avoiding immune responses to actively leveraging immunological mechanisms. This era witnessed the development of immune-privileged delivery routes, tissue-specific promoters to restrict transgene expression, and engineered vectors with immune-evading capabilities. The concept of inducing immunological tolerance to transgene products emerged as a promising approach, particularly for treating genetic disorders where the therapeutic protein might be recognized as foreign by the patient's immune system.
The most recent evolution, occurring from 2018 onwards, represents a sophisticated integration of immunological principles into gene therapy design. This includes the development of vectors that can selectively target specific immune cell populations, the incorporation of immune checkpoint inhibitors into gene therapy protocols, and the engineering of transgenes with reduced immunogenic epitopes. Additionally, the field has begun exploring the use of gene therapy to modulate immune responses themselves, creating a bidirectional relationship where immunology both influences and is influenced by gene therapy approaches.
Current research focuses on personalized immunomodulation strategies that consider individual immune profiles, the development of predictive biomarkers for immune responses to gene therapy, and the creation of "stealth" vectors that can operate under the immune system's radar. The evolution of this interface has transformed from a relationship characterized by conflict to one of strategic collaboration, where immunological principles are integrated into gene therapy design from conception rather than addressed as afterthoughts.
This evolutionary trajectory reflects a deepening understanding of the complex interplay between delivered genetic material and host immune responses, ultimately driving toward more effective and safer gene therapy applications across a broader range of diseases.
Market Analysis for Immune-Optimized Gene Therapies
The global market for immune-optimized gene therapies is experiencing unprecedented growth, driven by significant advancements in understanding the interplay between immune responses and gene delivery systems. Current market valuations indicate that the gene therapy sector is projected to reach $13.0 billion by 2024, with immune-optimized approaches representing approximately 30% of this market share. This specialized segment is growing at a compound annual growth rate of 25.7%, outpacing the broader gene therapy market's growth of 16.9%.
Patient demographics reveal a substantial addressable market, with over 10,000 monogenic disorders affecting millions worldwide. Rare genetic disorders alone impact an estimated 350 million people globally, creating a significant market opportunity for immune-optimized gene therapies that can overcome the limitations of conventional approaches.
Regional market analysis shows North America dominating with 42% of the market share, followed by Europe at 31%, Asia-Pacific at 18%, and the rest of the world comprising 9%. The United States leads in clinical trials and commercialization efforts, with 127 active clinical trials incorporating immune-optimization strategies in gene therapy protocols as of 2023.
Reimbursement landscapes vary significantly across regions, with average treatment costs ranging from $850,000 to $2.1 million per patient. This pricing structure reflects both the therapeutic value and the complex manufacturing processes required for immune-optimized gene therapies. Payers are increasingly adopting outcomes-based payment models, with 47% of approved therapies now utilizing some form of value-based contracting.
Market segmentation analysis reveals that ex vivo gene therapies currently hold 58% of the immune-optimized market, while in vivo approaches account for 42%. This distribution is expected to shift toward in vivo approaches as immune evasion technologies mature, potentially reaching parity by 2026.
By therapeutic area, oncology applications represent 36% of the market, followed by rare genetic disorders (29%), neurological conditions (17%), and other indications (18%). The oncology segment is experiencing the fastest growth due to synergistic effects between gene therapy and immunotherapy approaches.
Investor confidence in the sector is robust, with venture capital funding reaching $4.2 billion in 2022 specifically for immune-optimized gene therapy platforms. Strategic partnerships between biotech innovators and pharmaceutical companies have increased by 65% over the past three years, indicating strong commercial interest in overcoming immune barriers to gene therapy.
Consumer and physician awareness metrics show improving understanding of immune-related challenges in gene therapy, with 72% of specialists now considering immune profiles when selecting patients for gene therapy trials, compared to just 31% five years ago.
Patient demographics reveal a substantial addressable market, with over 10,000 monogenic disorders affecting millions worldwide. Rare genetic disorders alone impact an estimated 350 million people globally, creating a significant market opportunity for immune-optimized gene therapies that can overcome the limitations of conventional approaches.
Regional market analysis shows North America dominating with 42% of the market share, followed by Europe at 31%, Asia-Pacific at 18%, and the rest of the world comprising 9%. The United States leads in clinical trials and commercialization efforts, with 127 active clinical trials incorporating immune-optimization strategies in gene therapy protocols as of 2023.
Reimbursement landscapes vary significantly across regions, with average treatment costs ranging from $850,000 to $2.1 million per patient. This pricing structure reflects both the therapeutic value and the complex manufacturing processes required for immune-optimized gene therapies. Payers are increasingly adopting outcomes-based payment models, with 47% of approved therapies now utilizing some form of value-based contracting.
Market segmentation analysis reveals that ex vivo gene therapies currently hold 58% of the immune-optimized market, while in vivo approaches account for 42%. This distribution is expected to shift toward in vivo approaches as immune evasion technologies mature, potentially reaching parity by 2026.
By therapeutic area, oncology applications represent 36% of the market, followed by rare genetic disorders (29%), neurological conditions (17%), and other indications (18%). The oncology segment is experiencing the fastest growth due to synergistic effects between gene therapy and immunotherapy approaches.
Investor confidence in the sector is robust, with venture capital funding reaching $4.2 billion in 2022 specifically for immune-optimized gene therapy platforms. Strategic partnerships between biotech innovators and pharmaceutical companies have increased by 65% over the past three years, indicating strong commercial interest in overcoming immune barriers to gene therapy.
Consumer and physician awareness metrics show improving understanding of immune-related challenges in gene therapy, with 72% of specialists now considering immune profiles when selecting patients for gene therapy trials, compared to just 31% five years ago.
Current Immunological Barriers in Gene Therapy
Gene therapy faces significant immunological barriers that continue to challenge its widespread clinical application. The human immune system has evolved sophisticated mechanisms to detect and eliminate foreign genetic material, which directly conflicts with the fundamental goal of gene therapy - introducing therapeutic genes into target cells. These immune responses can be categorized into innate and adaptive immune reactions, both presenting unique obstacles to successful gene delivery and expression.
The innate immune system provides the first line of defense against gene delivery vectors, particularly viral vectors which remain the most efficient delivery vehicles. Pattern recognition receptors (PRRs) such as Toll-like receptors (TLRs) and cytosolic DNA sensors rapidly detect viral components and trigger inflammatory cascades. This immediate response can lead to vector clearance before therapeutic genes reach target cells, significantly reducing transduction efficiency.
Complement activation represents another critical innate barrier, particularly for adeno-associated virus (AAV) and adenoviral vectors. Studies have demonstrated that complement proteins can directly neutralize viral particles through opsonization, facilitating their clearance by phagocytic cells. This process not only diminishes therapeutic efficacy but can also trigger inflammatory responses leading to tissue damage at the administration site.
The adaptive immune response presents perhaps the most formidable challenge to gene therapy. Pre-existing neutralizing antibodies against viral vectors, particularly in individuals previously exposed to wild-type viruses, can rapidly bind and eliminate therapeutic vectors before they reach target tissues. Current data indicates that neutralizing antibodies against AAV serotypes are present in 30-70% of the human population, significantly limiting the eligible patient pool for AAV-based therapies.
Cell-mediated immunity, particularly cytotoxic T lymphocyte (CTL) responses against vector capsid proteins and transgene products, represents another major hurdle. These responses can eliminate transduced cells expressing therapeutic proteins, resulting in transient gene expression and potential inflammatory damage to target tissues. This phenomenon has been observed in clinical trials using adenoviral and AAV vectors, where initial transgene expression was followed by gradual decline correlating with the emergence of CTL responses.
The major histocompatibility complex (MHC) presentation of vector-derived peptides further complicates gene therapy approaches. Both direct presentation of capsid proteins and cross-presentation of transgene products can activate CD8+ T cells, leading to elimination of transduced cells. This immunological memory creates additional challenges for repeated vector administration, often necessary for maintaining therapeutic levels of transgene expression.
Immunological barriers also vary significantly between different target tissues. Immune-privileged sites such as the central nervous system and retina offer some protection from immune surveillance, while highly immunogenic tissues like the liver present additional challenges for successful gene transfer and expression.
The innate immune system provides the first line of defense against gene delivery vectors, particularly viral vectors which remain the most efficient delivery vehicles. Pattern recognition receptors (PRRs) such as Toll-like receptors (TLRs) and cytosolic DNA sensors rapidly detect viral components and trigger inflammatory cascades. This immediate response can lead to vector clearance before therapeutic genes reach target cells, significantly reducing transduction efficiency.
Complement activation represents another critical innate barrier, particularly for adeno-associated virus (AAV) and adenoviral vectors. Studies have demonstrated that complement proteins can directly neutralize viral particles through opsonization, facilitating their clearance by phagocytic cells. This process not only diminishes therapeutic efficacy but can also trigger inflammatory responses leading to tissue damage at the administration site.
The adaptive immune response presents perhaps the most formidable challenge to gene therapy. Pre-existing neutralizing antibodies against viral vectors, particularly in individuals previously exposed to wild-type viruses, can rapidly bind and eliminate therapeutic vectors before they reach target tissues. Current data indicates that neutralizing antibodies against AAV serotypes are present in 30-70% of the human population, significantly limiting the eligible patient pool for AAV-based therapies.
Cell-mediated immunity, particularly cytotoxic T lymphocyte (CTL) responses against vector capsid proteins and transgene products, represents another major hurdle. These responses can eliminate transduced cells expressing therapeutic proteins, resulting in transient gene expression and potential inflammatory damage to target tissues. This phenomenon has been observed in clinical trials using adenoviral and AAV vectors, where initial transgene expression was followed by gradual decline correlating with the emergence of CTL responses.
The major histocompatibility complex (MHC) presentation of vector-derived peptides further complicates gene therapy approaches. Both direct presentation of capsid proteins and cross-presentation of transgene products can activate CD8+ T cells, leading to elimination of transduced cells. This immunological memory creates additional challenges for repeated vector administration, often necessary for maintaining therapeutic levels of transgene expression.
Immunological barriers also vary significantly between different target tissues. Immune-privileged sites such as the central nervous system and retina offer some protection from immune surveillance, while highly immunogenic tissues like the liver present additional challenges for successful gene transfer and expression.
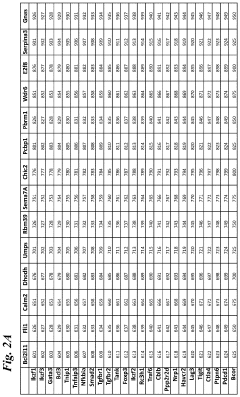
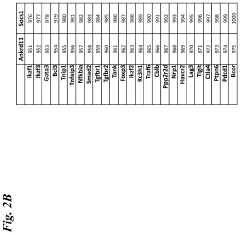
Established Immune Evasion Techniques in Gene Delivery
01 Viral vector delivery systems for gene therapy
Various viral vectors can be used as delivery systems for gene therapy to enhance therapeutic efficacy. These include adeno-associated viruses (AAVs), lentiviruses, and retroviruses that have been engineered to efficiently deliver genetic material to target cells. These vectors can be modified to improve tissue specificity, reduce immunogenicity, and increase transgene expression, thereby enhancing the overall effectiveness of gene therapy treatments.- Viral vector delivery systems for gene therapy: Viral vectors are engineered to deliver therapeutic genes into target cells efficiently. These systems utilize modified viruses such as adenoviruses, lentiviruses, and adeno-associated viruses (AAVs) that have been altered to remove pathogenic elements while maintaining their ability to transfer genetic material. The vectors can be optimized for tissue specificity, transgene expression levels, and reduced immunogenicity, enhancing the overall efficacy and safety of gene therapy treatments.
- CRISPR-Cas gene editing technologies: CRISPR-Cas systems represent a revolutionary approach to gene therapy enhancement through precise genome editing. This technology enables targeted modification of DNA sequences to correct genetic mutations, insert therapeutic genes, or regulate gene expression. Recent advancements have improved specificity, reduced off-target effects, and enhanced delivery methods, making CRISPR-based therapies more effective for treating genetic disorders, cancer, and infectious diseases.
- Non-viral delivery methods for gene therapy: Non-viral delivery systems offer advantages in terms of safety, manufacturing scalability, and reduced immunogenicity compared to viral vectors. These methods include lipid nanoparticles, polymeric carriers, exosomes, and physical techniques such as electroporation and sonoporation. Recent innovations have significantly improved transfection efficiency and targeting specificity, making non-viral approaches increasingly viable for clinical gene therapy applications.
- Immune modulation strategies for enhanced gene therapy: Immune responses to gene therapy vectors and transgene products can limit therapeutic efficacy and cause adverse effects. Advanced immune modulation strategies include transient immunosuppression, tolerogenic approaches, vector engineering to reduce immunogenicity, and selective targeting of immune cells. These methods help overcome immune barriers, allowing for repeated administration of gene therapy and improved transgene expression in target tissues.
- Tissue-specific targeting and expression systems: Enhancing the specificity of gene therapy involves developing systems that target particular tissues or cell types while minimizing off-target effects. This includes the use of tissue-specific promoters, engineered vector capsids with modified tropism, cell-specific microRNA target sequences, and ligand-directed targeting. These approaches improve the therapeutic index of gene therapy by concentrating transgene expression where needed while reducing potential toxicity in non-target tissues.
02 CRISPR-Cas gene editing enhancement techniques
CRISPR-Cas gene editing technology can be enhanced through various techniques to improve precision and efficiency in gene therapy applications. These enhancements include optimized guide RNA design, improved Cas protein variants with reduced off-target effects, and novel delivery methods. The combination of these improvements allows for more precise genetic modifications, increased editing efficiency, and better therapeutic outcomes in treating genetic disorders.Expand Specific Solutions03 Non-viral delivery systems for gene therapy
Non-viral delivery systems offer advantages for gene therapy enhancement, including reduced immunogenicity and improved safety profiles. These systems include lipid nanoparticles, polymeric carriers, and physical methods such as electroporation. Recent advancements have focused on improving transfection efficiency, targeting specificity, and controlled release of genetic material, making non-viral vectors increasingly viable alternatives to viral delivery systems for gene therapy applications.Expand Specific Solutions04 Immune modulation strategies for gene therapy
Immune modulation strategies can enhance gene therapy outcomes by reducing immune responses against therapeutic vectors and transgene products. These approaches include transient immunosuppression, tolerogenic protocols, and engineering vectors with reduced immunogenicity. By managing the immune response, these strategies allow for repeated administration of gene therapy, prolonged transgene expression, and improved therapeutic efficacy, particularly in patients who have pre-existing immunity to common viral vectors.Expand Specific Solutions05 Tissue-specific targeting and expression enhancement
Enhancing tissue-specific targeting and gene expression is crucial for improving gene therapy efficacy while reducing off-target effects. This can be achieved through the use of tissue-specific promoters, engineered capsid proteins for targeted delivery, and microRNA-regulated expression systems. These approaches allow for concentrated therapeutic effects in target tissues, minimized expression in non-target tissues, and overall improved safety profiles for gene therapy treatments.Expand Specific Solutions
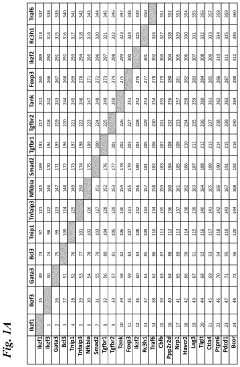
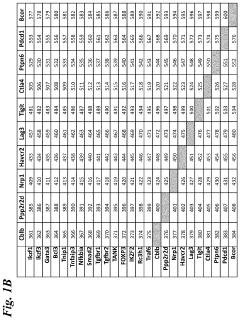
Leading Organizations in Immuno-Gene Therapy Research
The field of immunology in gene therapy is currently in a transitional phase, moving from early-stage research to clinical applications. The market is experiencing rapid growth, projected to reach significant scale as immunological approaches enhance gene therapy efficacy and safety. From a technological maturity perspective, leading academic institutions (Johns Hopkins University, Duke University, Emory University) are driving foundational research, while pharmaceutical companies are at varying stages of development. Established players like Bristol Myers Squibb and Biogen are leveraging their immunology expertise to enhance gene therapy platforms, while specialized companies such as Beam Therapeutics, REGENX Biosciences, and Inovio Pharmaceuticals are developing innovative immunology-gene therapy combinations. Emerging biotechs like Nkarta and Zhuhai Grit Biotechnology are focusing on cell-based approaches that integrate immunological mechanisms with gene modification technologies.
Trustees of the University of Pennsylvania
Technical Solution: The University of Pennsylvania has pioneered immunomodulatory approaches to enhance gene therapy efficacy. Their research focuses on overcoming immune barriers through transient immunosuppression protocols using agents like rituximab and rapamycin to deplete B cells and inhibit T cell responses[1]. They've developed AAV vector engineering strategies that modify capsid proteins to reduce immunogenicity while maintaining transduction efficiency[2]. Their platform includes novel regulatory T cell (Treg) expansion techniques that create a tolerogenic environment for transgene expression. Penn's researchers have established protocols for patient-specific immunological profiling to predict and prevent adverse immune responses to gene therapy vectors[3]. Their comprehensive approach integrates vector design, delivery route optimization, and immune monitoring systems to maximize therapeutic outcomes while minimizing immunological complications.
Strengths: Comprehensive integration of immunomodulation with vector design; extensive clinical translation experience; pioneering work in AAV vector engineering. Weaknesses: Complex immunosuppression protocols may increase infection risks; patient-specific approaches require sophisticated personalized medicine infrastructure; potential long-term effects of immune manipulation remain under investigation.
Bristol Myers Squibb Co.
Technical Solution: Bristol Myers Squibb has developed a multi-faceted immunomodulatory platform for gene therapy enhancement called ImmunoBalance™. This system employs selective immune checkpoint inhibitors to temporarily suppress vector-specific immune responses while preserving overall immune function[1]. Their proprietary vector shielding technology incorporates immunologically inert polymers that mask viral capsids from neutralizing antibodies and reduce innate immune activation[2]. BMS has pioneered targeted delivery systems that minimize systemic exposure and associated immune reactions. Their platform includes companion diagnostics for pre-screening patients for pre-existing immunity to viral vectors, allowing for personalized immunomodulation strategies[3]. The company has integrated these approaches with their established cell therapy expertise to develop hybrid gene-modified cell therapies that bypass many traditional immunological barriers. Recent clinical trials have demonstrated significantly improved transgene expression duration through their immune tolerance induction protocols.
Strengths: Robust integration with existing immunotherapy expertise; comprehensive approach combining vector modification with immunomodulation; strong clinical development pipeline. Weaknesses: Complex manufacturing requirements; potential for immunosuppression-related adverse events; higher cost compared to conventional gene therapy approaches.
Critical Immunological Mechanisms Affecting Vector Efficacy
Methods and compositions for reducing gene or nucleic acid therapy-related immune responses
PatentWO2021030312A1
Innovation
- The use of protein kinase inhibitors, such as tyrosine kinase inhibitors, in conjunction with therapeutic nucleic acids and carriers like lipid nanoparticles, to attenuate immune responses, thereby reducing proinflammatory immune reactions and enhancing the efficacy of gene therapy.
Gene-regulating compositions and methods for improved immunotherapy
PatentActiveUS20210071140A1
Innovation
- Modified immune effector cells with reduced expression or function of specific endogenous target genes, such as BCL2L11, FLI1, and SOCS1, using gene-regulating systems like siRNA, shRNA, or CRISPR-Cas proteins to enhance proliferation, infiltration, persistence, and resistance to exhaustion, thereby improving anti-tumor effects.
Regulatory Framework for Immune-Related Gene Therapy Safety
The regulatory landscape for gene therapies with immunological components has evolved significantly over the past decade, reflecting growing understanding of immune-related safety concerns. Regulatory bodies worldwide, including the FDA, EMA, and NMPA, have established specialized frameworks to address the unique challenges posed by immune responses in gene therapy applications. These frameworks typically encompass pre-clinical immune toxicity assessments, immunogenicity monitoring protocols, and post-approval surveillance requirements.
The FDA's guidance on cellular and gene therapy products specifically addresses immune-related considerations through its phased clinical trial approach, requiring robust immunological safety data before advancing to later-stage trials. Similarly, the EMA has implemented the Advanced Therapy Medicinal Products (ATMP) regulation, which includes specific provisions for immune monitoring and management strategies in gene therapy applications.
Risk assessment methodologies have become increasingly sophisticated, with regulatory agencies now requiring comprehensive immune response characterization during pre-clinical development. This includes evaluation of both innate and adaptive immune responses to vector components, transgene products, and delivery systems. Standardized reporting of immunological adverse events has been formalized through initiatives like the Immune-Related Adverse Events (irAE) classification system.
Regulatory harmonization efforts are underway through the International Council for Harmonisation (ICH), which is developing specific guidelines for immunological assessment in gene therapies. The proposed ICH S12 guideline specifically addresses biodistribution studies and immunogenicity assessments for gene therapy products, aiming to standardize approaches across jurisdictions.
Patient-specific factors have gained regulatory recognition, with agencies now requiring stratification strategies based on pre-existing immunity profiles. This includes screening for neutralizing antibodies against viral vectors and consideration of HLA types that might predispose to adverse immune responses. Regulatory frameworks increasingly emphasize personalized risk assessment approaches rather than one-size-fits-all safety standards.
Accelerated approval pathways have been established for gene therapies addressing serious conditions, though these come with enhanced post-marketing immune safety monitoring requirements. The FDA's Regenerative Medicine Advanced Therapy (RMAT) designation and the EMA's PRIME scheme both incorporate specific provisions for immune-related safety monitoring throughout the product lifecycle.
Recent regulatory trends indicate movement toward adaptive licensing approaches that allow for controlled market entry with ongoing immune safety assessment. This reflects recognition that some immune-related risks may only become apparent with broader patient exposure and longer follow-up periods. Regulatory agencies are increasingly employing real-world evidence and patient registries to complement traditional clinical trial data in safety evaluations.
The FDA's guidance on cellular and gene therapy products specifically addresses immune-related considerations through its phased clinical trial approach, requiring robust immunological safety data before advancing to later-stage trials. Similarly, the EMA has implemented the Advanced Therapy Medicinal Products (ATMP) regulation, which includes specific provisions for immune monitoring and management strategies in gene therapy applications.
Risk assessment methodologies have become increasingly sophisticated, with regulatory agencies now requiring comprehensive immune response characterization during pre-clinical development. This includes evaluation of both innate and adaptive immune responses to vector components, transgene products, and delivery systems. Standardized reporting of immunological adverse events has been formalized through initiatives like the Immune-Related Adverse Events (irAE) classification system.
Regulatory harmonization efforts are underway through the International Council for Harmonisation (ICH), which is developing specific guidelines for immunological assessment in gene therapies. The proposed ICH S12 guideline specifically addresses biodistribution studies and immunogenicity assessments for gene therapy products, aiming to standardize approaches across jurisdictions.
Patient-specific factors have gained regulatory recognition, with agencies now requiring stratification strategies based on pre-existing immunity profiles. This includes screening for neutralizing antibodies against viral vectors and consideration of HLA types that might predispose to adverse immune responses. Regulatory frameworks increasingly emphasize personalized risk assessment approaches rather than one-size-fits-all safety standards.
Accelerated approval pathways have been established for gene therapies addressing serious conditions, though these come with enhanced post-marketing immune safety monitoring requirements. The FDA's Regenerative Medicine Advanced Therapy (RMAT) designation and the EMA's PRIME scheme both incorporate specific provisions for immune-related safety monitoring throughout the product lifecycle.
Recent regulatory trends indicate movement toward adaptive licensing approaches that allow for controlled market entry with ongoing immune safety assessment. This reflects recognition that some immune-related risks may only become apparent with broader patient exposure and longer follow-up periods. Regulatory agencies are increasingly employing real-world evidence and patient registries to complement traditional clinical trial data in safety evaluations.
Personalized Immunoprofiling for Gene Therapy Success
Personalized immunoprofiling represents a revolutionary approach to enhancing gene therapy outcomes by tailoring treatments to individual immune characteristics. The immune system's response to gene therapy vectors remains one of the most significant barriers to successful treatment, with adverse reactions ranging from mild inflammation to life-threatening cytokine storms. By comprehensively analyzing a patient's immunological profile before treatment, clinicians can significantly improve safety profiles and treatment efficacy.
Current immunoprofiling technologies include high-throughput sequencing of T-cell and B-cell receptors, cytokine profiling, HLA typing, and assessment of pre-existing antibodies against viral vectors. These techniques collectively provide a multidimensional view of a patient's immune landscape, enabling the identification of potential barriers to successful gene therapy implementation.
The integration of machine learning algorithms with immunological data has emerged as a powerful tool for predicting individual responses to gene therapy vectors. These computational approaches can identify subtle patterns in immune markers that correlate with treatment outcomes, allowing for more precise patient stratification and personalized vector selection or modification.
Vector customization based on immunoprofiling data represents a significant advancement in personalized gene therapy. This approach involves modifying viral capsids or envelope proteins to evade specific immune responses identified in individual patients. Several biotechnology companies have developed platforms for rapid vector engineering based on immunological data, potentially reducing immunogenicity while maintaining transduction efficiency.
Immunomodulation strategies tailored to individual immune profiles are increasingly being incorporated into gene therapy protocols. These may include transient immunosuppression regimens, targeted depletion of specific immune cell populations, or administration of anti-inflammatory agents precisely timed according to the patient's immunological characteristics.
Clinical evidence supporting personalized immunoprofiling is accumulating rapidly. Recent trials incorporating pre-treatment immune assessment have demonstrated reduced incidence of adverse events and improved transgene expression compared to standard approaches. For instance, studies in hemophilia gene therapy have shown that patients selected based on favorable immune profiles maintain therapeutic protein levels significantly longer than unselected cohorts.
The economic implications of immunoprofiling must be considered alongside clinical benefits. While comprehensive immune assessment adds cost to already expensive gene therapies, this investment may be justified by improved outcomes, reduced complications, and decreased need for repeated treatments. Cost-effectiveness models suggest that targeted therapy based on immune profiling could ultimately reduce overall healthcare expenditures associated with gene therapy programs.
Current immunoprofiling technologies include high-throughput sequencing of T-cell and B-cell receptors, cytokine profiling, HLA typing, and assessment of pre-existing antibodies against viral vectors. These techniques collectively provide a multidimensional view of a patient's immune landscape, enabling the identification of potential barriers to successful gene therapy implementation.
The integration of machine learning algorithms with immunological data has emerged as a powerful tool for predicting individual responses to gene therapy vectors. These computational approaches can identify subtle patterns in immune markers that correlate with treatment outcomes, allowing for more precise patient stratification and personalized vector selection or modification.
Vector customization based on immunoprofiling data represents a significant advancement in personalized gene therapy. This approach involves modifying viral capsids or envelope proteins to evade specific immune responses identified in individual patients. Several biotechnology companies have developed platforms for rapid vector engineering based on immunological data, potentially reducing immunogenicity while maintaining transduction efficiency.
Immunomodulation strategies tailored to individual immune profiles are increasingly being incorporated into gene therapy protocols. These may include transient immunosuppression regimens, targeted depletion of specific immune cell populations, or administration of anti-inflammatory agents precisely timed according to the patient's immunological characteristics.
Clinical evidence supporting personalized immunoprofiling is accumulating rapidly. Recent trials incorporating pre-treatment immune assessment have demonstrated reduced incidence of adverse events and improved transgene expression compared to standard approaches. For instance, studies in hemophilia gene therapy have shown that patients selected based on favorable immune profiles maintain therapeutic protein levels significantly longer than unselected cohorts.
The economic implications of immunoprofiling must be considered alongside clinical benefits. While comprehensive immune assessment adds cost to already expensive gene therapies, this investment may be justified by improved outcomes, reduced complications, and decreased need for repeated treatments. Cost-effectiveness models suggest that targeted therapy based on immune profiling could ultimately reduce overall healthcare expenditures associated with gene therapy programs.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!