Autoclave vs. Gamma Irradiation: Load Suitability Comparison
SEP 2, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Sterilization Technologies Background and Objectives
Sterilization has been a critical process in healthcare, pharmaceutical, and food industries for over a century, with significant technological advancements occurring particularly in the last 50 years. The evolution of sterilization technologies has been driven by the need for more efficient, cost-effective, and safer methods to eliminate microorganisms from medical devices, pharmaceuticals, and various other products. Among these technologies, autoclave (steam sterilization) and gamma irradiation have emerged as two predominant methods, each with distinct operational principles and applications.
Autoclave sterilization, developed in the late 19th century, utilizes pressurized steam to achieve high temperatures necessary for microbial inactivation. This method has become the gold standard in many healthcare settings due to its reliability, cost-effectiveness, and environmental friendliness. The technology has evolved from basic pressure cookers to sophisticated computer-controlled systems capable of precise parameter control and validation.
Gamma irradiation, by contrast, emerged as a commercial sterilization method in the 1950s, leveraging ionizing radiation from isotope sources (typically Cobalt-60) to disrupt microbial DNA. This technology gained prominence due to its ability to sterilize products in their final packaging and its effectiveness at ambient temperatures, making it suitable for heat-sensitive materials.
The global sterilization technology market is projected to reach approximately $12.5 billion by 2025, with healthcare applications representing the largest segment. Technological innovation in this field continues to focus on improving efficiency, reducing processing times, minimizing material compatibility issues, and enhancing safety profiles for operators and end-users.
The primary objective of this technical research report is to conduct a comprehensive comparison between autoclave and gamma irradiation sterilization methods specifically regarding their suitability for different load types. This analysis aims to provide evidence-based guidance for selecting the optimal sterilization method based on material properties, product configurations, throughput requirements, and economic considerations.
Additionally, this report seeks to identify emerging trends in sterilization technology that may influence future decision-making processes in various industries. By examining current limitations and potential innovations in both autoclave and gamma irradiation technologies, we aim to forecast how these methods might evolve to address existing challenges and accommodate new materials and product designs entering the market.
The findings from this research will serve as a strategic resource for stakeholders involved in sterilization technology selection, implementation, and development, ultimately contributing to improved product safety, operational efficiency, and regulatory compliance across multiple industries.
Autoclave sterilization, developed in the late 19th century, utilizes pressurized steam to achieve high temperatures necessary for microbial inactivation. This method has become the gold standard in many healthcare settings due to its reliability, cost-effectiveness, and environmental friendliness. The technology has evolved from basic pressure cookers to sophisticated computer-controlled systems capable of precise parameter control and validation.
Gamma irradiation, by contrast, emerged as a commercial sterilization method in the 1950s, leveraging ionizing radiation from isotope sources (typically Cobalt-60) to disrupt microbial DNA. This technology gained prominence due to its ability to sterilize products in their final packaging and its effectiveness at ambient temperatures, making it suitable for heat-sensitive materials.
The global sterilization technology market is projected to reach approximately $12.5 billion by 2025, with healthcare applications representing the largest segment. Technological innovation in this field continues to focus on improving efficiency, reducing processing times, minimizing material compatibility issues, and enhancing safety profiles for operators and end-users.
The primary objective of this technical research report is to conduct a comprehensive comparison between autoclave and gamma irradiation sterilization methods specifically regarding their suitability for different load types. This analysis aims to provide evidence-based guidance for selecting the optimal sterilization method based on material properties, product configurations, throughput requirements, and economic considerations.
Additionally, this report seeks to identify emerging trends in sterilization technology that may influence future decision-making processes in various industries. By examining current limitations and potential innovations in both autoclave and gamma irradiation technologies, we aim to forecast how these methods might evolve to address existing challenges and accommodate new materials and product designs entering the market.
The findings from this research will serve as a strategic resource for stakeholders involved in sterilization technology selection, implementation, and development, ultimately contributing to improved product safety, operational efficiency, and regulatory compliance across multiple industries.
Market Demand Analysis for Medical Device Sterilization
The medical device sterilization market is experiencing robust growth, driven by increasing surgical procedures, rising healthcare-associated infections, and stringent regulatory requirements for infection control. The global medical device sterilization market was valued at approximately $8.5 billion in 2022 and is projected to reach $13.1 billion by 2028, growing at a CAGR of 7.5% during the forecast period.
Autoclave sterilization and gamma irradiation represent two dominant sterilization methods, collectively accounting for over 60% of the global medical device sterilization market. Gamma irradiation holds approximately 40% market share due to its effectiveness for high-volume, pre-packaged medical devices, while autoclave sterilization commands roughly 25% of the market, primarily in hospital settings for heat-resistant instruments.
The demand for appropriate sterilization method selection based on load suitability is intensifying as medical devices become increasingly complex and incorporate diverse materials. Healthcare facilities are seeking optimized sterilization protocols that maintain device integrity while ensuring complete sterilization. This trend is particularly evident in the orthopedic and cardiovascular device segments, where material compatibility issues with sterilization methods can significantly impact product performance and lifespan.
Regional analysis reveals varying preferences, with North America and Europe showing increased adoption of gamma irradiation for industrial-scale sterilization, while autoclave sterilization remains predominant in hospital settings. Emerging markets in Asia-Pacific and Latin America are experiencing rapid growth in both methods, with a CAGR exceeding 9% in these regions.
The COVID-19 pandemic has substantially accelerated market demand, creating unprecedented pressure on sterilization capacity worldwide. This has prompted healthcare facilities to reassess their sterilization method selection criteria, with greater emphasis on throughput capacity and turnaround time alongside traditional considerations of material compatibility.
End-user segmentation indicates hospitals represent the largest market segment (45%), followed by medical device manufacturers (30%) and pharmaceutical companies (15%). The remaining 10% comprises contract sterilization services and research institutions. Each segment demonstrates distinct preferences regarding sterilization methods based on their specific operational requirements and device portfolios.
Future market growth will be significantly influenced by advancements in material science enabling broader compatibility across sterilization methods, as well as the development of hybrid sterilization technologies that optimize the benefits of multiple approaches while minimizing their limitations. Additionally, increasing regulatory scrutiny regarding sterilization residuals and environmental impact is expected to reshape market dynamics over the coming decade.
Autoclave sterilization and gamma irradiation represent two dominant sterilization methods, collectively accounting for over 60% of the global medical device sterilization market. Gamma irradiation holds approximately 40% market share due to its effectiveness for high-volume, pre-packaged medical devices, while autoclave sterilization commands roughly 25% of the market, primarily in hospital settings for heat-resistant instruments.
The demand for appropriate sterilization method selection based on load suitability is intensifying as medical devices become increasingly complex and incorporate diverse materials. Healthcare facilities are seeking optimized sterilization protocols that maintain device integrity while ensuring complete sterilization. This trend is particularly evident in the orthopedic and cardiovascular device segments, where material compatibility issues with sterilization methods can significantly impact product performance and lifespan.
Regional analysis reveals varying preferences, with North America and Europe showing increased adoption of gamma irradiation for industrial-scale sterilization, while autoclave sterilization remains predominant in hospital settings. Emerging markets in Asia-Pacific and Latin America are experiencing rapid growth in both methods, with a CAGR exceeding 9% in these regions.
The COVID-19 pandemic has substantially accelerated market demand, creating unprecedented pressure on sterilization capacity worldwide. This has prompted healthcare facilities to reassess their sterilization method selection criteria, with greater emphasis on throughput capacity and turnaround time alongside traditional considerations of material compatibility.
End-user segmentation indicates hospitals represent the largest market segment (45%), followed by medical device manufacturers (30%) and pharmaceutical companies (15%). The remaining 10% comprises contract sterilization services and research institutions. Each segment demonstrates distinct preferences regarding sterilization methods based on their specific operational requirements and device portfolios.
Future market growth will be significantly influenced by advancements in material science enabling broader compatibility across sterilization methods, as well as the development of hybrid sterilization technologies that optimize the benefits of multiple approaches while minimizing their limitations. Additionally, increasing regulatory scrutiny regarding sterilization residuals and environmental impact is expected to reshape market dynamics over the coming decade.
Current State and Challenges in Sterilization Methods
Sterilization methods have evolved significantly over the past century, with autoclave and gamma irradiation emerging as two predominant techniques in medical, pharmaceutical, and food industries. Currently, steam sterilization via autoclave represents approximately 50% of all sterilization processes globally, while radiation methods, including gamma irradiation, account for approximately 40% of the market share.
Autoclave sterilization utilizes saturated steam under pressure (typically 121°C at 15 psi) to eliminate microorganisms through protein denaturation. This method remains the gold standard for heat-stable items but faces significant limitations with heat-sensitive materials. Modern autoclaves have incorporated advanced monitoring systems, vacuum-assisted cycles, and improved chamber designs to enhance efficiency and reliability. However, challenges persist in achieving uniform heat distribution for complex loads and penetration into dense materials.
Gamma irradiation, utilizing cobalt-60 or cesium-137 sources, has gained prominence for its ability to sterilize products in their final packaging and process heat-sensitive materials. The technology operates by emitting high-energy photons that disrupt microbial DNA. Current industrial facilities can process large volumes efficiently, with dose rates typically ranging from 15 to 25 kGy for medical devices. The non-thermal nature of this process presents distinct advantages for temperature-sensitive items.
A significant challenge facing both methods is the increasing complexity of modern medical devices and pharmaceutical products. Multi-material assemblies, intricate geometries, and novel biomaterials often require specialized validation protocols that exceed traditional sterilization parameters. Additionally, regulatory frameworks have become more stringent, with the FDA and European regulatory bodies implementing more comprehensive requirements for sterilization validation and monitoring.
Material compatibility represents another critical challenge. Polymers commonly used in medical devices may undergo degradation during sterilization, with gamma irradiation potentially causing chain scission or cross-linking, while autoclave processes can lead to hydrolysis or dimensional changes. Recent studies indicate that approximately 30% of new medical device materials exhibit some form of incompatibility with standard sterilization protocols.
Environmental and safety concerns have also emerged as significant challenges. Gamma irradiation facilities require extensive safety measures due to radiation hazards, while autoclaves consume substantial energy and water resources. The industry is actively seeking more sustainable alternatives, with reduced cycle times and improved energy efficiency becoming key development priorities.
Supply chain considerations further complicate sterilization method selection, as centralized gamma irradiation facilities may introduce logistical challenges compared to on-site autoclave capabilities. This geographical distribution of sterilization technologies has created regional disparities in access to appropriate sterilization methods for different product categories.
Autoclave sterilization utilizes saturated steam under pressure (typically 121°C at 15 psi) to eliminate microorganisms through protein denaturation. This method remains the gold standard for heat-stable items but faces significant limitations with heat-sensitive materials. Modern autoclaves have incorporated advanced monitoring systems, vacuum-assisted cycles, and improved chamber designs to enhance efficiency and reliability. However, challenges persist in achieving uniform heat distribution for complex loads and penetration into dense materials.
Gamma irradiation, utilizing cobalt-60 or cesium-137 sources, has gained prominence for its ability to sterilize products in their final packaging and process heat-sensitive materials. The technology operates by emitting high-energy photons that disrupt microbial DNA. Current industrial facilities can process large volumes efficiently, with dose rates typically ranging from 15 to 25 kGy for medical devices. The non-thermal nature of this process presents distinct advantages for temperature-sensitive items.
A significant challenge facing both methods is the increasing complexity of modern medical devices and pharmaceutical products. Multi-material assemblies, intricate geometries, and novel biomaterials often require specialized validation protocols that exceed traditional sterilization parameters. Additionally, regulatory frameworks have become more stringent, with the FDA and European regulatory bodies implementing more comprehensive requirements for sterilization validation and monitoring.
Material compatibility represents another critical challenge. Polymers commonly used in medical devices may undergo degradation during sterilization, with gamma irradiation potentially causing chain scission or cross-linking, while autoclave processes can lead to hydrolysis or dimensional changes. Recent studies indicate that approximately 30% of new medical device materials exhibit some form of incompatibility with standard sterilization protocols.
Environmental and safety concerns have also emerged as significant challenges. Gamma irradiation facilities require extensive safety measures due to radiation hazards, while autoclaves consume substantial energy and water resources. The industry is actively seeking more sustainable alternatives, with reduced cycle times and improved energy efficiency becoming key development priorities.
Supply chain considerations further complicate sterilization method selection, as centralized gamma irradiation facilities may introduce logistical challenges compared to on-site autoclave capabilities. This geographical distribution of sterilization technologies has created regional disparities in access to appropriate sterilization methods for different product categories.
Technical Comparison of Autoclave and Gamma Irradiation Methods
01 Autoclave sterilization for medical devices and materials
Autoclave sterilization uses high-pressure steam to eliminate microorganisms from medical devices and materials. This method is particularly suitable for heat-resistant items such as surgical instruments, laboratory equipment, and certain types of packaging. The process typically involves temperatures of 121-134°C under pressure for specific time periods to ensure complete sterilization. The suitability of items for autoclave sterilization depends on their heat resistance, moisture tolerance, and material composition.- Autoclave sterilization for medical devices and materials: Autoclave sterilization uses high-pressure steam to eliminate microorganisms from medical devices and materials. This method is particularly suitable for heat-resistant items such as surgical instruments, laboratory equipment, and certain types of packaging. The process typically involves temperatures of 121-134°C under pressure for specific time periods to ensure complete sterilization. The suitability of items for autoclave sterilization depends on their heat and moisture tolerance, with considerations for material integrity after repeated sterilization cycles.
- Gamma irradiation for heat-sensitive materials: Gamma irradiation is a sterilization method particularly suitable for heat-sensitive materials that cannot withstand autoclave temperatures. This method uses ionizing radiation from sources like Cobalt-60 to destroy microorganisms by damaging their DNA. It's effective for sterilizing pharmaceuticals, medical devices, polymers, and biological tissues. The process can be performed on pre-packaged products, eliminating the risk of post-sterilization contamination. Load suitability depends on material radiation resistance, with consideration for potential degradation effects on certain polymers and active ingredients.
- Material compatibility and validation methods: Determining sterilization load suitability requires comprehensive material compatibility testing and validation protocols. Different materials respond uniquely to sterilization methods - some polymers may degrade under gamma radiation while others cannot withstand autoclave temperatures. Validation methods include bioburden testing, sterility assurance level (SAL) determination, and material integrity assessments before and after sterilization. Proper validation ensures that the chosen sterilization method effectively eliminates microorganisms while maintaining the functional and structural properties of the sterilized items.
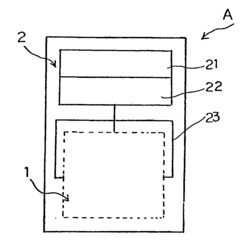
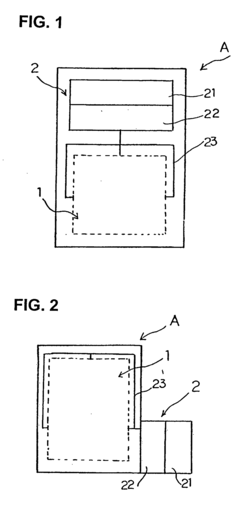
- Specialized sterilization equipment and load configurations: Specialized equipment and optimized load configurations enhance sterilization effectiveness for both autoclave and gamma irradiation methods. For autoclaves, this includes pre-vacuum systems, pulsed steam injection, and load-specific chamber designs. For gamma irradiation, specialized conveyor systems, radiation shielding, and precise dosimetry equipment ensure uniform exposure. Proper load configuration is critical - items must be arranged to allow steam penetration in autoclaves or radiation exposure in gamma chambers. Monitoring systems track critical parameters like temperature, pressure, time, and radiation dose to ensure sterilization efficacy.
- Combination and novel sterilization approaches: Innovative approaches combine multiple sterilization methods or introduce novel techniques to overcome limitations of traditional methods. These include sequential processing with both gamma irradiation and autoclave sterilization for challenging materials, low-temperature steam formaldehyde processes for heat-sensitive items, and radiation-activated sterilants. Other advancements include pulsed light systems, supercritical CO2 sterilization, and plasma-based methods. These combination and novel approaches expand the range of materials suitable for effective sterilization while preserving material integrity and functionality.
02 Gamma irradiation for heat-sensitive products
Gamma irradiation is a sterilization method particularly suitable for heat-sensitive products that cannot withstand autoclave temperatures. This method uses ionizing radiation from sources like Cobalt-60 to destroy microorganisms by damaging their DNA. It's effective for sterilizing pharmaceuticals, medical devices, polymers, and biological materials. The process can be performed at room temperature without significant heat generation, making it ideal for thermolabile materials. However, certain materials may experience degradation or color changes due to radiation exposure.Expand Specific Solutions03 Material compatibility and load configuration
The compatibility of materials with sterilization methods is crucial for maintaining product integrity. Different materials respond differently to autoclave and gamma irradiation. For autoclave, heat-resistant materials like stainless steel, glass, and certain plastics are suitable, while heat-sensitive materials may deform or degrade. For gamma irradiation, radiation-resistant materials are preferred, as some polymers may experience cross-linking or chain scission. Load configuration also affects sterilization efficacy, with proper spacing needed to ensure steam penetration in autoclaves or uniform radiation exposure in gamma sterilization.Expand Specific Solutions04 Validation and monitoring of sterilization processes
Validation and monitoring are essential to ensure the effectiveness of both autoclave and gamma irradiation sterilization processes. This involves establishing parameters such as temperature, pressure, and exposure time for autoclaves, or radiation dose for gamma irradiation. Biological indicators containing resistant microorganisms are used to verify sterilization efficacy. Physical monitors like thermocouples, pressure gauges, and dosimeters provide real-time data during the process. Regular validation ensures consistent sterilization results and helps identify potential issues with load suitability or process parameters.Expand Specific Solutions05 Innovative approaches to enhance sterilization efficiency
Recent innovations aim to enhance the efficiency and applicability of autoclave and gamma irradiation sterilization methods. These include the development of specialized packaging materials that maintain sterility while allowing effective sterilization, combination sterilization approaches that leverage the benefits of multiple methods, and advanced monitoring systems that provide more accurate data on sterilization parameters. Other innovations focus on reducing sterilization cycle times, minimizing material degradation, and expanding the range of materials suitable for each sterilization method.Expand Specific Solutions
Key Industry Players in Sterilization Equipment and Services
The sterilization technology market for "Autoclave vs. Gamma Irradiation" is in a mature growth phase, with an estimated global market size exceeding $2.5 billion. Autoclave technology, represented by companies like Jiangyin Binjiang Medical Equipment and B. Braun Melsungen, offers cost-effective solutions for heat-resistant materials but faces limitations with heat-sensitive items. Conversely, gamma irradiation, championed by Becton Dickinson and Curium US LLC, provides superior penetration for complex medical devices and pharmaceuticals without temperature concerns. The competitive landscape shows established medical technology leaders like Olympus and Elekta advancing hybrid solutions, while specialized players like ACIST Medical Systems focus on niche applications requiring specific load compatibility characteristics, driving innovation in material-specific sterilization protocols.
Becton, Dickinson & Co.
Technical Solution: Becton, Dickinson & Co. (BD) has developed a comprehensive sterilization approach that strategically utilizes both autoclave and gamma irradiation technologies based on load characteristics. For temperature-sensitive medical devices, BD employs gamma irradiation at doses between 25-40 kGy, which effectively penetrates sealed packaging and eliminates microorganisms without generating heat. Their proprietary dose mapping technology ensures uniform radiation exposure across complex product geometries. For reusable surgical instruments and laboratory equipment, BD implements validated autoclave protocols using saturated steam at 121-134°C with precise pressure cycling to achieve sterility assurance levels (SAL) of 10^-6. BD has also pioneered hybrid sterilization approaches for certain composite devices, where components undergo separate sterilization processes before final assembly, maximizing material compatibility while maintaining product integrity.
Strengths: BD's dual-technology approach provides flexibility to match sterilization method with specific material requirements. Their extensive validation protocols ensure consistent sterility across diverse product lines. Weaknesses: The company's gamma irradiation facilities require significant capital investment and specialized safety infrastructure, while autoclave processes can be more energy-intensive and time-consuming for large-volume production.
Curium US LLC
Technical Solution: Curium US LLC has developed specialized load suitability assessment protocols for comparing autoclave and gamma irradiation sterilization methods across their radiopharmaceutical product line. Their approach centers on a proprietary Material Compatibility Matrix that categorizes products based on thermal sensitivity, moisture tolerance, and radiation stability. For temperature-sensitive radiopharmaceuticals, Curium employs gamma irradiation at controlled doses (typically 15-25 kGy) with advanced dosimetry systems that ensure uniform radiation distribution while preserving product efficacy. Their gamma facilities feature automated conveyor systems with precise dose mapping capabilities to accommodate varying product densities. For equipment and components that can withstand high temperatures, Curium implements validated autoclave cycles with saturated steam at 121-134°C, utilizing pre-vacuum phases to enhance steam penetration into complex geometries. Their sterilization validation protocols include comprehensive bioburden testing, sterility verification, and post-sterilization stability assessments to ensure both methods achieve the required sterility assurance level (SAL) of 10^-6.
Strengths: Curium's dual-technology approach provides exceptional flexibility for their diverse product portfolio, with specialized expertise in radiopharmaceutical sterilization requirements. Their comprehensive validation protocols ensure consistent sterility while maintaining product efficacy. Weaknesses: Their gamma irradiation facilities require significant capital investment and specialized safety infrastructure, while autoclave processes can introduce moisture that may affect certain product formulations and packaging integrity.
Critical Parameters Affecting Load Suitability in Sterilization
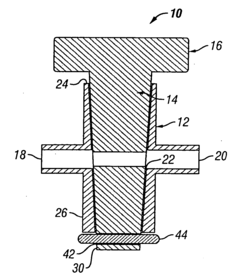
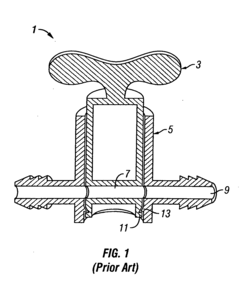
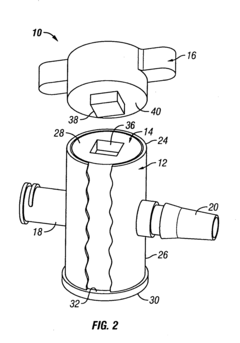
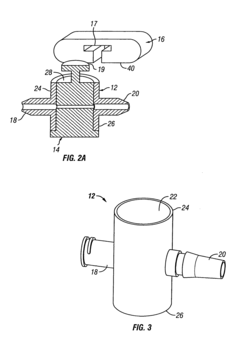
Stopcocks and methods of manufacture thereof
PatentInactiveUS20050035324A1
Innovation
- A stopcock constructed entirely of gamma radiation-stable materials like polyetheretherketone (PEEK) and polycarbonate, with a secure attachment method and a grip for ease of operation, allowing for a watertight fit and compatibility with high pressures, and optionally using non-gamma-stable materials for cost-effectiveness and design flexibility.
Sterilization apparatus using sterilizing superheated steam under normal pressure and hypoxia environment
PatentInactiveUS20070212282A1
Innovation
- A sterilization apparatus using superheated steam generated by colliding saturated steam with a heated medium at 120 to 150°C under normal pressure, creating a low-oxygen environment, which effectively kills microorganisms, bacteria, and viruses on medical treatment tools.
Material Compatibility and Degradation Considerations
Material compatibility is a critical factor when selecting between autoclave and gamma irradiation sterilization methods. Different materials respond uniquely to each process, with potential degradation effects that must be carefully considered. Polymers, particularly thermoplastics, often exhibit significant differences in performance post-sterilization. Polypropylene, for instance, maintains structural integrity well under autoclave conditions but may experience chain scission and embrittlement when exposed to gamma radiation above certain dosage thresholds.
Metals and alloys generally demonstrate excellent resistance to both sterilization methods, though some specialized alloys may experience surface oxidation during repeated autoclave cycles. Stainless steel, titanium, and aluminum remain largely unaffected by either process, making them versatile choices for reusable medical devices and equipment.
Glass and ceramic materials typically withstand both sterilization methods effectively, though thermal shock during autoclave cycling can potentially compromise structural integrity of certain glass formulations. Gamma irradiation presents minimal risk to these materials, offering an advantage for delicate glass components.
Composite materials present unique challenges, as the differential response of constituent materials may lead to delamination or interface weakening. Autoclave processes, with their combination of heat, pressure, and moisture, can accelerate these degradation mechanisms in poorly designed composites. Gamma irradiation may induce cross-linking or chain scission in the polymer matrix of composites, potentially altering mechanical properties.
Elastomers and rubbers demonstrate varying compatibility profiles. Silicone rubbers generally maintain properties well under both sterilization methods, while natural rubber may experience accelerated aging with gamma exposure. Autoclave sterilization can cause swelling and dimensional changes in certain elastomers, potentially compromising sealing applications.
Adhesives and bonded interfaces represent particular vulnerability points in multi-material assemblies. Heat and moisture from autoclaving may weaken adhesive bonds, while gamma radiation can either strengthen bonds through additional cross-linking or degrade them through polymer chain breakage, depending on the specific chemistry involved.
Colorants, additives, and surface treatments may also experience degradation, with potential for color shifting, blooming of additives, or surface property alterations. Gamma irradiation typically causes more pronounced color changes in many polymer systems compared to autoclave processing, which must be considered for aesthetically critical applications.
Metals and alloys generally demonstrate excellent resistance to both sterilization methods, though some specialized alloys may experience surface oxidation during repeated autoclave cycles. Stainless steel, titanium, and aluminum remain largely unaffected by either process, making them versatile choices for reusable medical devices and equipment.
Glass and ceramic materials typically withstand both sterilization methods effectively, though thermal shock during autoclave cycling can potentially compromise structural integrity of certain glass formulations. Gamma irradiation presents minimal risk to these materials, offering an advantage for delicate glass components.
Composite materials present unique challenges, as the differential response of constituent materials may lead to delamination or interface weakening. Autoclave processes, with their combination of heat, pressure, and moisture, can accelerate these degradation mechanisms in poorly designed composites. Gamma irradiation may induce cross-linking or chain scission in the polymer matrix of composites, potentially altering mechanical properties.
Elastomers and rubbers demonstrate varying compatibility profiles. Silicone rubbers generally maintain properties well under both sterilization methods, while natural rubber may experience accelerated aging with gamma exposure. Autoclave sterilization can cause swelling and dimensional changes in certain elastomers, potentially compromising sealing applications.
Adhesives and bonded interfaces represent particular vulnerability points in multi-material assemblies. Heat and moisture from autoclaving may weaken adhesive bonds, while gamma radiation can either strengthen bonds through additional cross-linking or degrade them through polymer chain breakage, depending on the specific chemistry involved.
Colorants, additives, and surface treatments may also experience degradation, with potential for color shifting, blooming of additives, or surface property alterations. Gamma irradiation typically causes more pronounced color changes in many polymer systems compared to autoclave processing, which must be considered for aesthetically critical applications.
Environmental Impact and Sustainability of Sterilization Methods
The environmental impact of sterilization methods has become increasingly important as healthcare facilities and manufacturers seek to reduce their ecological footprint. Autoclave sterilization and gamma irradiation present distinctly different environmental profiles that must be considered alongside their technical capabilities.
Autoclave sterilization primarily consumes water and electricity, with modern units requiring 40-60 gallons of water and 6-15 kWh of electricity per cycle. While this represents significant resource consumption, autoclaves benefit from using only utilities without requiring specialized consumables or generating hazardous waste. The environmental impact is largely determined by the source of electricity; facilities using renewable energy can substantially reduce their carbon footprint from autoclave operations.
In contrast, gamma irradiation facilities utilize radioactive isotopes (typically Cobalt-60) that require careful management throughout their lifecycle. The production, transportation, and eventual disposal of these isotopes present unique environmental challenges. However, gamma irradiation requires minimal water usage and operates continuously rather than in cycles, potentially offering greater energy efficiency for high-volume sterilization needs.
Waste generation differs significantly between these methods. Autoclaves produce non-hazardous wastewater that can typically enter standard treatment systems, though it may contain chemical indicators and biological residues. Gamma irradiation generates no direct waste during operation but requires specialized handling for spent radioactive sources at end-of-life, involving complex regulatory compliance and specialized disposal facilities.
From a sustainability perspective, autoclave technology has evolved toward greater efficiency, with newer models incorporating water reclamation systems that reduce consumption by up to 80%. Similarly, vacuum-assisted cycles have decreased energy requirements. These improvements have significantly enhanced the ecological profile of autoclave sterilization over the past decade.
Gamma irradiation facilities have focused sustainability efforts on extending source life and improving shielding technology to maximize utilization while minimizing replacement frequency. The long operational life of irradiation sources (typically 15-20 years) represents a sustainability advantage when amortized across the enormous volume of products processed during this period.
Carbon footprint assessments indicate that for small to medium loads, properly optimized autoclaves generally maintain a lower environmental impact. However, for industrial-scale sterilization of compatible materials, gamma irradiation's continuous processing capability and high throughput can result in lower per-unit environmental impact despite the challenges associated with radioactive materials management.
Autoclave sterilization primarily consumes water and electricity, with modern units requiring 40-60 gallons of water and 6-15 kWh of electricity per cycle. While this represents significant resource consumption, autoclaves benefit from using only utilities without requiring specialized consumables or generating hazardous waste. The environmental impact is largely determined by the source of electricity; facilities using renewable energy can substantially reduce their carbon footprint from autoclave operations.
In contrast, gamma irradiation facilities utilize radioactive isotopes (typically Cobalt-60) that require careful management throughout their lifecycle. The production, transportation, and eventual disposal of these isotopes present unique environmental challenges. However, gamma irradiation requires minimal water usage and operates continuously rather than in cycles, potentially offering greater energy efficiency for high-volume sterilization needs.
Waste generation differs significantly between these methods. Autoclaves produce non-hazardous wastewater that can typically enter standard treatment systems, though it may contain chemical indicators and biological residues. Gamma irradiation generates no direct waste during operation but requires specialized handling for spent radioactive sources at end-of-life, involving complex regulatory compliance and specialized disposal facilities.
From a sustainability perspective, autoclave technology has evolved toward greater efficiency, with newer models incorporating water reclamation systems that reduce consumption by up to 80%. Similarly, vacuum-assisted cycles have decreased energy requirements. These improvements have significantly enhanced the ecological profile of autoclave sterilization over the past decade.
Gamma irradiation facilities have focused sustainability efforts on extending source life and improving shielding technology to maximize utilization while minimizing replacement frequency. The long operational life of irradiation sources (typically 15-20 years) represents a sustainability advantage when amortized across the enormous volume of products processed during this period.
Carbon footprint assessments indicate that for small to medium loads, properly optimized autoclaves generally maintain a lower environmental impact. However, for industrial-scale sterilization of compatible materials, gamma irradiation's continuous processing capability and high throughput can result in lower per-unit environmental impact despite the challenges associated with radioactive materials management.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!