Systems, assemblies, and methods for treating a bronchial tree
a technology of bronchial tree and system, applied in the field of systems, assemblies, and methods for treating bronchial tree, can solve the problems of adverse effects on the size of the population, adverse effects on the performance of the lungs, health-related costs, etc., and achieve the effect of increasing the resistance to airflow in the lungs
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
In the following description, certain specific details are set forth in order to provide a thorough understanding of various embodiments of the invention. However, one skilled in the art will understand that the invention may be practiced without these details. In other instances, well-known structures associated with catheter systems, delivery assemblies, activatable elements, circuitry, and electrodes have not been described in detail to avoid unnecessarily obscuring descriptions of the embodiments of the invention.
Unless the context requires otherwise, throughout the specification and claims which follow, the word “comprise” and variations thereof, such as “comprises” and “comprising” are to be construed in an open, inclusive sense, that is, as “including but not limited to.”
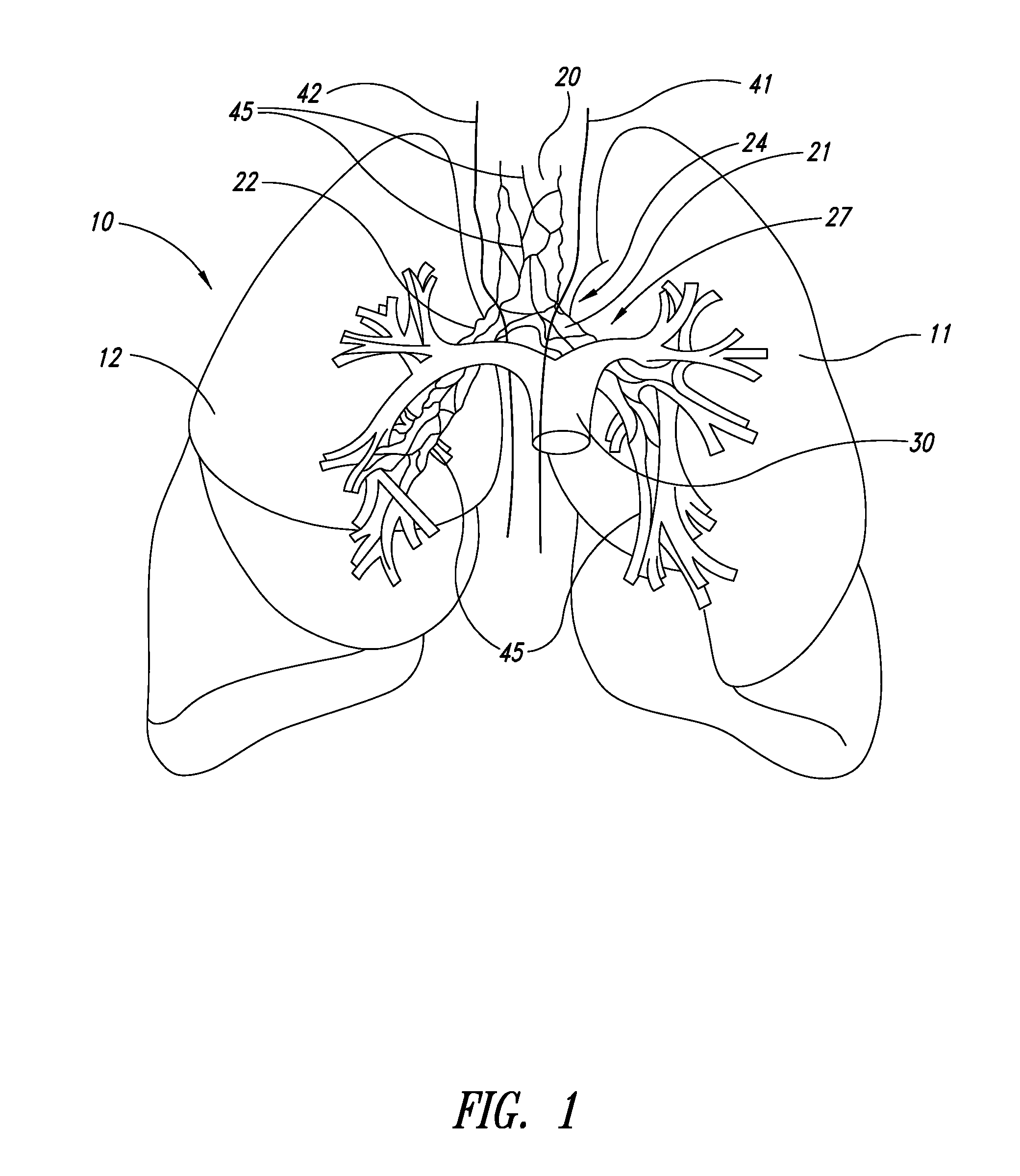
FIG. 1 illustrates human lungs 10 having a left lung 11 and a right lung 12. A trachea 20 extends downwardly from the nose and mouth and divides into a left main bronchus 21 and a right main bronchus 22. The ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com