Endovascular graft with pressure, temperature, flow and voltage sensors
a technology of endovascular grafts and sensors, which is applied in the field of body lumen treatment, can solve the problems of high morbidity and mortality rates of abdominal surgery, and the associated high rate of implantation of endovascular grafts, and achieve the effect of less cost and increasing the potential for diagnosis and treatmen
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
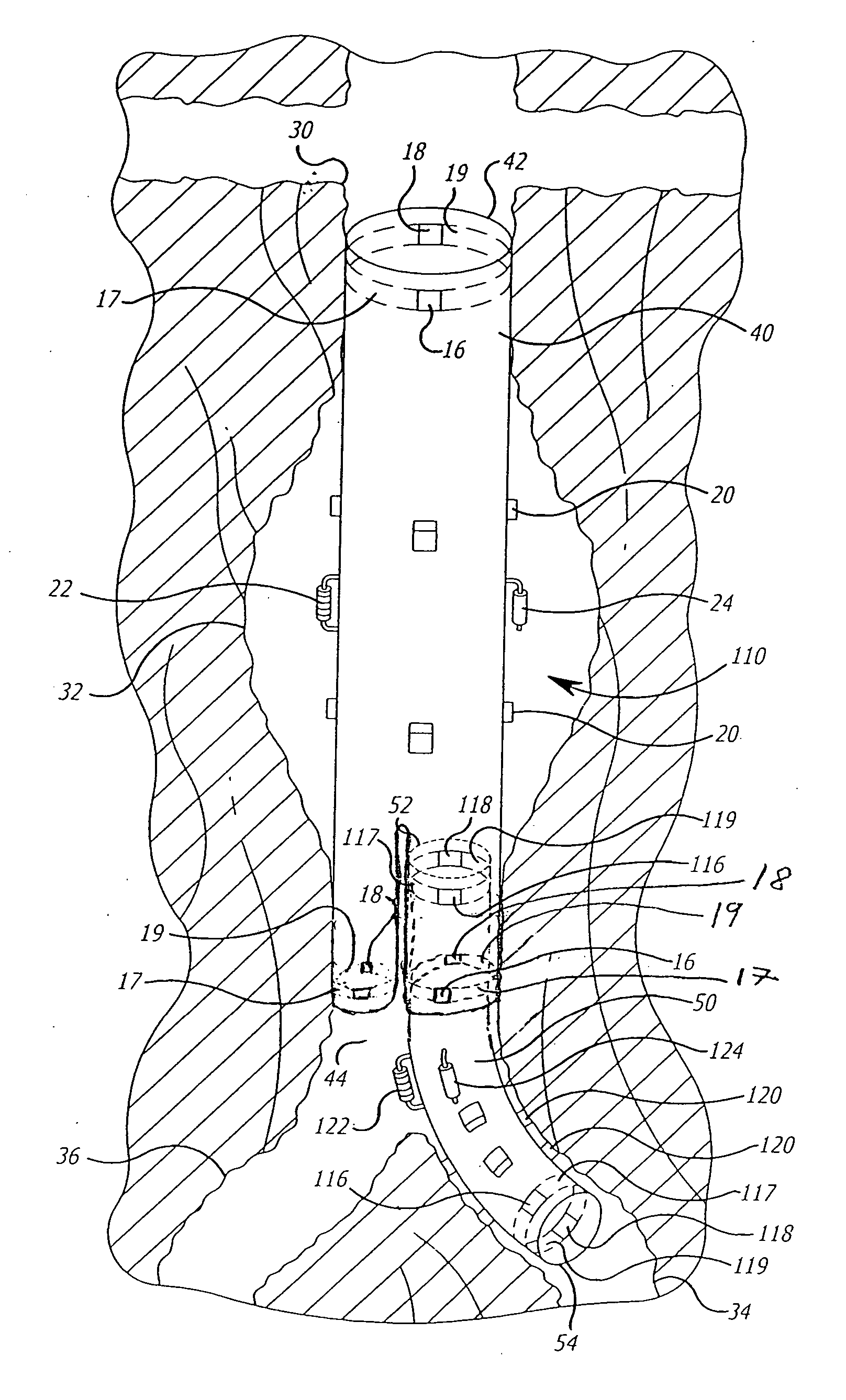
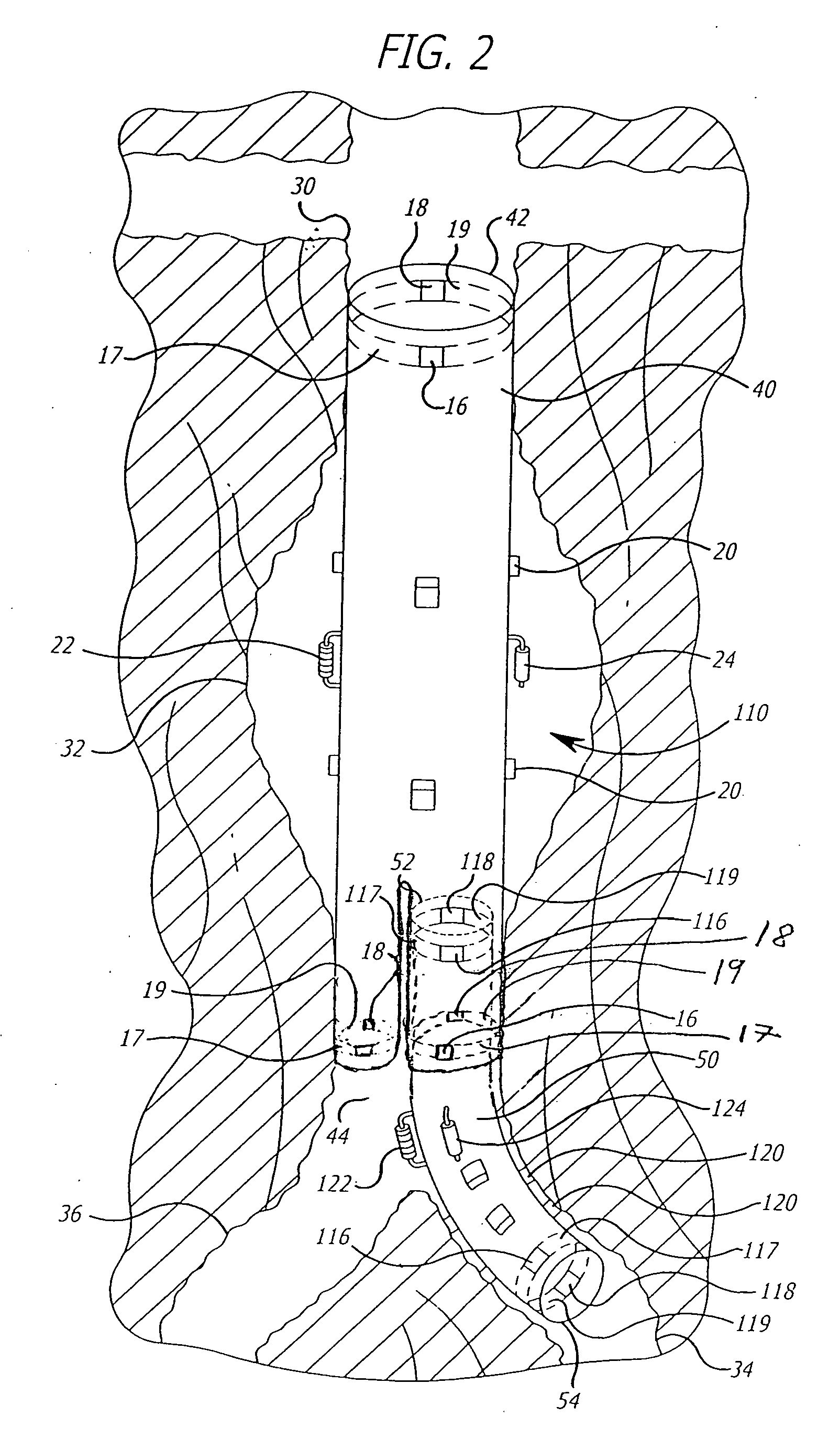
[0019] As shown in the exemplary drawings and for purposes of illustration, the invention is embodied in a prosthetic endovascular graft implant having the ability to measure pertinent parameters inside and outside the graft material and transmit the measurements to a receiver located external the patient within whom the endovascular graft is implanted. In one aspect, the invention includes a graft with sensors mounted on the external and internal surface that measure parameters such as pressure, temperature or voltage. In another aspect the invention includes a transmitter and energy source which facilitate transmission of parameters measured by the sensors to a receiver located outside the patient's body.
[0020] Referring to FIG. 1, an embodiment of the invention is shown in which a generally tubular, including flared or tapered, endovascular graft 10 having a superior end 12 and inferior end 14 is implanted in a body vessel 30 across an aneurysm sac 32 with the superior end 12 se...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com