Healthcare delivery system
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
[0043]The following detailed description is of the best currently contemplated modes of carrying out exemplary embodiments of the invention. The description is not to be taken in a limiting sense, but is made merely for the purpose of illustrating the general principles of the invention, since the scope of the invention is best defined by the appended claims.
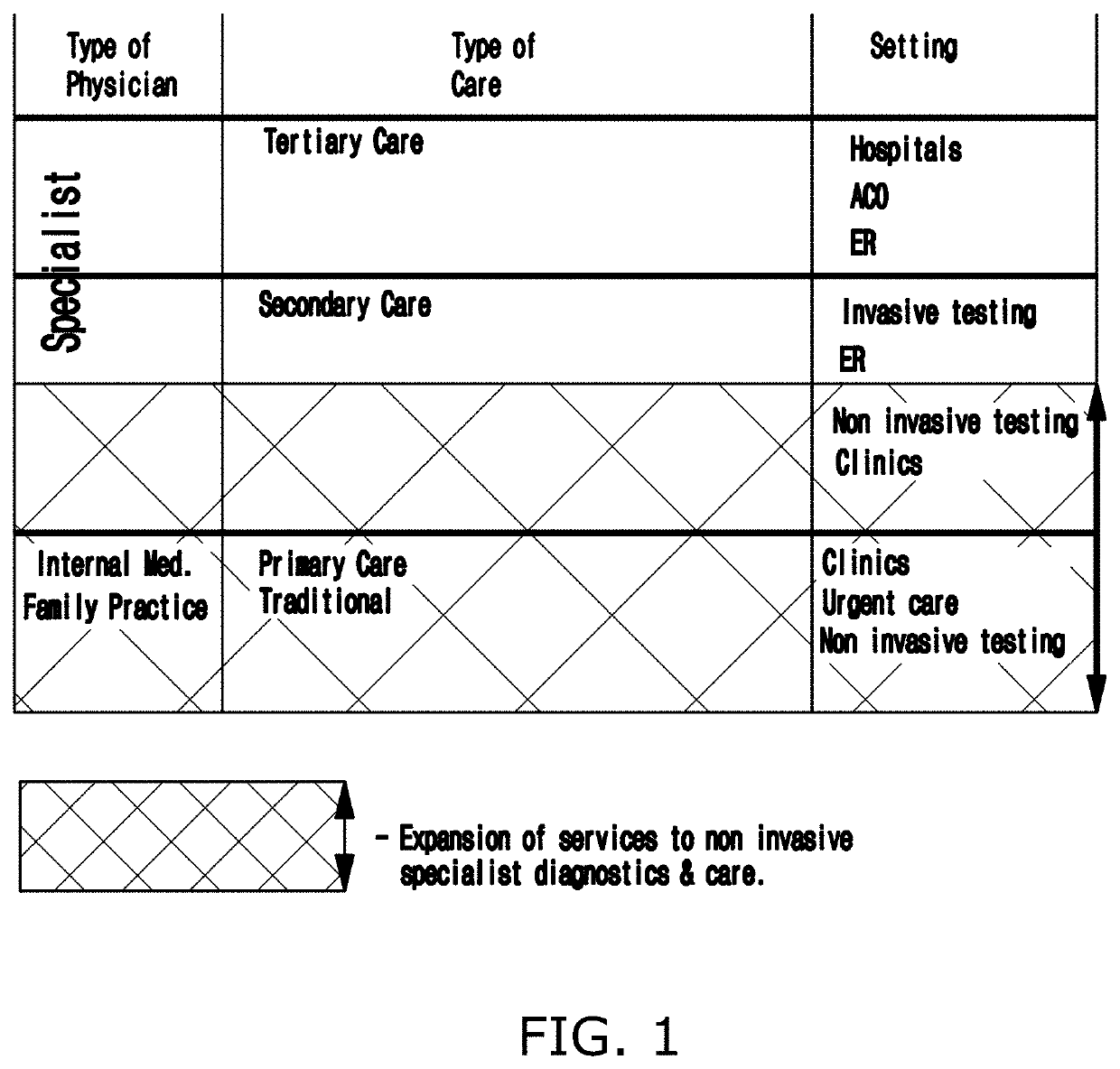
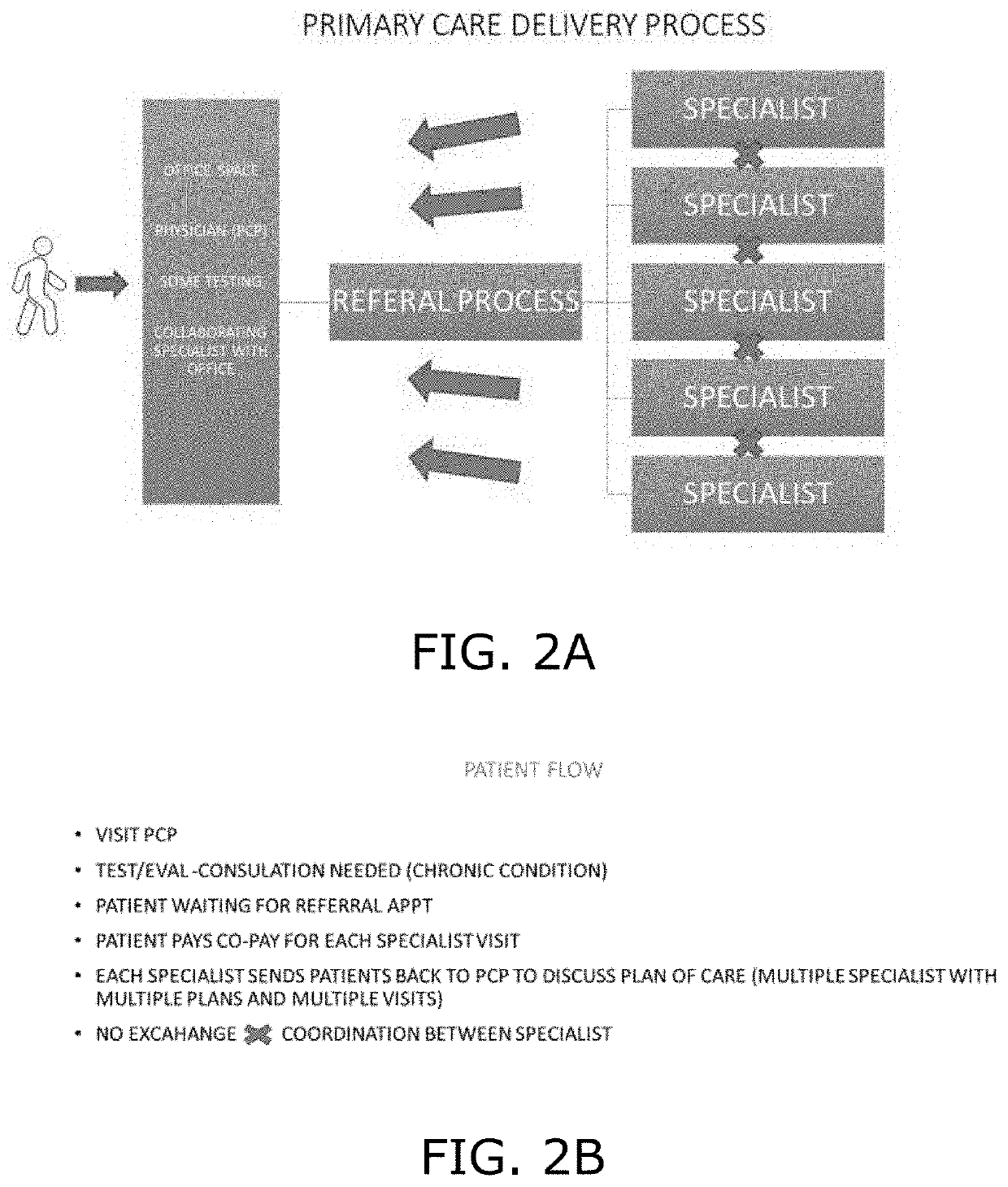
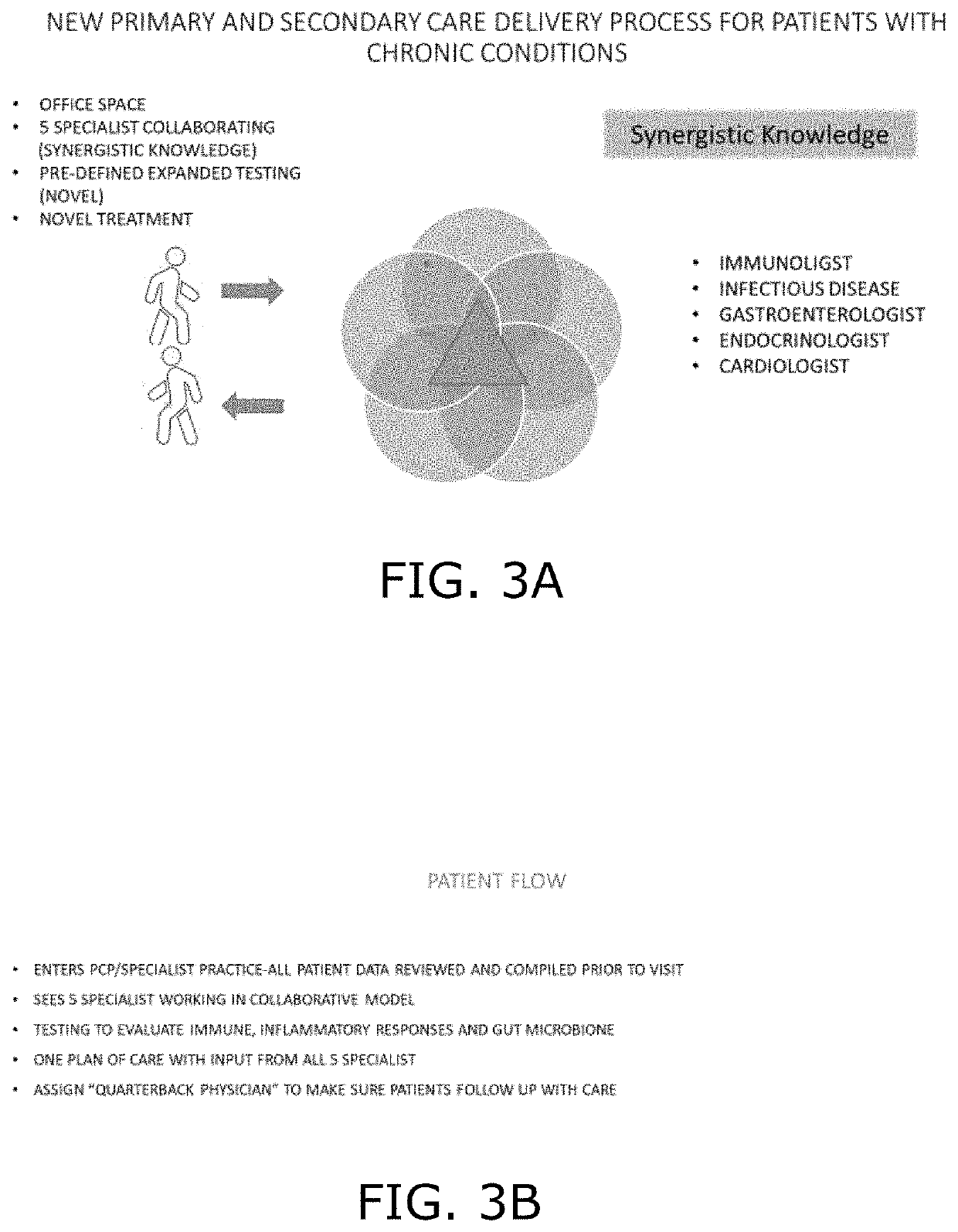
[0044]Broadly, an embodiment of the present invention provides a healthcare delivery system that embodies methods of empowering collaborative multidisciplinary healthcare for providing care to patients with chronic conditions.
[0045]Referring to FIGS. 3 through 5, the present invention may include use of at least one computer with a user interface. The computer may include at least one processing unit coupled to a form of memory. The computer may be any computing device including, but not limited to, desktops, laptops, and smart devices such as a tablet, smart watch, smart phone, and the like. The computer includes a program prod...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com