Oropharyngeal Airway
a technology of oropharyngeal airway and airway, which is applied in the direction of respiratory apparatus, medical devices, medical devices, etc., can solve the problems of irritation of the trachea, inconvenient administration of anesthesia via face mask technique, and difficulty in establishing and maintaining an airway of patients
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
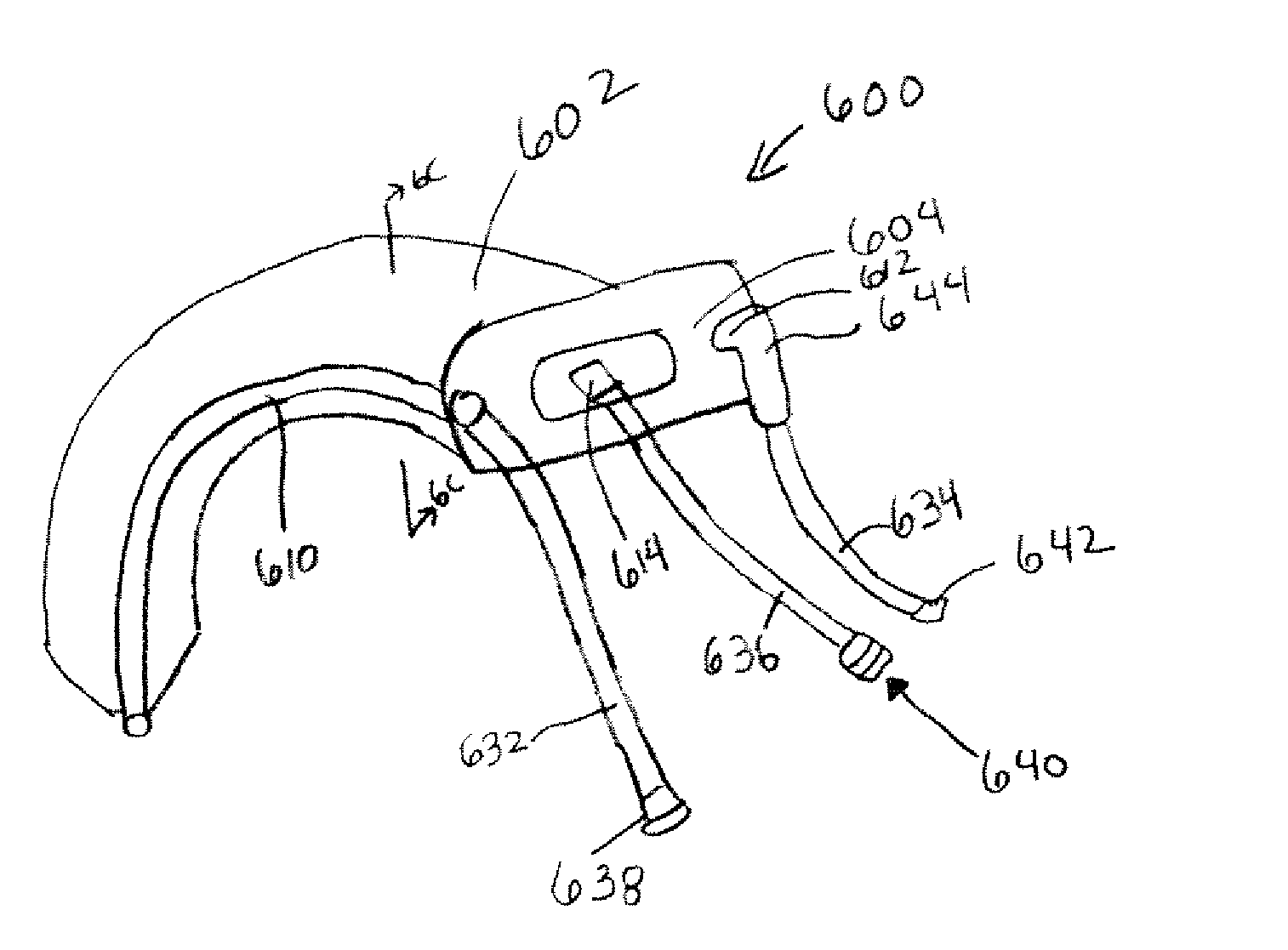
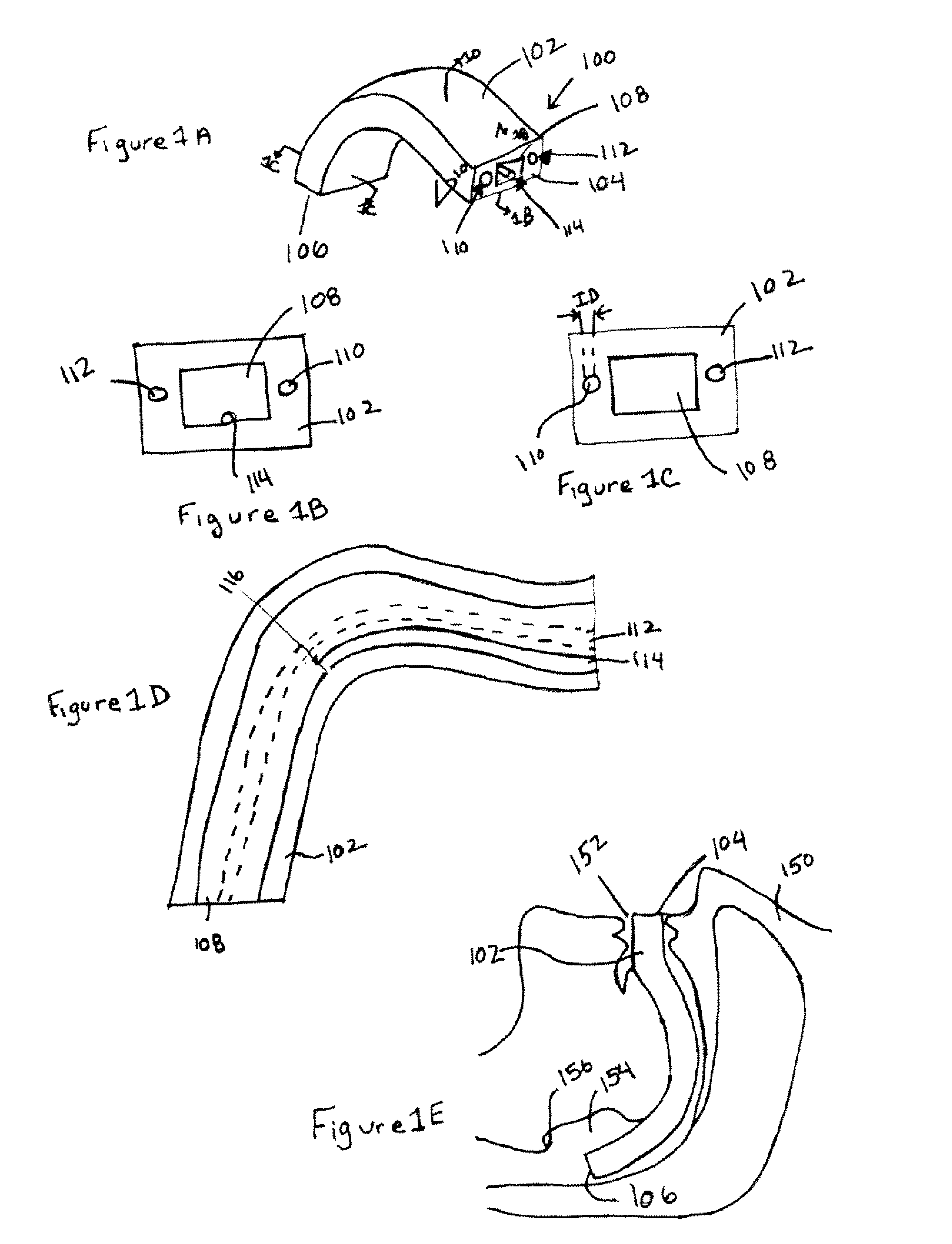
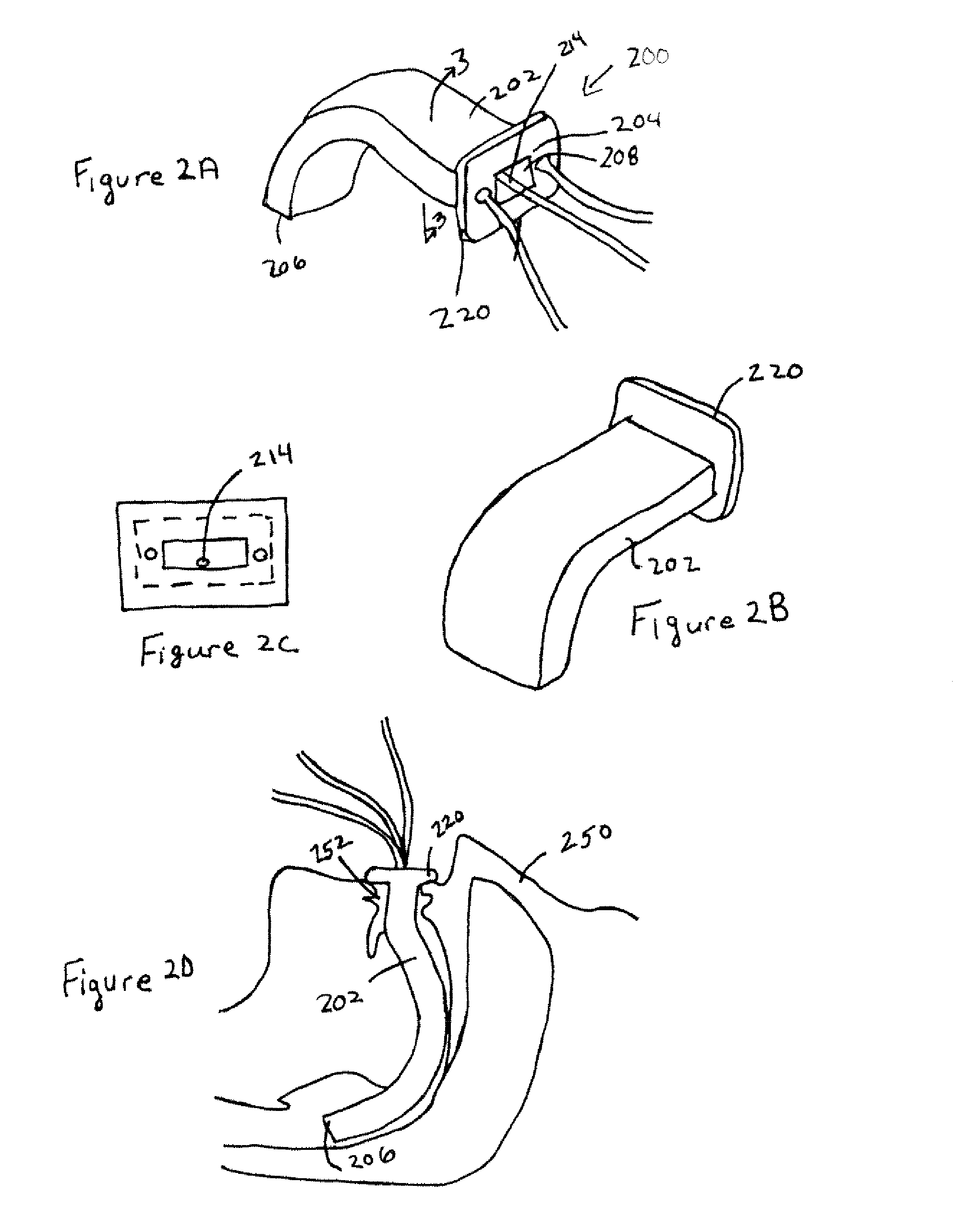
[0034] Referring to the drawings in which like reference numerals indicate like elements, there is shown in FIGS. 1A-E an oropharyngeal device 100 according to an exemplary embodiment of the present invention. The device 100 includes a body 102 having a proximal end 104 and a distal end 106.
[0035] A channel 108 forms an airway through the body 102 that extends through the body 102 from its proximal end 104 to its distal end 106. As illustrated in FIG. 1E, the body 102 is sized such that when the distal end 106 of the body 102 is inserted into the mouth 152 of a patient 150 until the proximal end 104 is disposed outside and adjacent to the patient's mouth 152, the distal end 106 of the body 102 is disposed within the pharynx 154 above the epiglottis 156. The body 102 may be formed of a rigid material to serve as a bite block to prevent the patient from biting any conduits inserted through the channel.
[0036] The airway channel may be completely enclosed within the body of the oropha...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com