Patents
Literature
25719results about "Intravenous devices" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
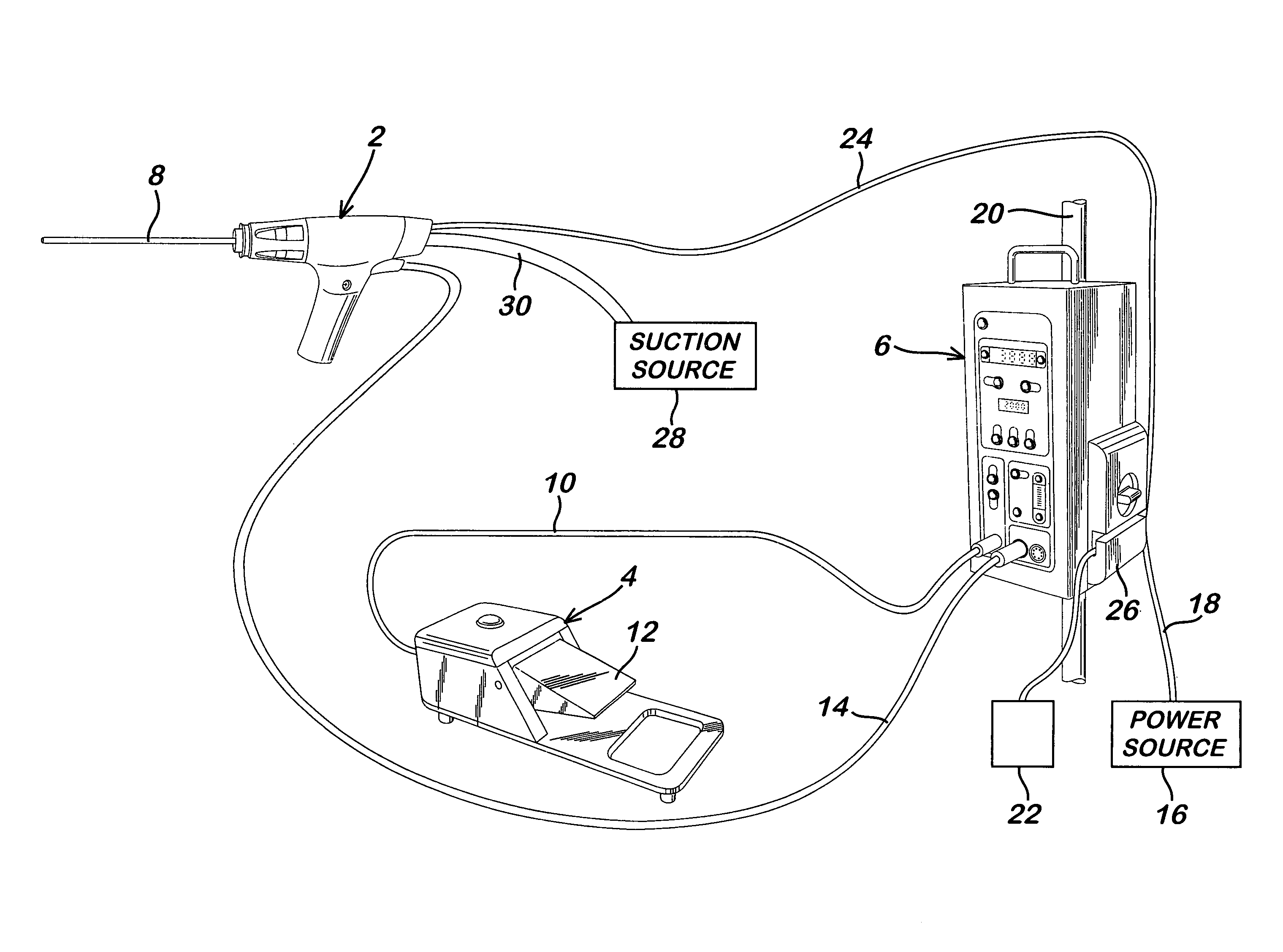
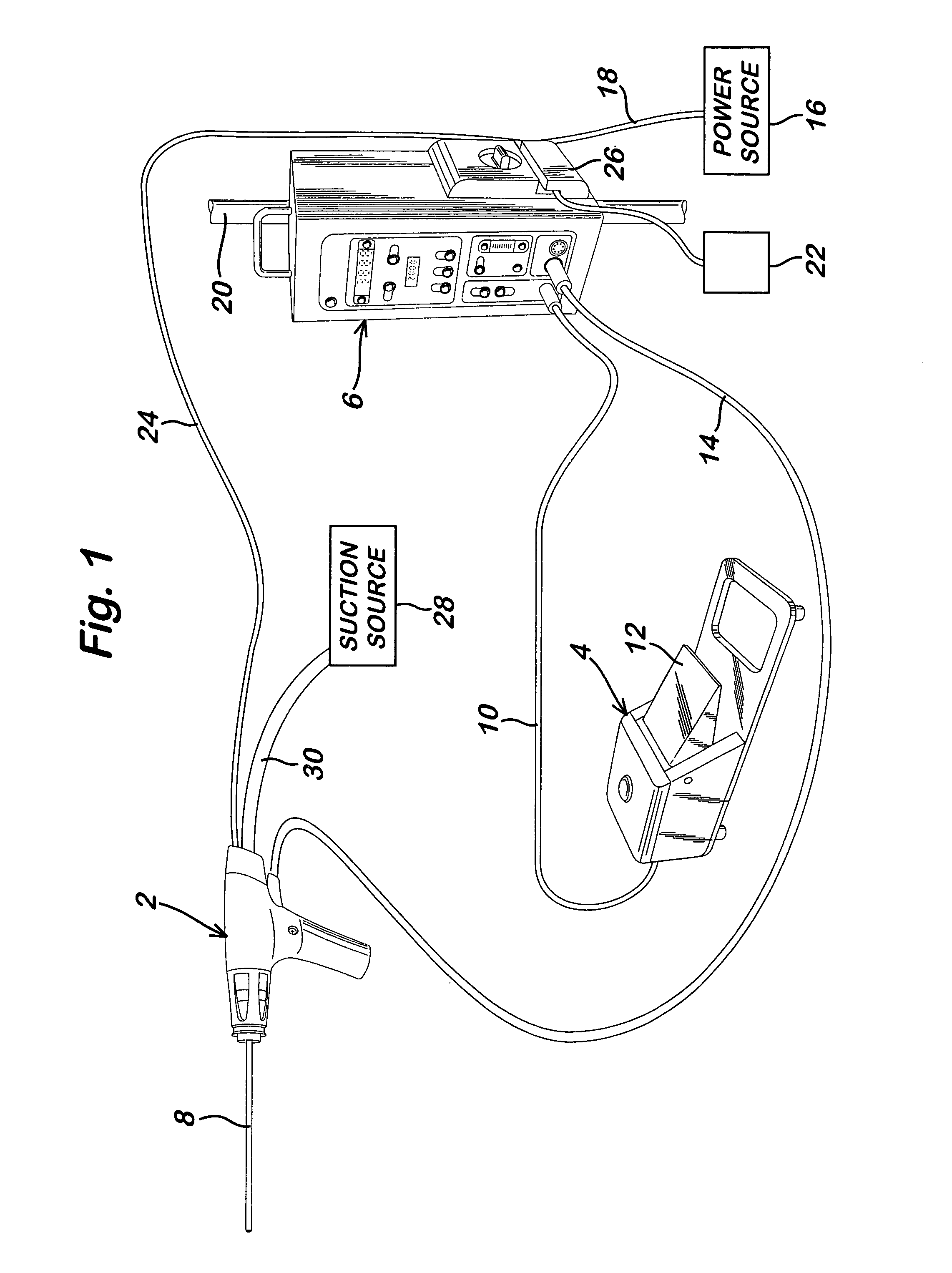
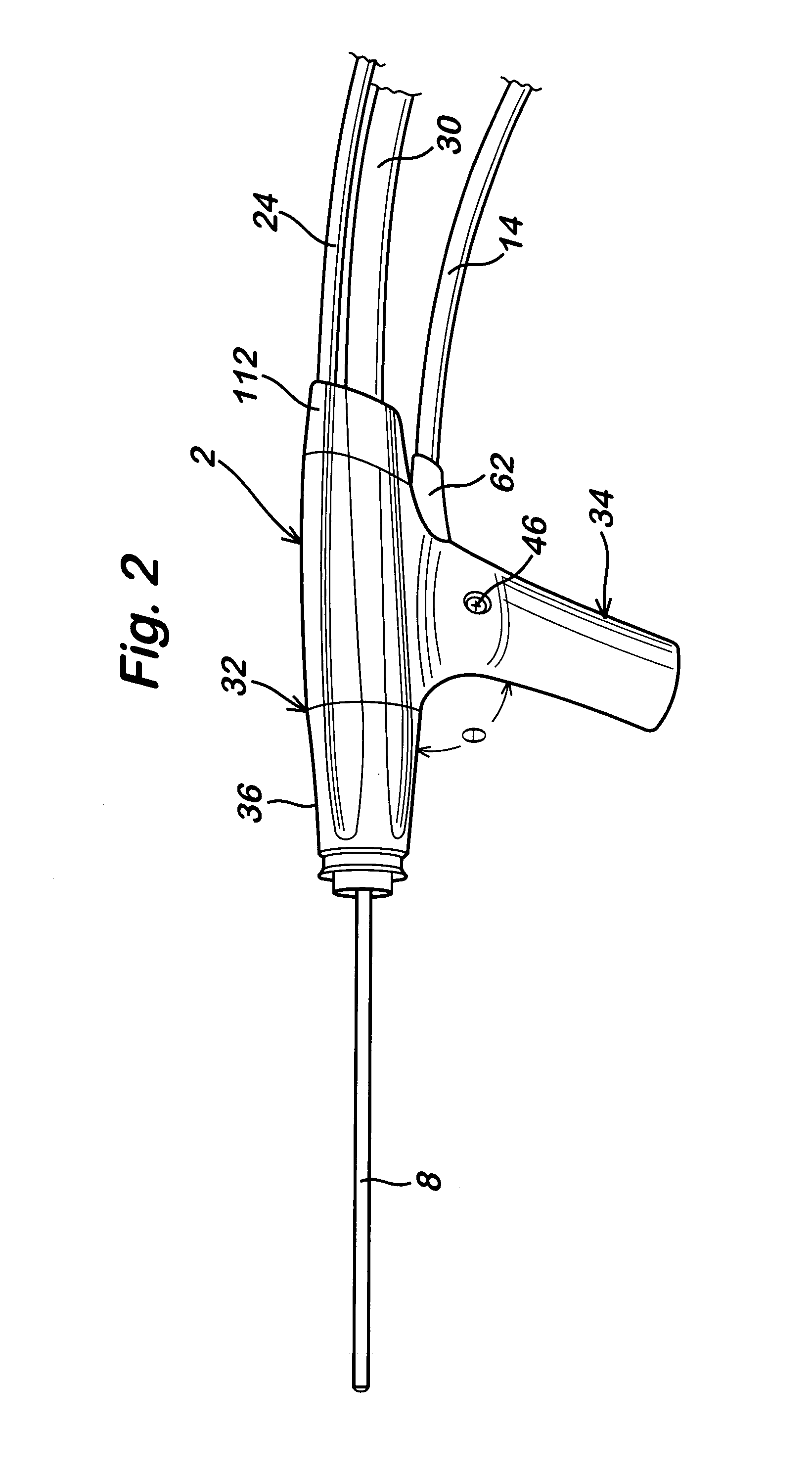
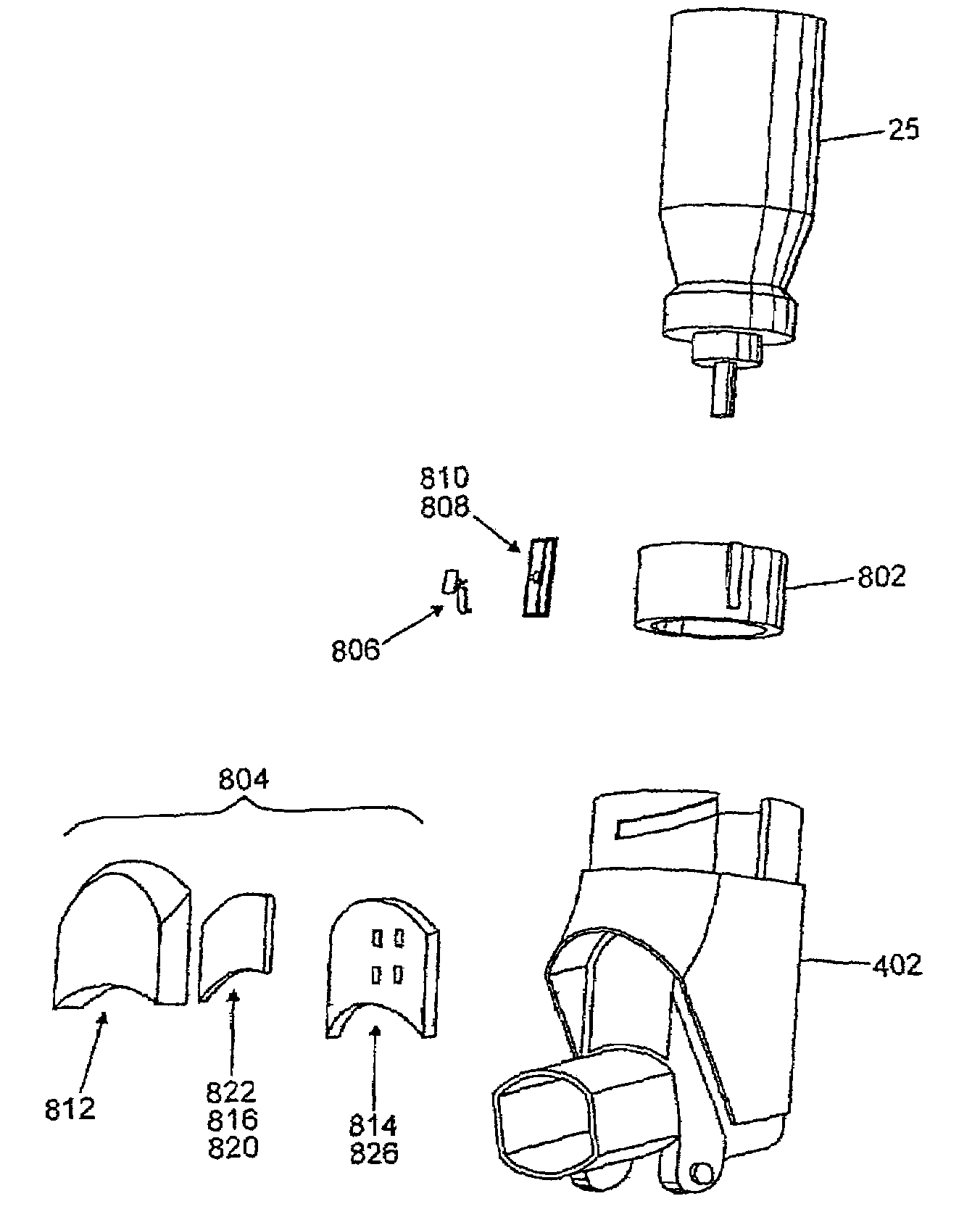
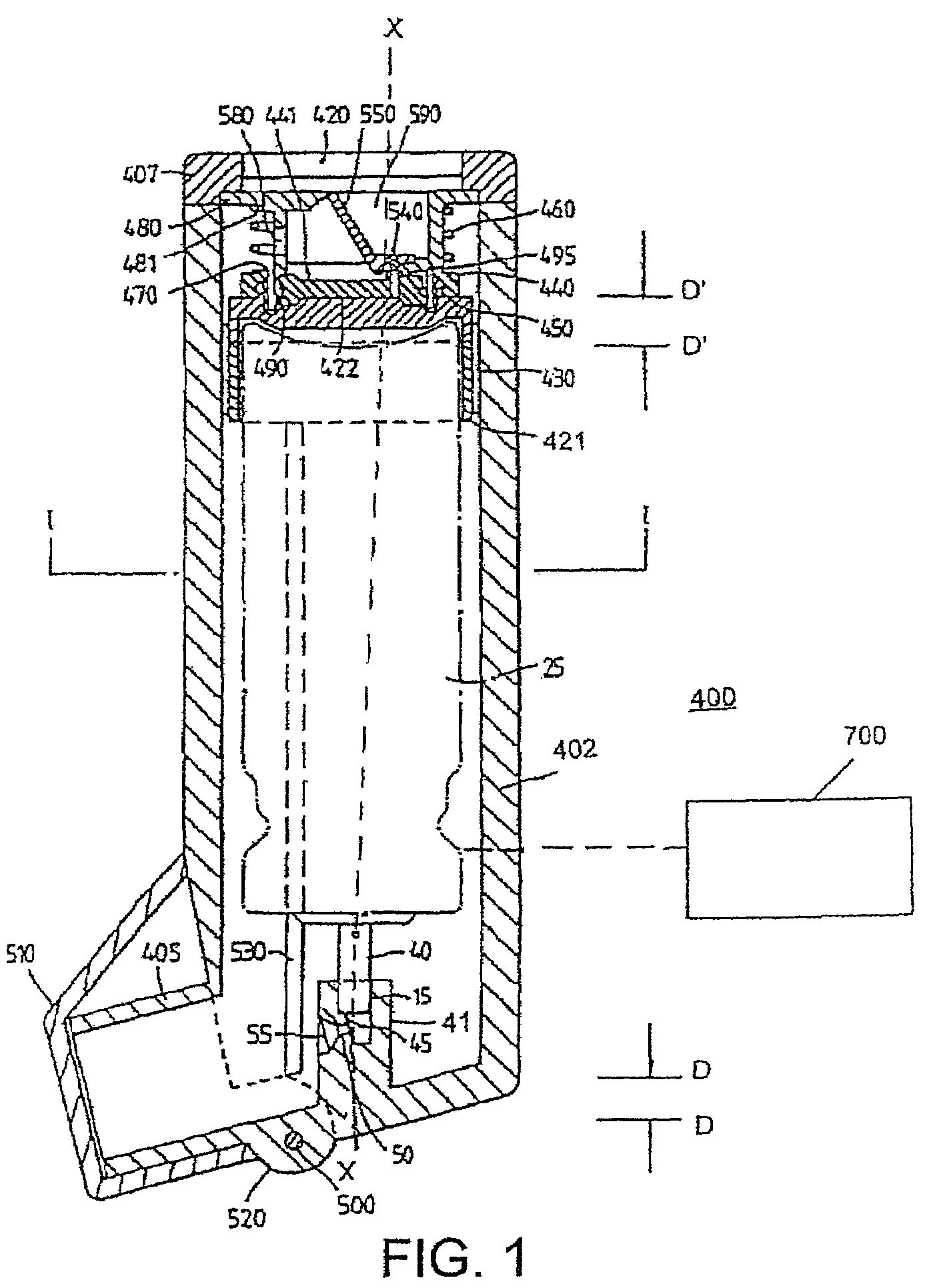
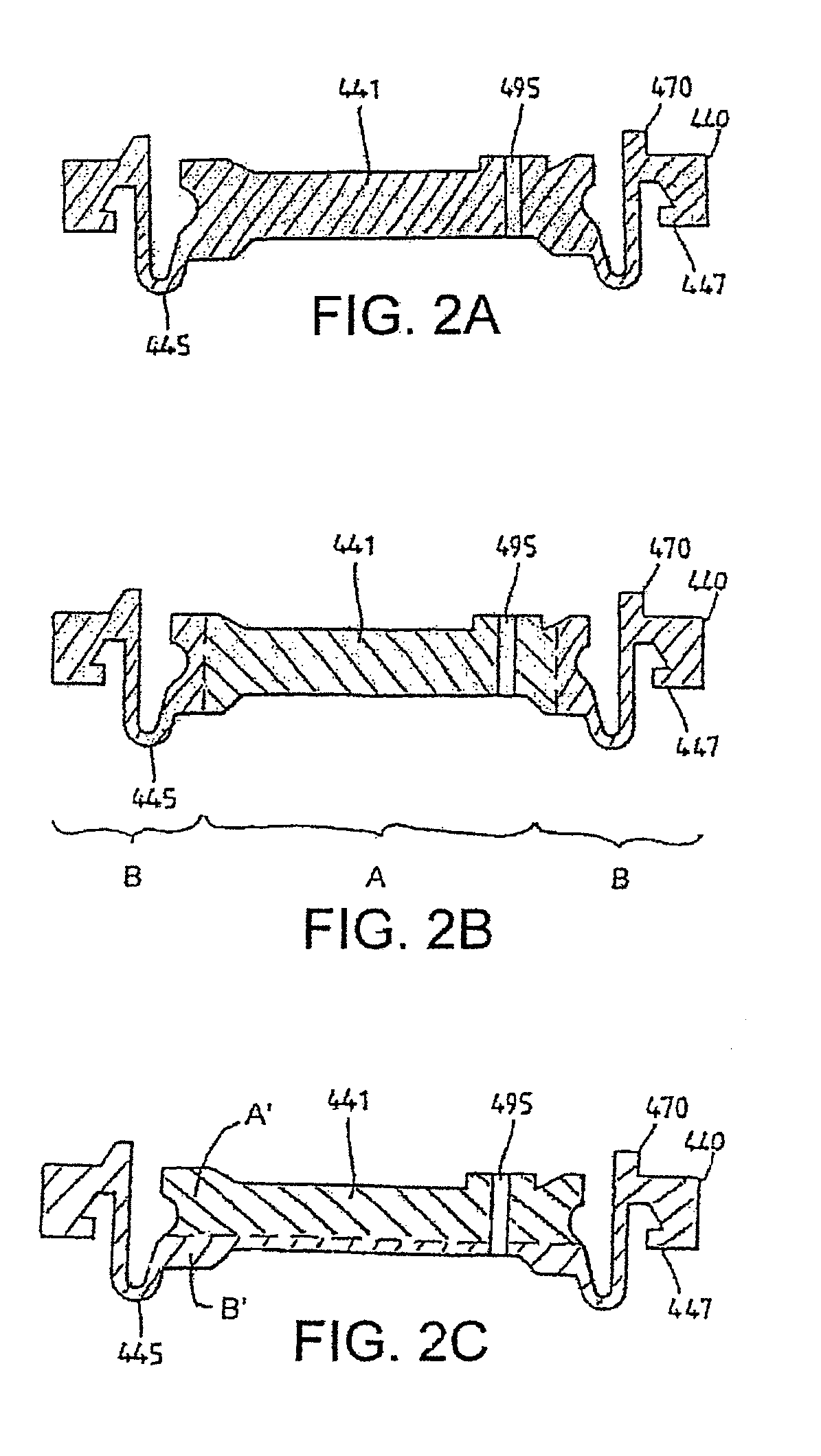
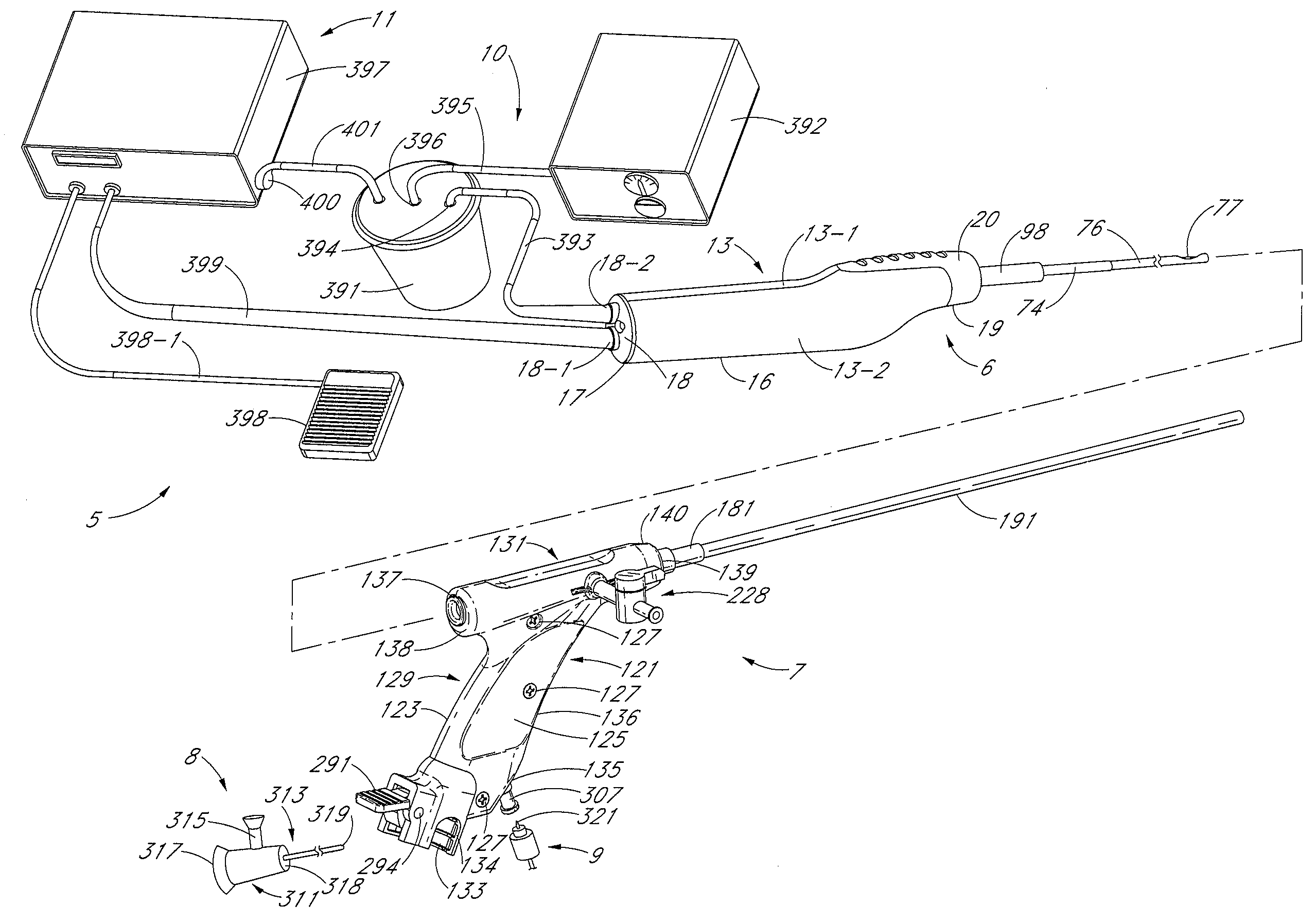
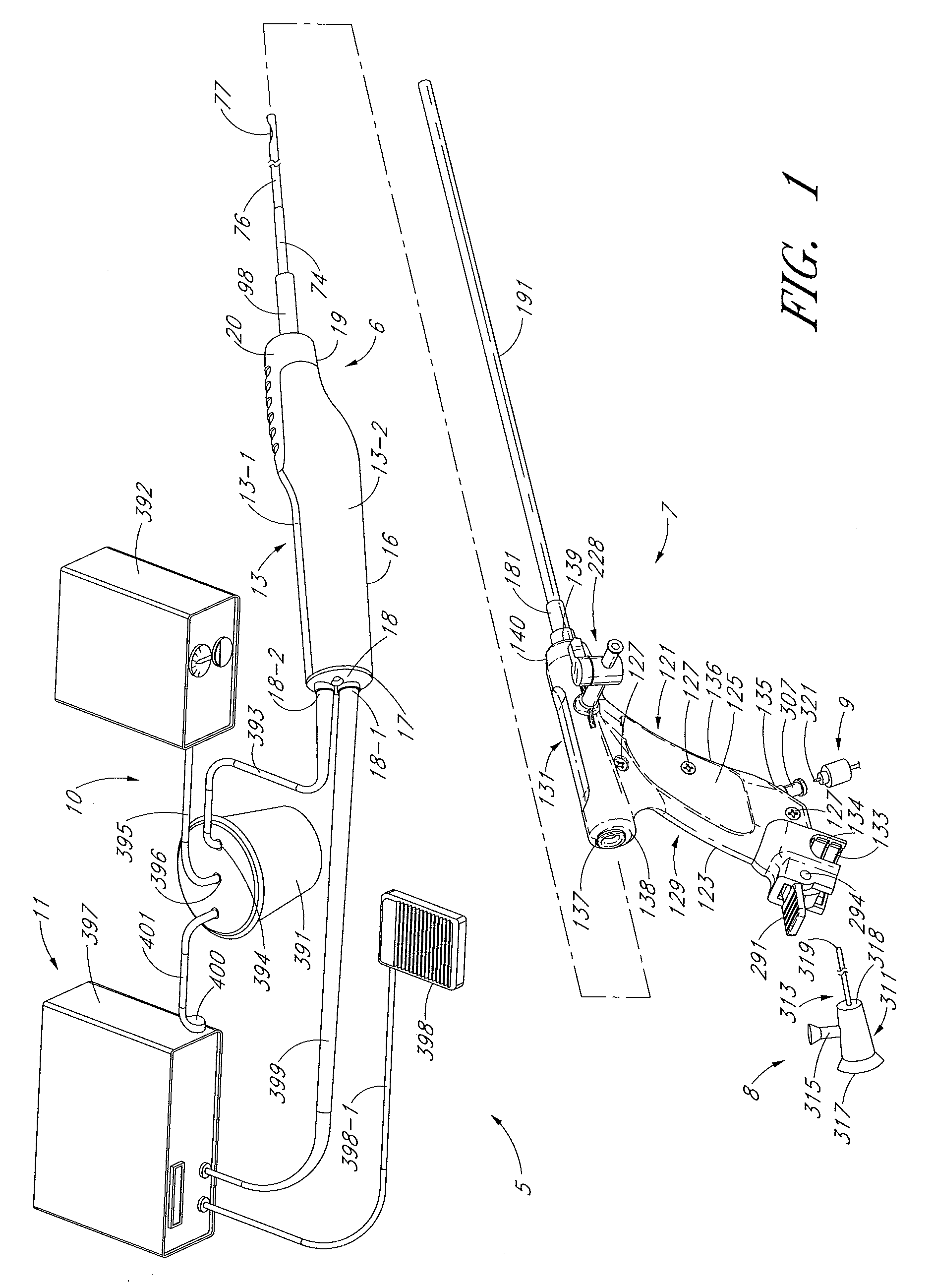
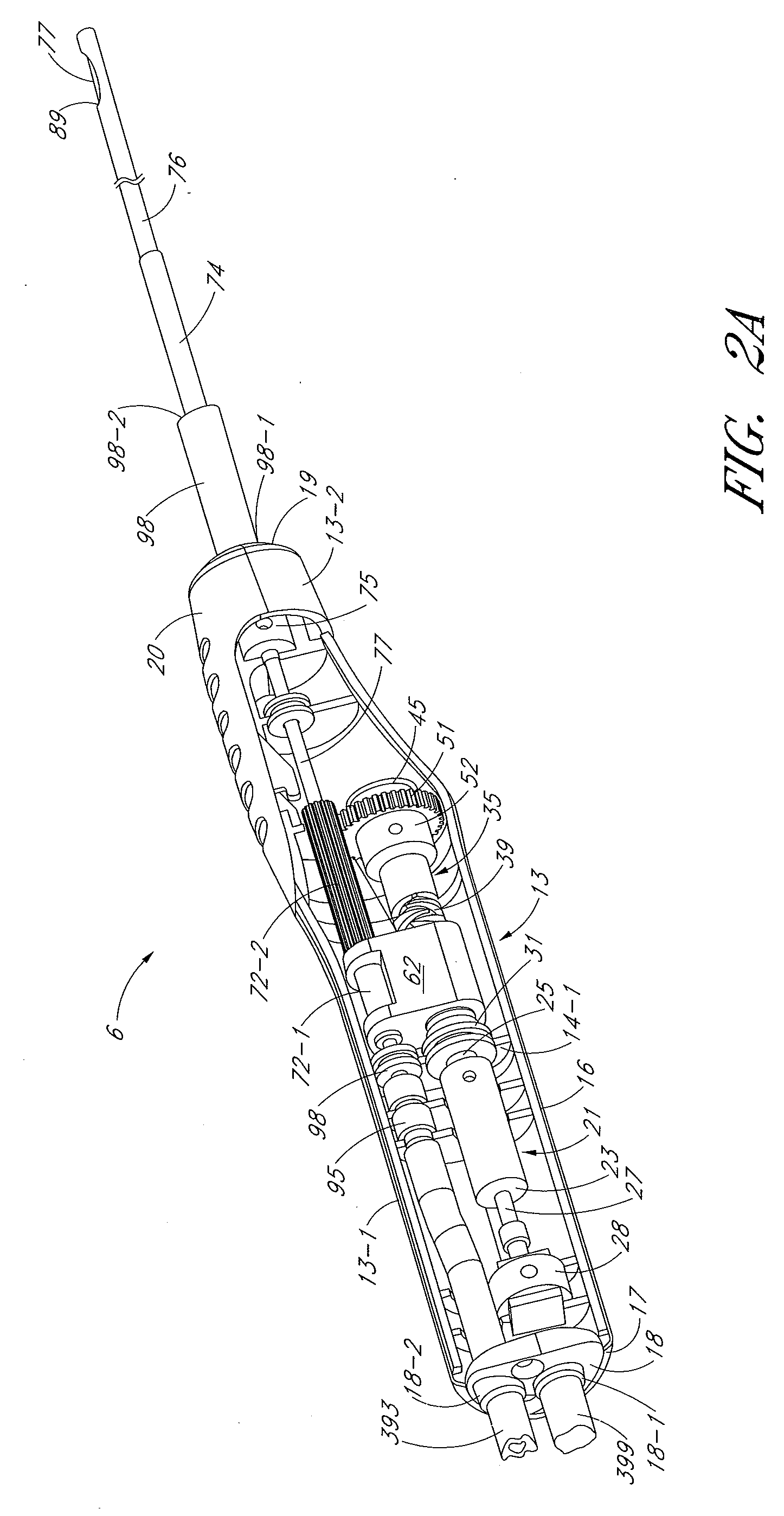
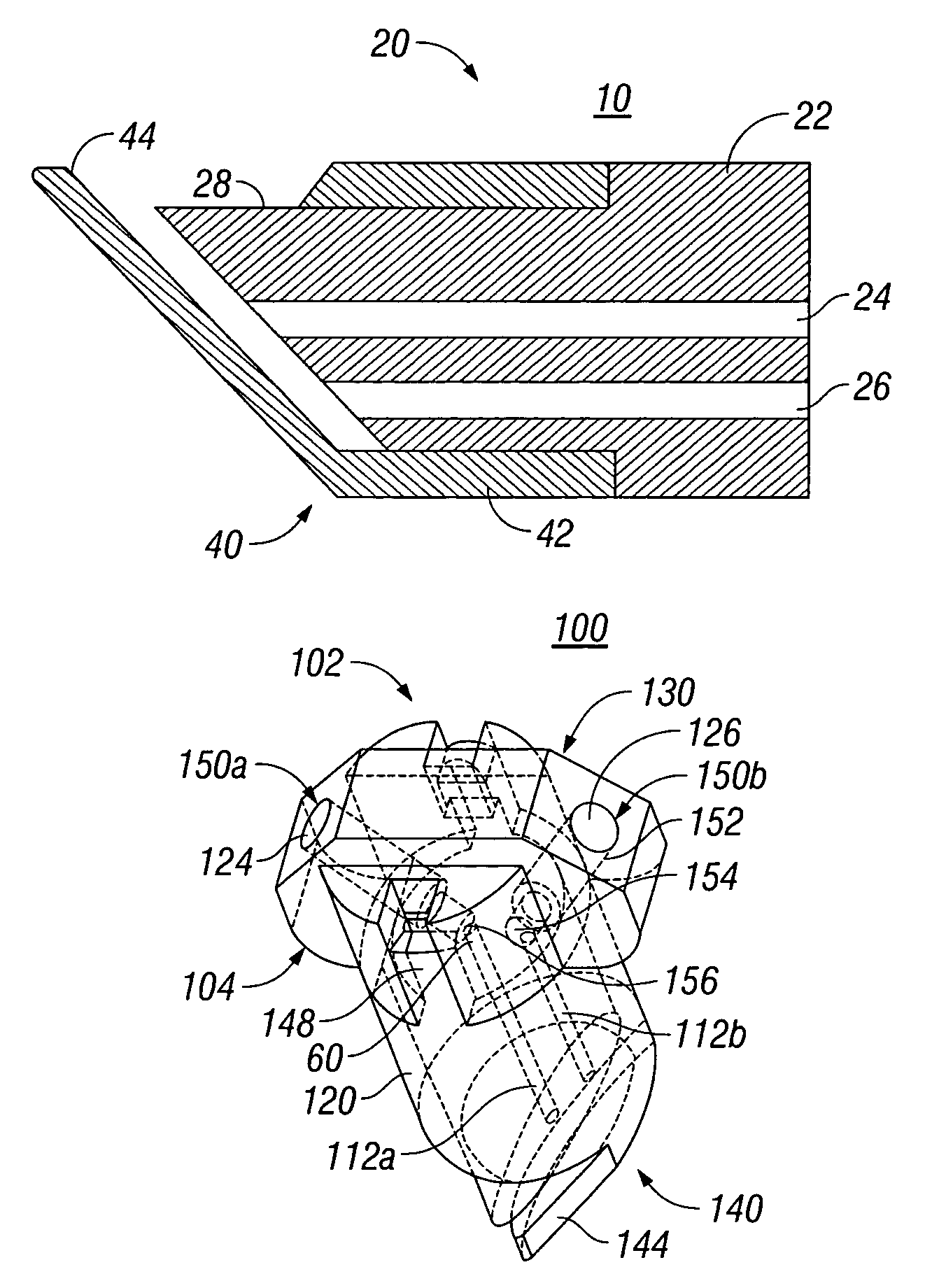
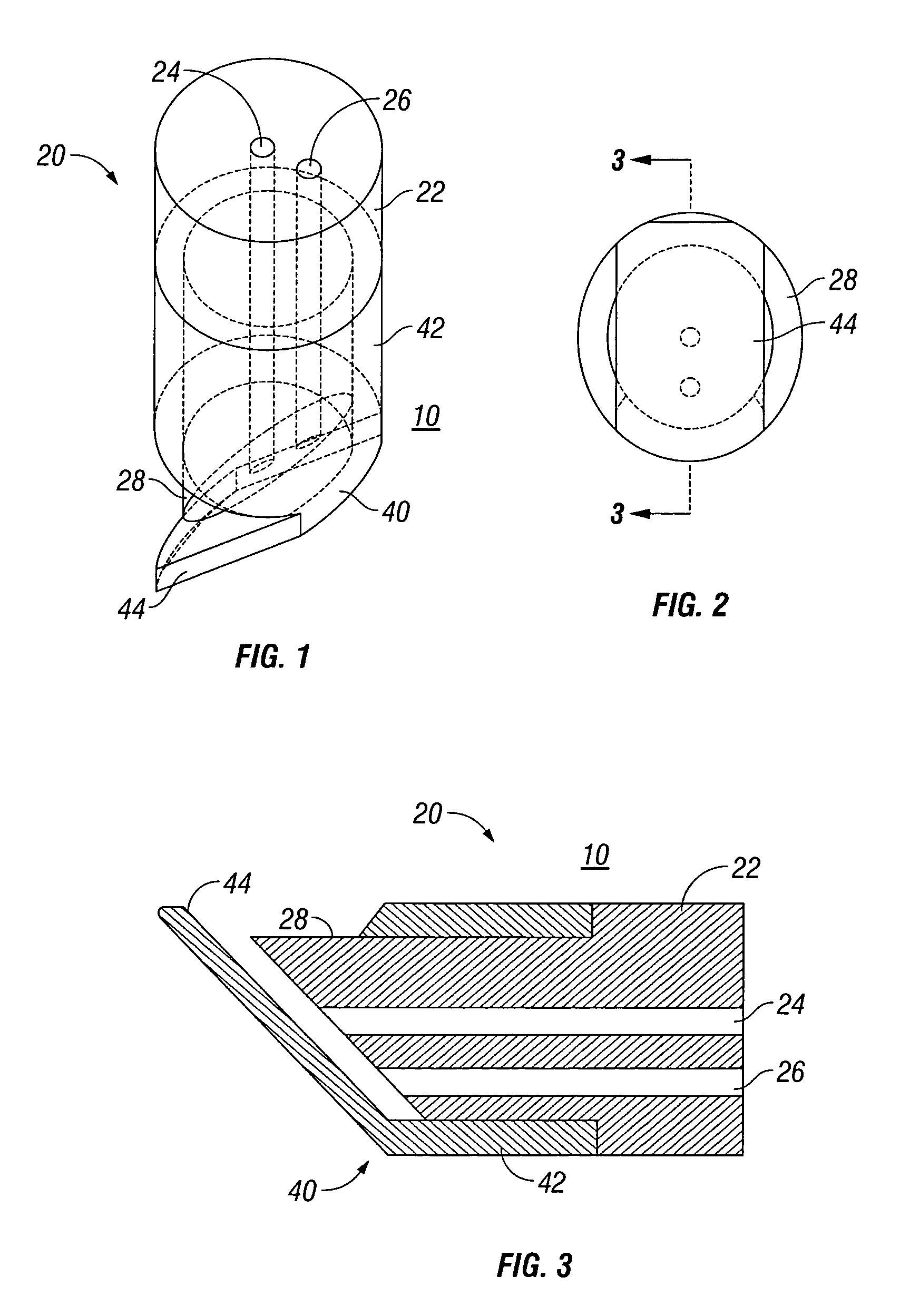
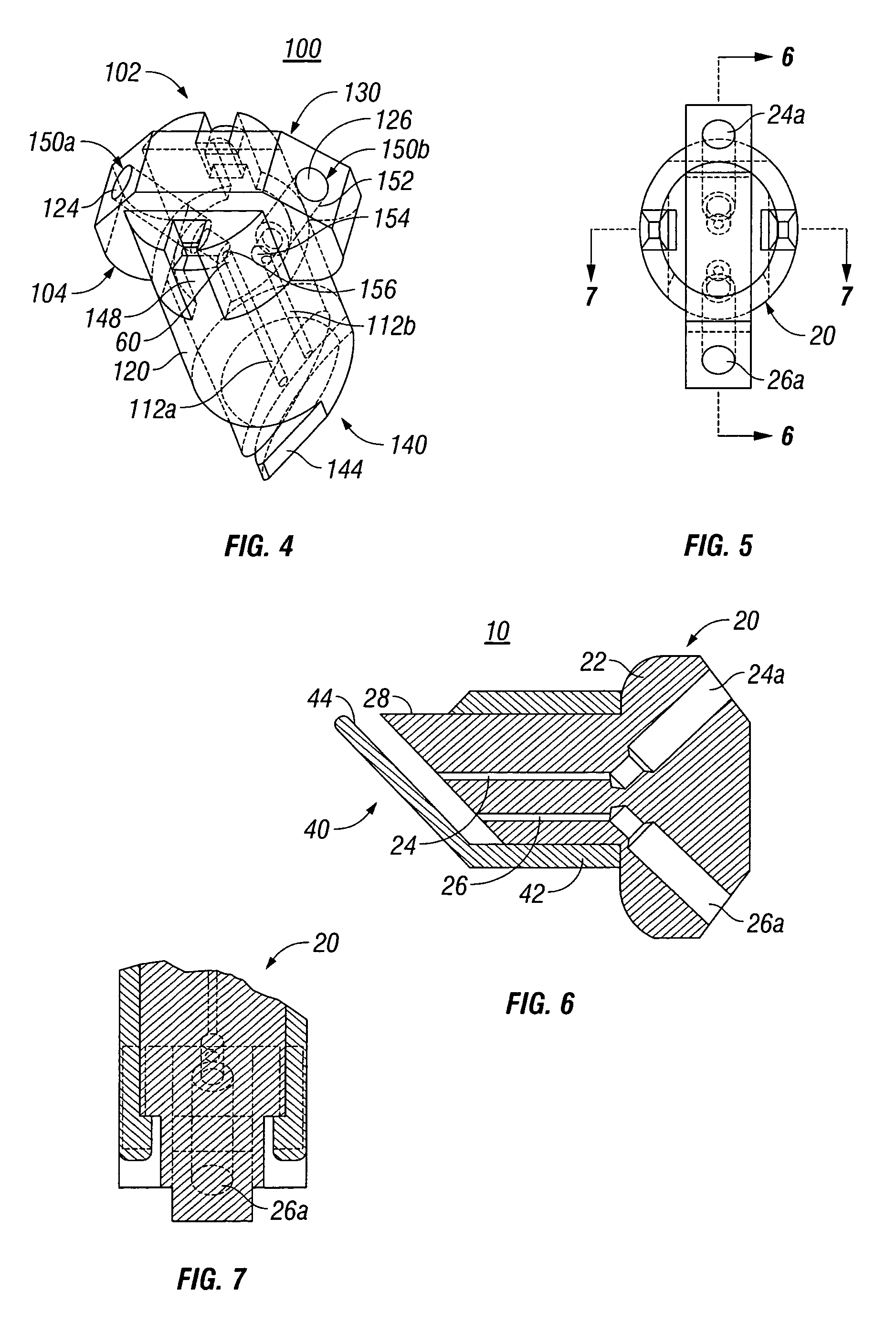
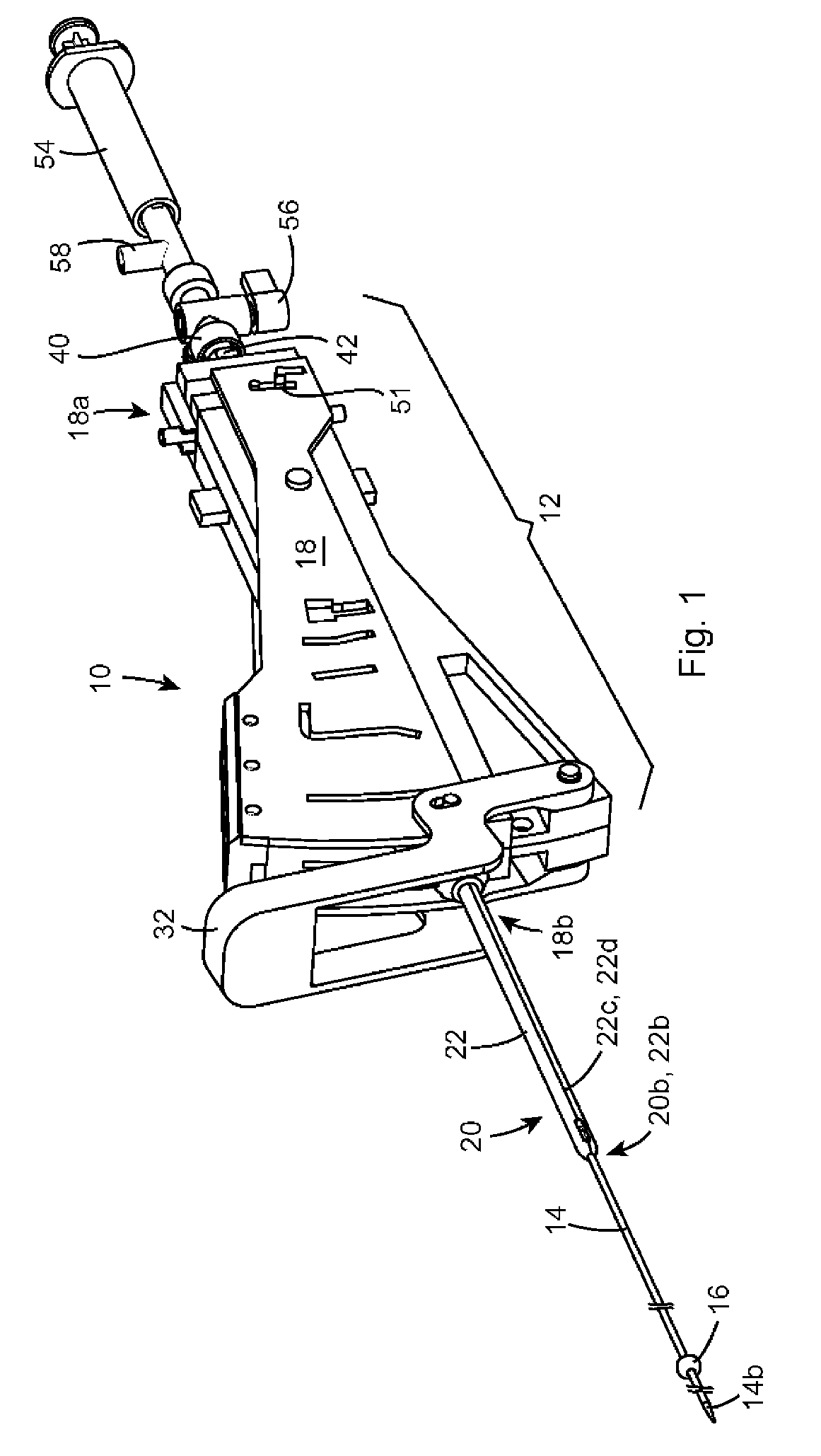
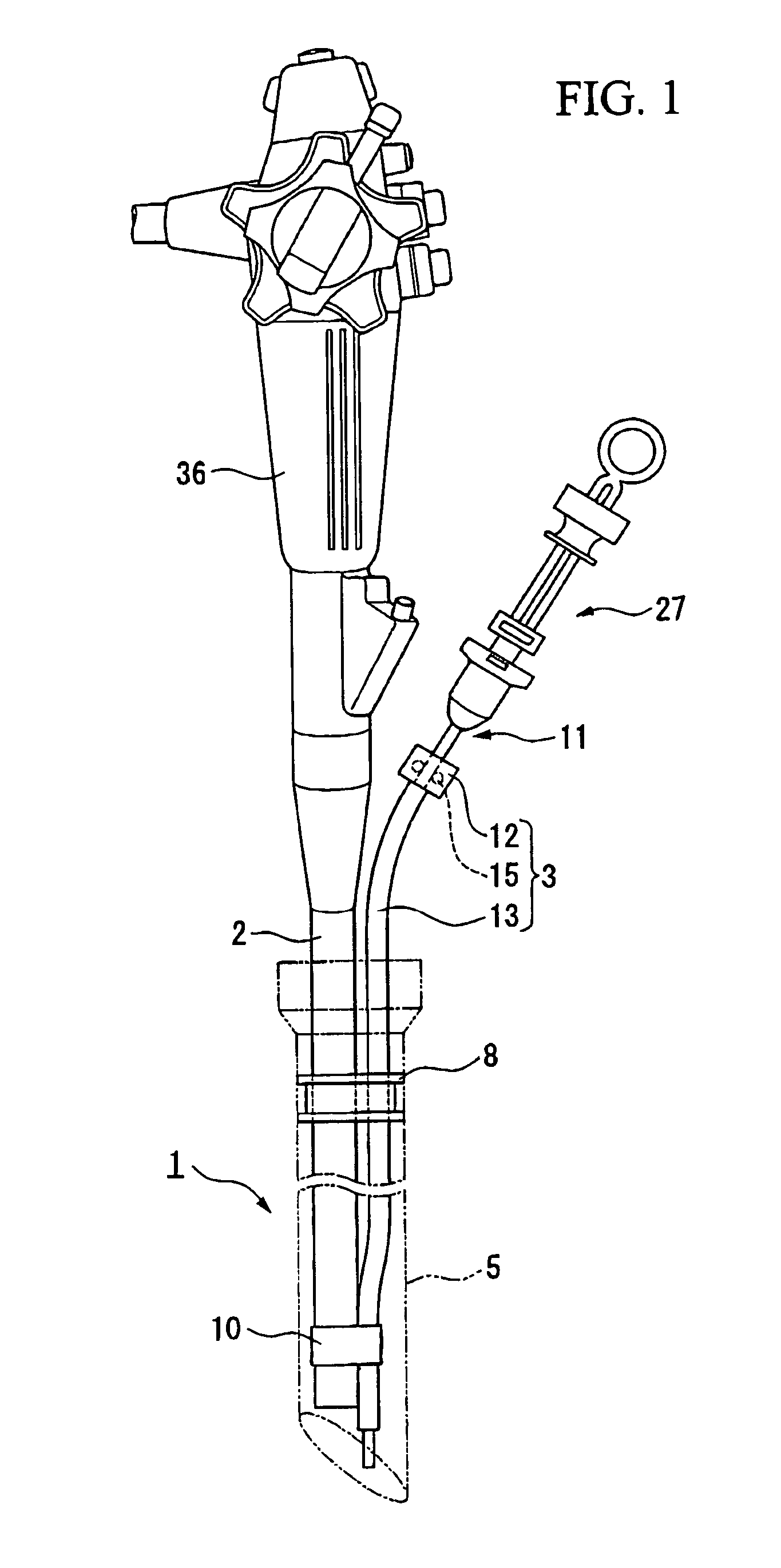
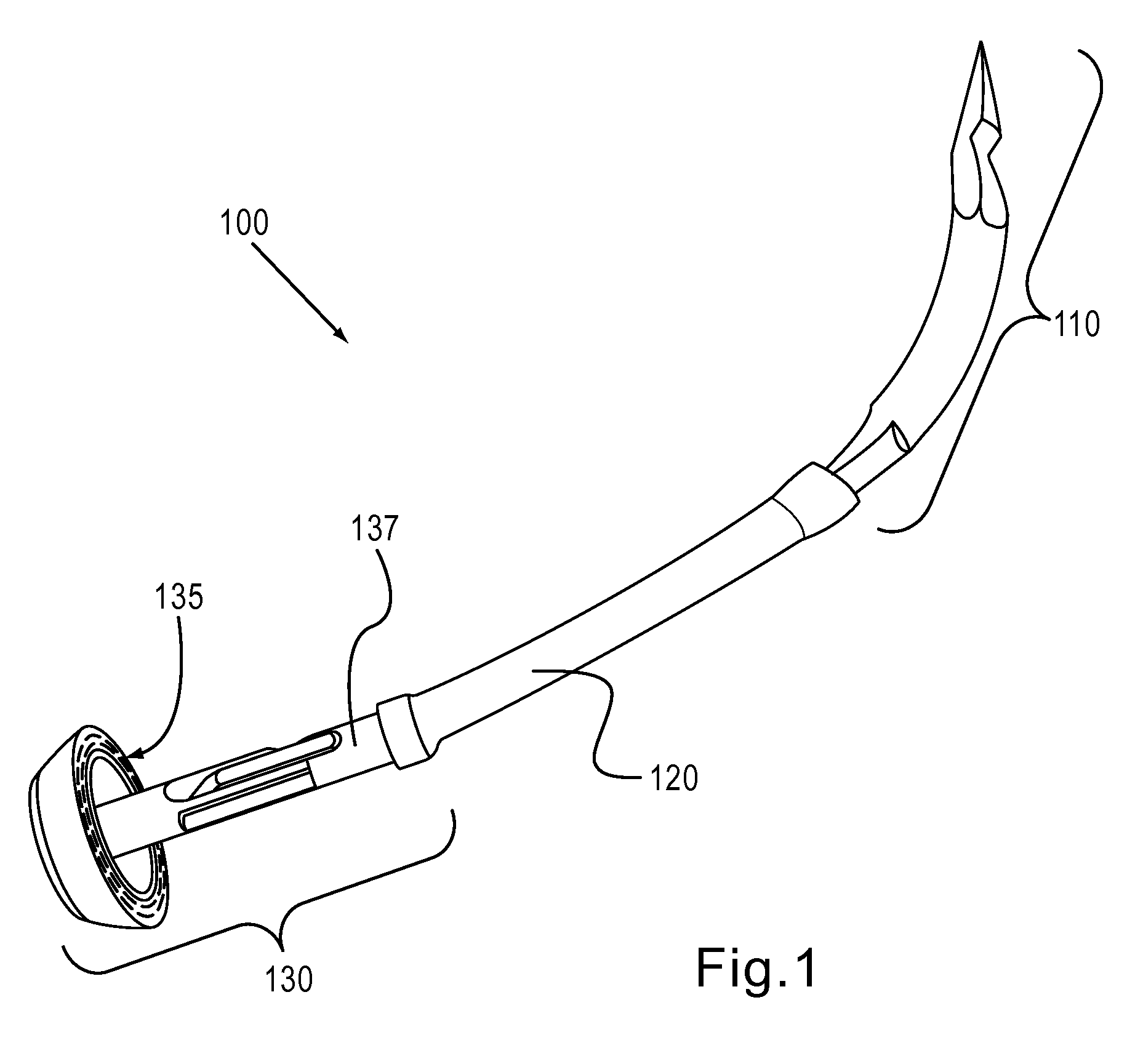
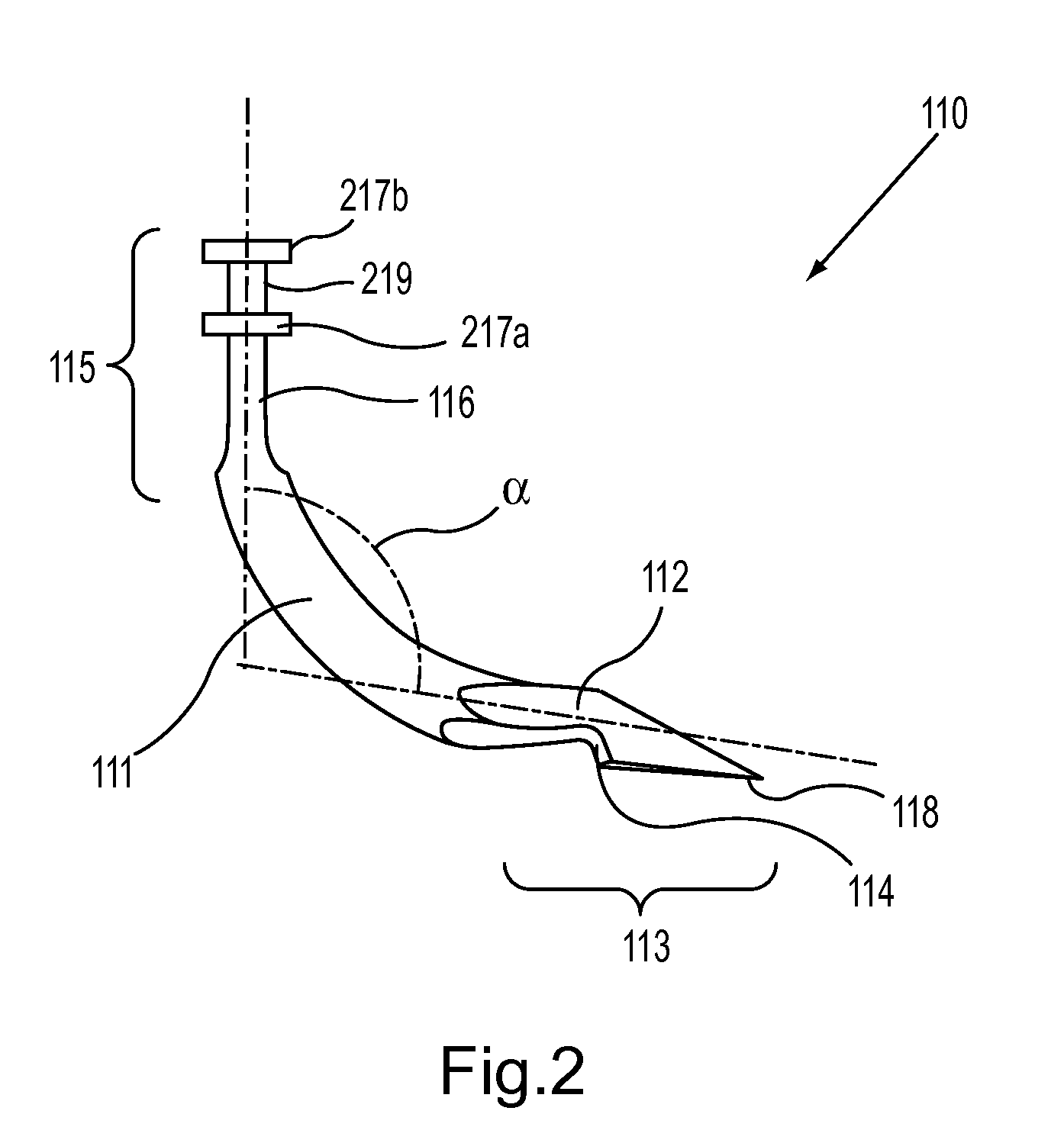
Powered surgical apparatus, method of manufacturing powered surgical apparatus, and method of using powered surgical apparatus
ActiveUS7247161B2Promotes its utilizationFacilitate and promote ease and effectiveness of cleaning and sterilizationSleeve/socket jointsIncision instrumentsEngineeringIrrigation fluids
A powered surgical apparatus can be used with a source of irrigation fluid and a source of suction. The powered surgical apparatus can include a cutting blade assembly and a handle. The handle can include an upper portion defining a distal section connectable to the cutting blade assembly and a lower portion extending downwardly from the upper portion. The handle can be connectable to the source of irrigation fluid and the source of suction. The system can also include a manually actuable input device that provides at least one signal relevant to at least one operation of the system, and a controller that receives the at least one input signal and provides an output signal to perform the at least one operation of the system.
Owner:GYRUS ACMI INC (D B A OLYMPUS SURGICAL TECH AMERICA) +1
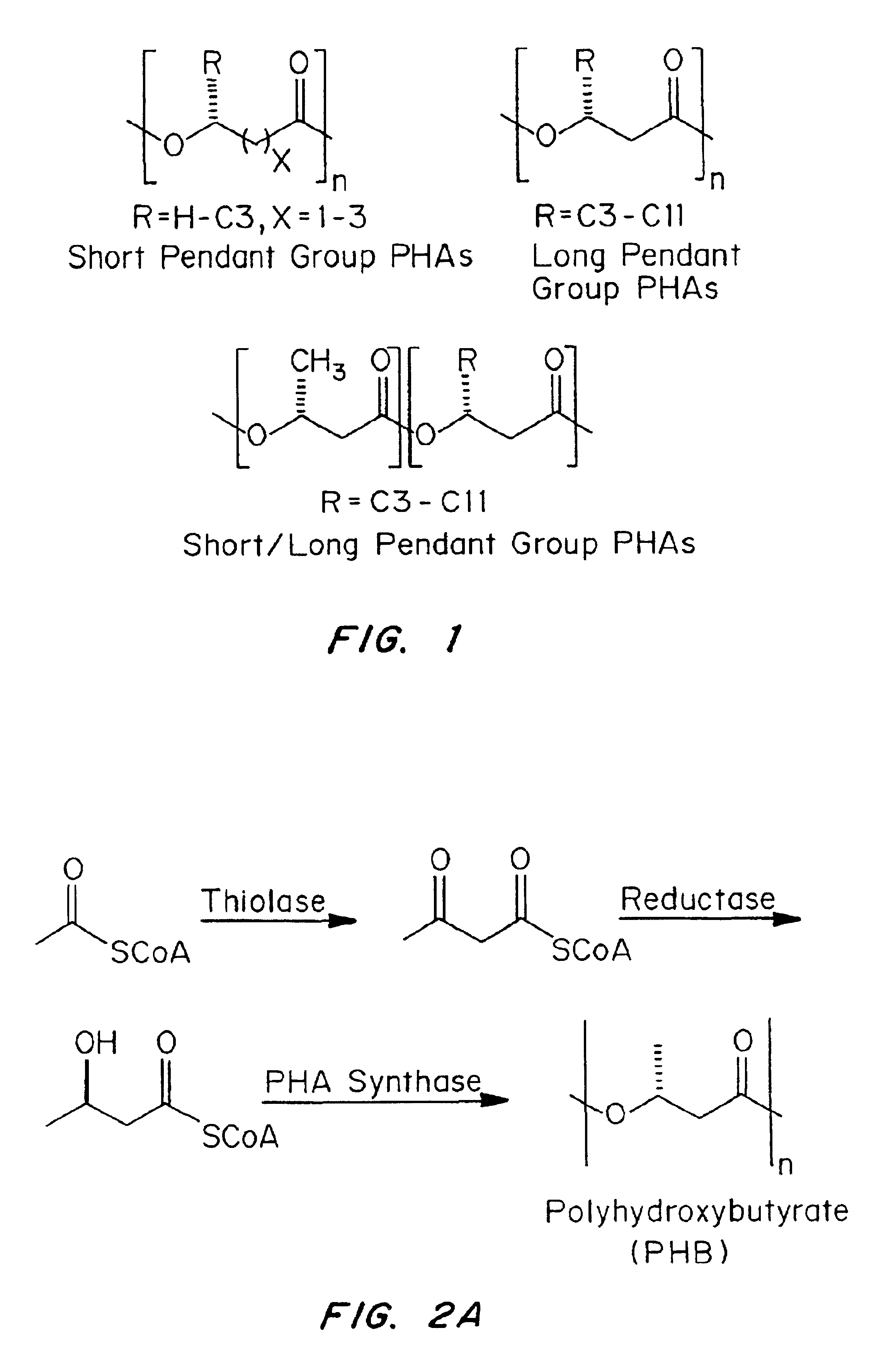
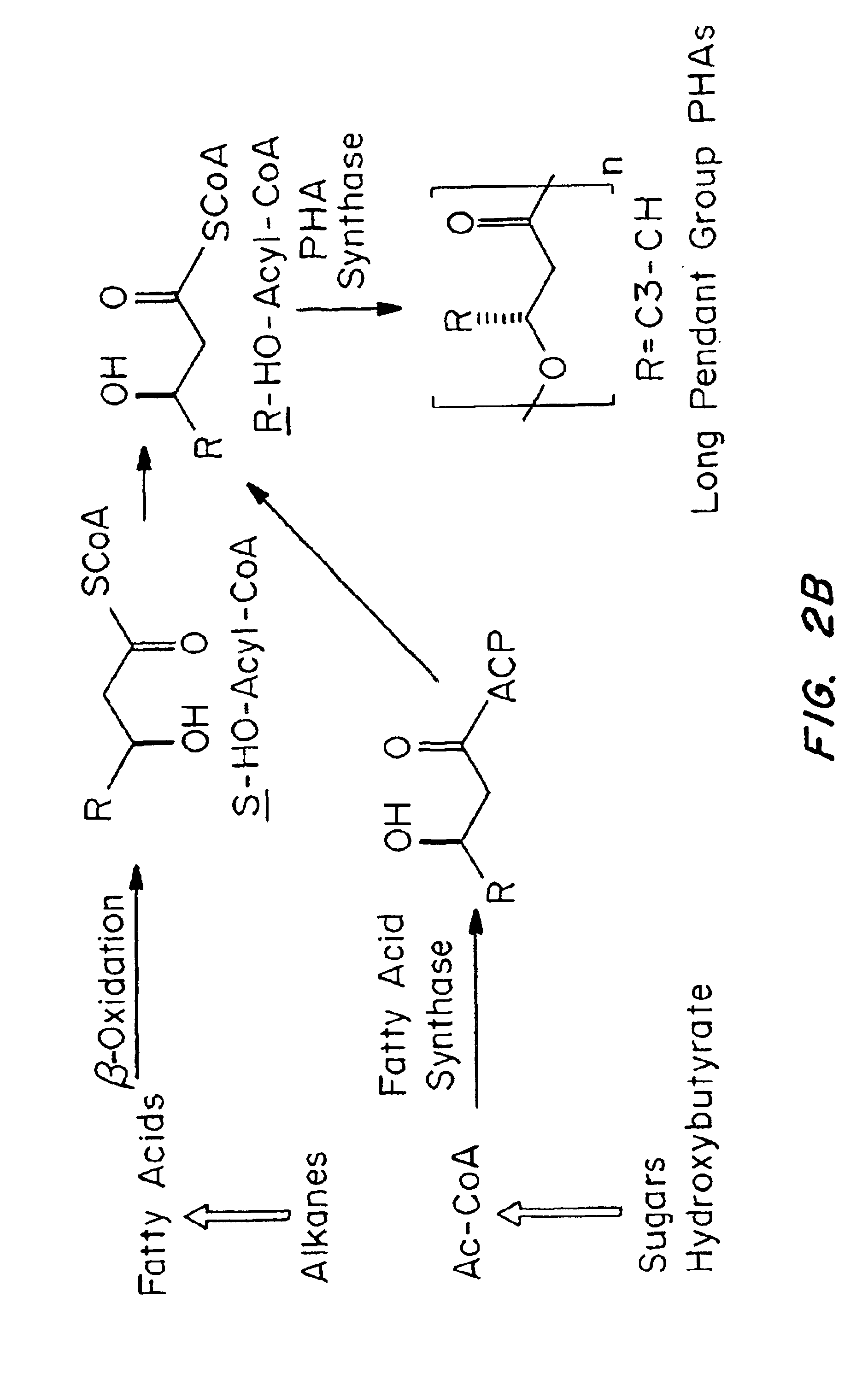
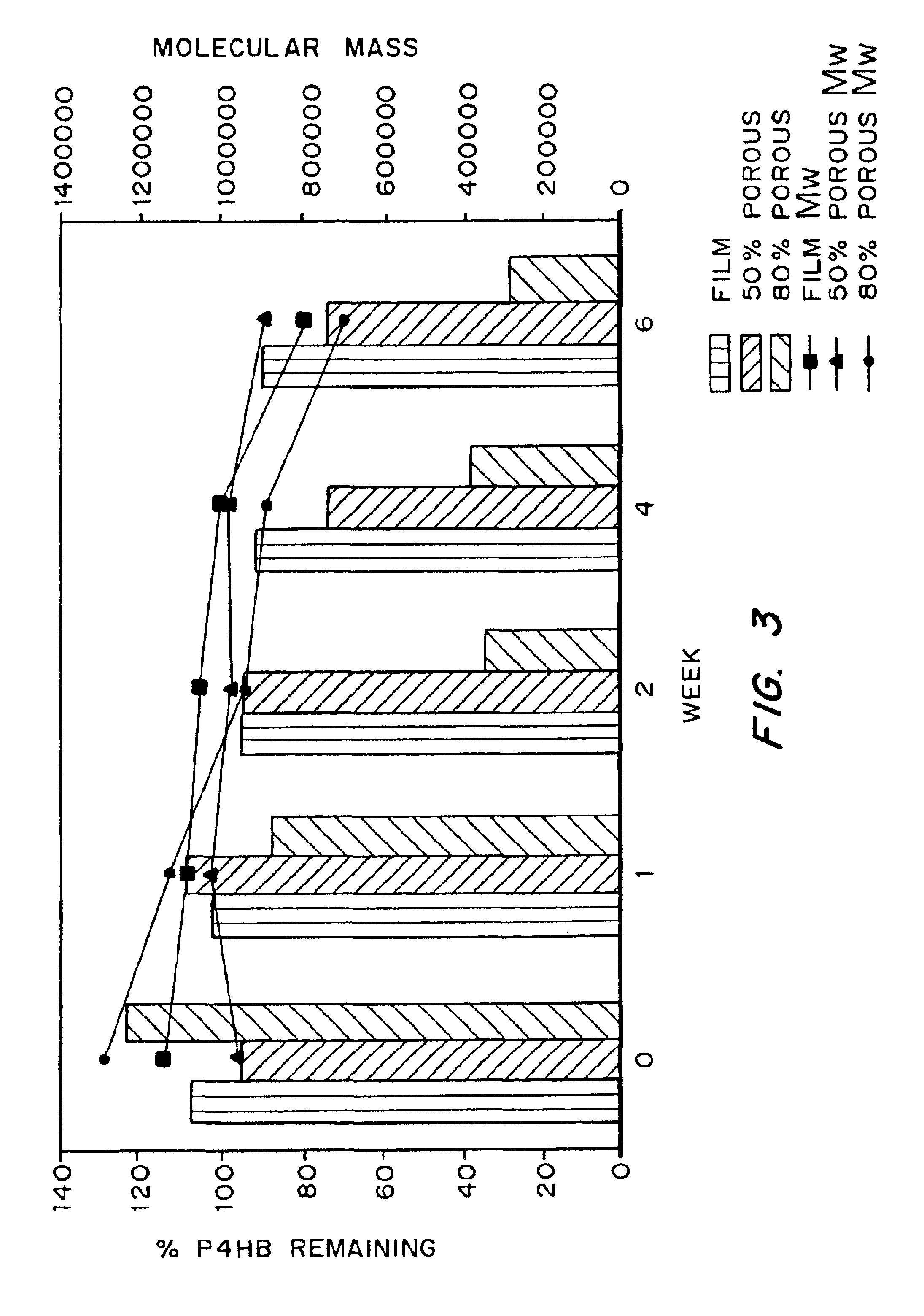
Medical devices and applications of polyhydroxyalkanoate polymers
InactiveUS6838493B2High porosityReduce probabilitySuture equipmentsOrganic active ingredientsTissue repairBiocompatibility Testing
Devices formed of or including biocompatible polyhydroxyalkanoates are provided with controlled degradation rates, preferably less than one year under physiological conditions. Preferred devices include sutures, suture fasteners, meniscus repair devices, rivets, tacks, staples, screws (including interference screws), bone plates and bone plating systems, surgical mesh, repair patches, slings, cardiovascular patches, orthopedic pins (including bone filling augmentation material), adhesion barriers, stents, guided tissue repair / regeneration devices, articular cartilage repair devices, nerve guides, tendon repair devices, atrial septal defect repair devices, pericardial patches, bulking and filling agents, vein valves, bone marrow scaffolds, meniscus regeneration devices, ligament and tendon grafts, ocular cell implants, spinal fusion cages, skin substitutes, dural substitutes, bone graft substitutes, bone dowels, wound dressings, and hemostats. The polyhydroxyalkanoates can contain additives, be formed of mixtures of monomers or include pendant groups or modifications in their backbones, or can be chemically modified, all to alter the degradation rates. The polyhydroxyalkanoate compositions also provide favorable mechanical properties, biocompatibility, and degradation times within desirable time frames under physiological conditions.
Owner:TEPHA INC
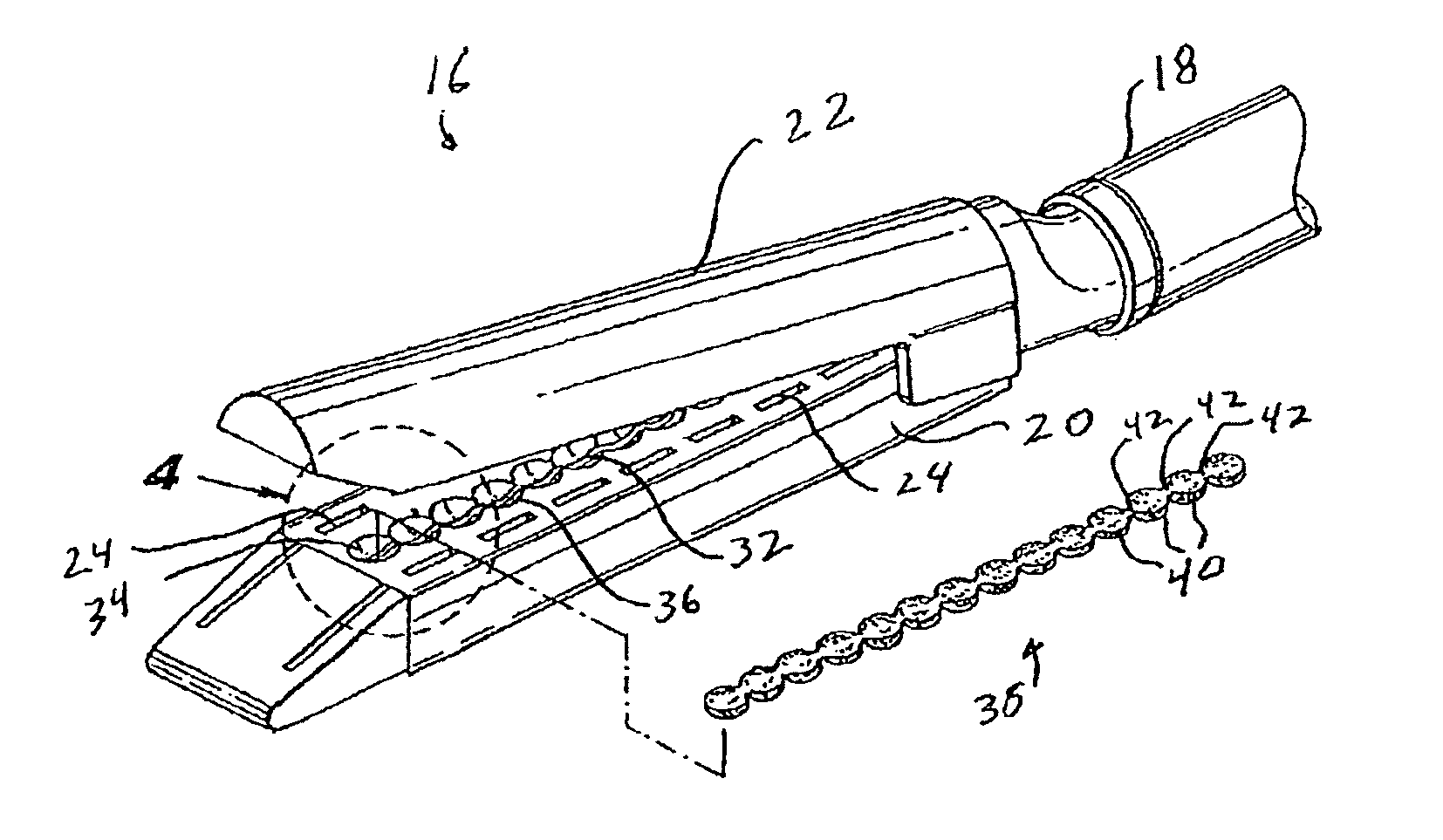
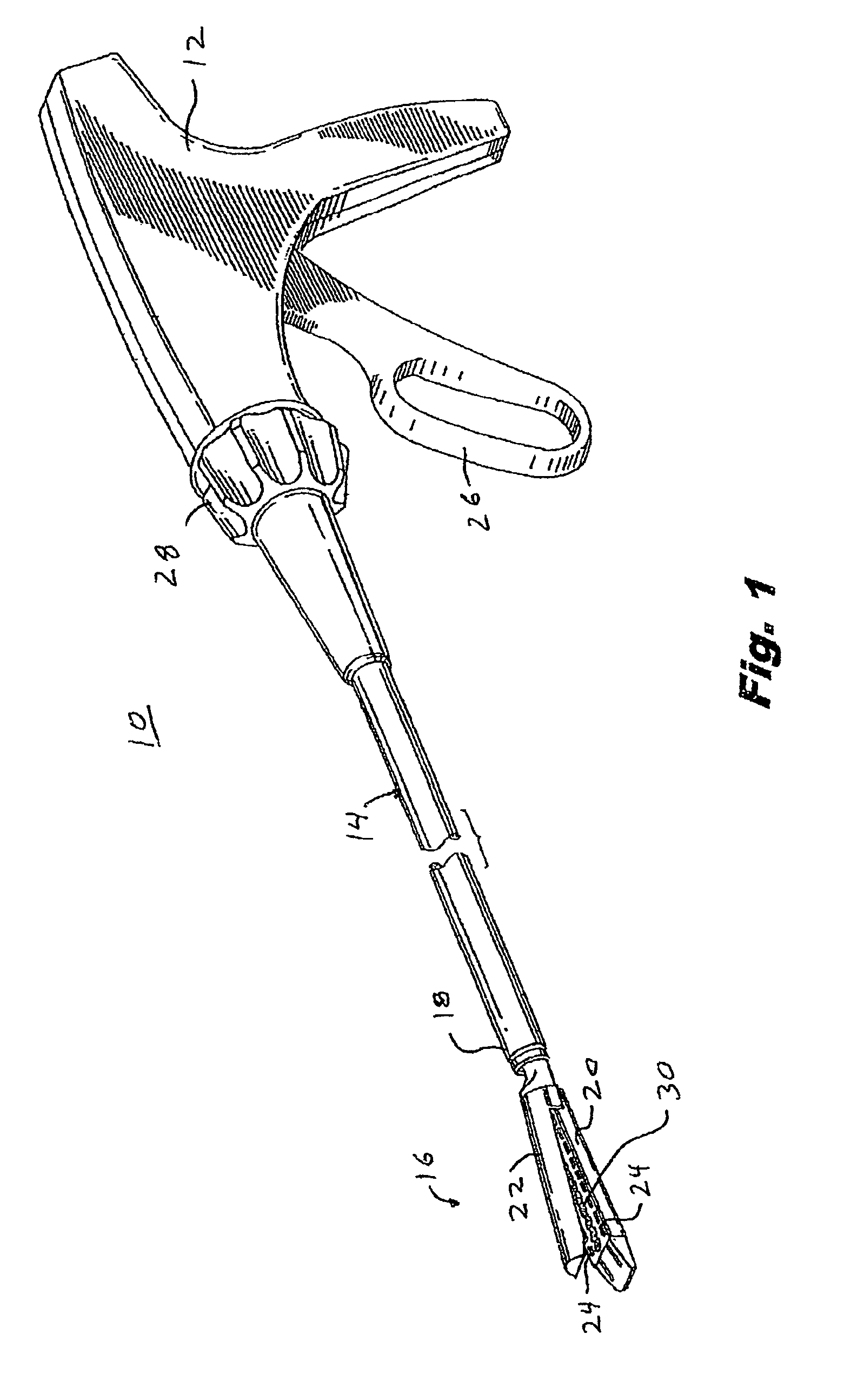
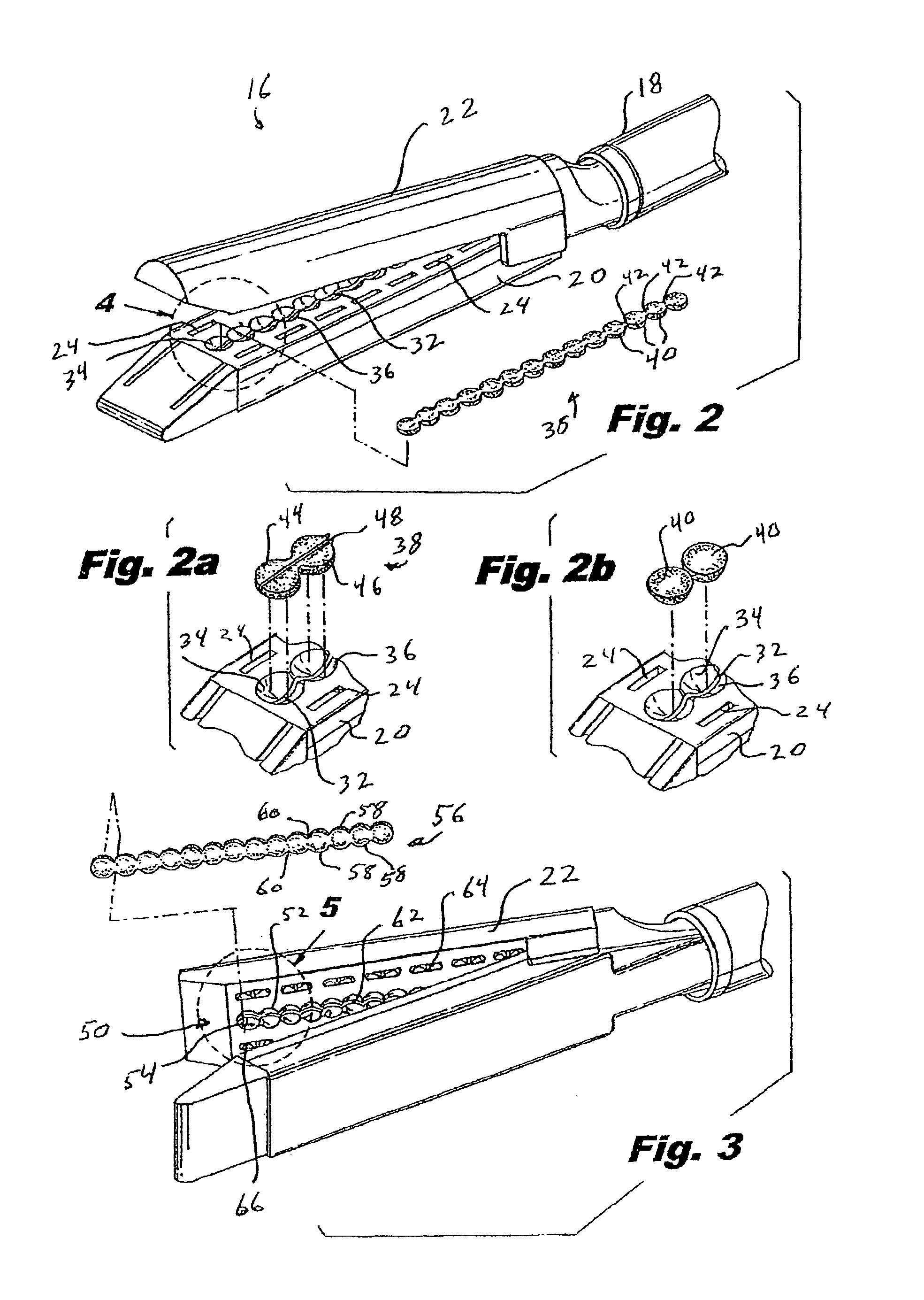
Materials delivery system for stapling device
There is disclosed a materials delivery system for use with a surgical stapling instrument having at least one jaw including a knife slot. The materials delivery system includes a series of treatment material receiving pockets positioned adjacent the knife slot such that a portion of each pocket is open to the knife slot. A source of treatment material is positioned within the pockets such that passage of the knife blade adjacent to the pockets repeatedly coats the knife blade with the treatment material.
Owner:COVIDIEN LP
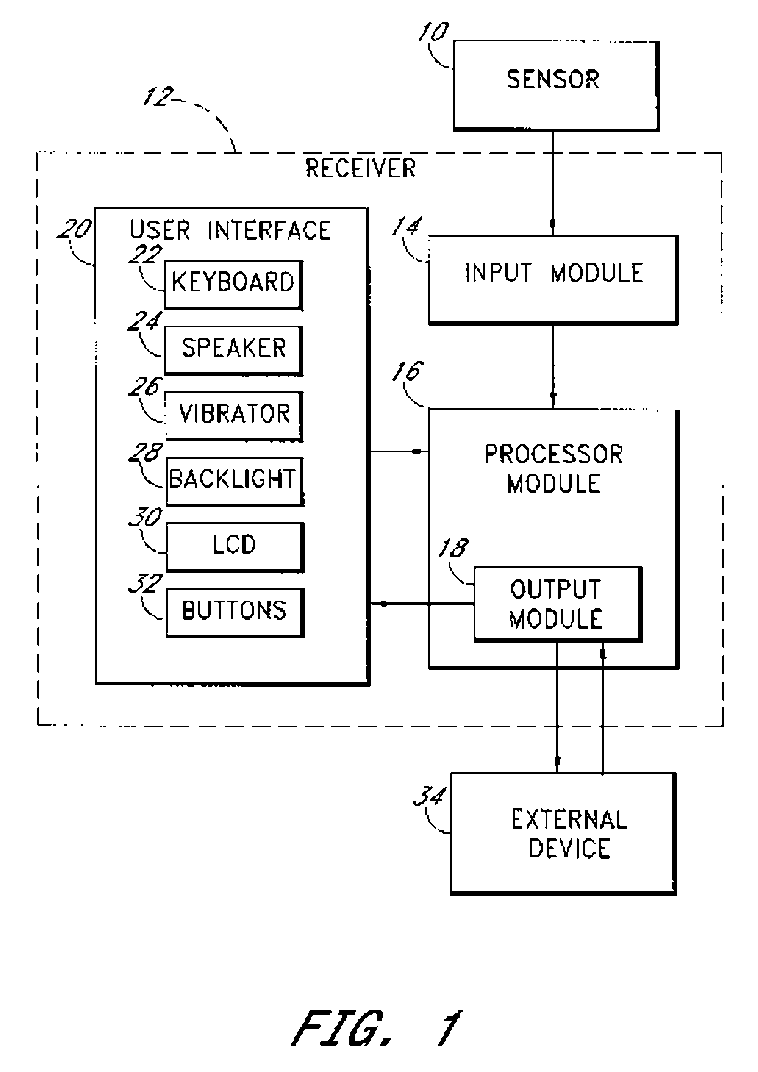
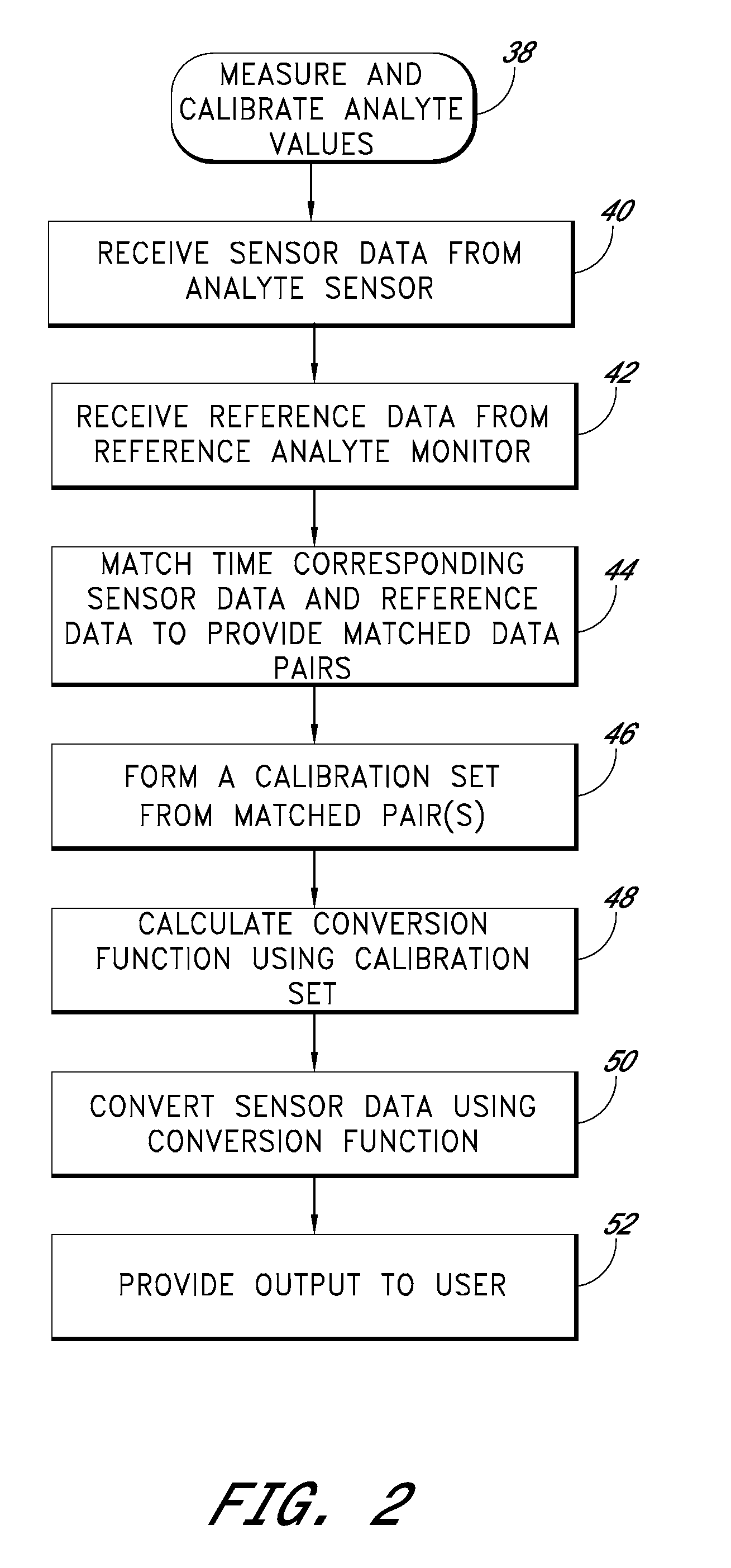
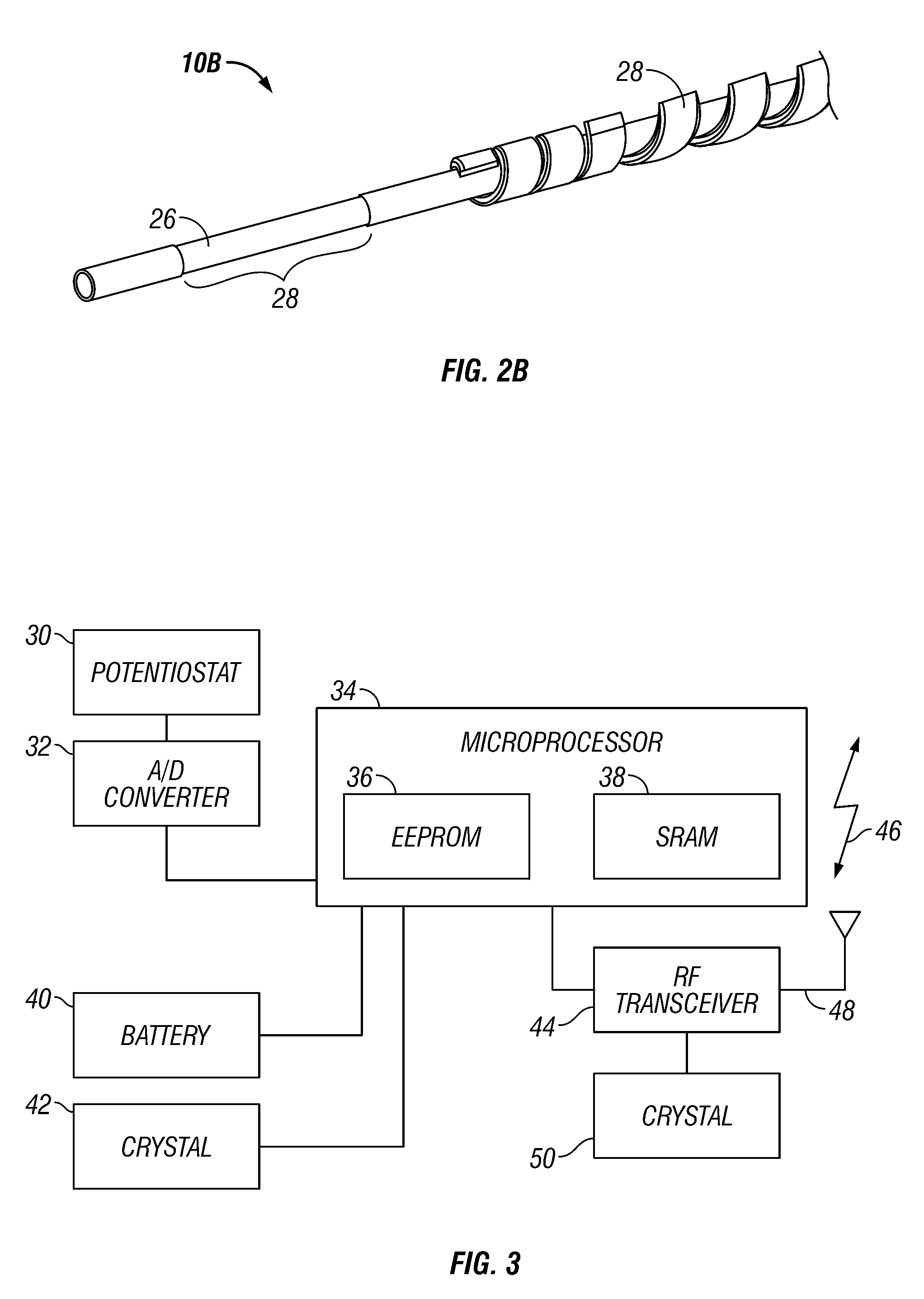
Signal processing for continuous analyte sensor
Abstract of the DisclosureSystems and methods for dynamically and intelligently estimating analyte data from a continuous analyte sensor, including receiving a data stream, selecting one of a plurality of algorithms, and employing the selected algorithm to estimate analyte values. Additional data processing includes evaluating the selected estimative algorithms, analyzing a variation of the estimated analyte values based on statistical, clinical, or physiological parameters, comparing the estimated analyte values with corresponding measure analyte values, and providing output to a user. Estimation can be used to compensate for time lag, match sensor data with corresponding reference data, warn of upcoming clinical risk, replace erroneous sensor data signals, and provide more timely analyte information encourage proactive behavior and preempt clinical risk.
Owner:DEXCOM
Medicament dispensing device with a display indicative of the state of an internal medicament reservoir
ActiveUS7331340B2Liquid surface applicatorsPowdered material dispensingDisplay deviceBiomedical engineering
A metered dose inhaler for use with a removable pressurized aerosol canister, or reservoir, having a display for indicating to a user the state of the canister. A memory device on the canister or a housing which houses the canister stores information indicative of doses dispensed from, or remaining in, the canister. That information is processed to provide and display information representative of the state of the canister.
Owner:IVAX CORP
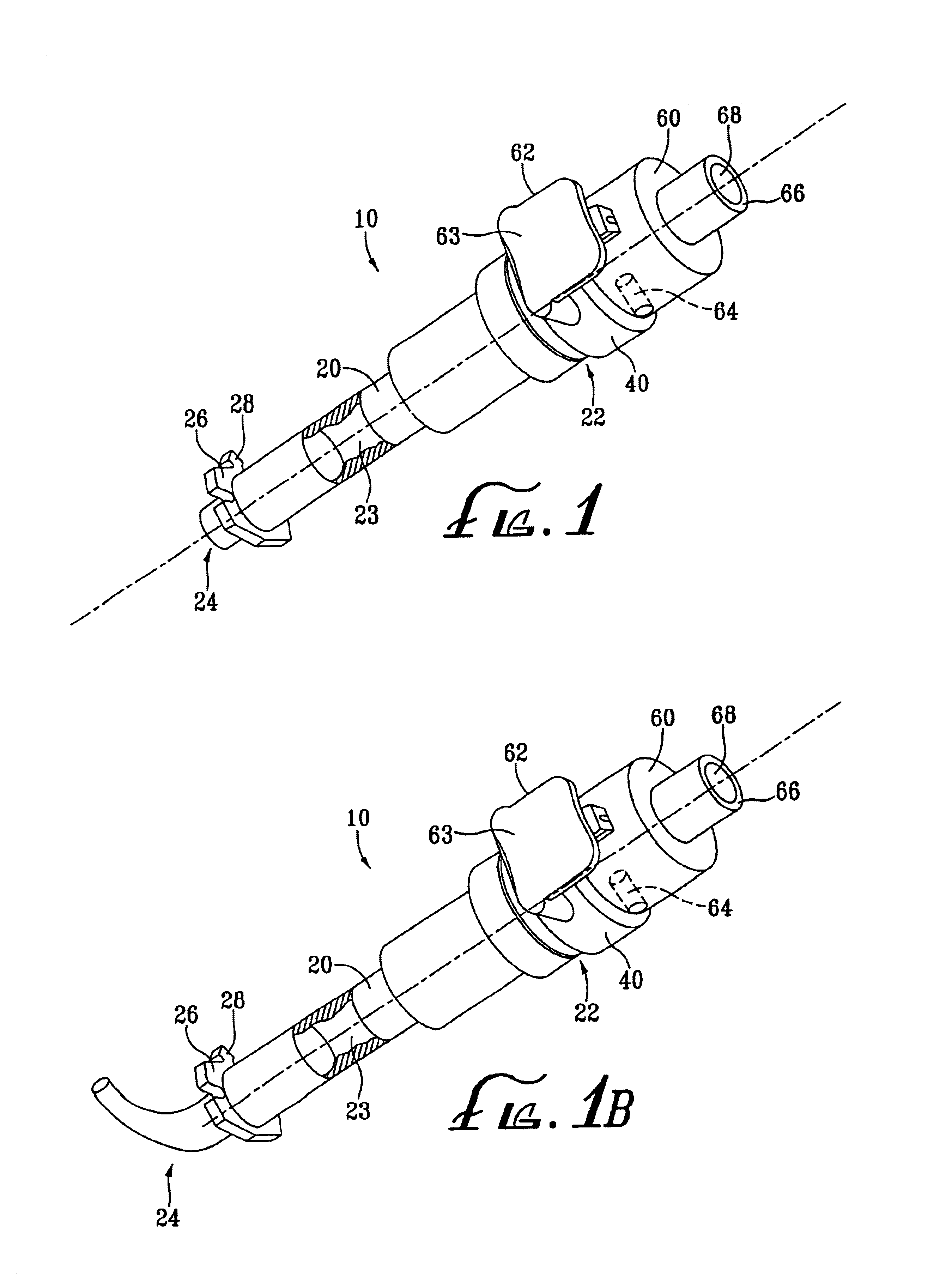
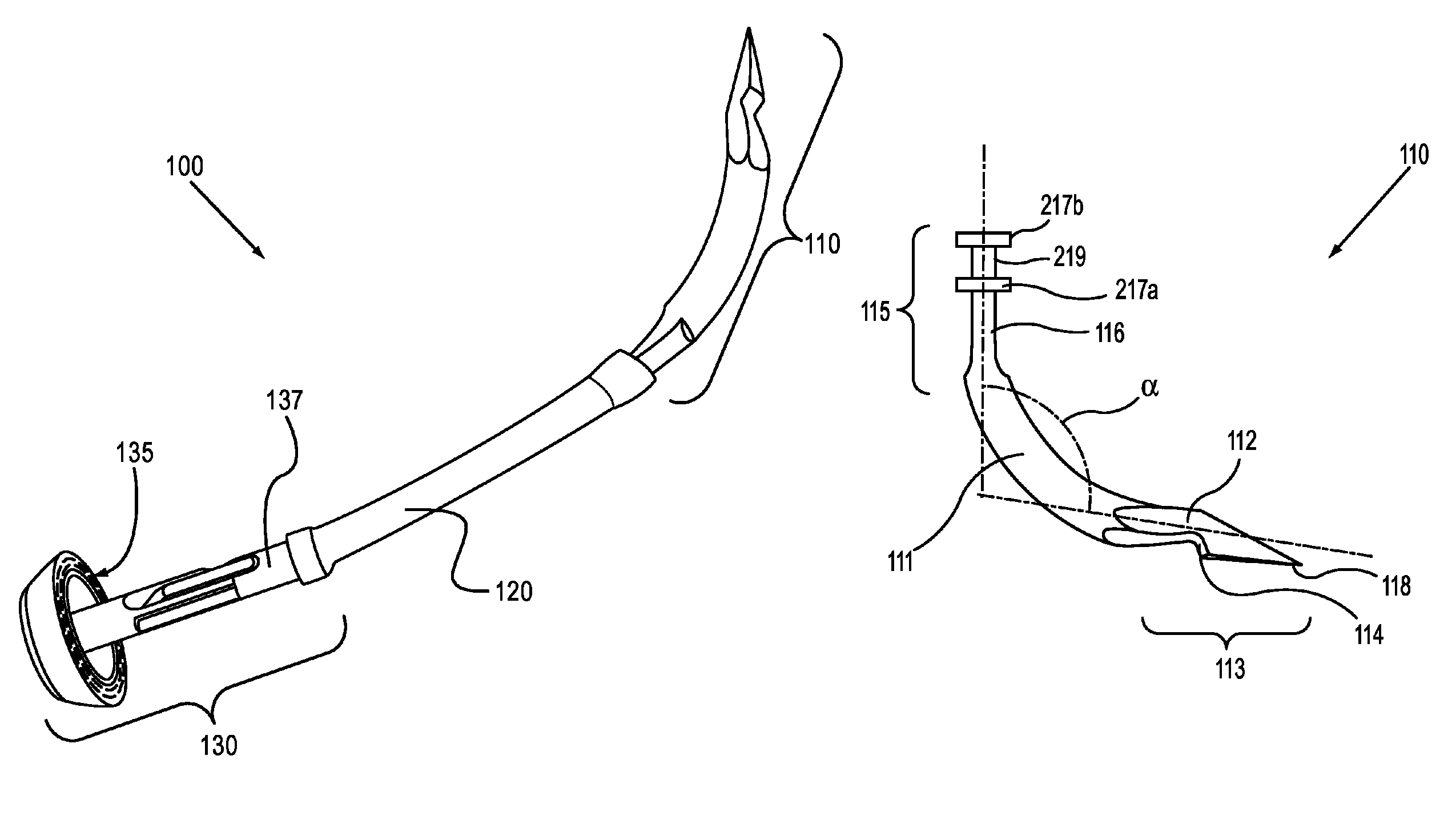
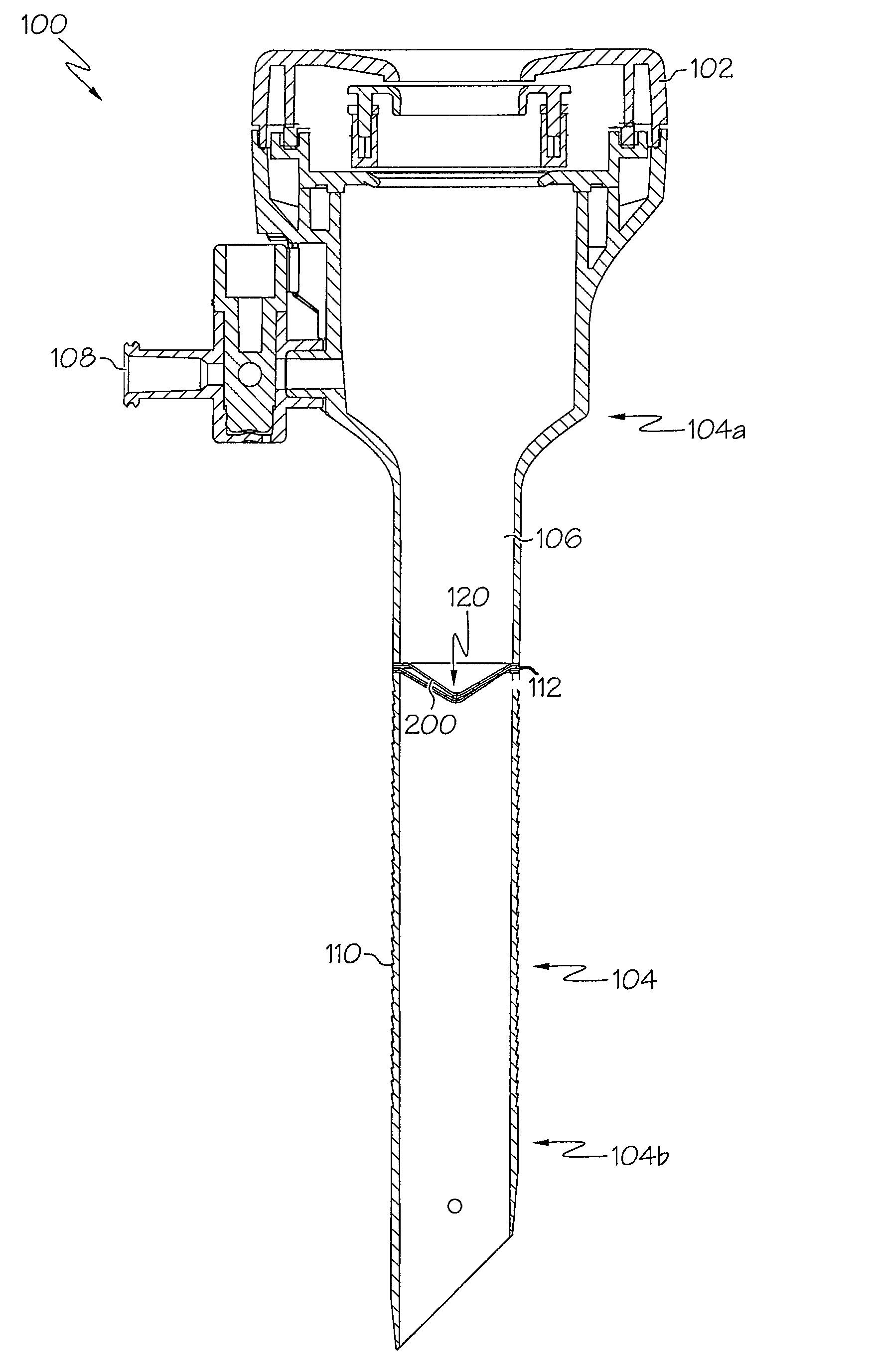
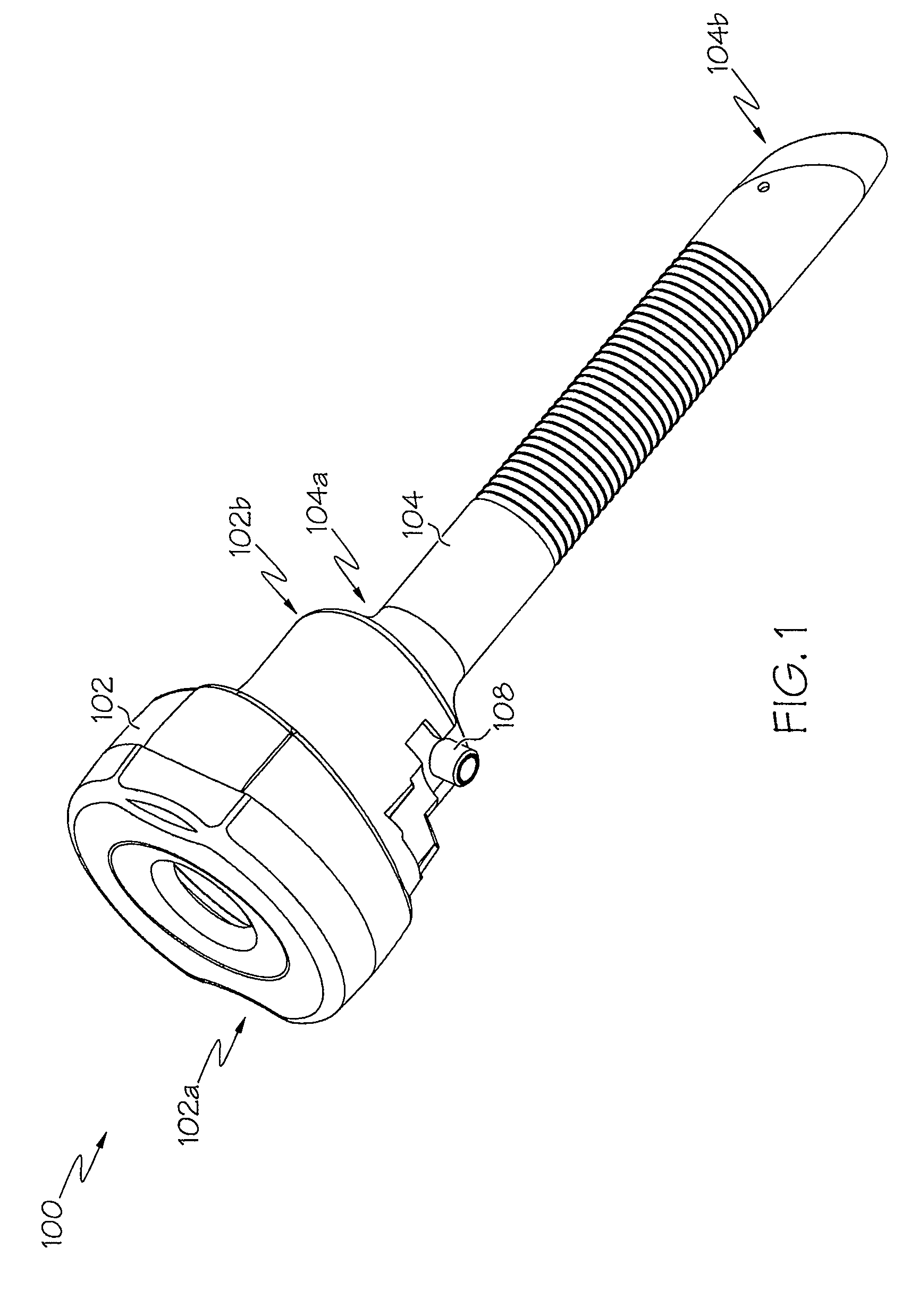
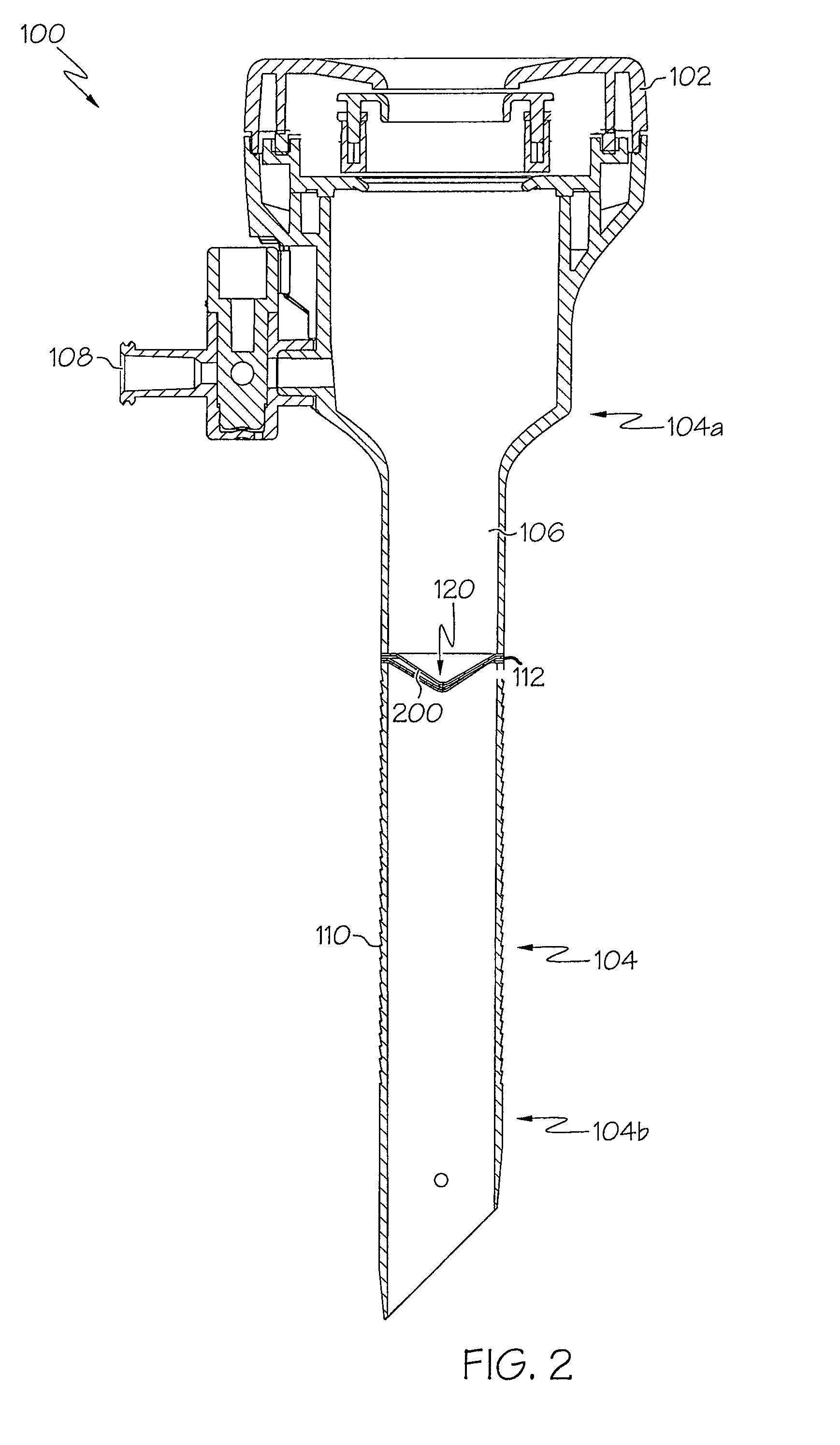
Medical device introducer and obturator
An introducer having an elongate tubular member and a device connector releasably attached to a proximal end of the tubular member. The introducer allows exchange of medical instruments, such as a blood filter and cardioplegia catheter, through a single lumen. An obturator having a retractable blade for making incision on a tissue is insertable through the lumen of the introducer. Methods of using the obturator and the introducer for introducing medical device(s) into body cavity, such as a vessel or cardiac tissue, are also disclosed.
Owner:EDWARDS LIFESCIENCES CORP
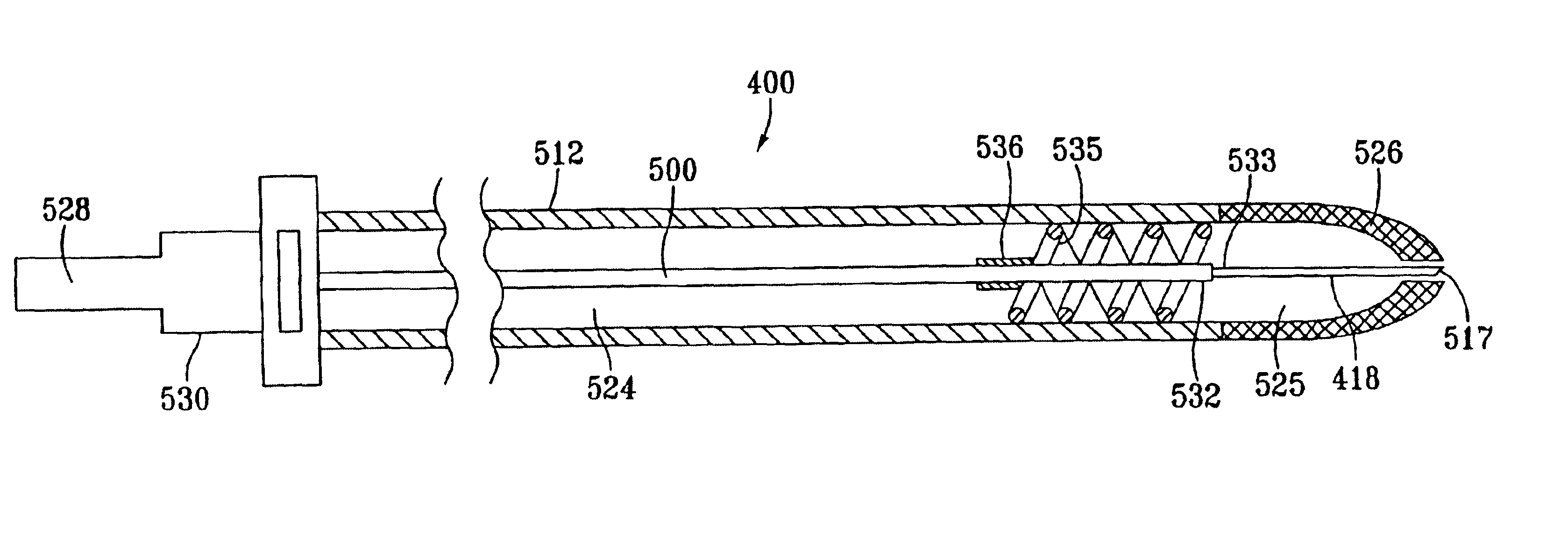
Low advance ratio, high reciprocation rate tissue removal device
Disclosed is a tissue removal device having an outer tube with a resection window and an inner tube disposed within the outer tube. The inner tube is slidable and rotatable relative to the outer tube so that the distal end of the inner tube moves back and forth across the resection window to sever tissue extending therethrough. The inner tube may be driven to rotate at a speed of at least about 1100 rpm, to axially translate at a rate of at least about 1.5 cps, and with an advance ratio of no more than about 0.25. The drive system for controlling axial reciprocation and rotation of the inner tube may be totally mechanical.
Owner:HOLOGIC INC
Vacuum assisted wound dressing
ActiveUS8715256B2Small and lightImprove portabilityPlastersAdhesive dressingsTopical Negative-Pressure TherapyVacuum assisted
Owner:SMITH & NEPHEW PLC
External mixer assembly
An external mixer assembly is provided which externally mixes and delivers a first and a second component of a biological adhesive to tissues or organs for sealing wounds, stopping bleeding and the like. The first and second components are mixed immediately after exiting from separate outlet ports disposed in fluid communication with component reservoirs. In on embodiment, the external mixer assembly includes a housing having a housing head for enclosing therein a first reservoir containing the first component, and a second reservoir containing the second component. The housing further includes a discharge nozzle defining a longitudinal axis for enclosing therein a conduit assembly having a first and a second conduit in communication with the first and second reservoir, respectively. A deflector assembly is connected to the discharge nozzle. The deflector assembly includes a deflector plate to provide a space for initial mixing of the first and second components. The deflector plate is oriented in generally parallel juxtaposed relation distal to the distal face of the discharge nozzle. The first and second components are preferably fibrinogen and thrombin which intermix to form a fibrin sealant.
Owner:TYCO HEALTHCARE GRP LP
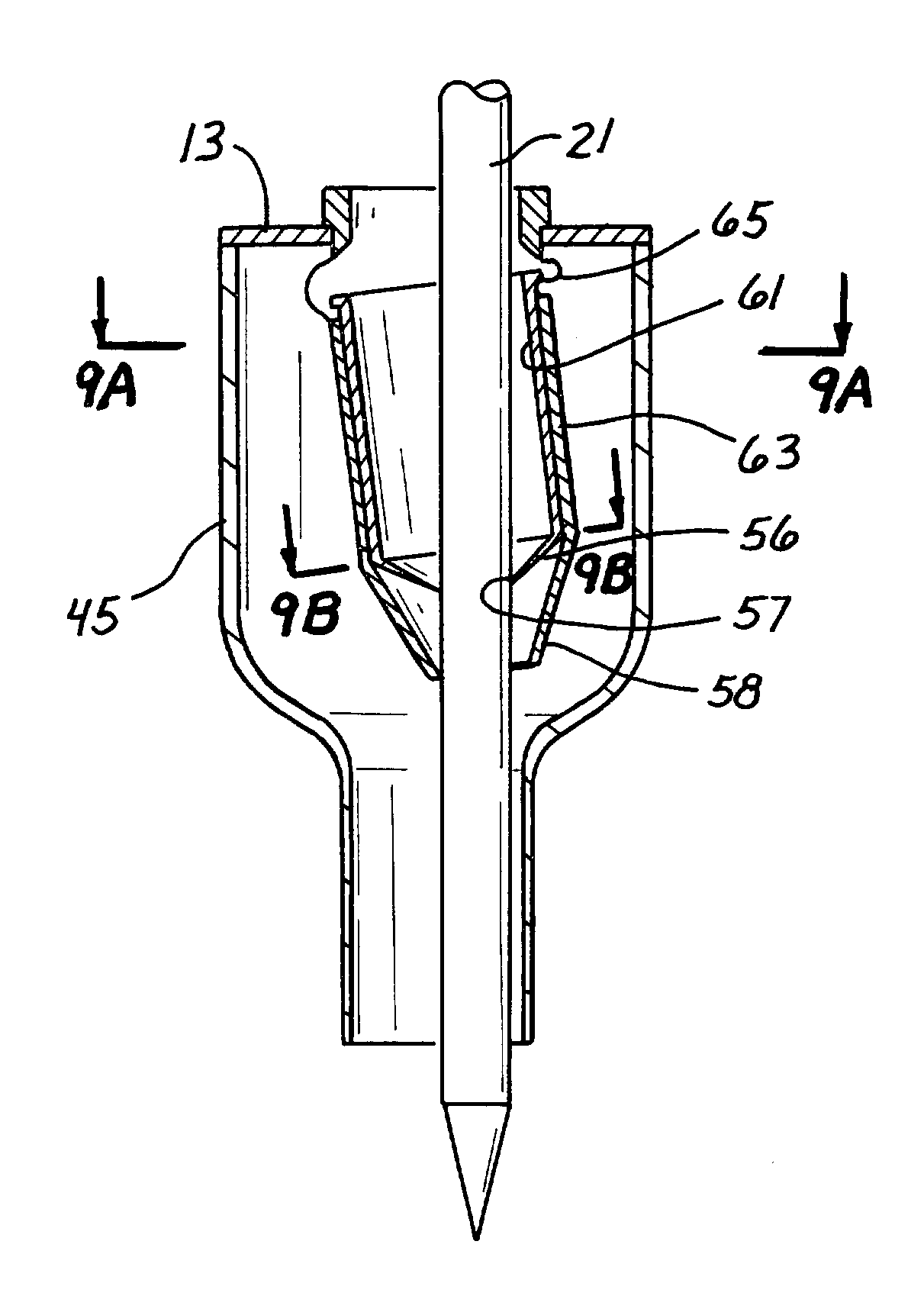
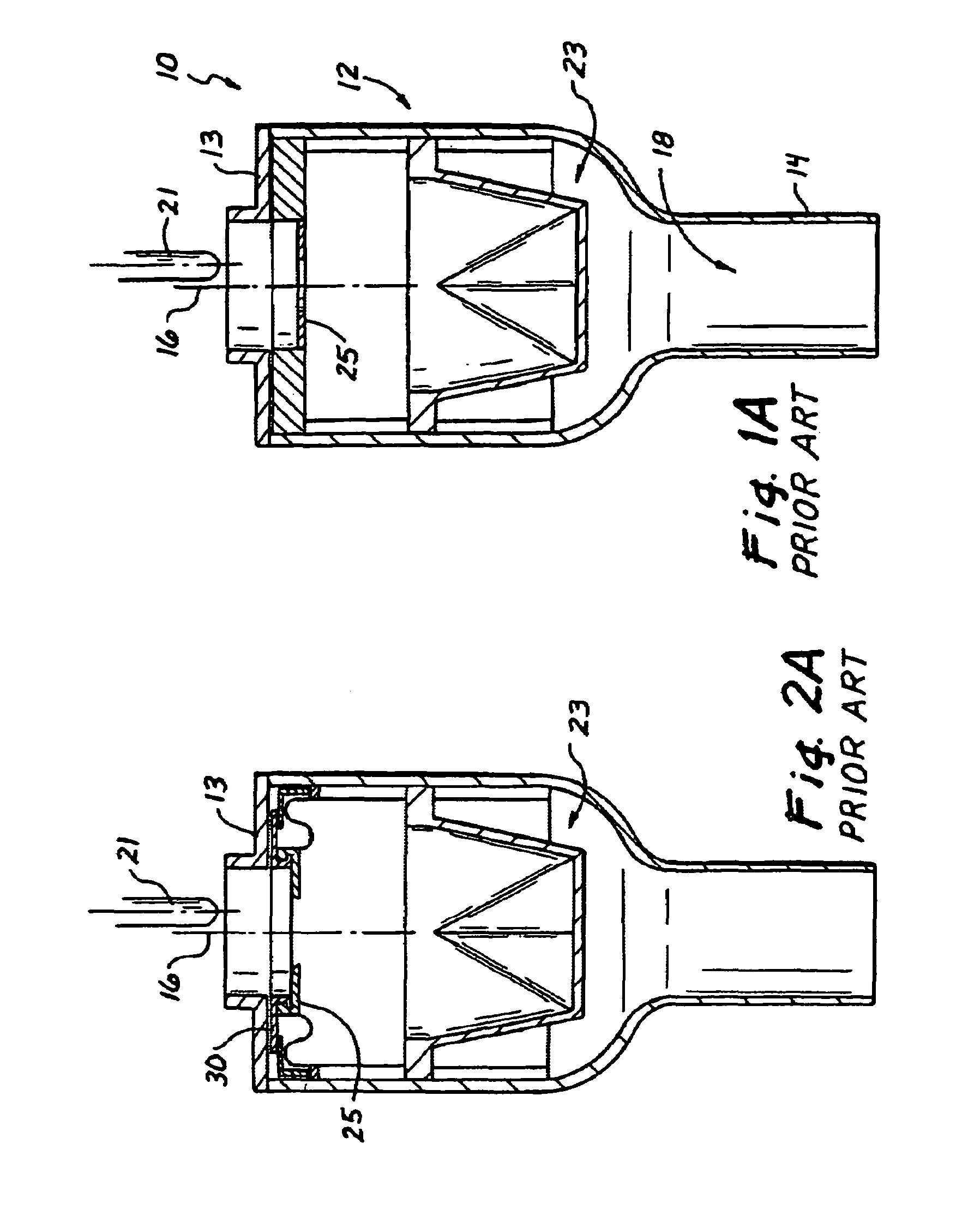
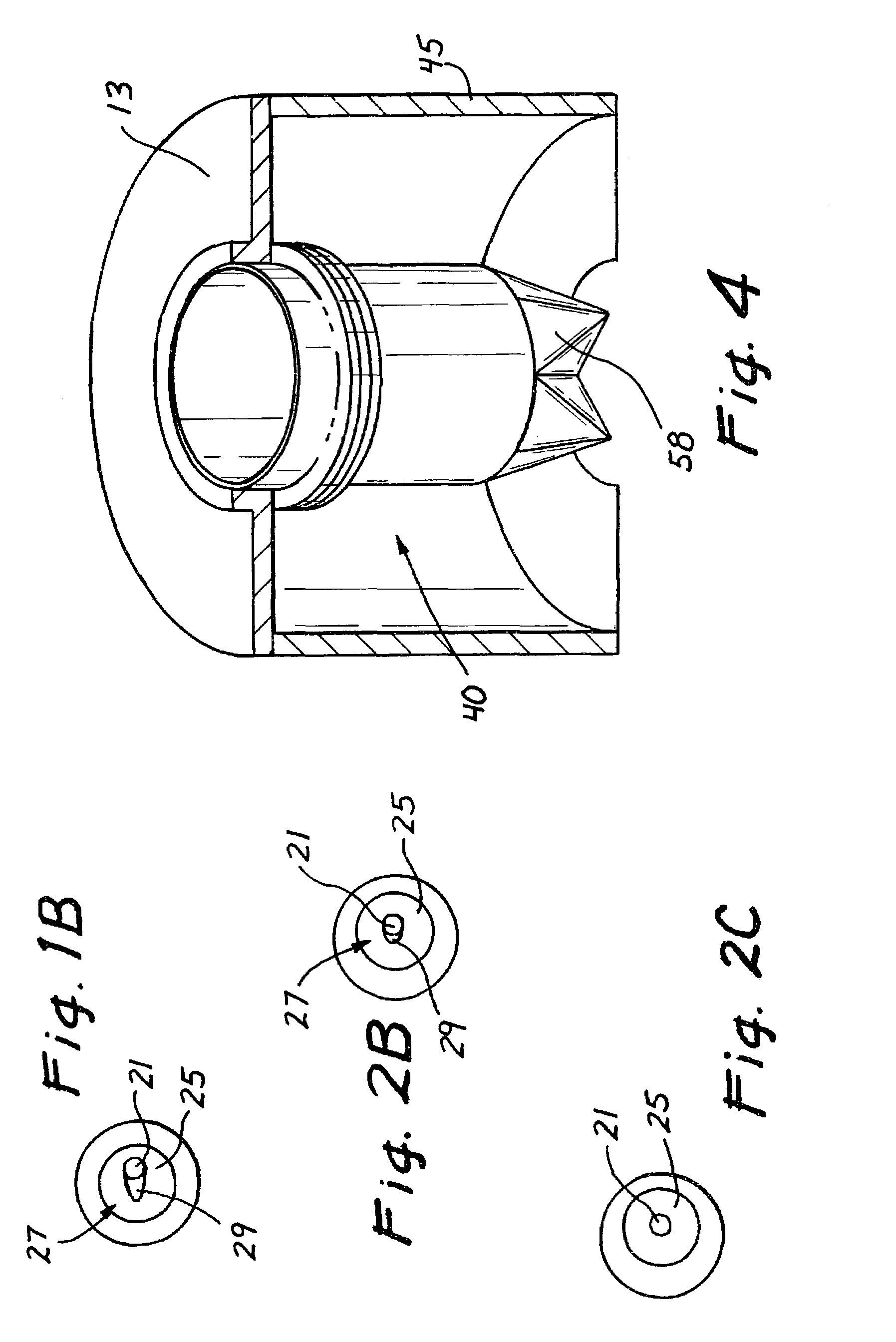
Surgical access device with pendent valve
InactiveUS7083626B2Precise positioningMaximize ease and safetyEar treatmentCannulasSurgical departmentVALVE PORT
A surgical access device, such as a trocar, includes a pendent valve having an elongate structure extending from a proximal end to a septum valve disposed at a distal end. In operation, the elongate structure follows the angle of the instrument to pre-position the septum valve into the path of the instrument where it is not significantly challenged during instrument insertion or manipulation. The pendant valve can be made to float at both the proximal end and the distal end of the elongate structure, to further reduce the vulnerability of the septum valve. Since the valve is less vulnerable to instrument insertion, it can be formed to minimize friction and maximize the functional range of the access device.
Owner:APPL MEDICAL RESOURCES CORP
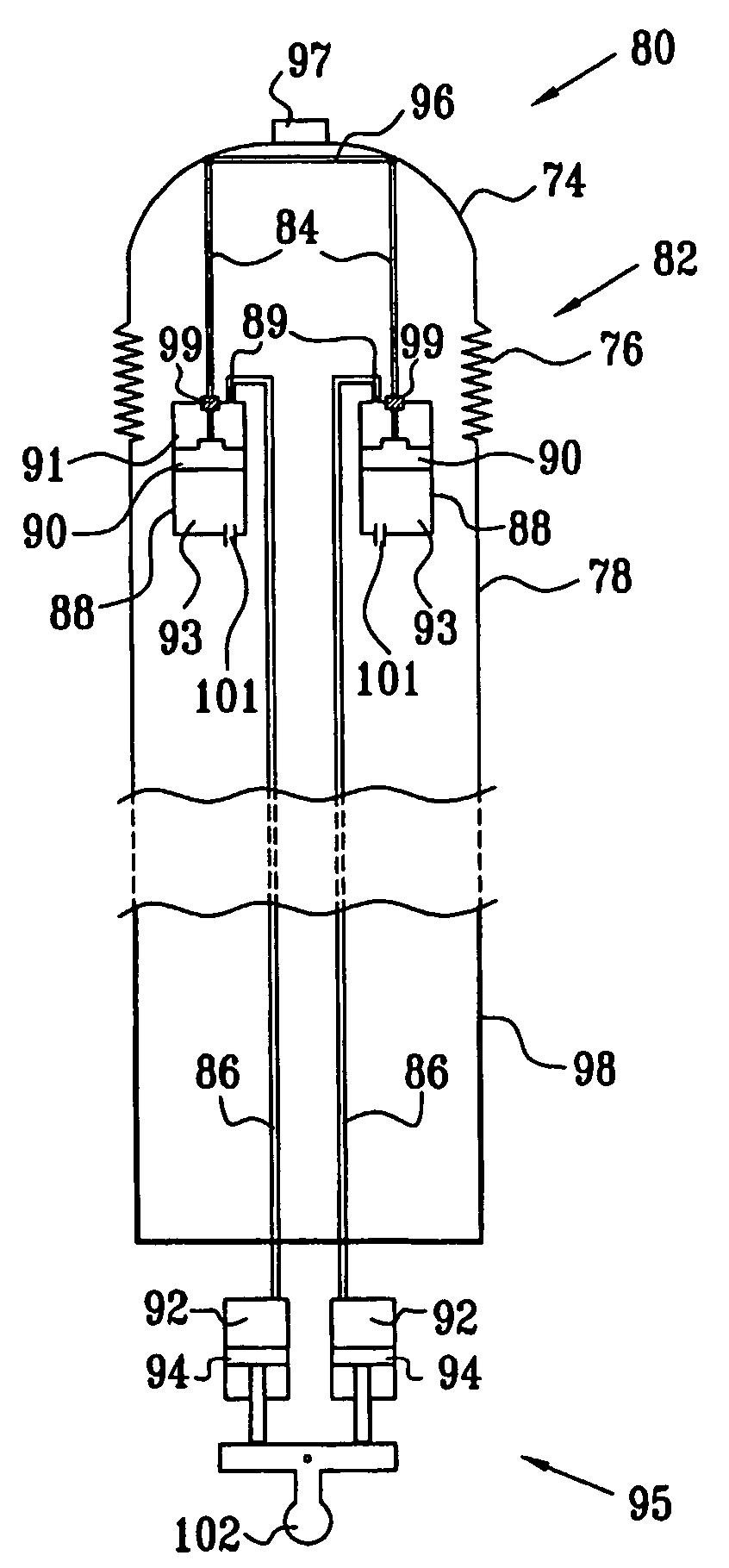
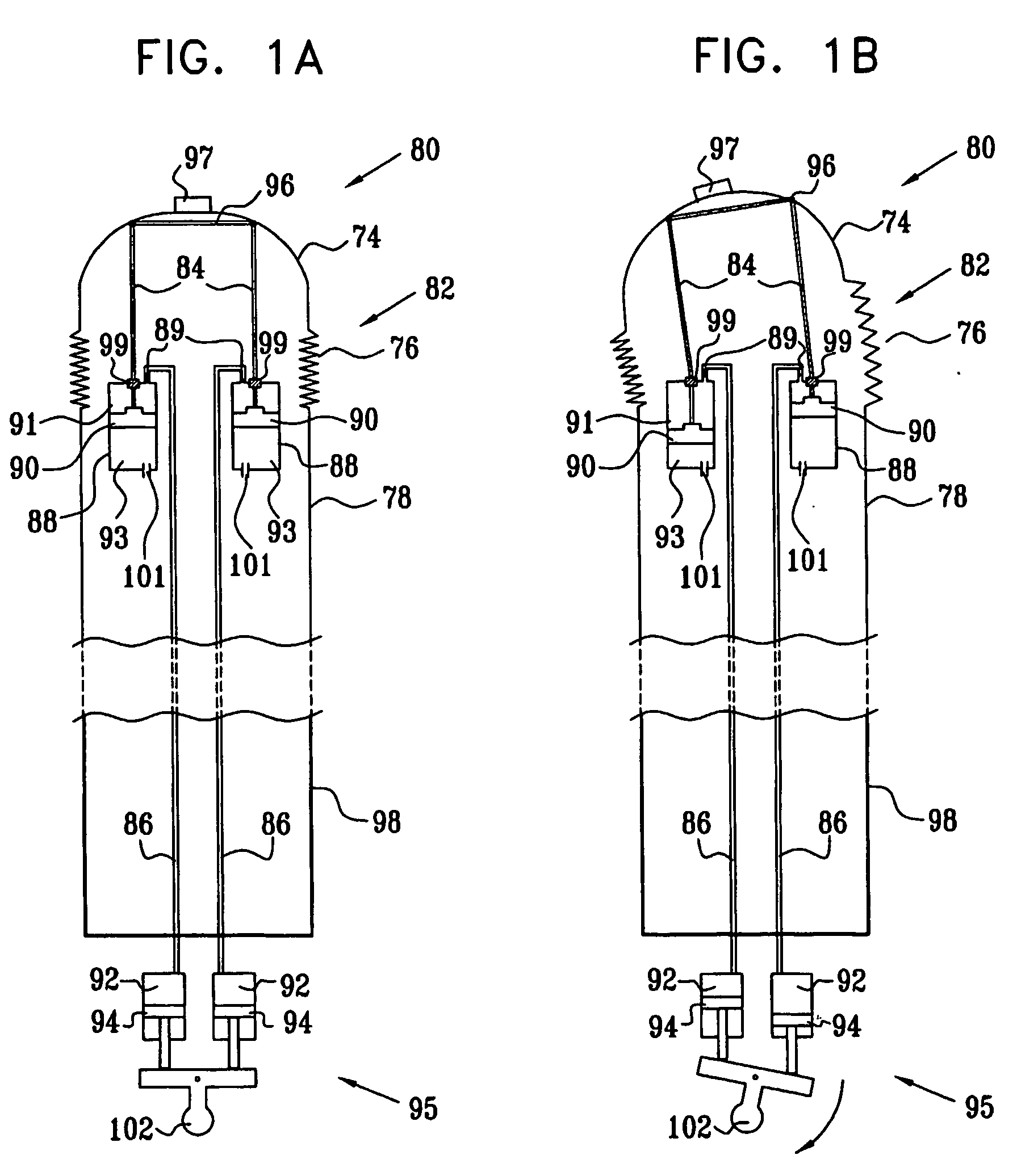
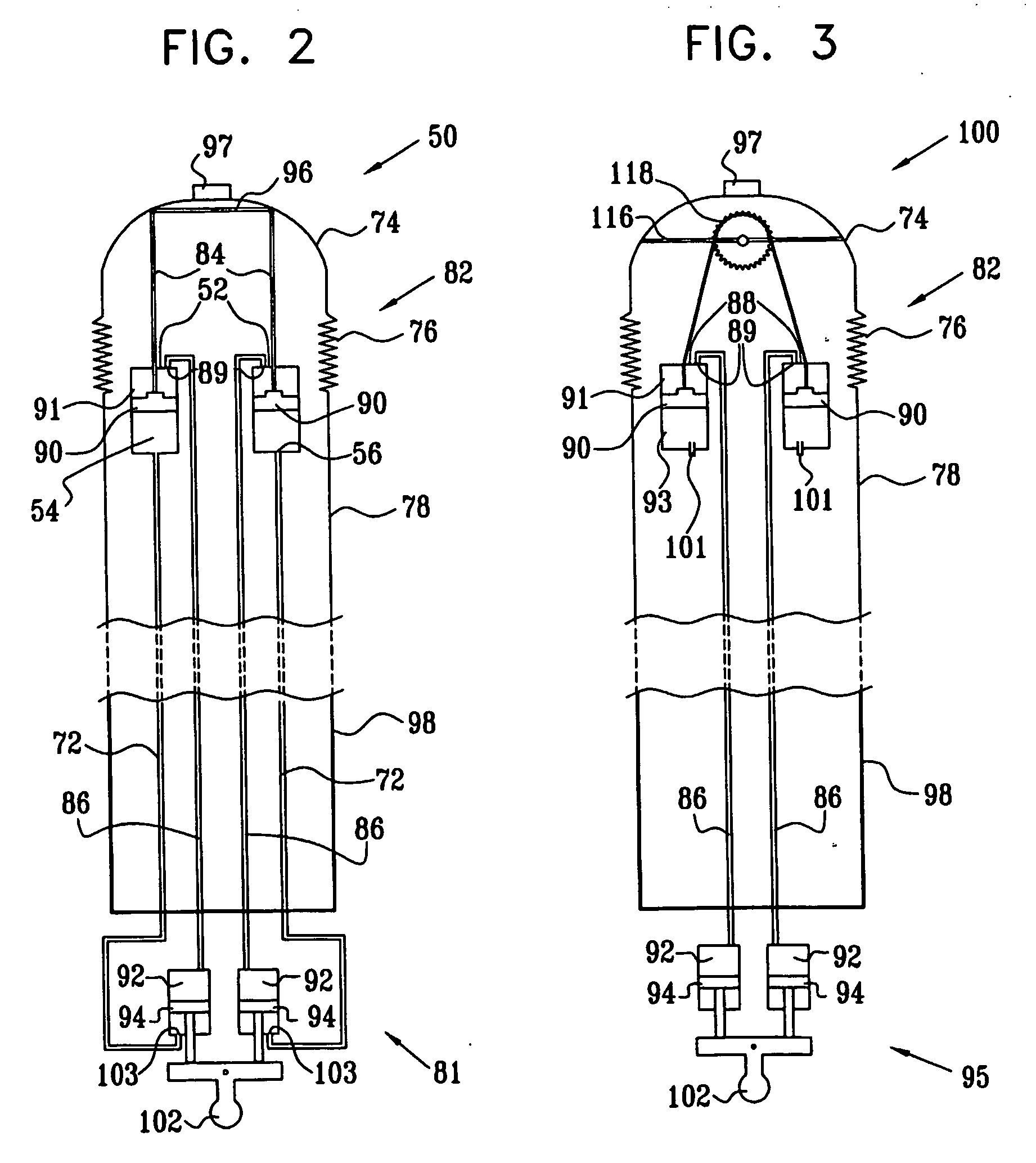
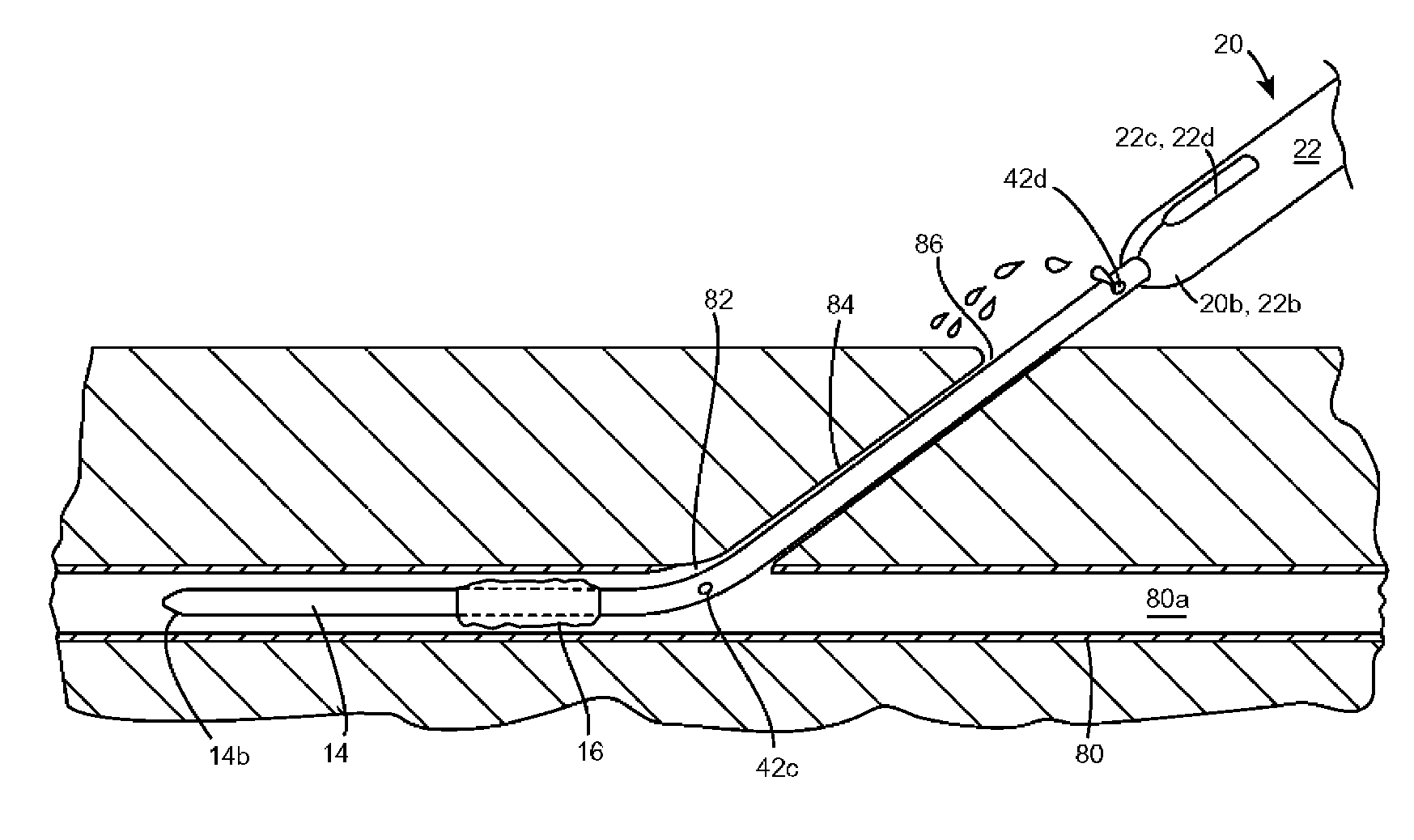
Piston-actuated endoscopic steering system
Endoscopic steering apparatus is provided, including an endoscope (80) having distal (82) and proximal (98) ends thereof. In a preferred embodiment, at least one proximal cylinder (92) is disposed in a vicinity of the proximal end of the endoscope, and at least one proximal piston (94) is slidably coupled to the at least one proximal cylinder. This piston is typically manually driven. A first distal cylinder (88) is disposed at the distal end of the endoscope, and a first distal piston (90) is slidably coupled to the first distal cylinder. A second distal cylinder (88) is disposed at the distal end of the endoscope, and a second distal piston (90) is slidably coupled to the second distal cylinder. A first tube (86) is coupled to the first distal cylinder and to the at least one proximal cylinder, and a second tube (86) is coupled to the second distal cylinder and to the at least one proximal cylinder. A linkage (96) is disposed at the distal end of the endoscope and coupled to the first distal piston and to the second distal piston, such that displacement of at least one of the distal pistons causes displacement of the linkage and steering of the distal end of the endoscope.
Owner:STRYKER GI
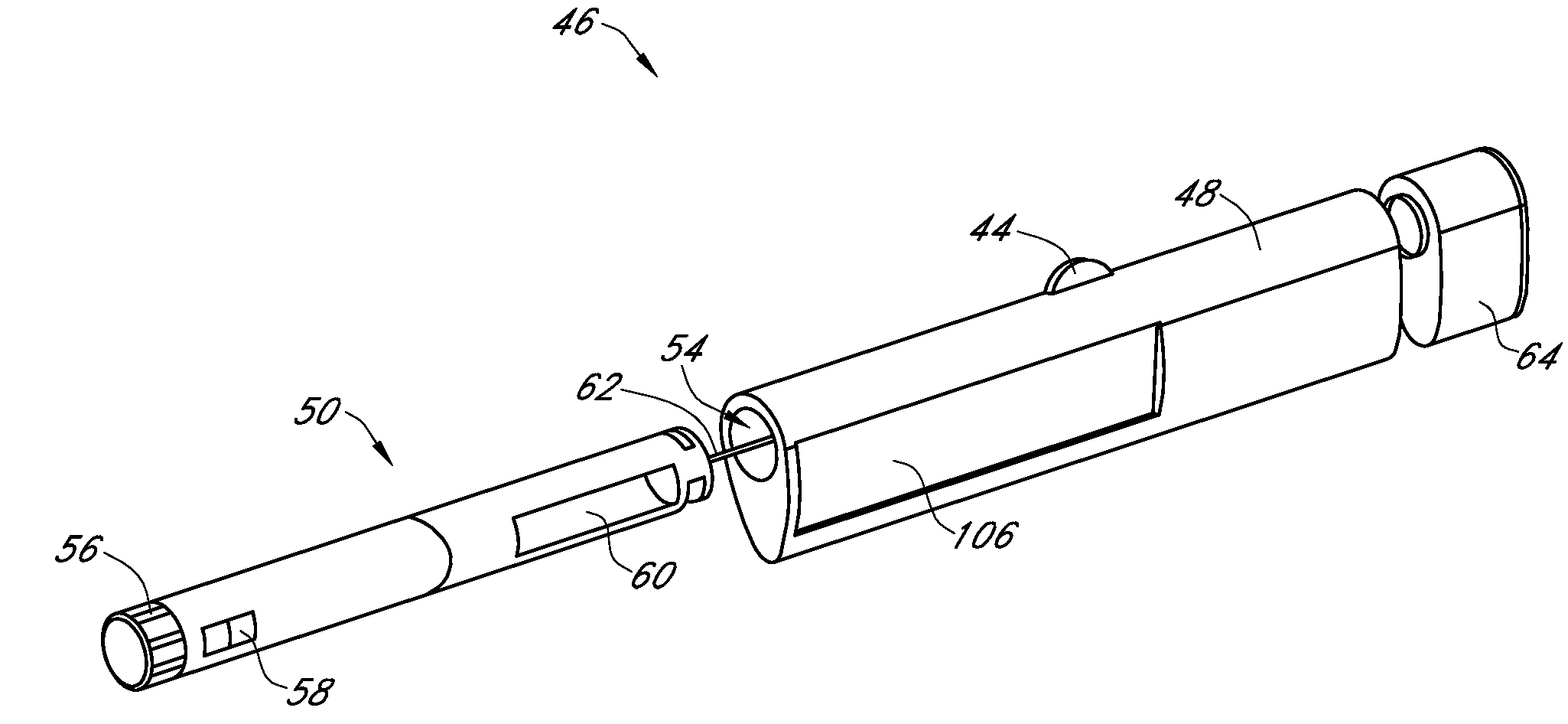
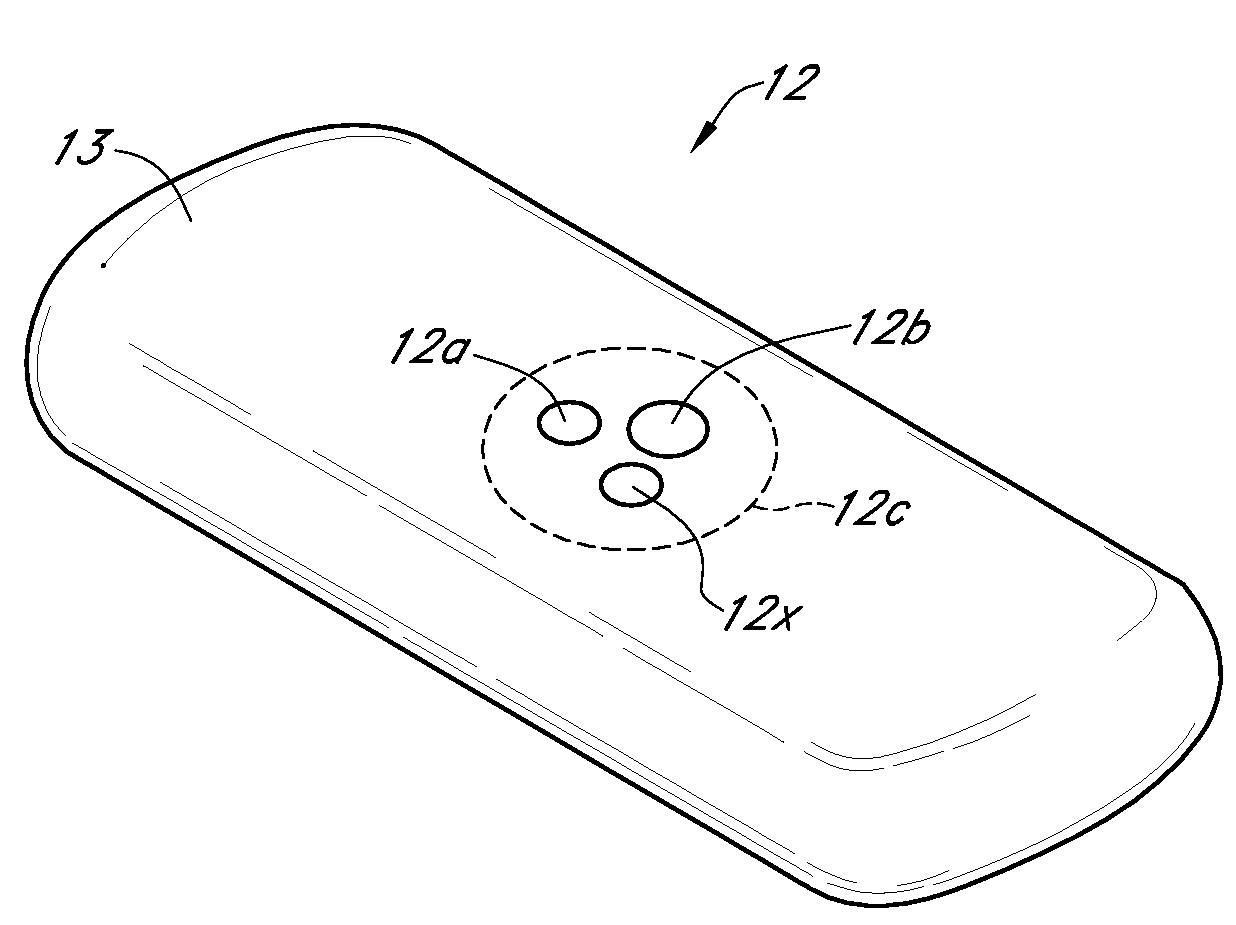
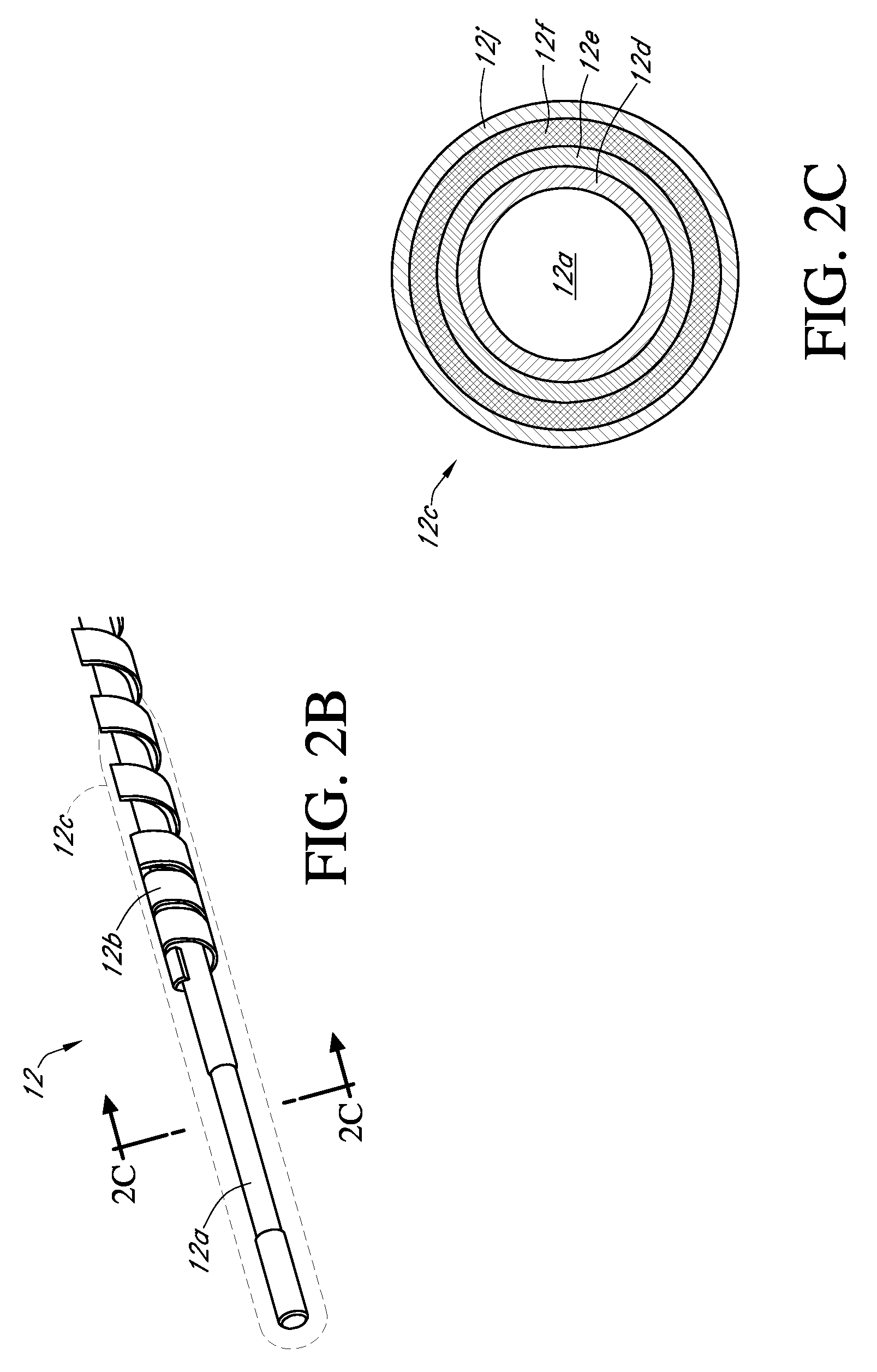
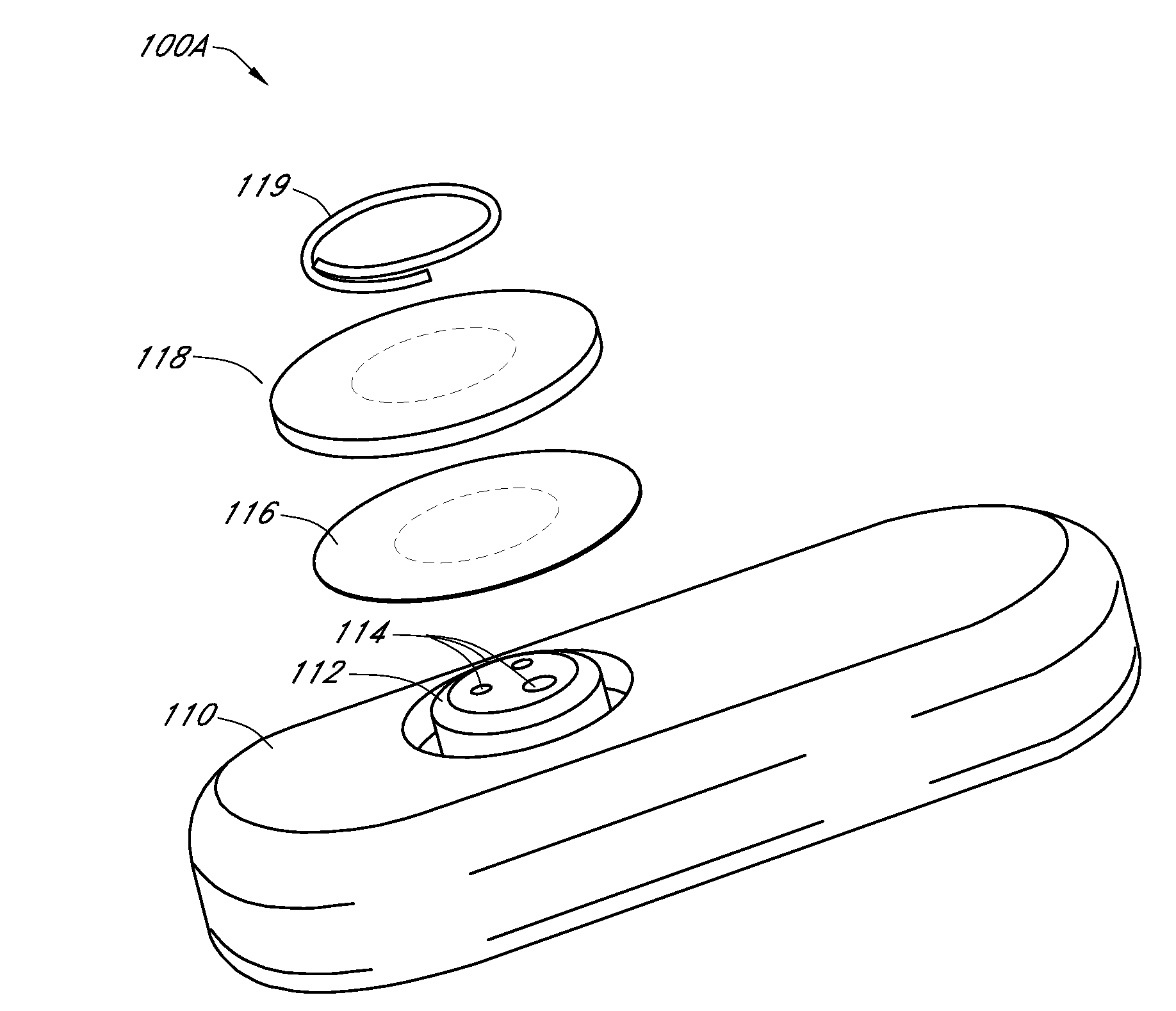
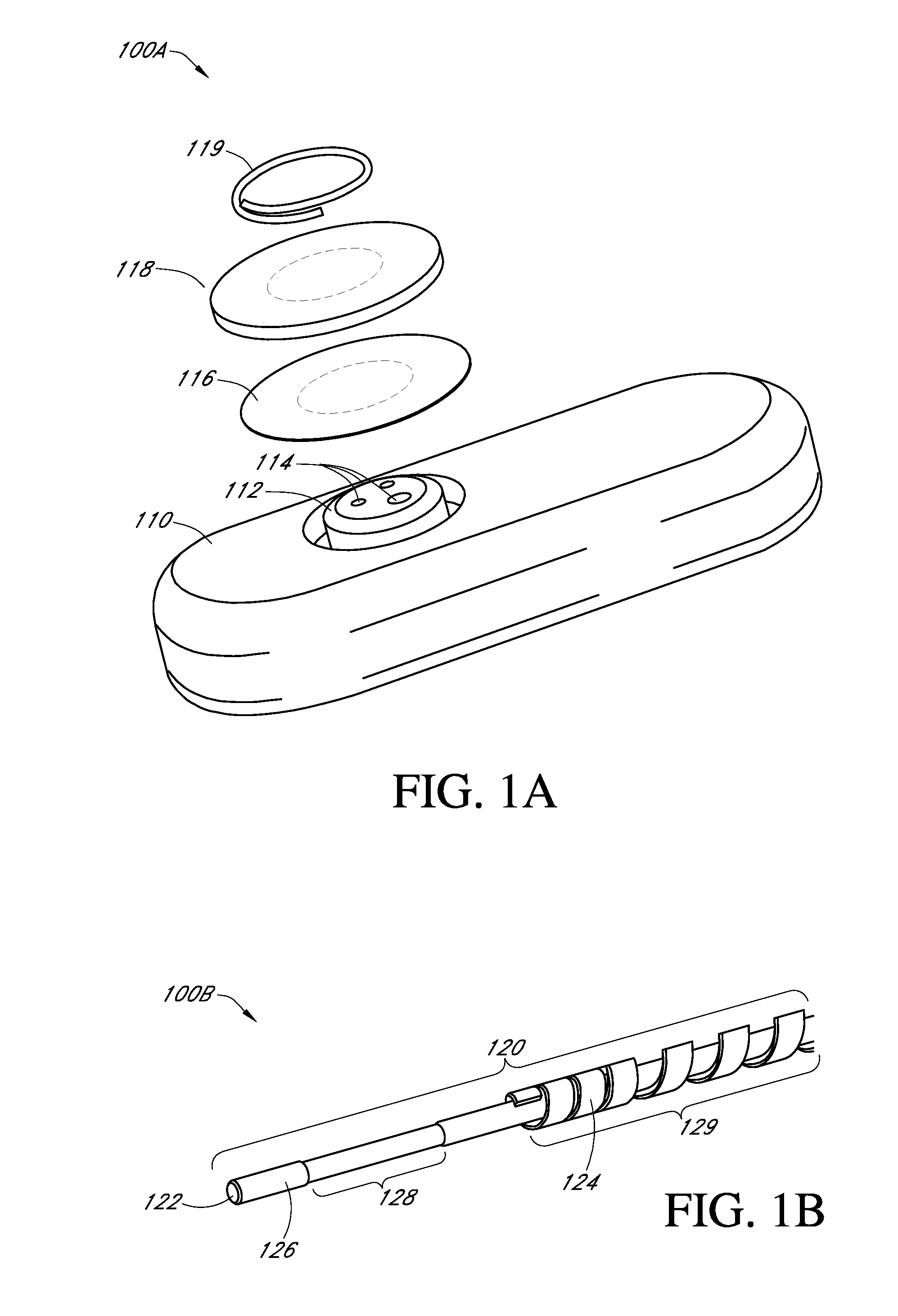
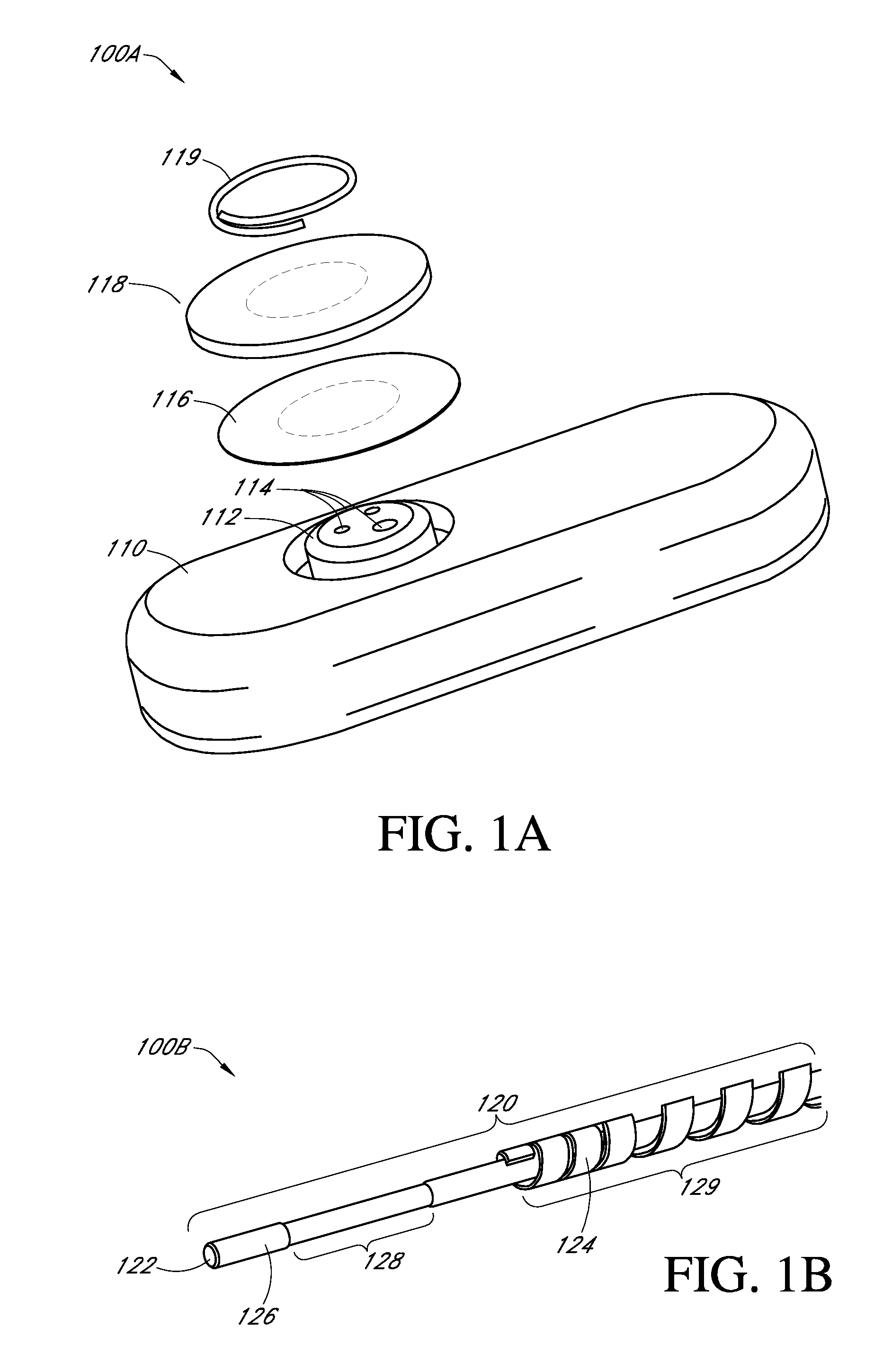
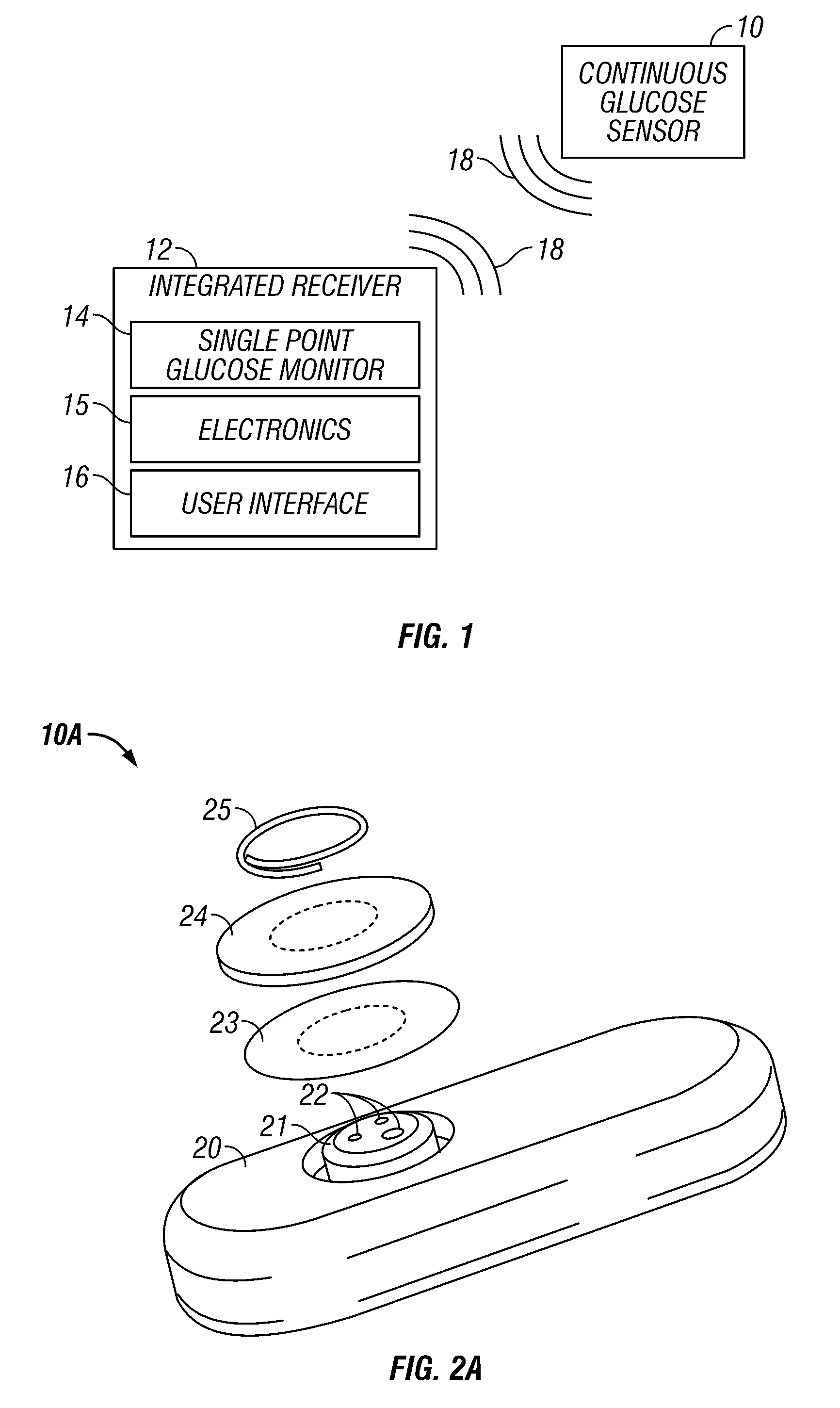
Integrated medicament delivery device for use with continuous analyte sensor
InactiveUS20080306434A1Reduce the burden onSimple processAmpoule syringes2D-image generationDiabetes mellitusMedication injection
An integrated system for the monitoring and treating diabetes is provided, including an integrated receiver / hand-held medicament injection pen, including electronics, for use with a continuous glucose sensor. In some embodiments, the receiver is configured to receive continuous glucose sensor data, to calculate a medicament therapy (e.g., via the integrated system electronics) and to automatically set a bolus dose of the integrated hand-held medicament injection pen, whereby the user can manually inject the bolus dose of medicament into the host. In some embodiments, the integrated receiver and hand-held medicament injection pen are integrally formed, while in other embodiments they are detachably connected and communicated via mutually engaging electrical contacts and / or via wireless communication.
Owner:DEXCOM
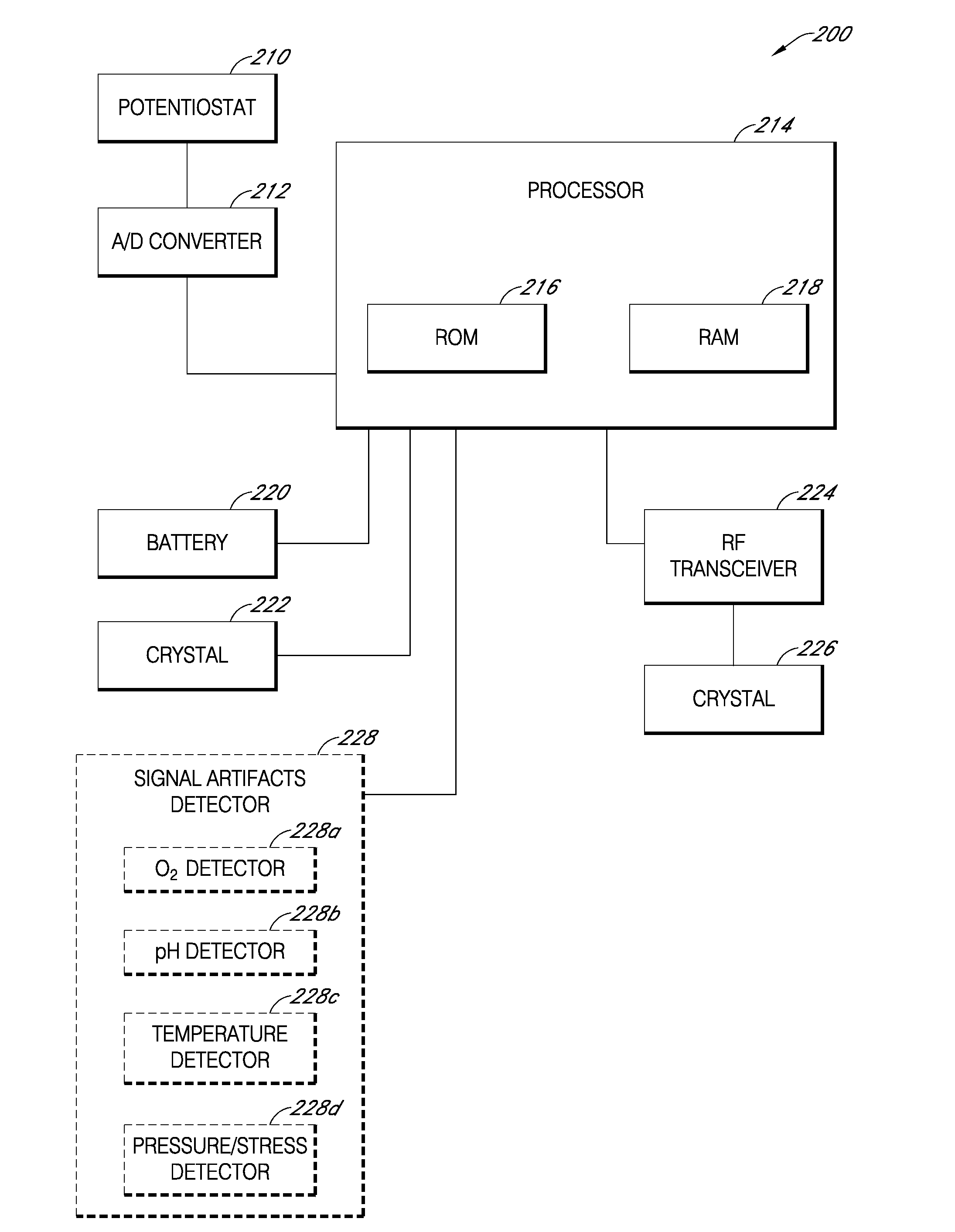
Signal processing for continuous analyte sensor
Systems and methods for dynamically and intelligently estimating analyte data from a continuous analyte sensor, including receiving a data stream, selecting one of a plurality of algorithms, and employing the selected algorithm to estimate analyte values. Additional data processing includes evaluating the selected estimative algorithms, analyzing a variation of the estimated analyte values based on statistical, clinical, or physiological parameters, comparing the estimated analyte values with corresponding measure analyte values, and providing output to a user. Estimation can be used to compensate for time lag, match sensor data with corresponding reference data, warn of upcoming clinical risk, replace erroneous sensor data signals, and provide more timely analyte information encourage proactive behavior and preempt clinical risk.
Owner:DEXCOM
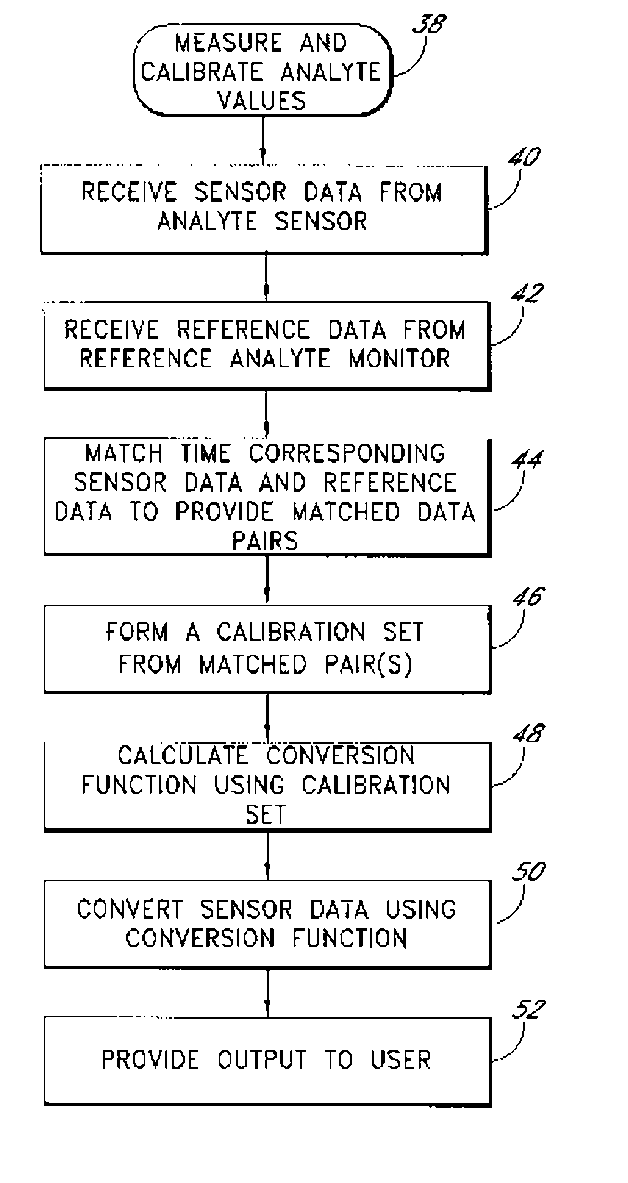
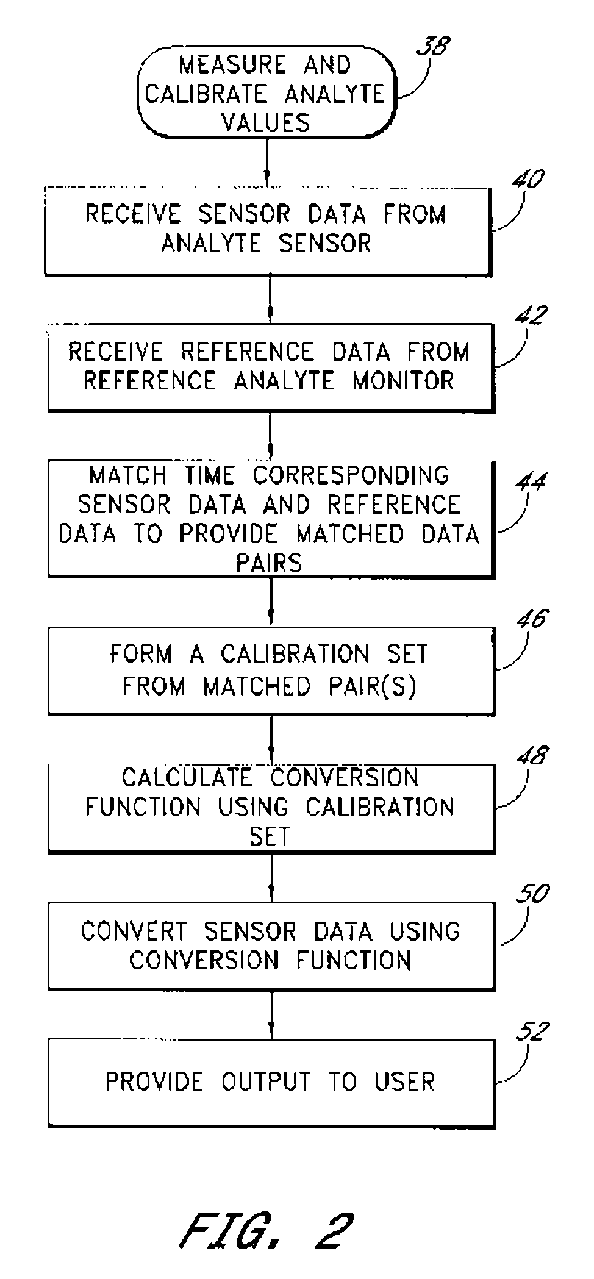
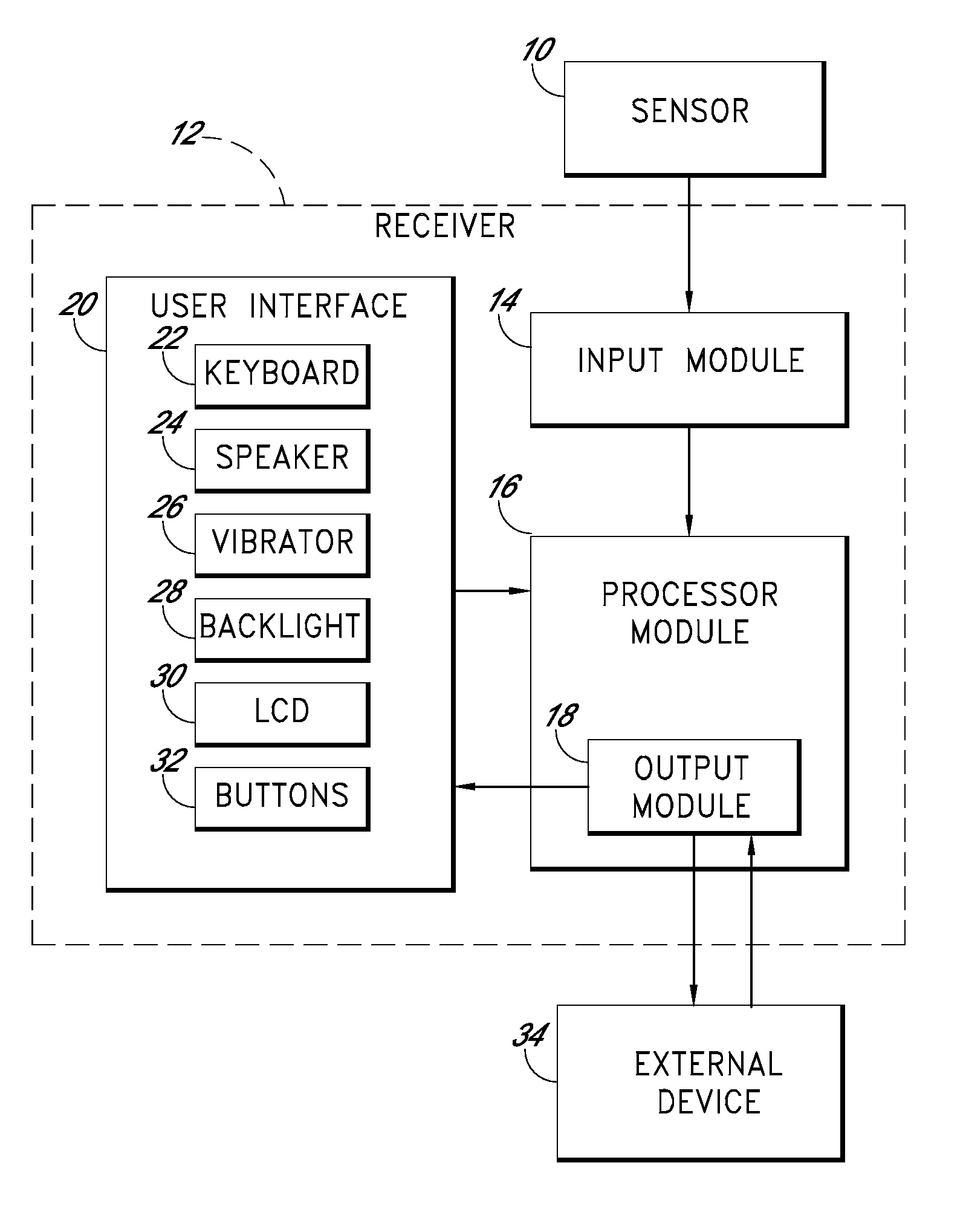
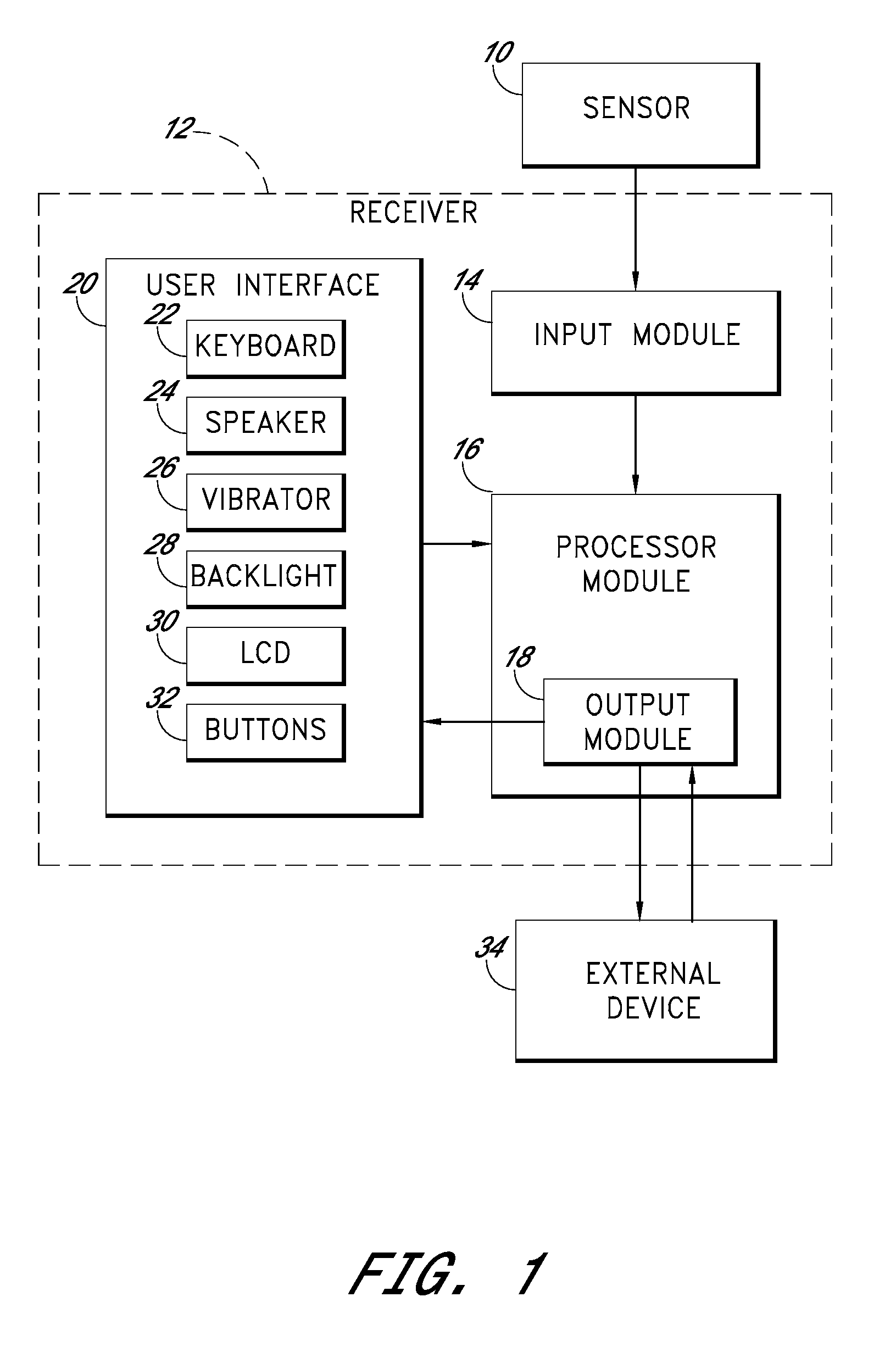
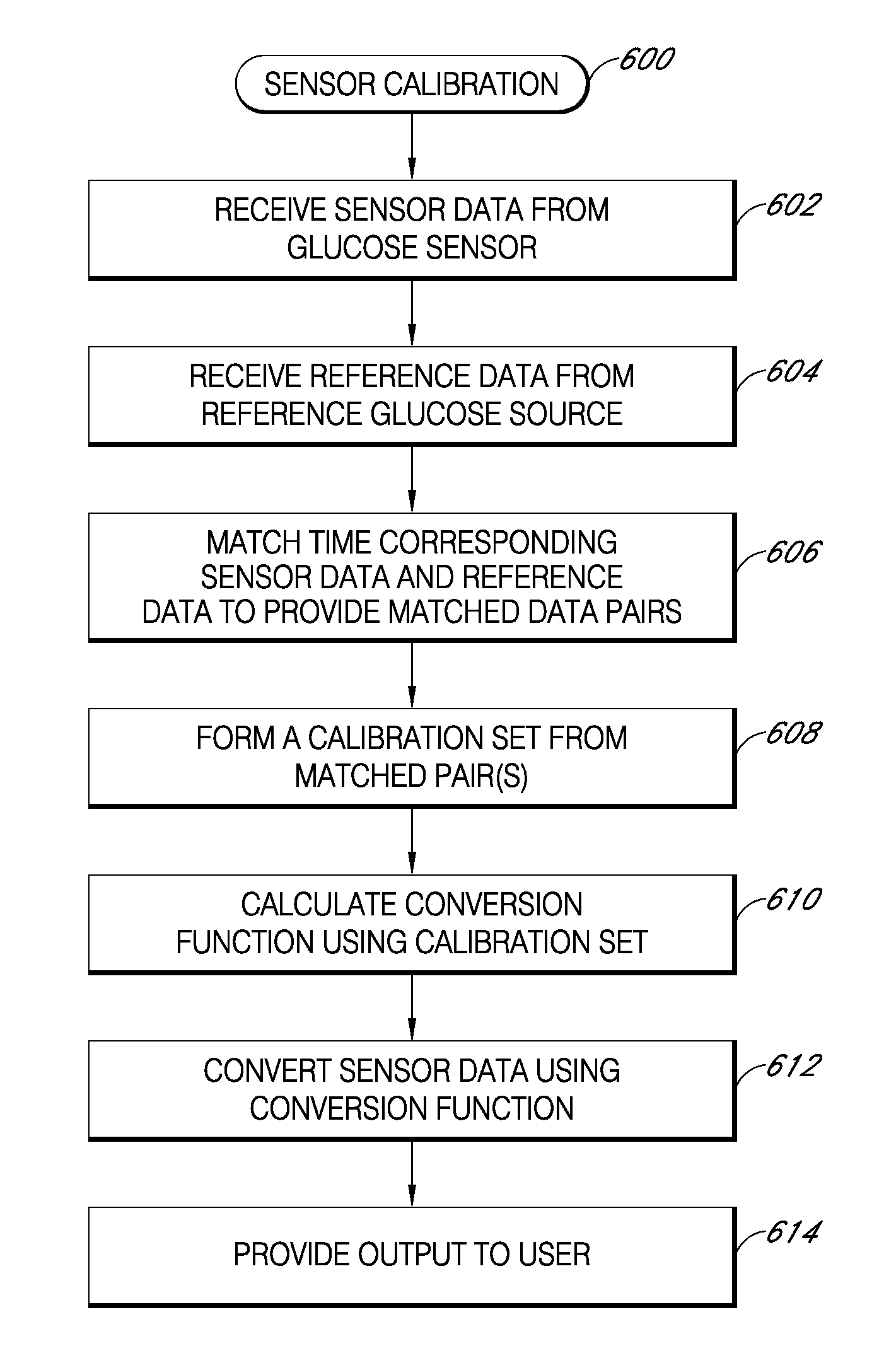
Systems and methods for processing sensor data
Systems and methods for processing sensor data are provided. In some embodiments, systems and methods are provided for calibration of a continuous analyte sensor. In some embodiments, systems and methods are provided for classification of a level of noise on a sensor signal. In some embodiments, systems and methods are provided for determining a rate of change for analyte concentration based on a continuous sensor signal. In some embodiments, systems and methods for alerting or alarming a patient based on prediction of glucose concentration are provided.
Owner:DEXCOM
Systems and methods for processing sensor data
Systems and methods for processing sensor data are provided. In some embodiments, systems and methods are provided for calibration of a continuous analyte sensor. In some embodiments, systems and methods are provided for classification of a level of noise on a sensor signal. In some embodiments, systems and methods are provided for determining a rate of change for analyte concentration based on a continuous sensor signal. In some embodiments, systems and methods for alerting or alarming a patient based on prediction of glucose concentration are provided.
Owner:DEXCOM INC
Integrated medicament delivery device for use with continuous analyte sensor
ActiveUS20080306435A1Reduce the burden onSimple processAmpoule syringes2D-image generationMedication injectionDiabetes mellitus
An integrated system for the monitoring and treating diabetes is provided, including an integrated receiver / hand-held medicament injection pen, including electronics, for use with a continuous glucose sensor. In some embodiments, the receiver is configured to receive continuous glucose sensor data, to calculate a medicament therapy (e.g., via the integrated system electronics) and to automatically set a bolus dose of the integrated hand-held medicament injection pen, whereby the user can manually inject the bolus dose of medicament into the host. In some embodiments, the integrated receiver and hand-held medicament injection pen are integrally formed, while in other embodiments they are detachably connected and communicated via mutually engaging electrical contacts and / or via wireless communication.
Owner:DEXCOM
Systems and methods for processing sensor data
Systems and methods for processing sensor data are provided. In some embodiments, systems and methods are provided for calibration of a continuous analyte sensor. In some embodiments, systems and methods are provided for classification of a level of noise on a sensor signal. In some embodiments, systems and methods are provided for determining a rate of change for analyte concentration based on a continuous sensor signal. In some embodiments, systems and methods for alerting or alarming a patient based on prediction of glucose concentration are provided.
Owner:DEXCOM
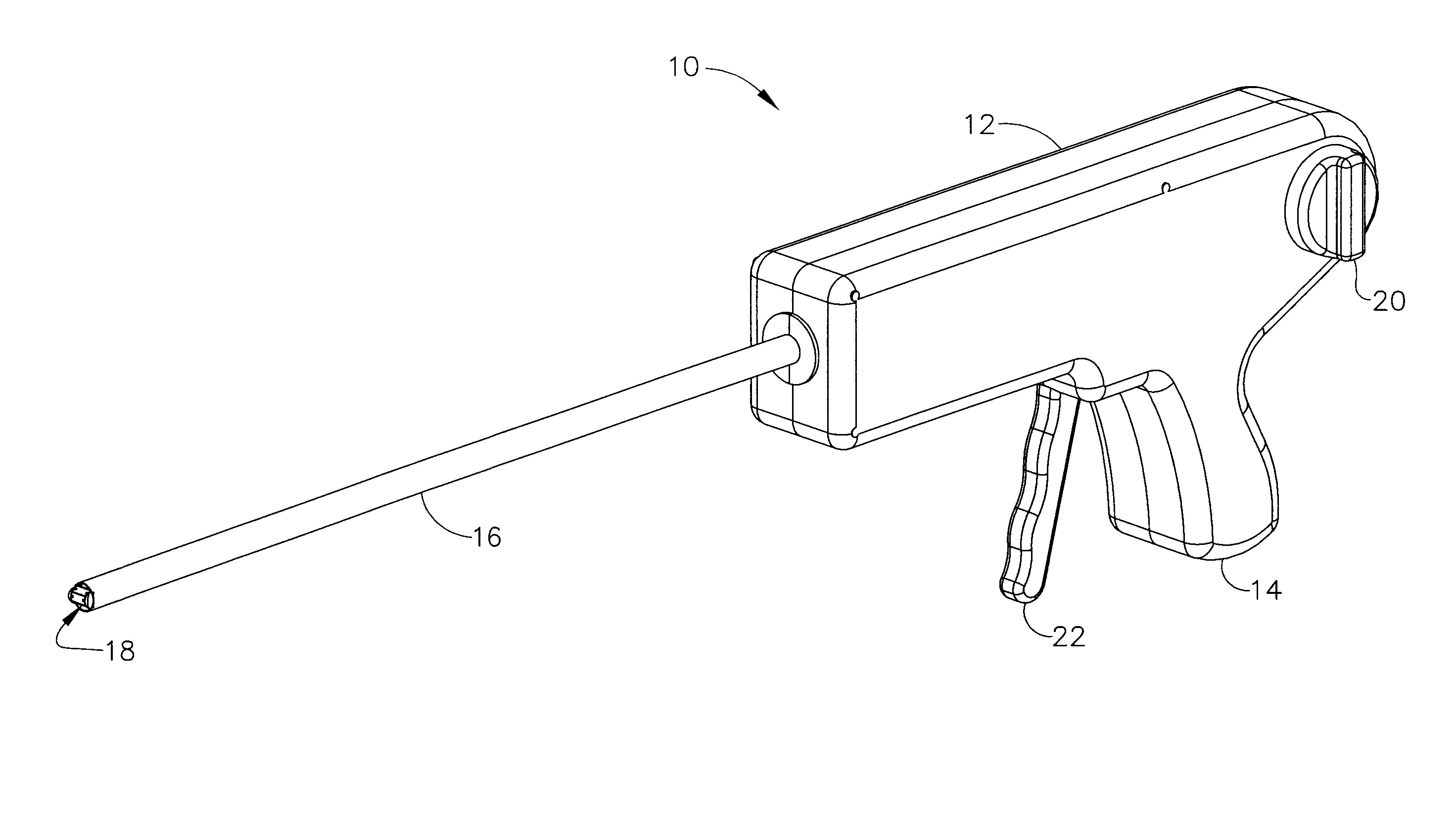
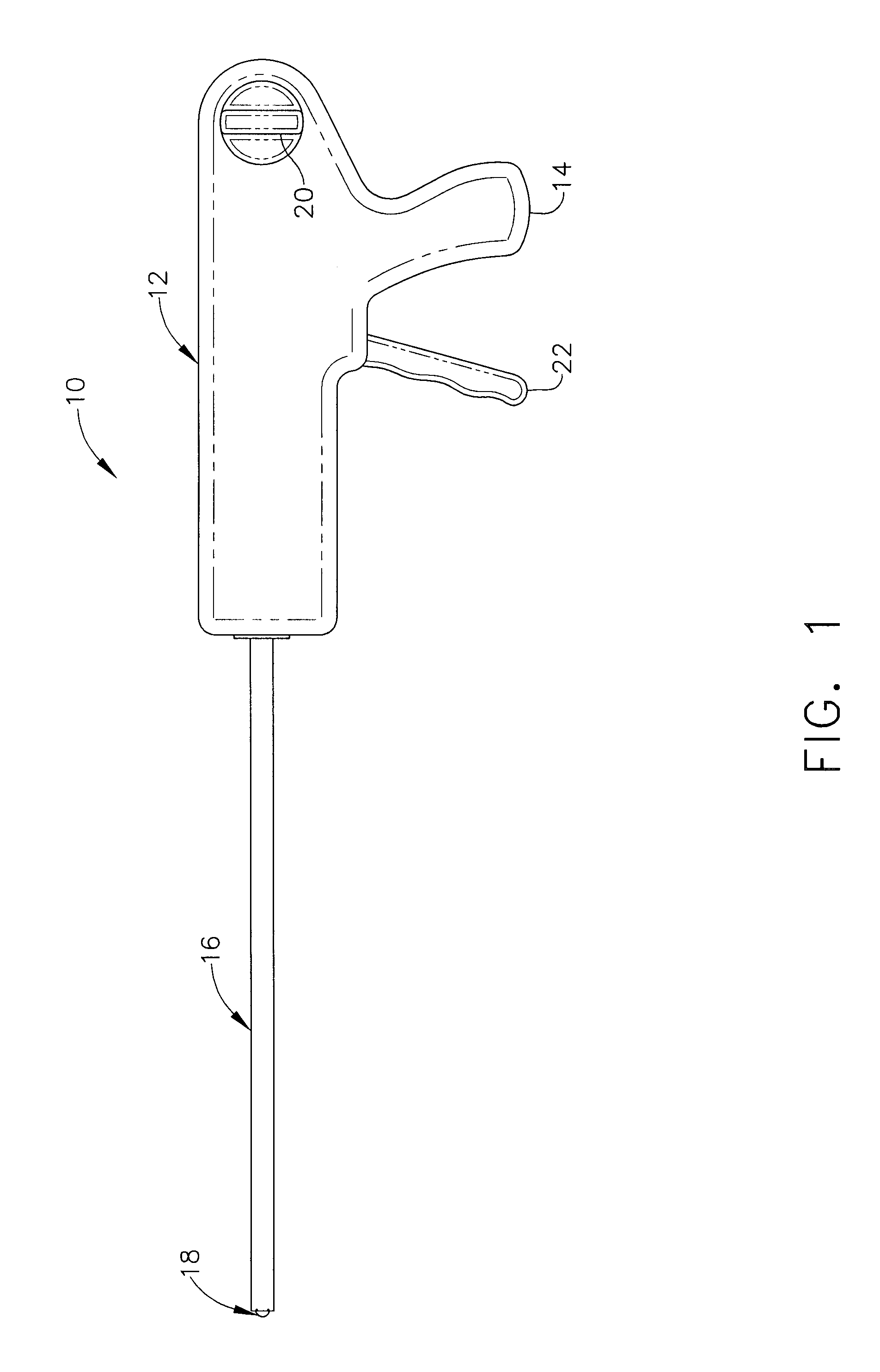
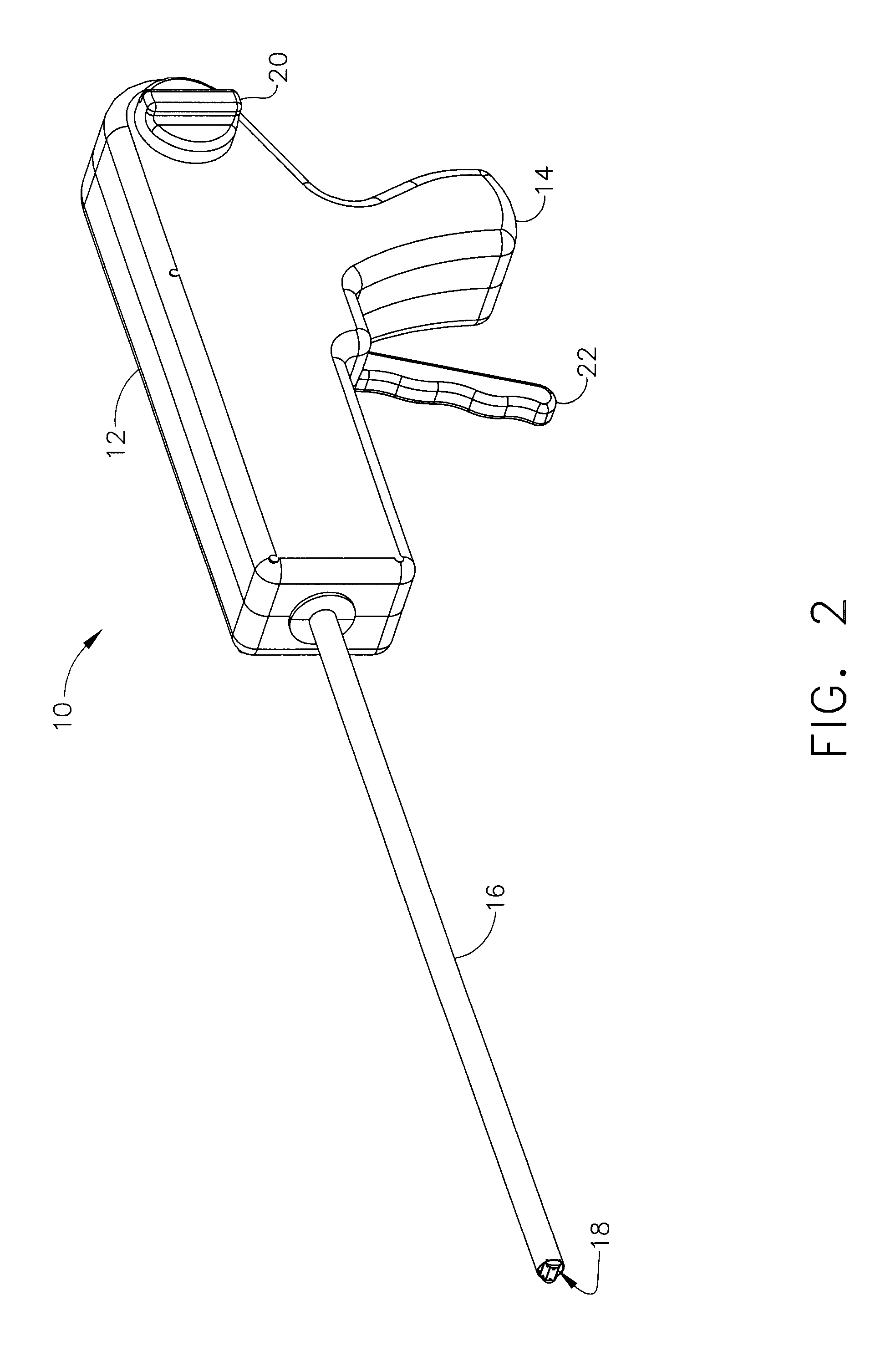
Surgical stapler
Methods and devices for closing a puncture wound in a liquid carrying vessel are provided. In one exemplary embodiment, a surgical stapler is provided having a locator tube with an inflatable member formed thereon and adapted to be positioned within a liquid carrying vessel adjacent a puncture wound, and a staple applying apparatus that is slidably disposed on a portion of the locator tube and that is adapted to apply a surgical staple to seal a puncture wound in a liquid carrying vessel.
Owner:ABBOTT CARDIOVASCULAR
Systems and methods for processing sensor data
Systems and methods for processing sensor data are provided. In some embodiments, systems and methods are provided for calibration of a continuous analyte sensor. In some embodiments, systems and methods are provided for classification of a level of noise on a sensor signal. In some embodiments, systems and methods are provided for determining a rate of change for analyte concentration based on a continuous sensor signal. In some embodiments, systems and methods for alerting or alarming a patient based on prediction of glucose concentration are provided.
Owner:DEXCOM
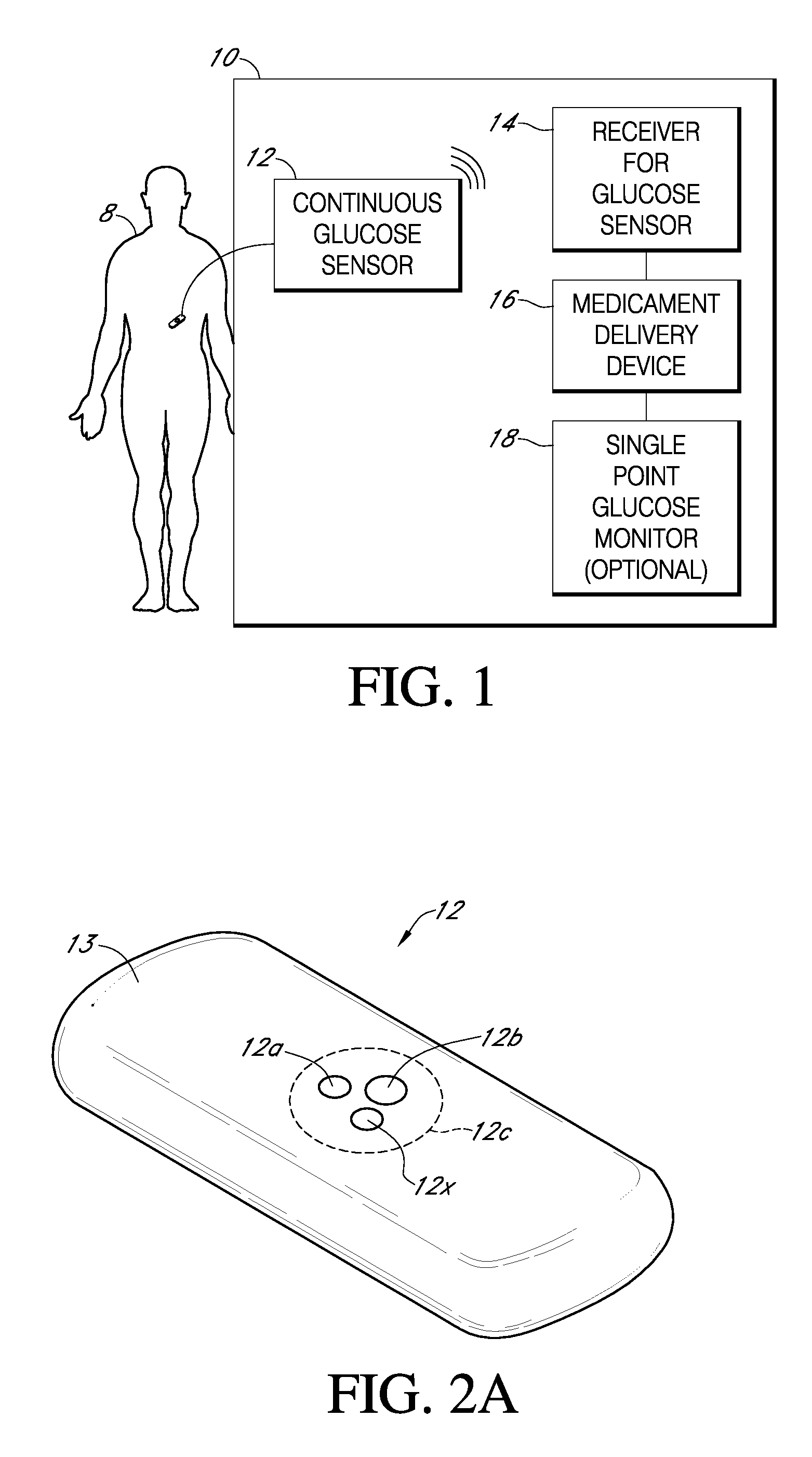
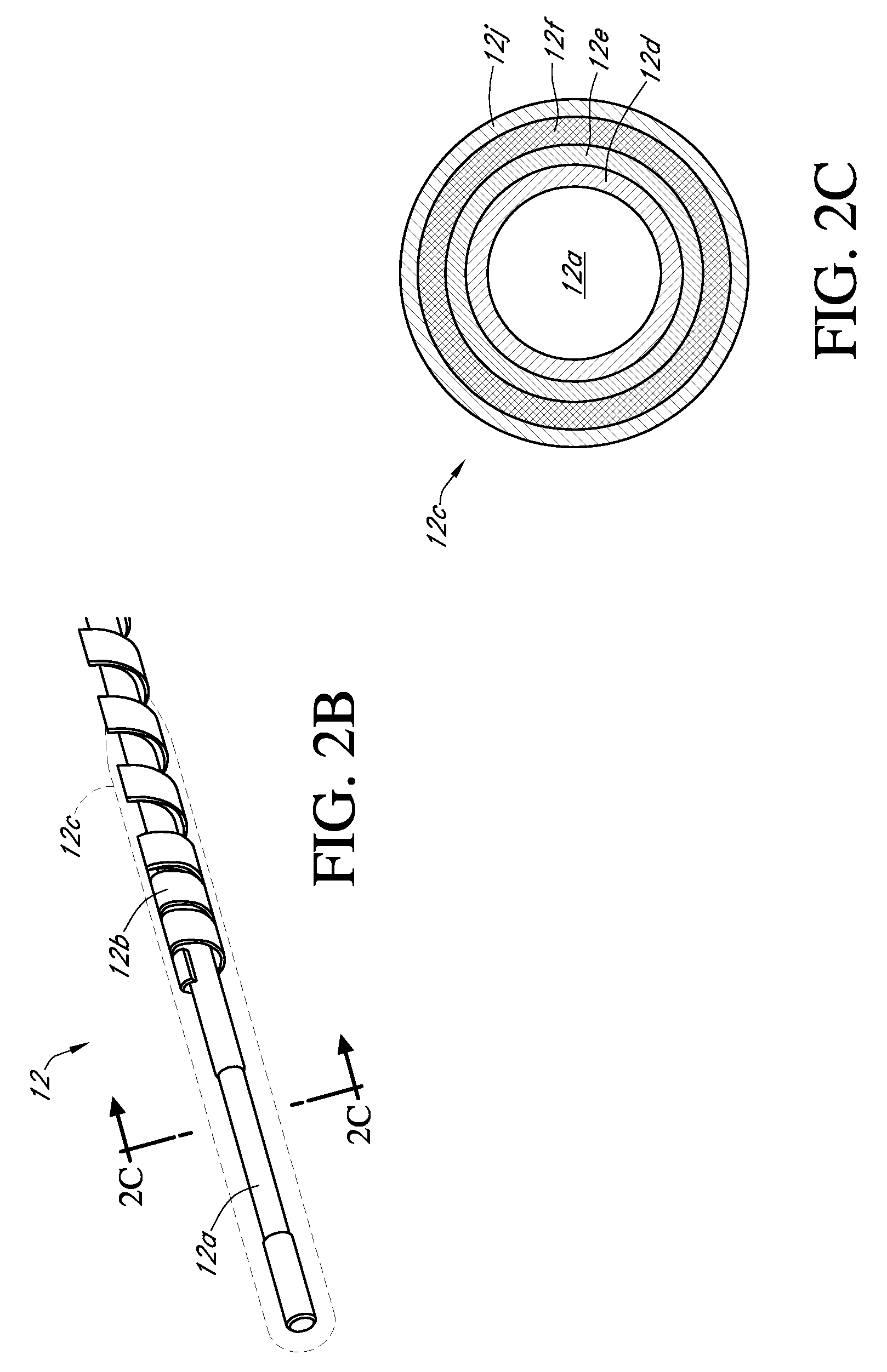
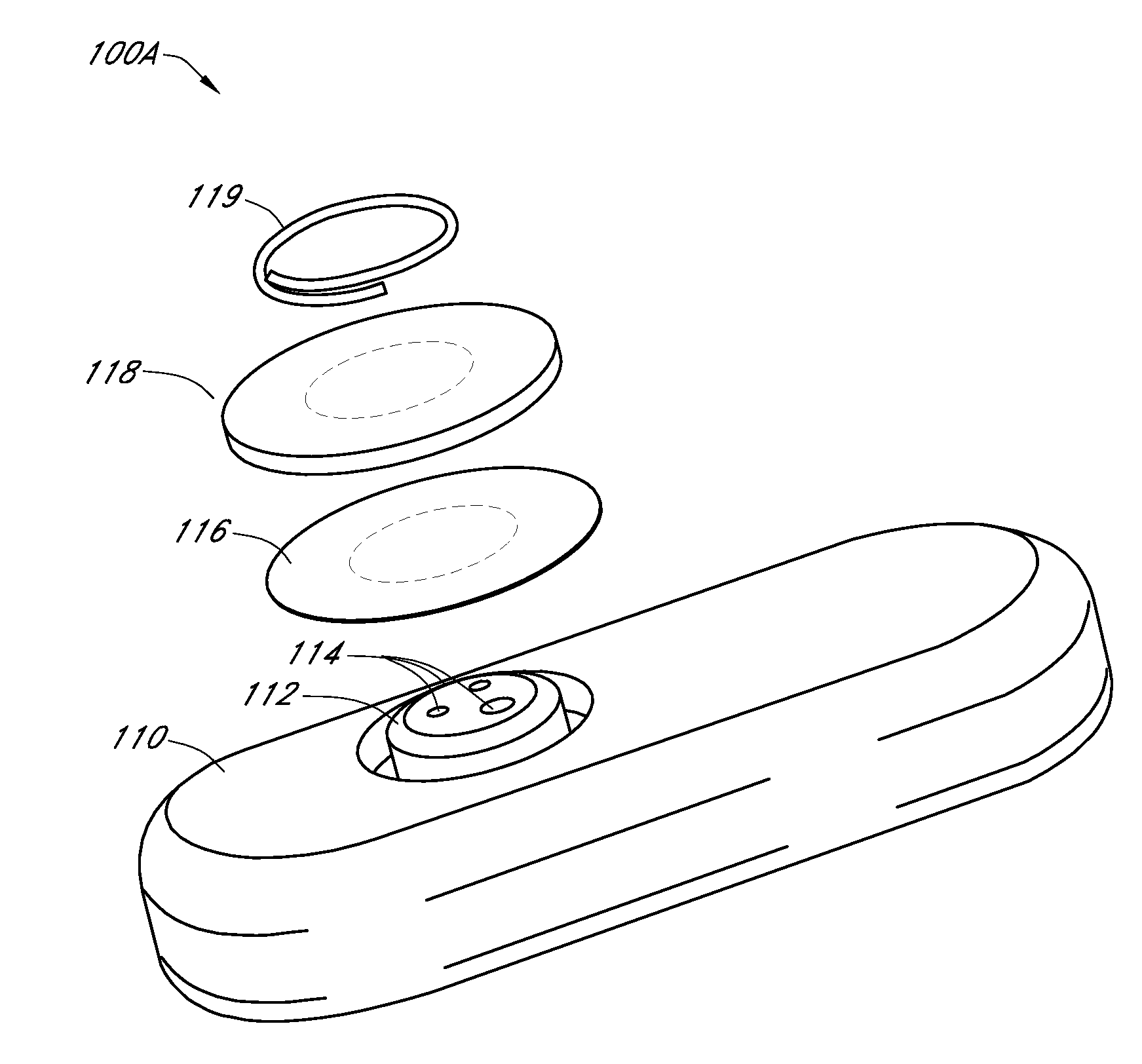
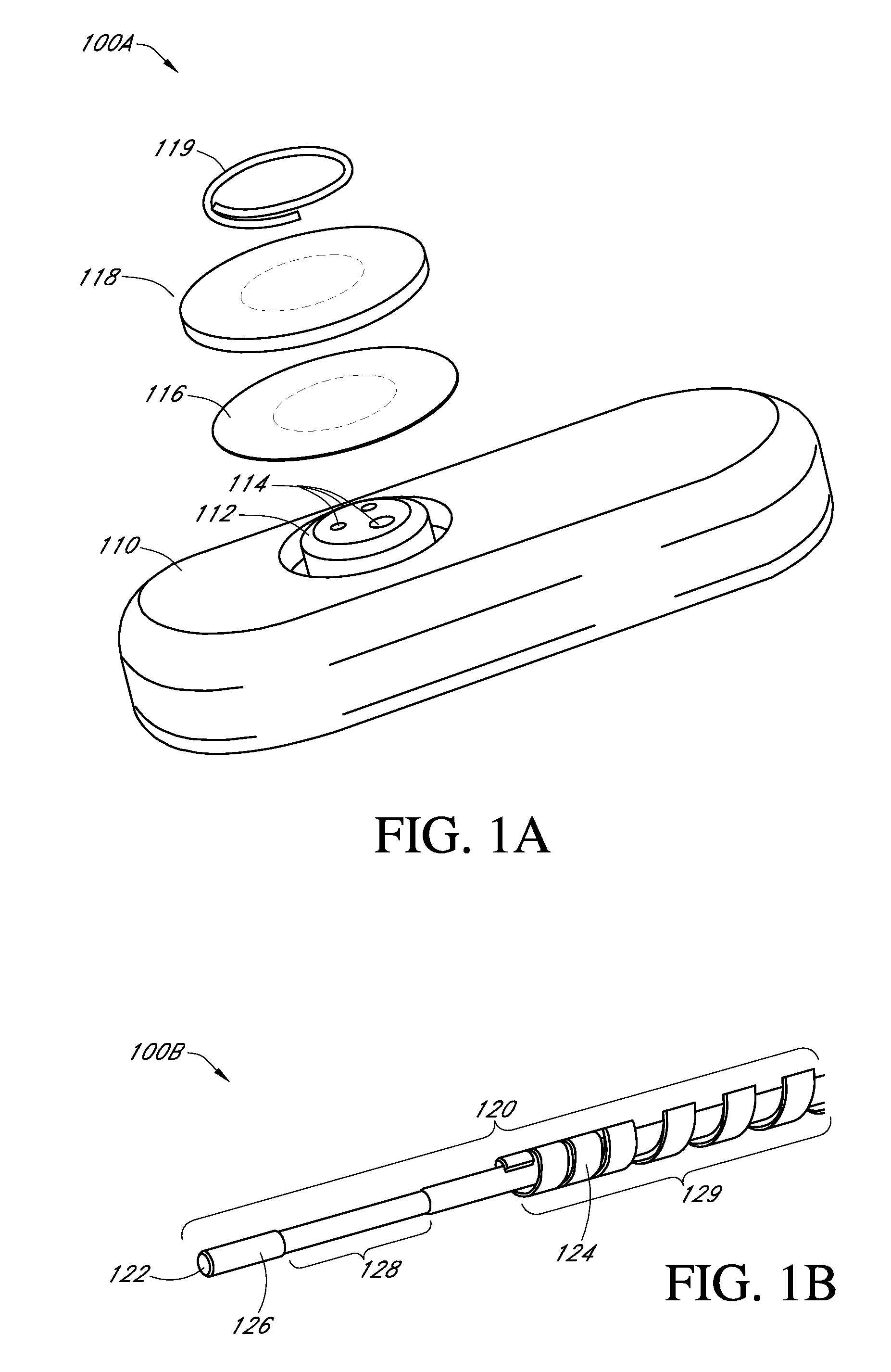
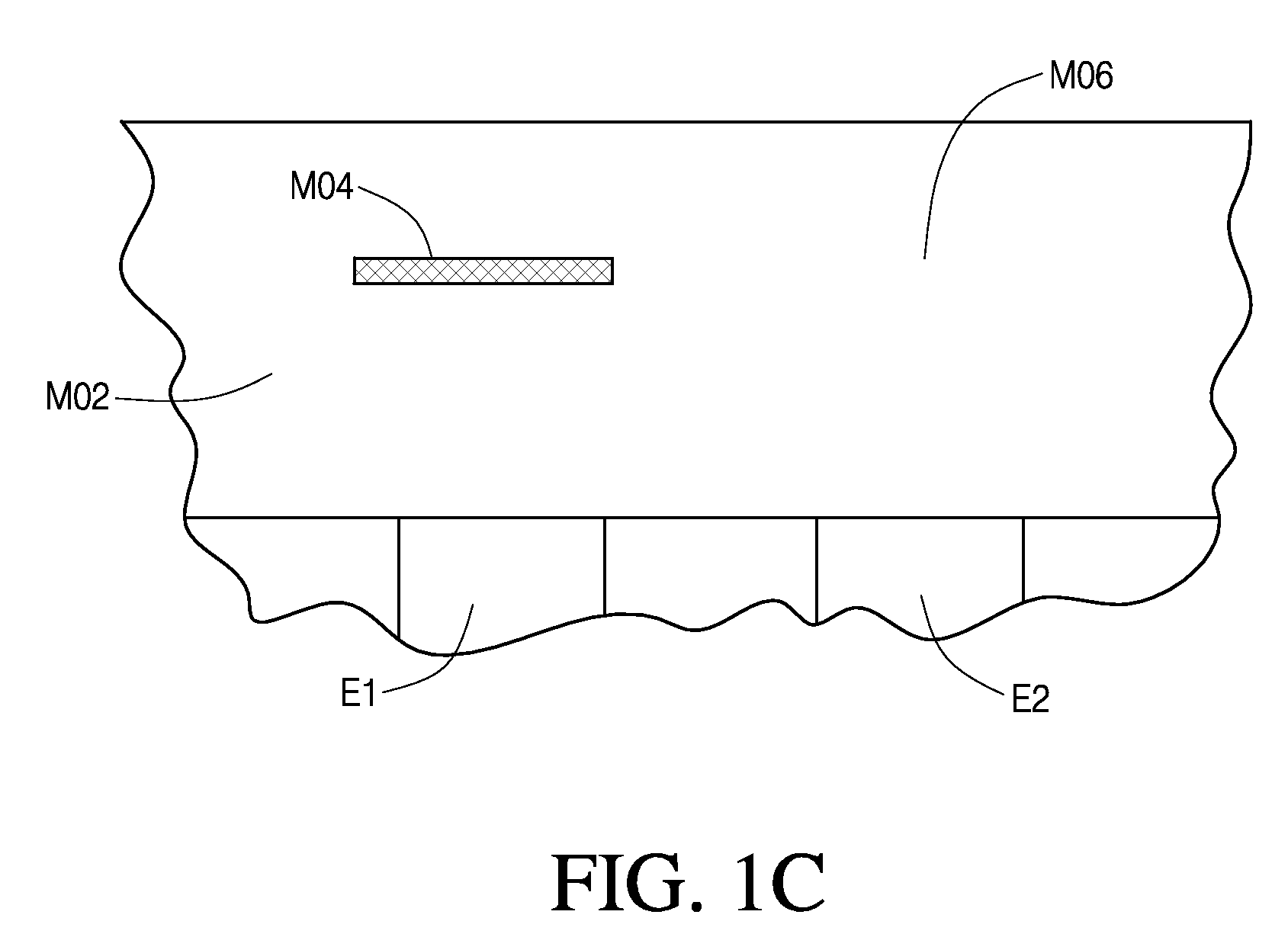
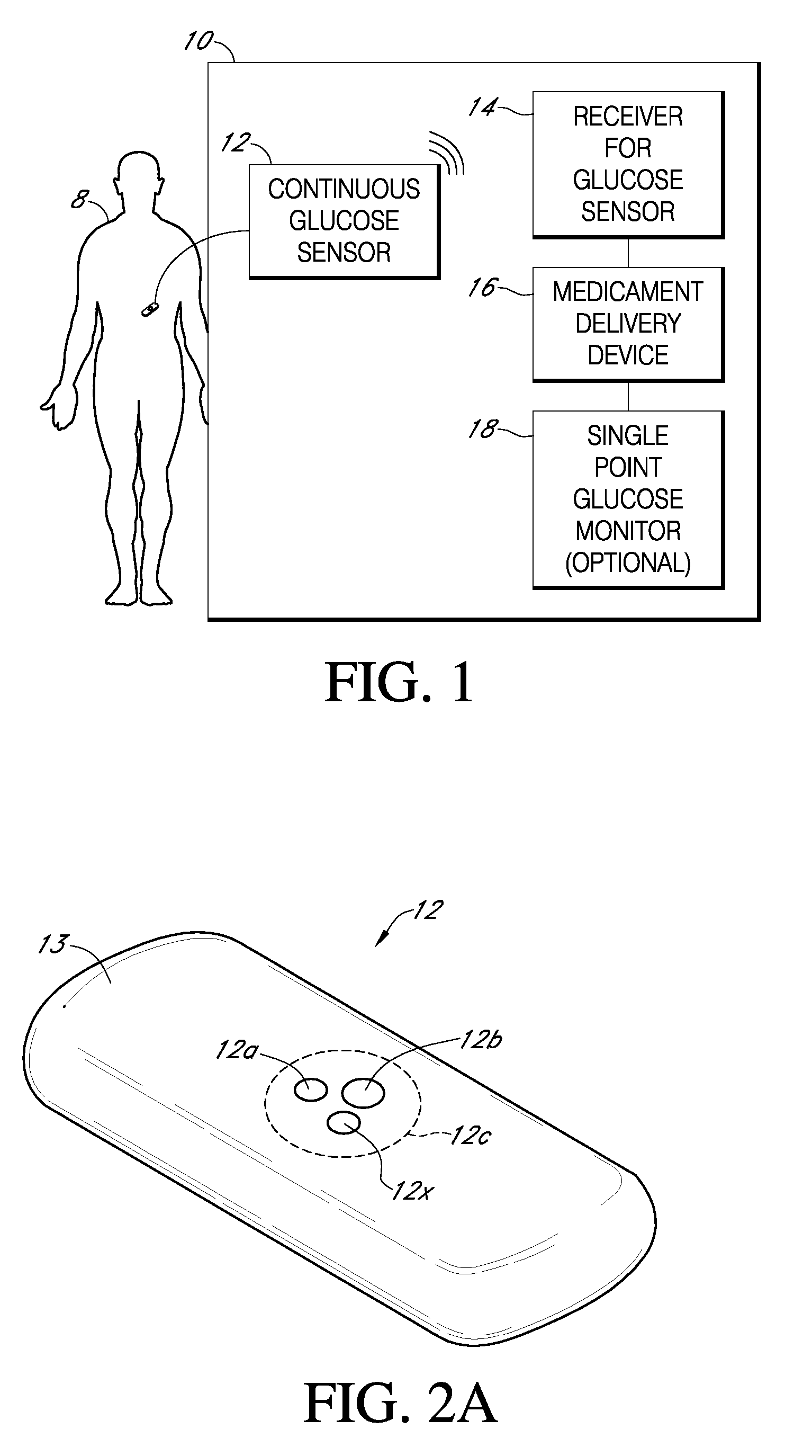
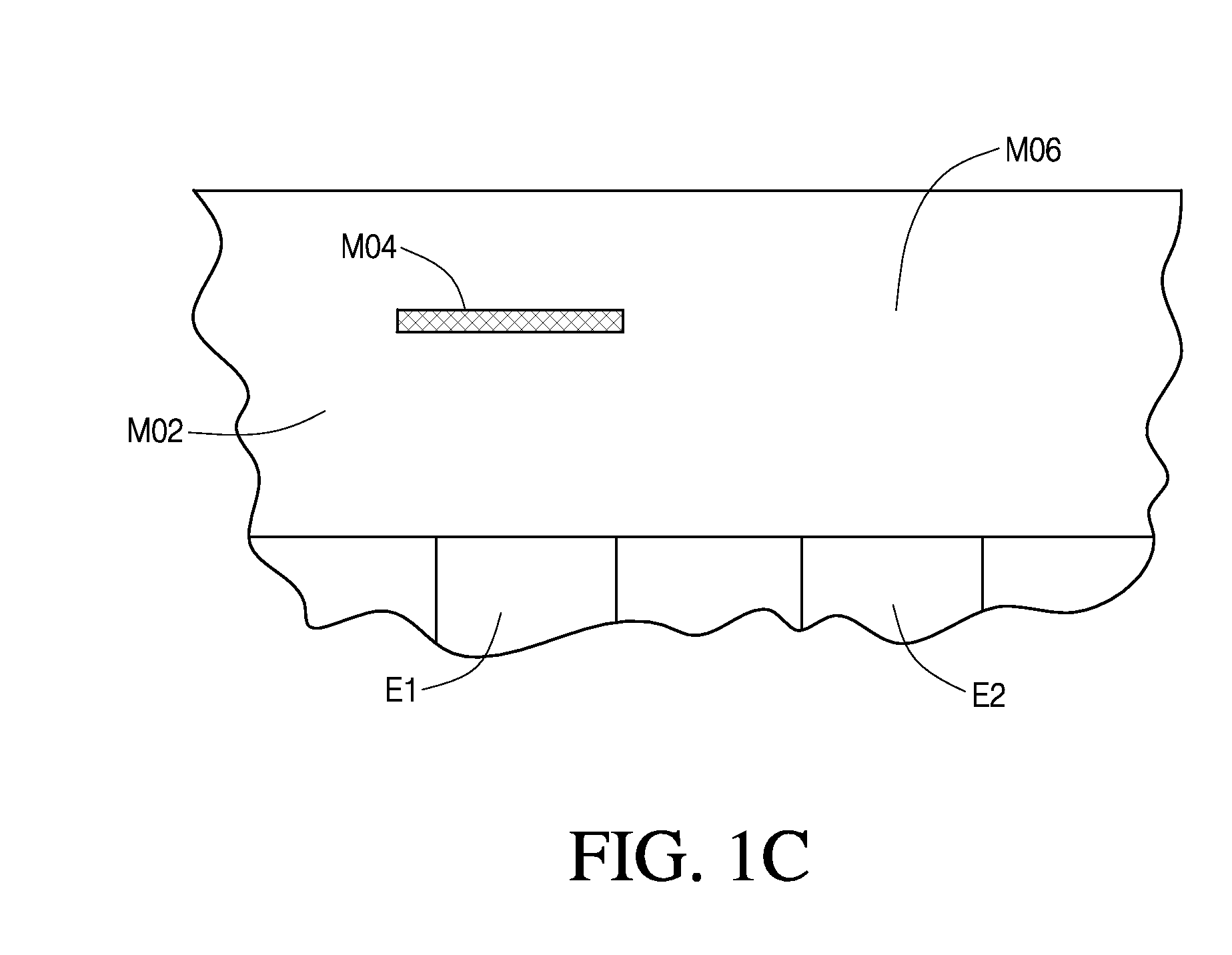
Integrated receiver for continuous analyte sensor
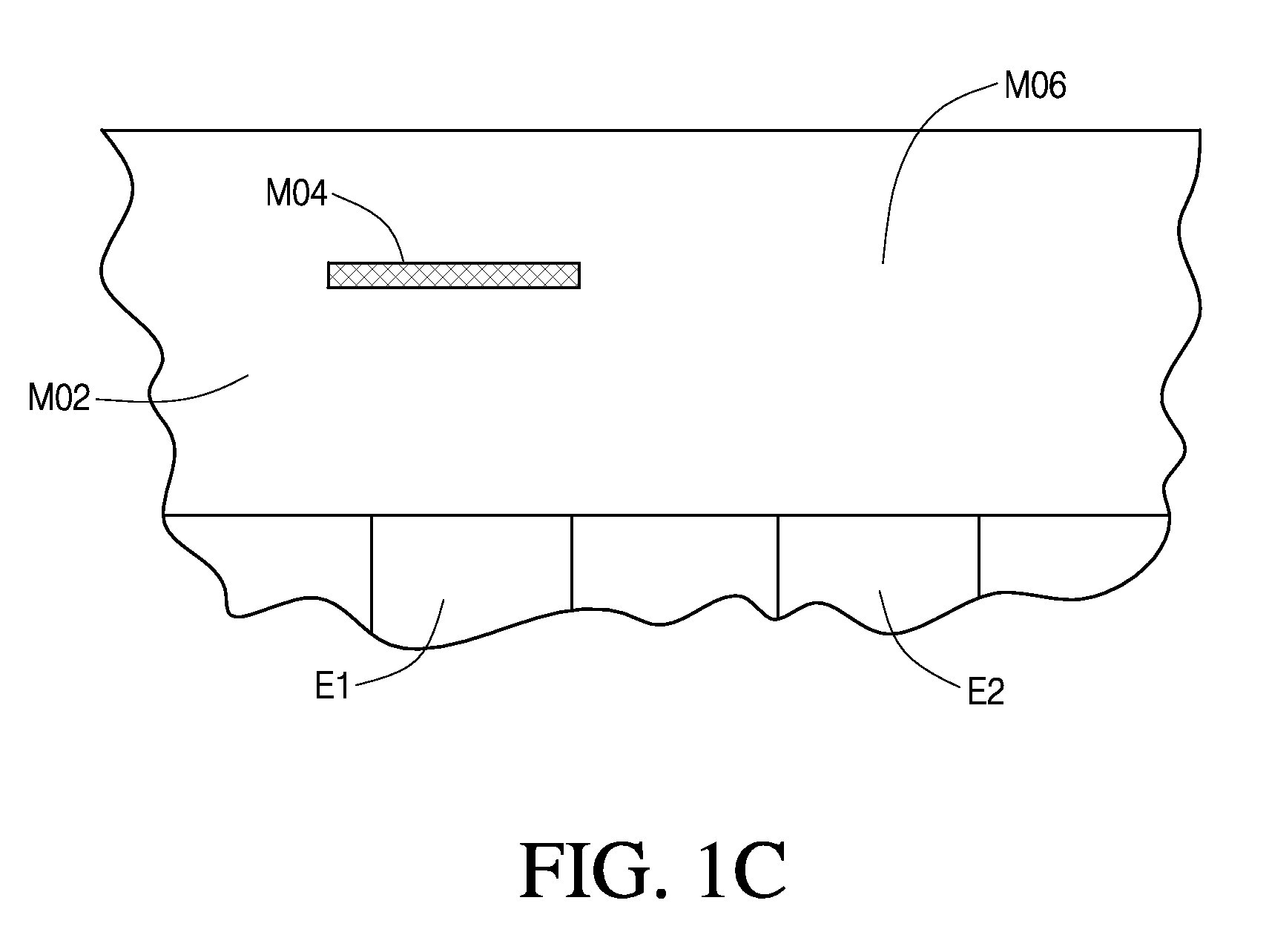
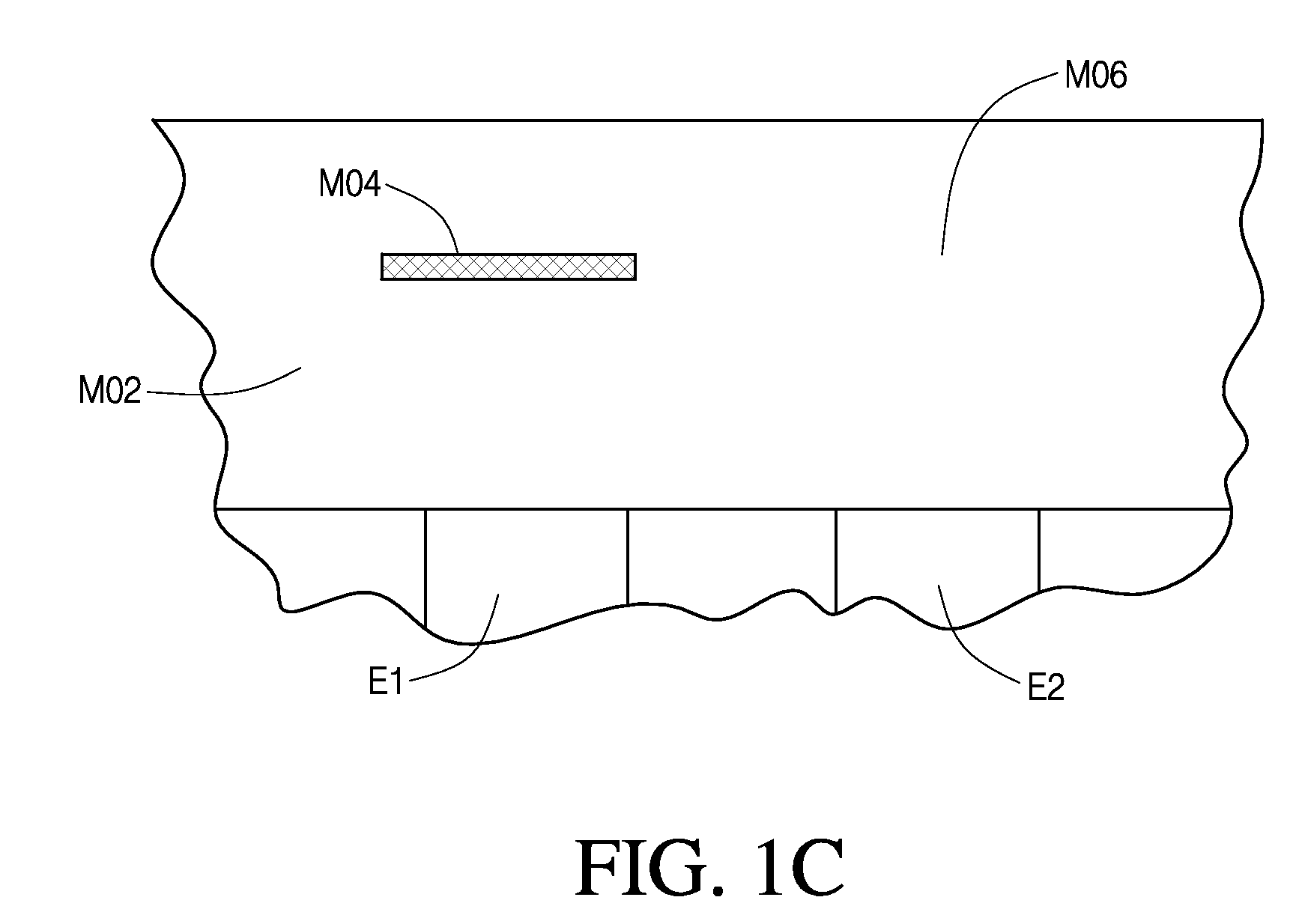
InactiveUS20080287764A1Simpler and few componentReduce errorsPharmaceutical delivery mechanismEndoradiosondesGlucose sensorsData stream
A system is provided for monitoring glucose in a host, including a continuous glucose sensor that produces a data stream indicative of a host's glucose concentration and an integrated receiver that receives the data stream from the continuous glucose sensor and calibrates the data stream using a single point glucose monitor that is integral with the integrated receiver. The integrated receiver obtains a glucose value from the single point glucose monitor, calibrates the sensor data stream received from the continuous glucose sensor, and displays one or both of the single point glucose measurement values and the calibrated continuous glucose sensor values on the user interface.
Owner:DEXCOM INC
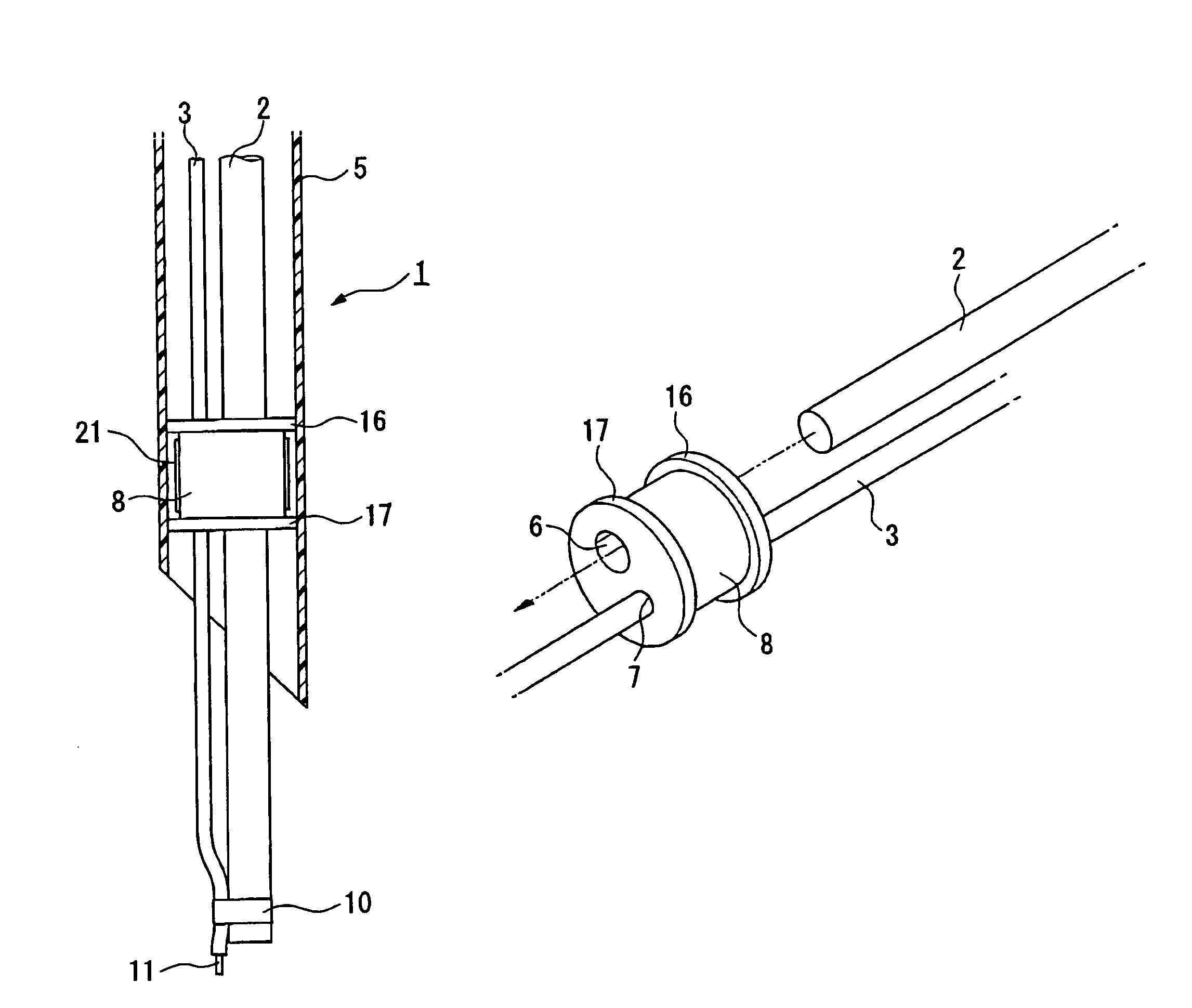
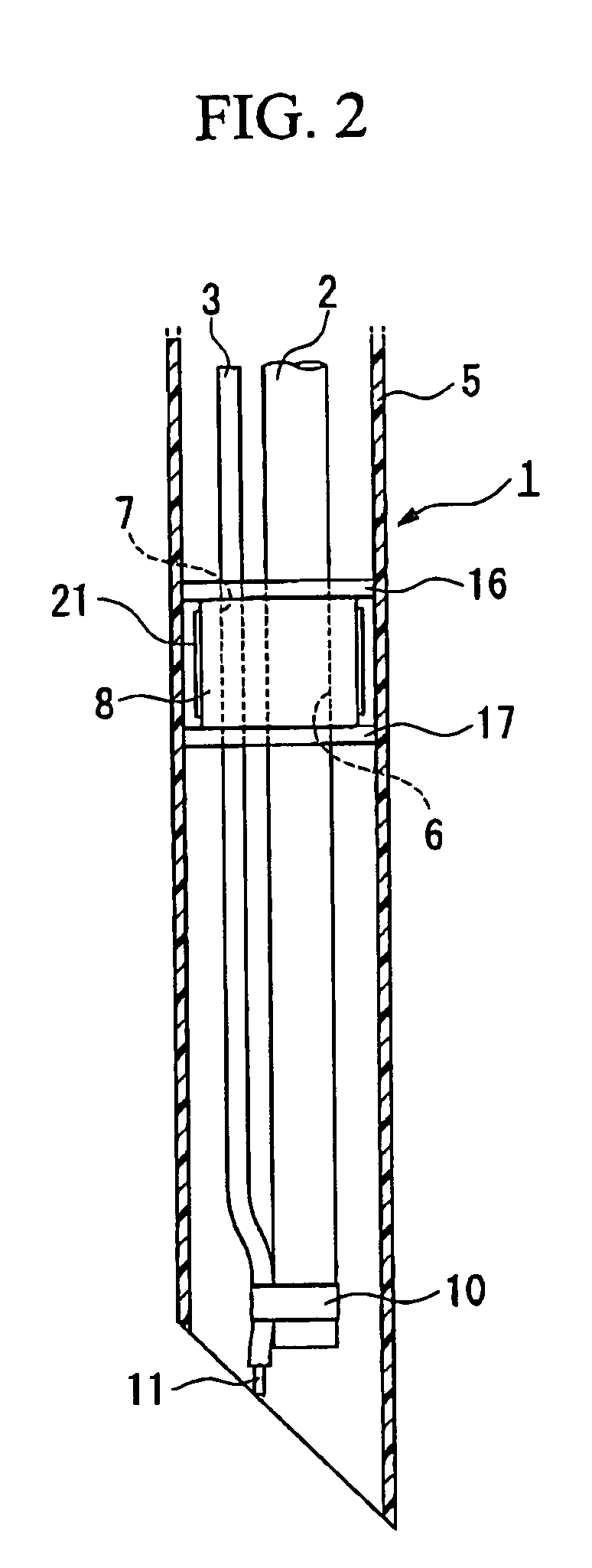
Insertion auxiliary implement
An insertion auxiliary implement of the present invention includes: a tubular part into which a flexible endoscope insertion part which is insertable into a body cavity, and one of a treatment tool and a channel into which the treatment tool is insertable, are insertable; and a sealing member which has through holes for supporting the endoscope insertion part and one of the treatment tool and the channel in the tubular part, and which airtightly and movably contacts each of a periphery of the endoscope insertion part, a periphery of the treatment tool or a periphery of the channel, and an inner surface of the tubular part, and thereby maintains airtightness between a distal end and a proximal end inside the tubular part.
Owner:OLYMPUS CORP
Laparoscopic gastric and intestinal trocar
InactiveUS8795308B2Easy to holdReduce the cross-sectional areaInfusion syringesSurgical needlesDistal portionSurgery
A trocar needle includes an elongate body having a distal end portion and a proximal end portion, a penetrating tip formed at the distal end portion of the body, and an attachment portion formed at the proximal end portion for attaching a tether thereto. A grip region can further be provided and can be formed for example, at the proximal end portion of the body to facilitate gripping by a surgical grasping device. Additionally or alternatively, a notch or otherwise reduced cross-sectional area can be provided. Such a feature can be formed, for example, at the distal end portion of the body, arranged proximal from a distal end thereof for enhancing haptic perception by a surgeon when utilizing the needle.
Owner:VALIN ELMER
Surgical access device
Methods and devices for accessing a body cavity are disclosed. In general, a surgical access device is provided that can include a cannula that defines a working channel that is sized and configured to receive a surgical instrument. A seal can be disposed in the cannula of the surgical access device. In one exemplary embodiment, the seal can be positioned at a point in the cannula that is effective to maintain contact between the seal and an instrument inserted therethrough as the instrument is rotated about that point.
Owner:CILAG GMBH INT
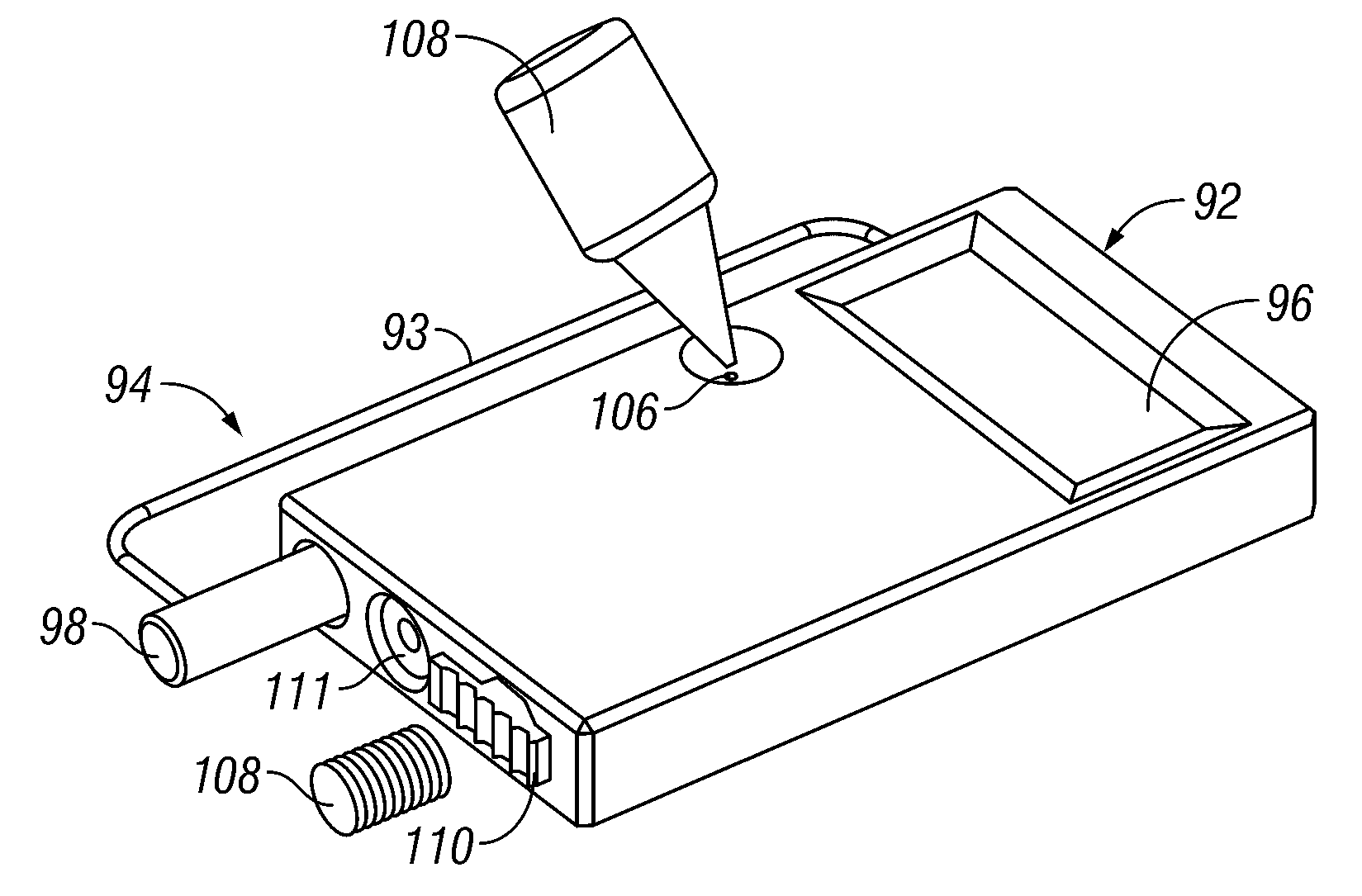
Surgical band fluid media dispenser
A multiple use fluid dispenser dispenses a flowable material in a precise pattern and quantity with leaking and clogging between dispensing avoided by employing a trigger fired syringe plunger to expel a fixed volume through a band. Between strokes, an advancement knob rotates the band over a distal dispensing tip to a nondispensing location that wipes excess flowable material and seals a dispensing orifice in a fluid conduit. The advancement knob further may rotate the band to a dispensing position wherein a combination of one or more dispensing holes produce a desired pattern and rate of flow with material over the dispensing hole(s) serving to initiate the flowable material, to control placement, serve as a detachable bandage or buttress material, etc.
Owner:ETHICON ENDO SURGERY INC
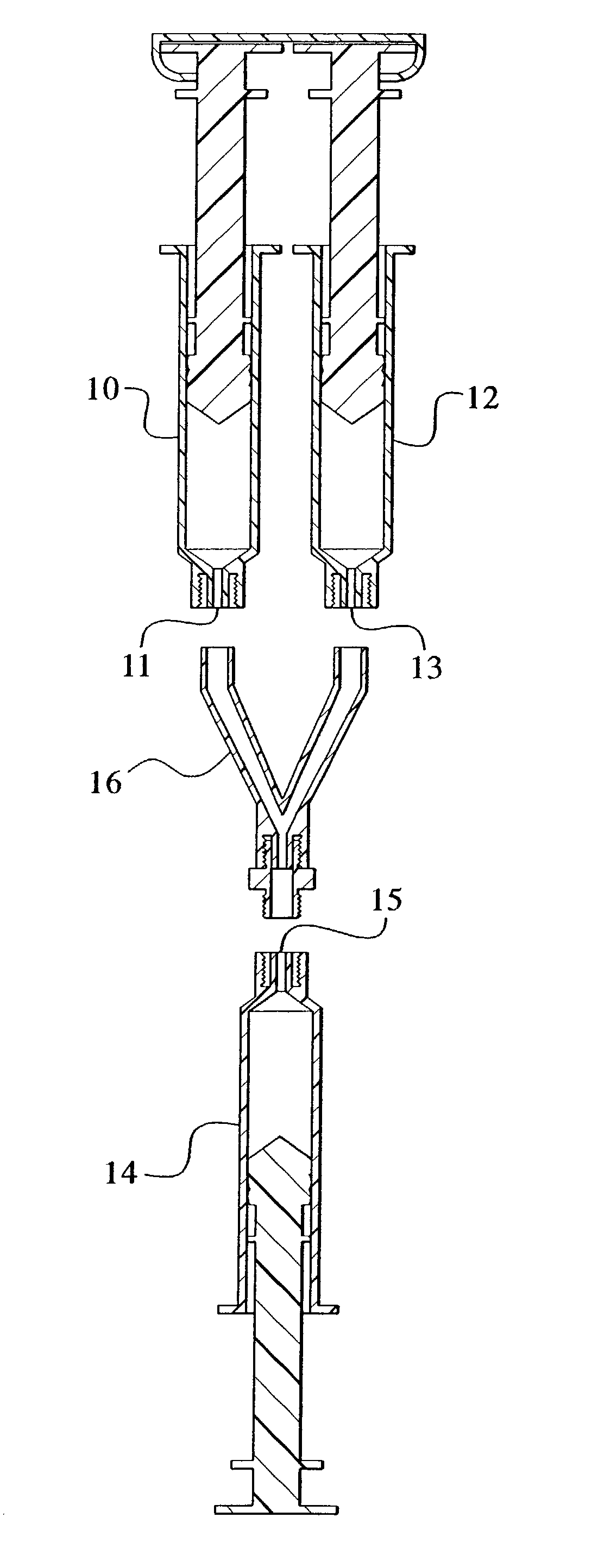
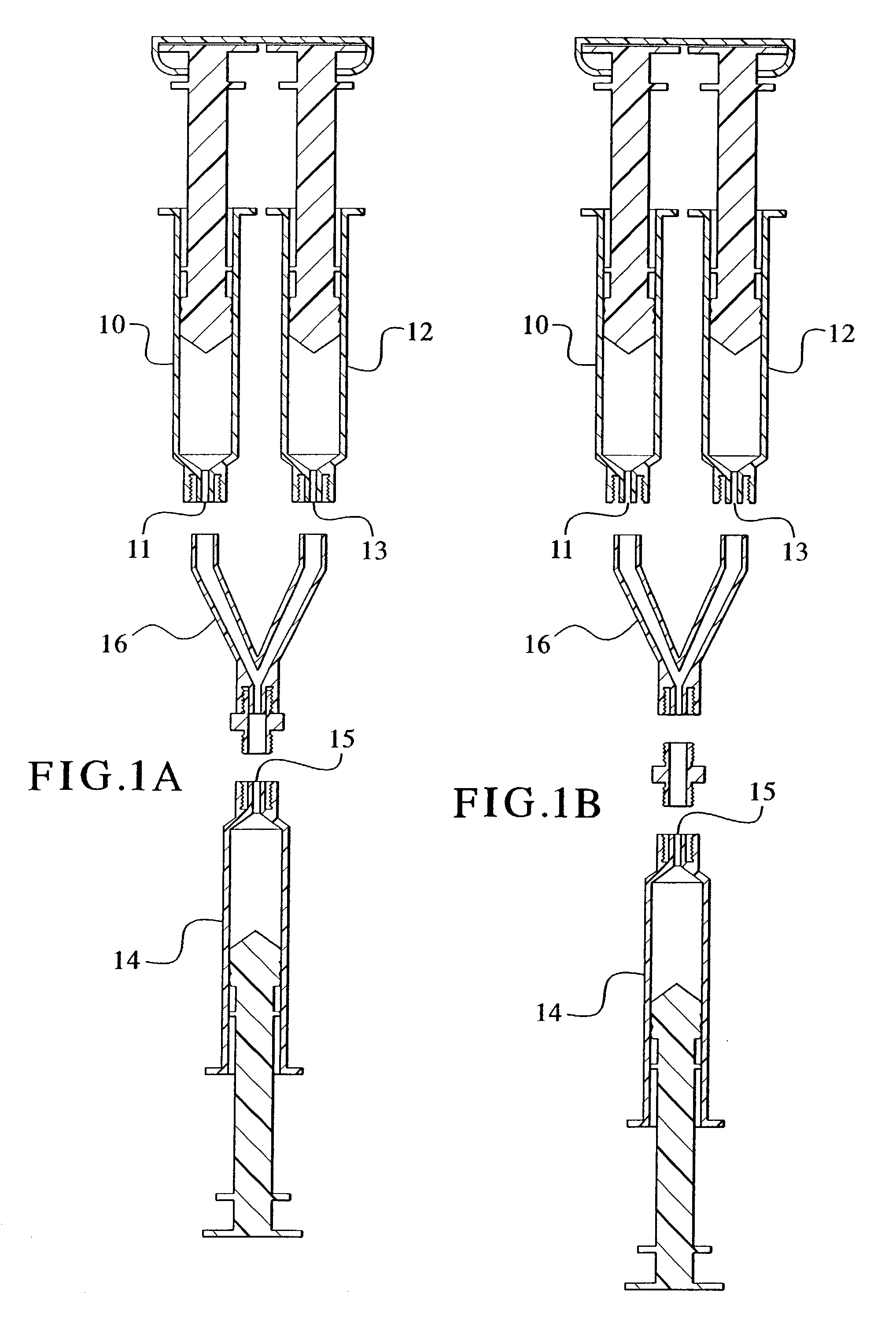
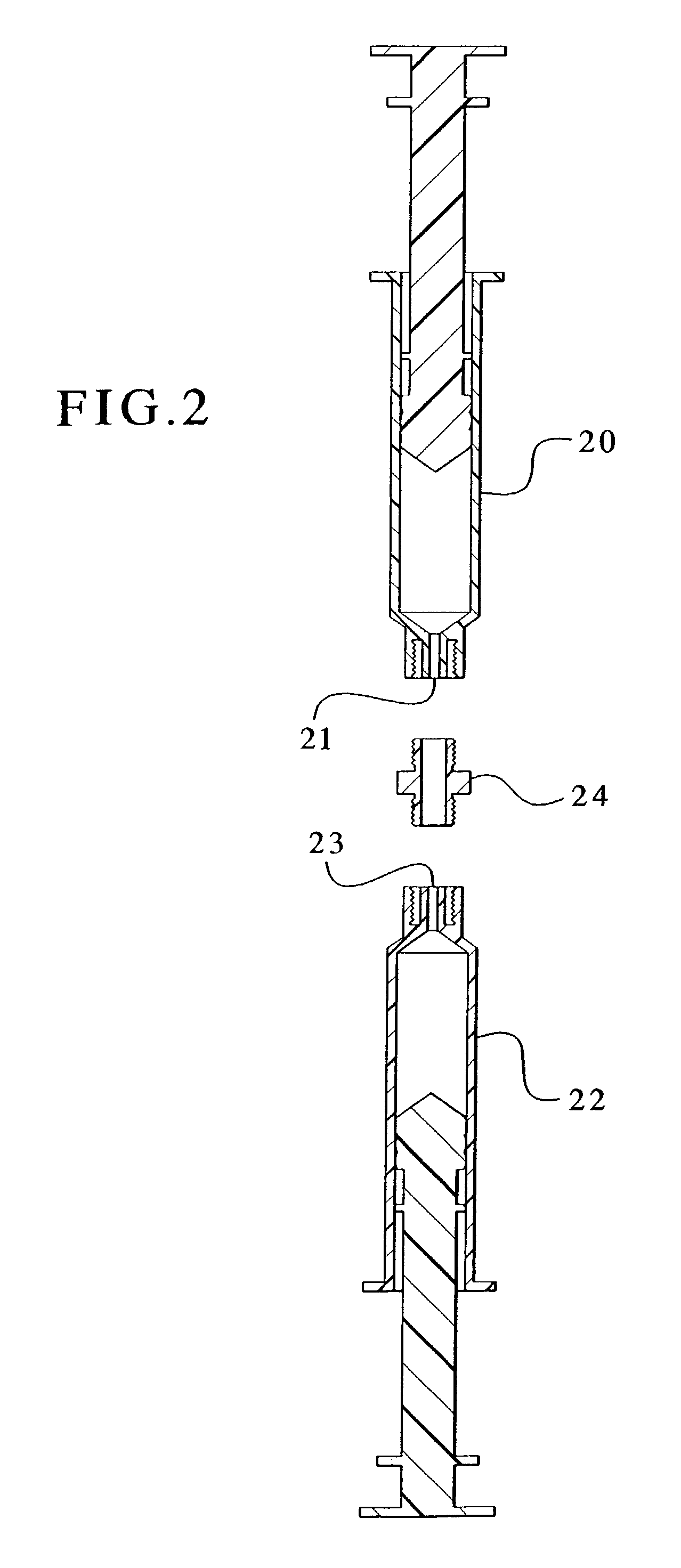
Devices and methods for mixing and extruding medically useful compositions
This invention provides devices and methods for mixing and extruding compositions which are medically and non-medically useful. The devices are particularly useful for mixing substances which are relatively inert when alone but become reactive when mixed. A common feature of all of the devices is that they allow the user to mix and ultimately extrude a composition from a single device which includes a single container or multiple interconnected containers.
Owner:BAXTER INT INC +1
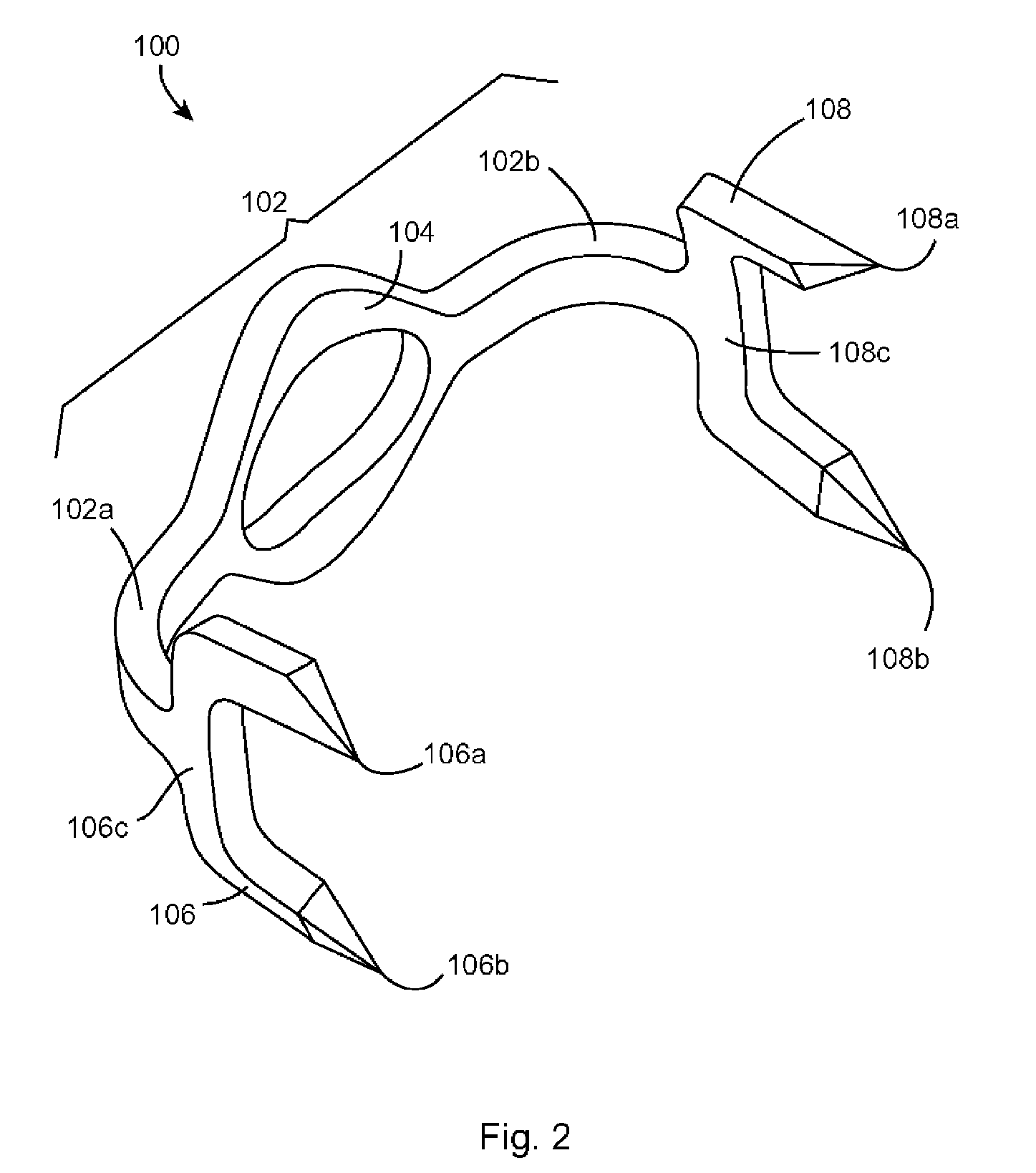
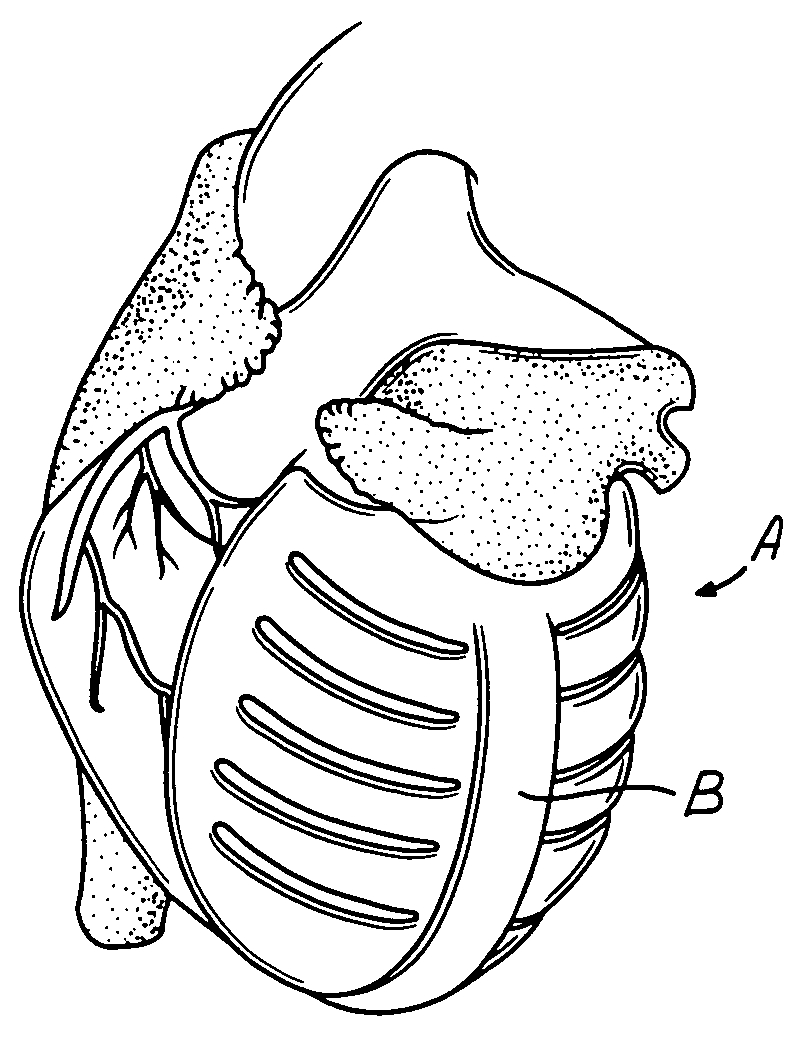
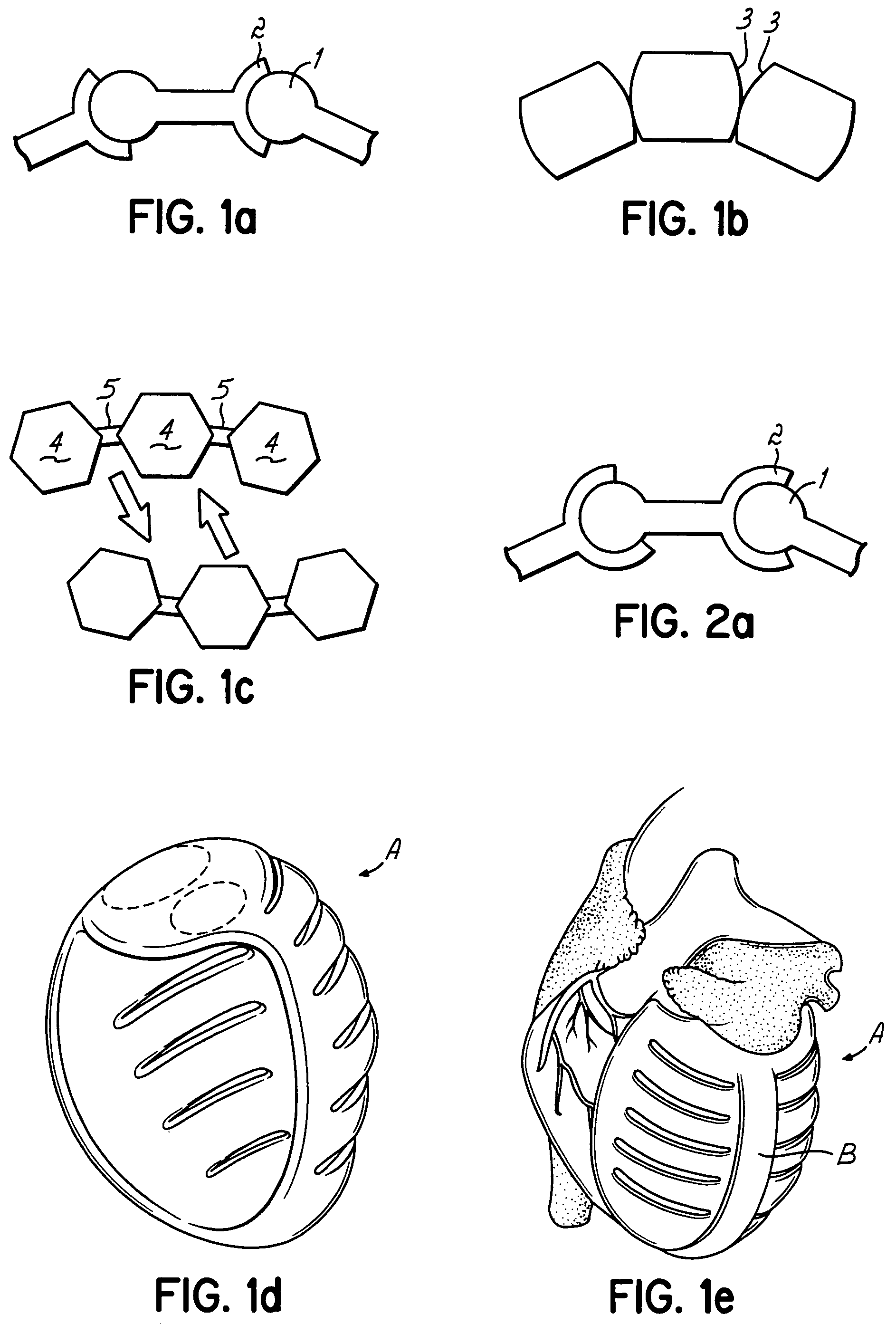
Actuation mechanisms for a heart actuation device
An actuation mechanism for assisting the operation of the natural heart has a varying shape for deforming the heart. In one embodiment, a plurality of links articulates with respect to each other for varying the shape of the actuation mechanism. The plurality of links is configured for being positioned proximate to an outer surface of the heart for deforming the heart by varying the shape of the actuation mechanism. In another embodiment, a jacket for coupling with an outer surface of the heart has a tether coupled to successive sections of the jacket. The tether is operable to be translated with respect to the jacket sections to vary the shape of the jacket for deforming the heart. In another embodiment, a plurality of concentric ring structures are coupled together to move with respect to each other in a concentric fashion. A movement mechanism coupled to the rings is operable to vary their positions with respect to each other to vary the overall shape for deforming the heart.
Owner:UNIVERSITY OF CINCINNATI +1
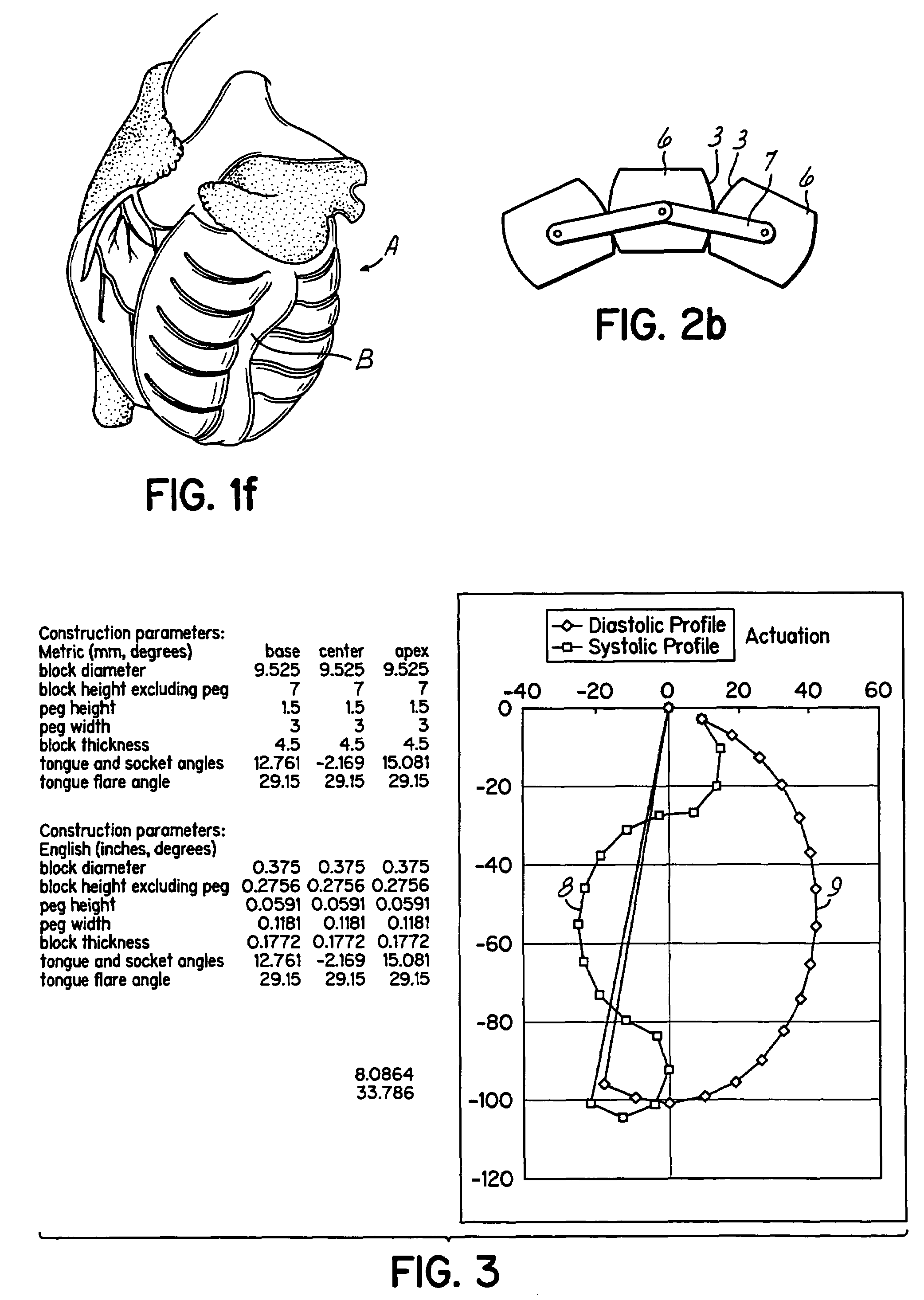
Apparatus, systems and methods for determining tissue oxygenation
Owner:SURGISENSE CORP
Wound dressing and method of use
ActiveUS20110282309A1Reduce decreaseExtended service lifeNon-adhesive dressingsPlastersWound.exudateMoisture
A system, method, and apparatus are disclosed for dressing a wound. The apparatus comprises a liquid and gas permeable transmission layer, an absorbent layer for absorbing wound exudate, the absorbent layer overlying the transmission layer, a gas impermeable cover layer overlying the absorbent layer and comprising a first orifice, wherein the cover layer is moisture vapor permeable.
Owner:SMITH & NEPHEW INC
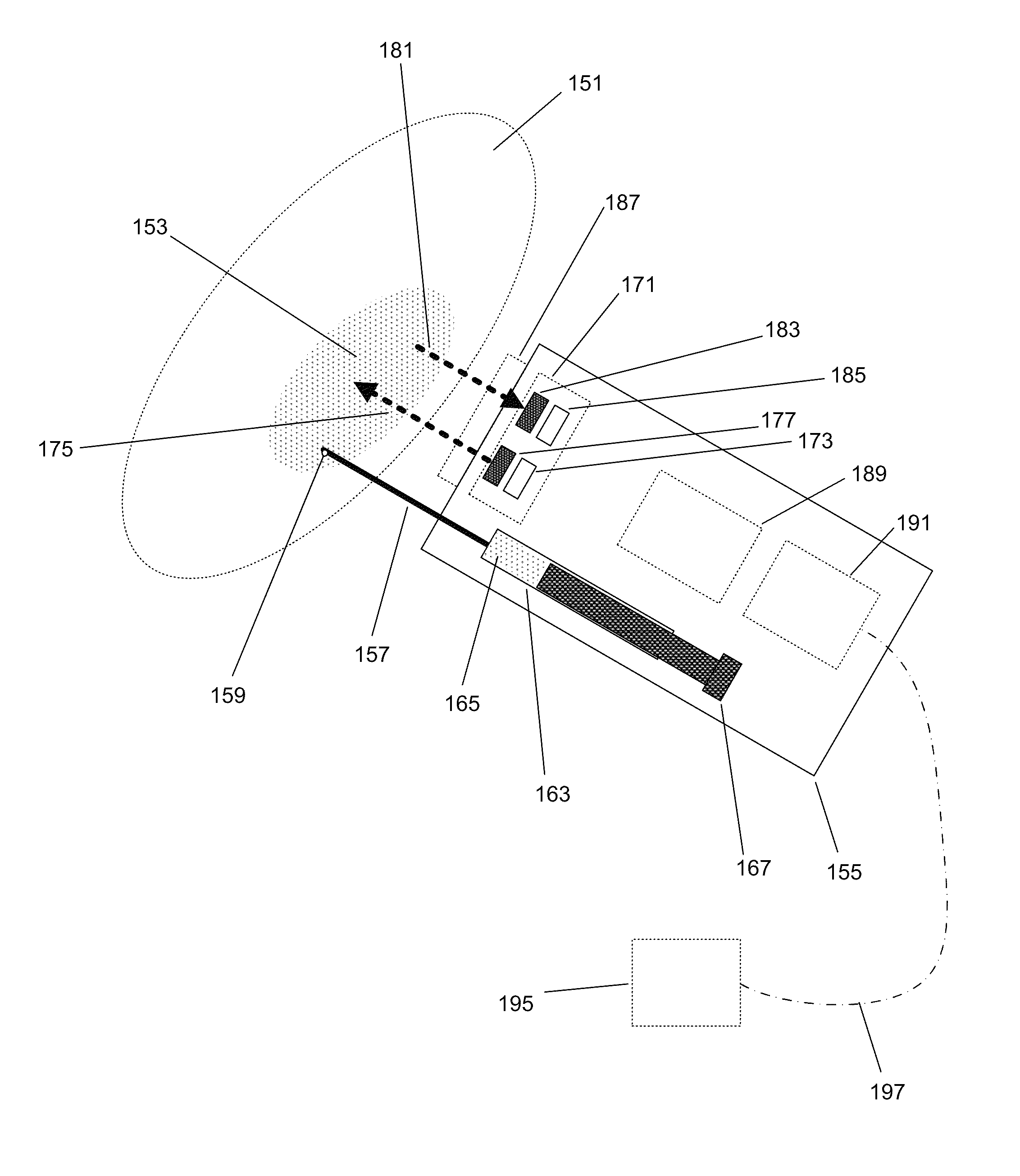
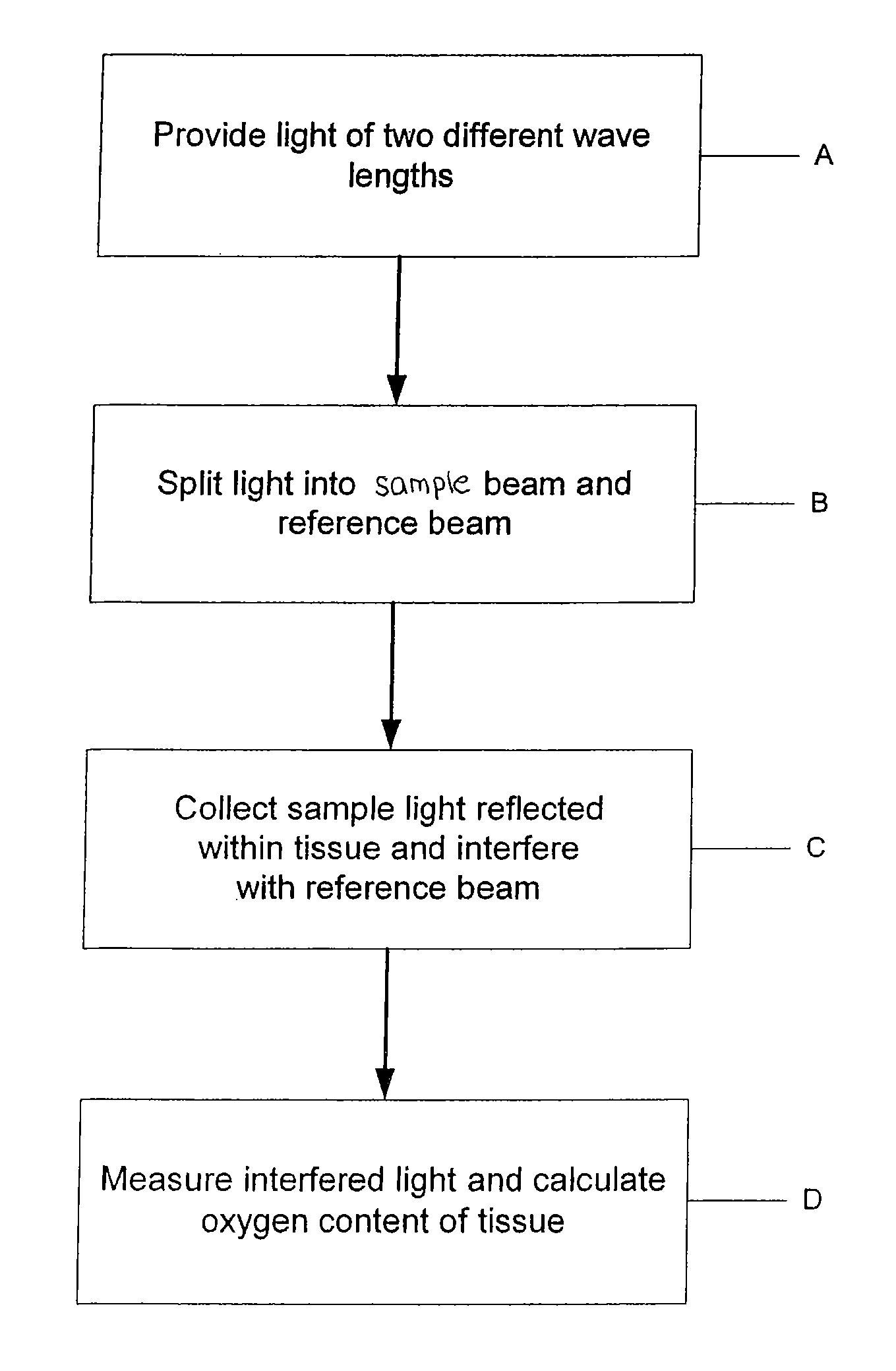
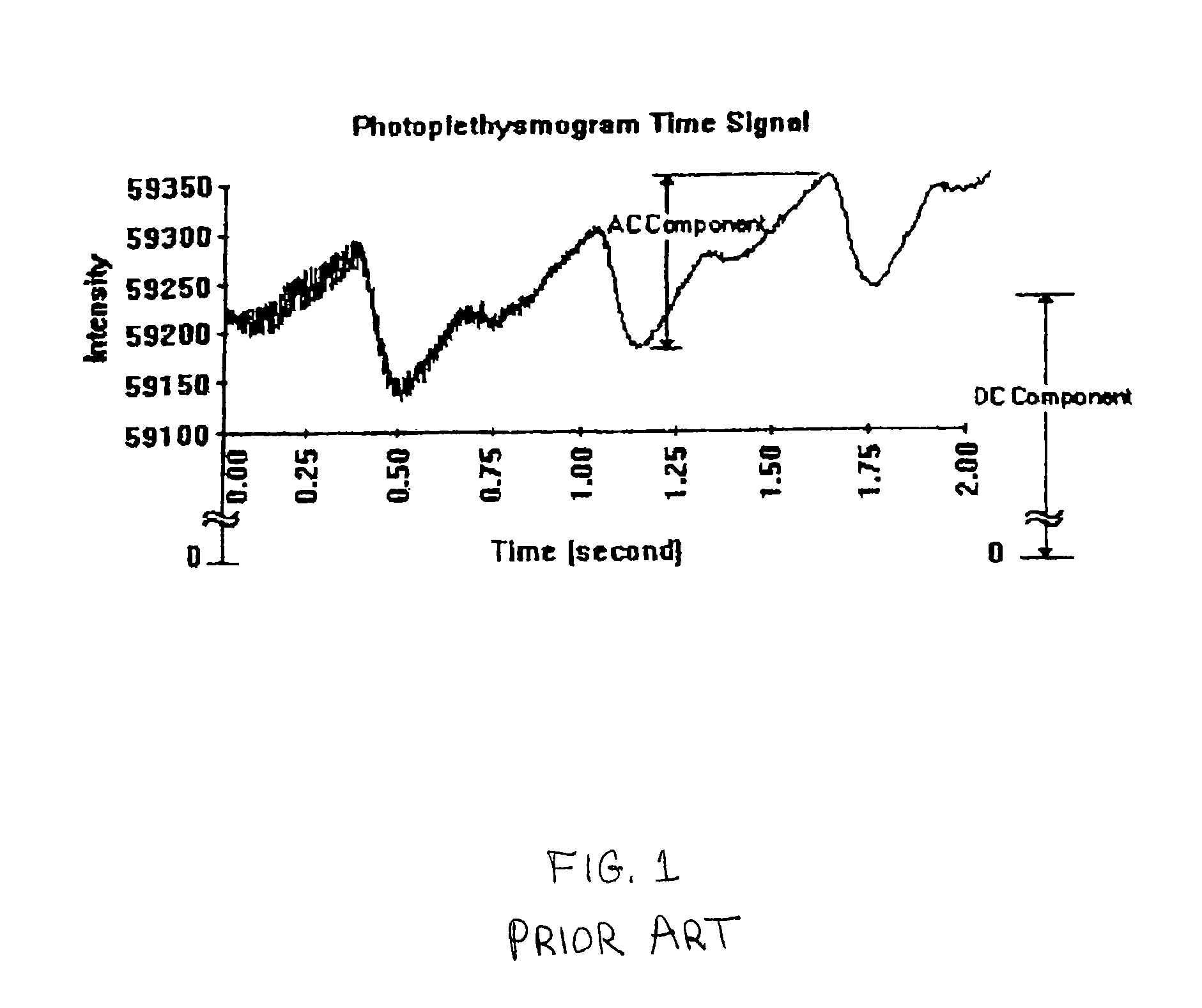
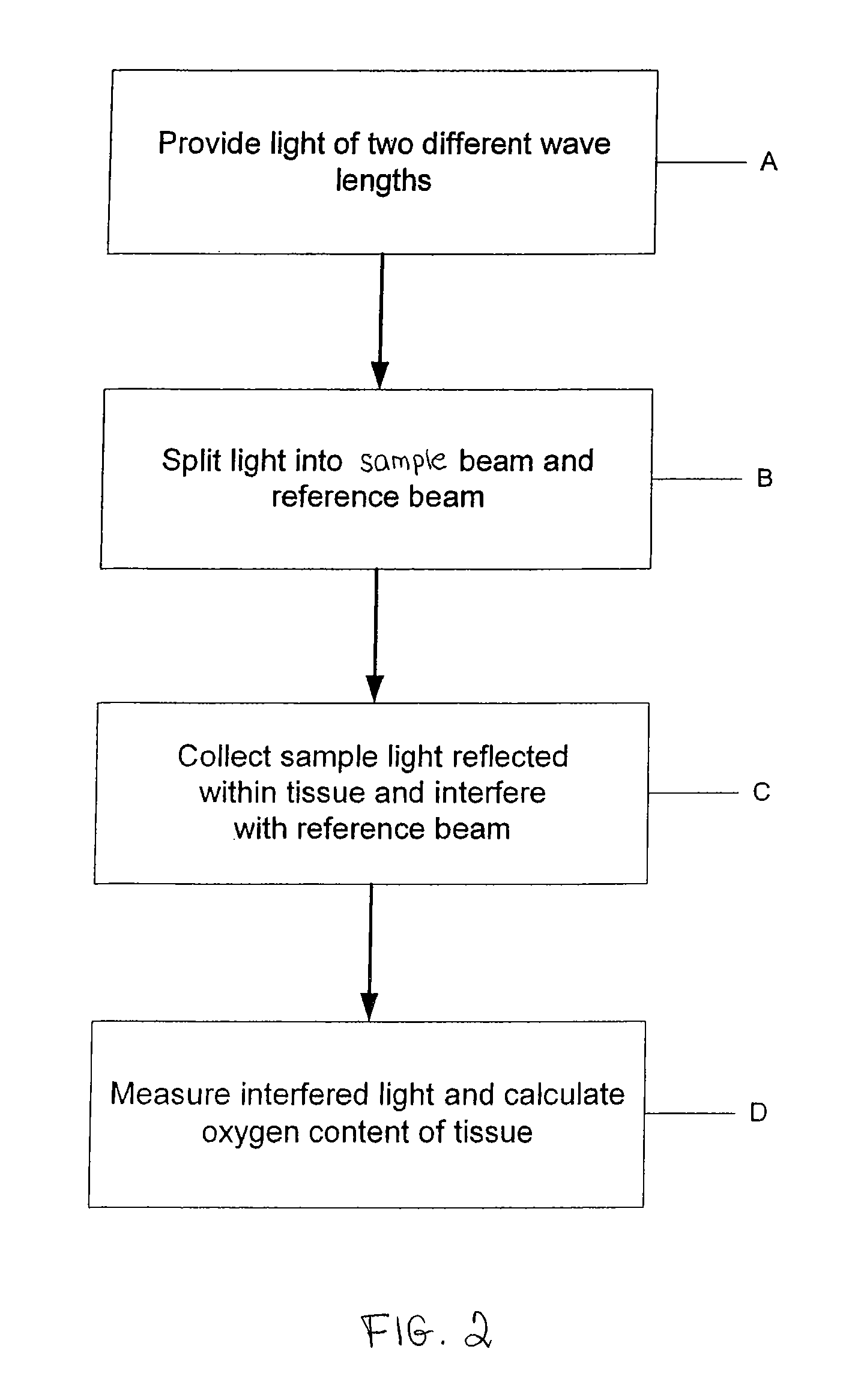
Method and apparatus for tissue oximetry
In accordance with the invention, the oxygenation of blood-profused tissue is measured by shining light into the profused tissue and analyzing the light reflected within the tissue. The light is reflected by cell walls in the tissue and is partially absorbed by hemoglobin in the blood. Since the extent of absorption is sensitive to the extent of hemoglobin oxygenation, measurement and processing of the reflected light provides a measure of the oxygenation of the blood. In one embodiment, the method is applied to measure the oxygenation of blood within the tympanic membrane (ear drum).
Owner:MASIMO CORP
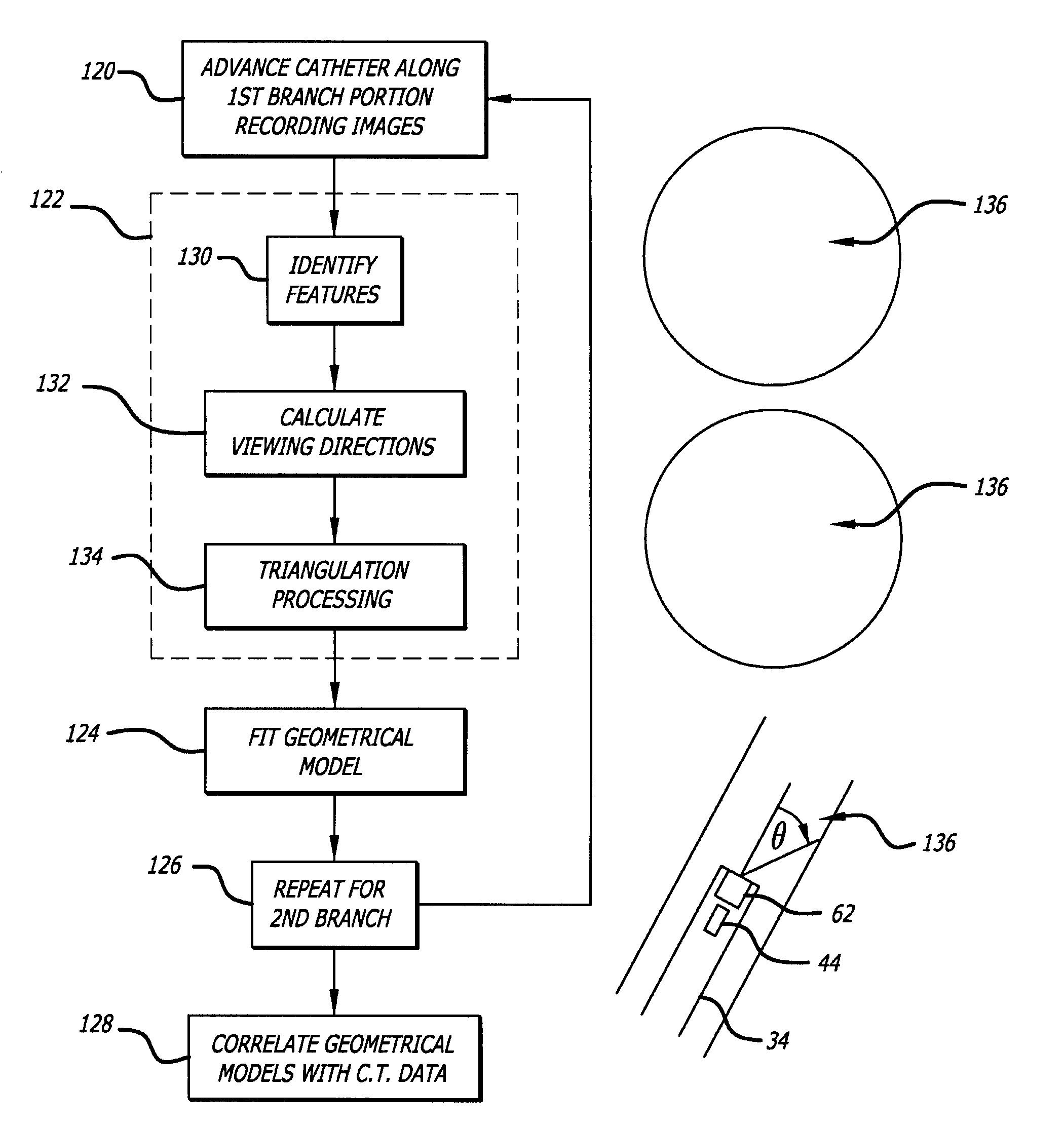
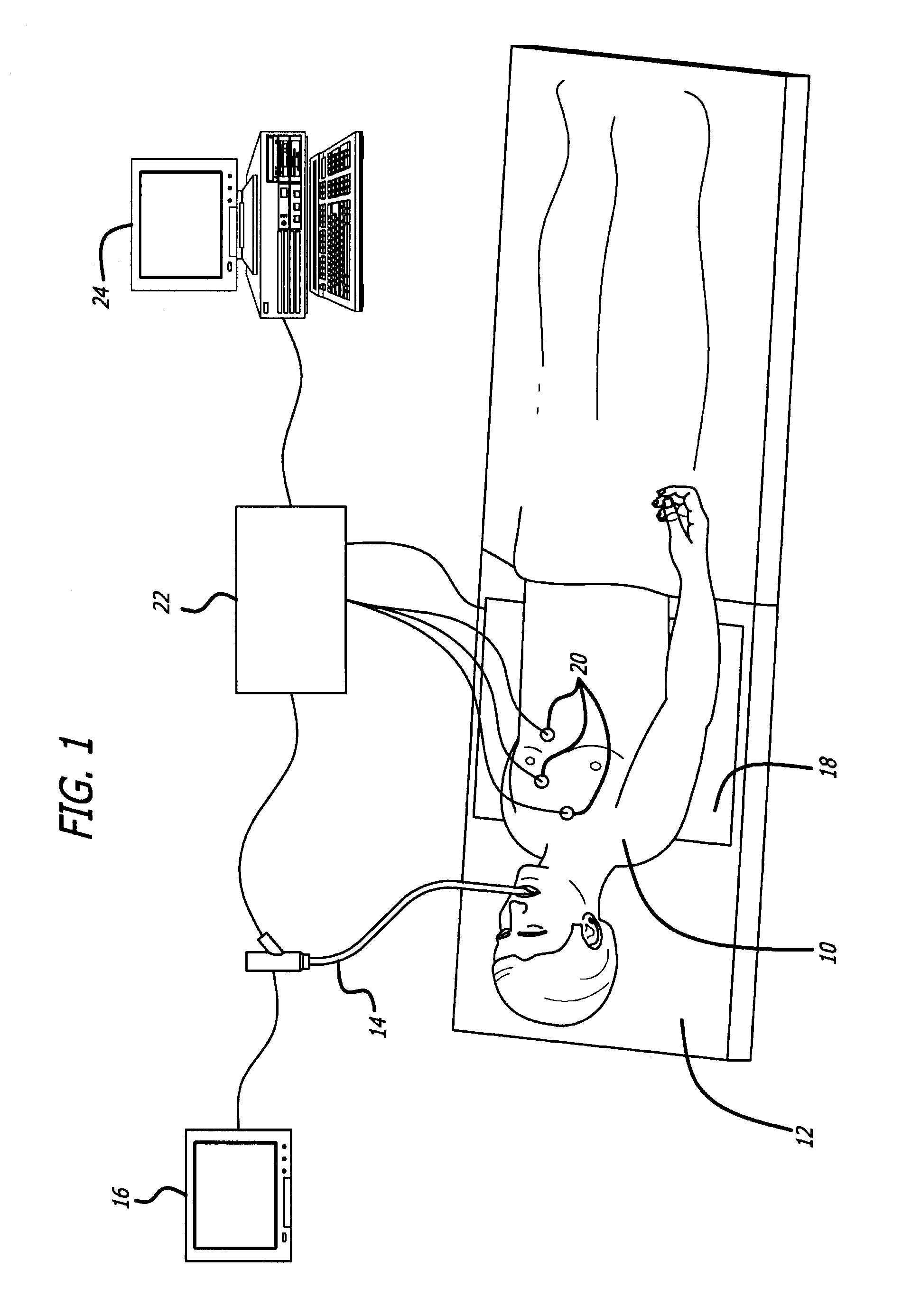
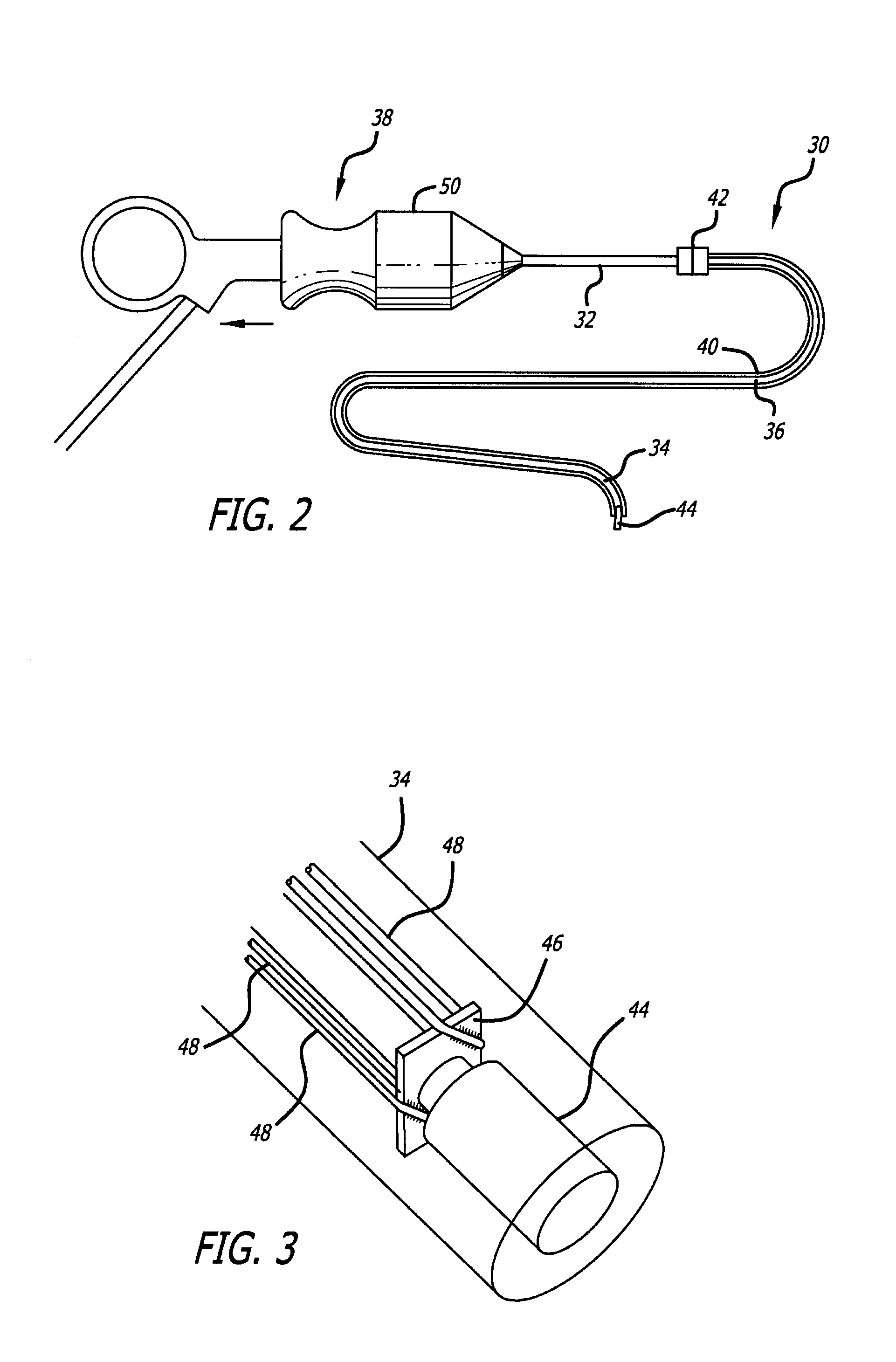
Endoscope structures and techniques for navigating to a target in branched structure
Systems and methods employing a small guage steerable catheter (30) including a locatable guide (32) with a sheath (40), particularly as an enhancement to a bronchoscope (14). A typical procedure is as follows. The location of a target in a reference coordinate system is detected or imported. The catheter (30) is navigated to the target which tracking the distal tip (34) of the guide (32) in the reference coordinate system. Insertion of the catheter is typically via a working channel of a convention bronchoscope. Once the tip of the catheter is positioned at the target, the guide (32) is withdrawn, leaving the sheath (40) secured in place. The sheath (40) is then used as a guide channel to direct a medical tool to target.
Owner:TYCO HEALTHCARE GRP LP
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com