Systems and methods for providing sensor fusion
a sensor and fusion technology, applied in bioelectric signal measurement, medical science, diagnostics, etc., can solve problems such as unnecessari alarms, system reliance on sensors to take potentially hazardous actions, and fail to take critical actions, so as to increase system specificity, reduce false alarms, and increase monitoring specificity
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
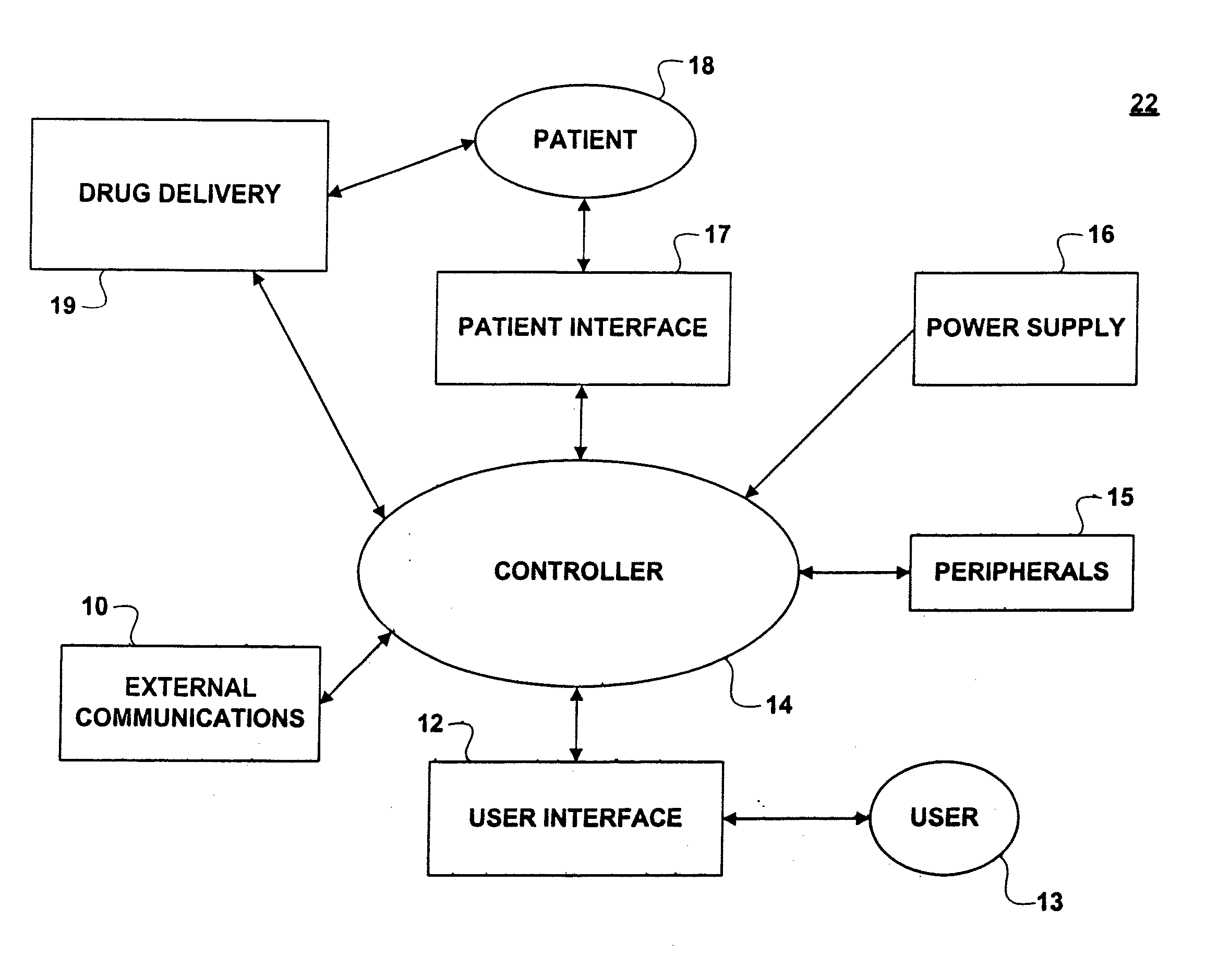
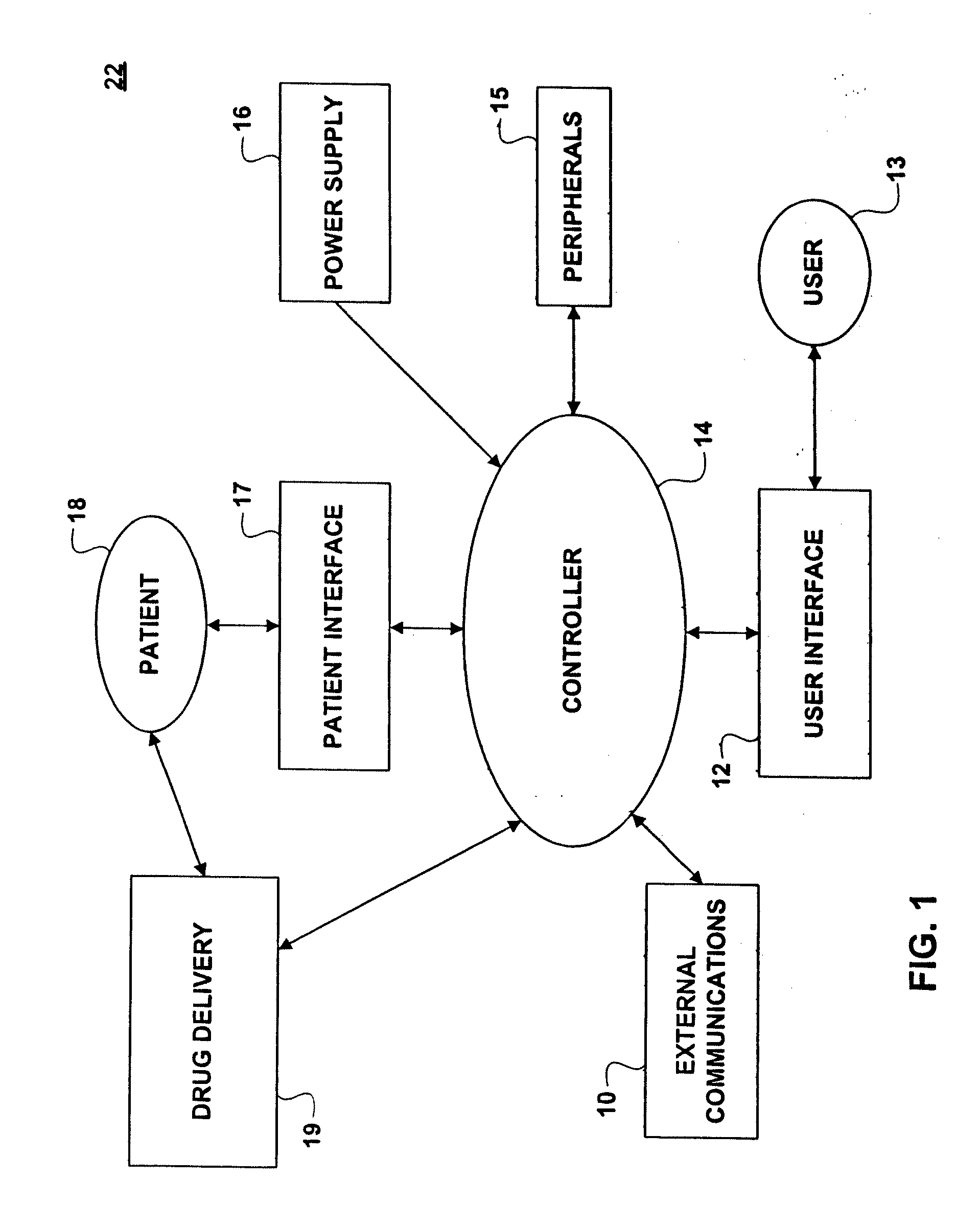
[0026]FIG. 1 illustrates a block diagram depicting a representative system in which the present invention can be incorporated. Sedation and analgesia system 22 includes user interface 12, software controlled controller 14, peripherals 15, power supply 16, external communications 10, pressure delivery 11, patient interface 17, and drug delivery 19, where sedation and analgesia system 22 is operated by user 13 in order to provide sedation and / or analgesia to patient 18. An example of sedation and analgesia system 22 is disclosed and enabled by U.S. patent application Ser. No. 09 / 324,759, filed Jun. 3, 1999 and incorporated herein by reference in its entirety. While sedation and analgesia system 22 is a representative system, the present invention can be incorporated in any system that can benefit from the incorporation of the natural relationships of patient parameters into a medical monitoring system.
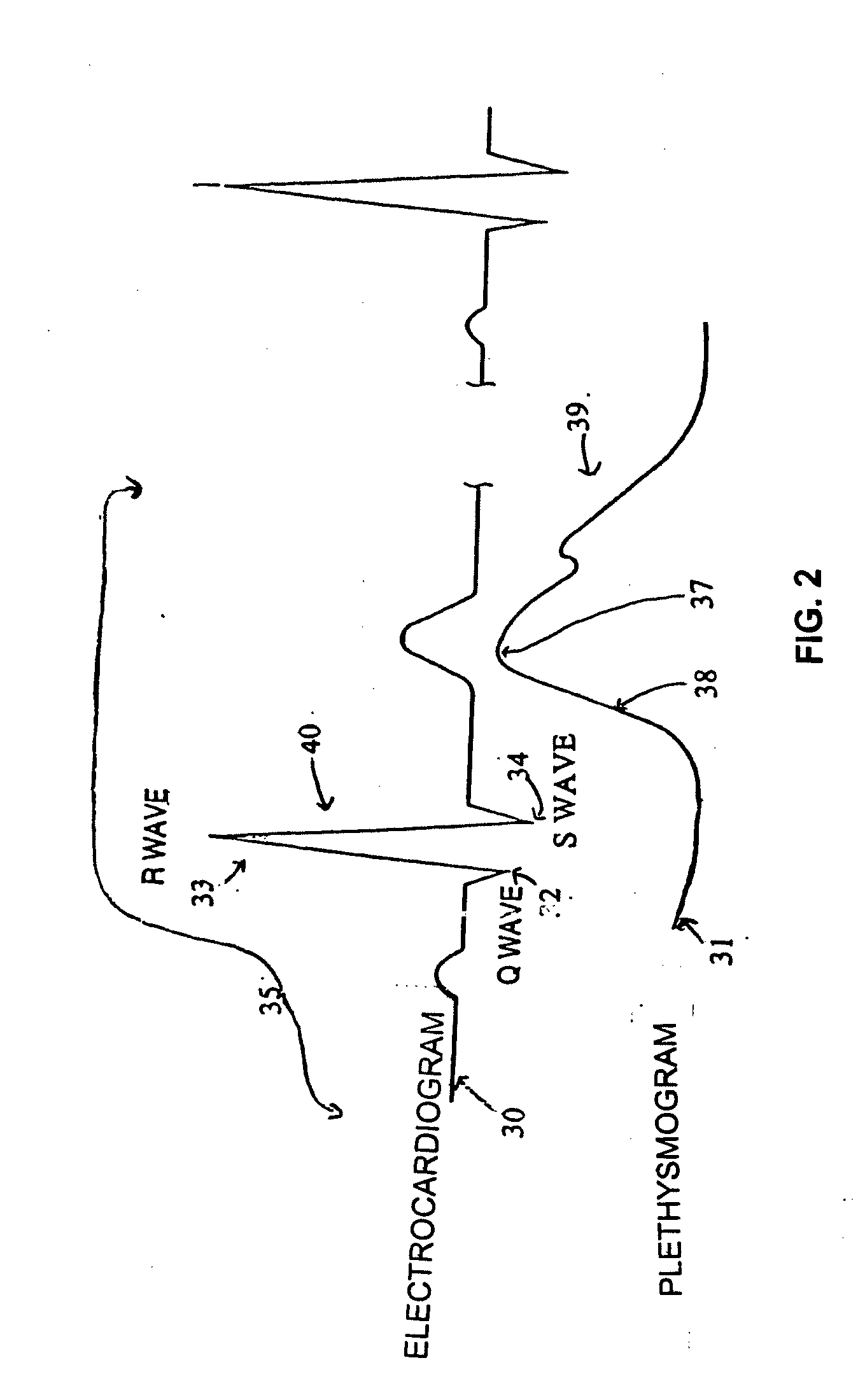
[0027]In the representative system of FIG. 1, patient interface 17 includes two or m...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com