System and method for management of health care services
a health care and management system technology, applied in the field of health care management system and management method, can solve the problems of increasing cost, increasing complexity, increasing complexity, etc., and achieves the effects of greater choice and freedom in accessing health care services, greater flexibility and portability of health care benefits, and greater transparency
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
[0031]Reference will now be made in greater detail to a preferred embodiment of the invention, an example of which is illustrated in the accompanying drawings. Wherever possible, the same reference numerals will be used throughout the drawings and the description to refer to the same or like parts.
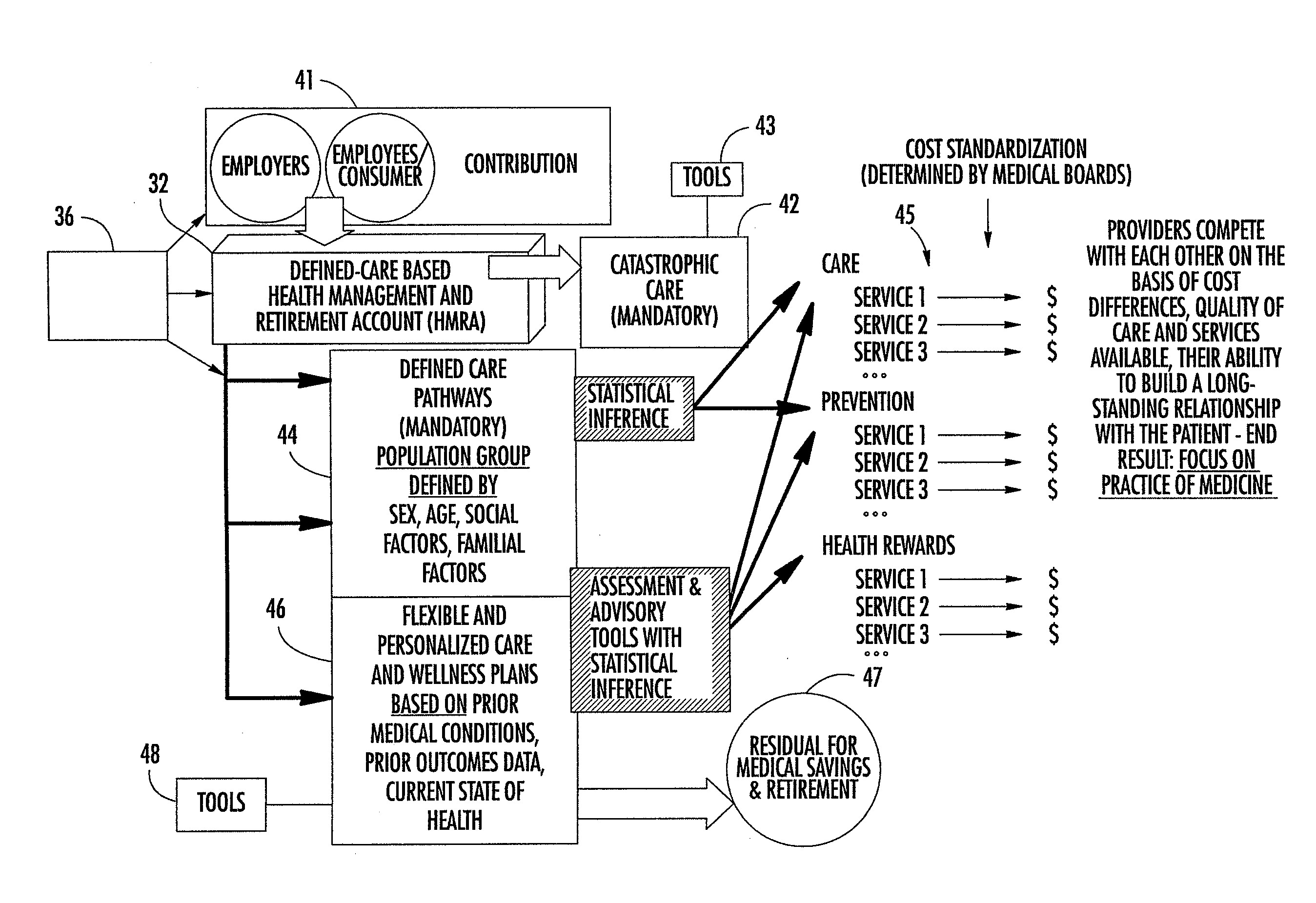
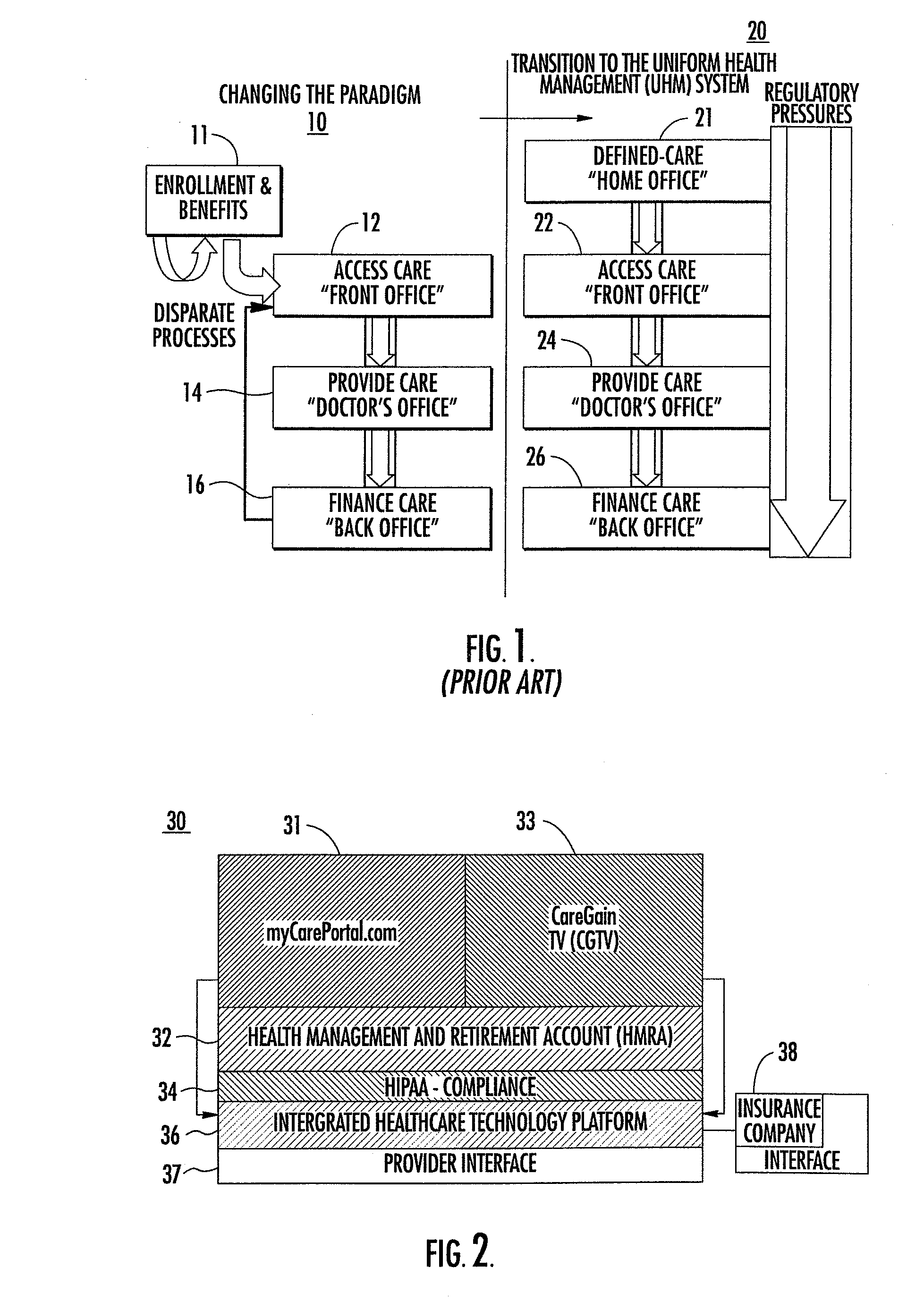
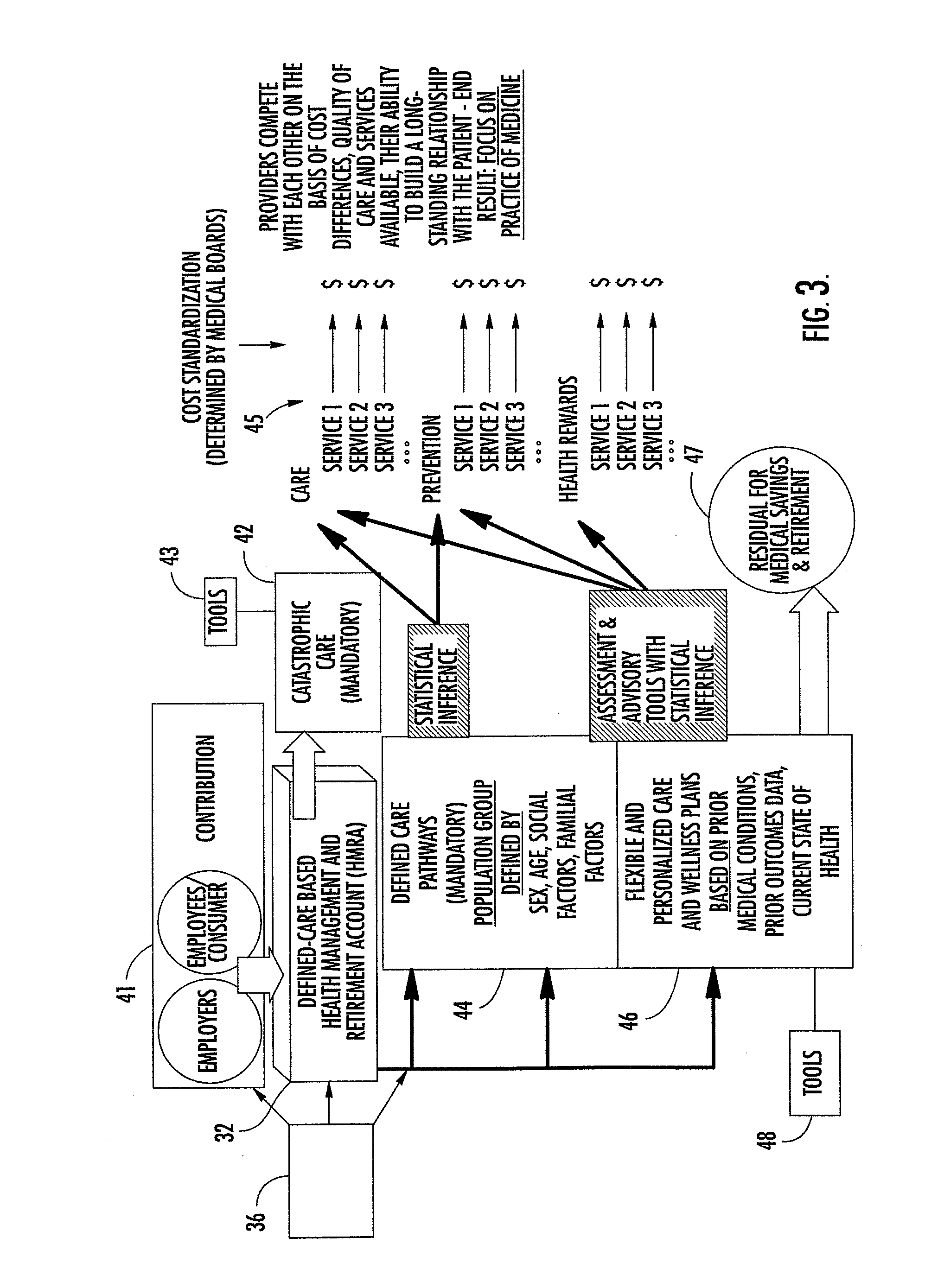
[0032]FIG. 1 illustrates a comparison of a prior art method for providing health care services 10 and uniform health management system 20 of the present invention. In the prior art method for providing health care services, enrollment and benefits 11 are disparate processes, which are performed by a patient's employer. Provide care “doctor's office”14 communicates via paperwork or telephone with an insurance company which provides an access care “front office”12 and finance care “back office”16 for payment of the physician's services.
[0033]Uniform health management (UHM) system 20 of the present invention defines a consumer-centric healthcare model, consistent with the new movement towards...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com