Fixation method for a nasal septum sensor for measuring medical parameters
A nasal septum and detector technology, applied in the direction of sensors, diagnostic recording/measurement, applications, etc., can solve the problems of not being able to install sensors, and achieve the effect of preventing pressure sores or tissue necrosis, and preventing signal artifacts
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
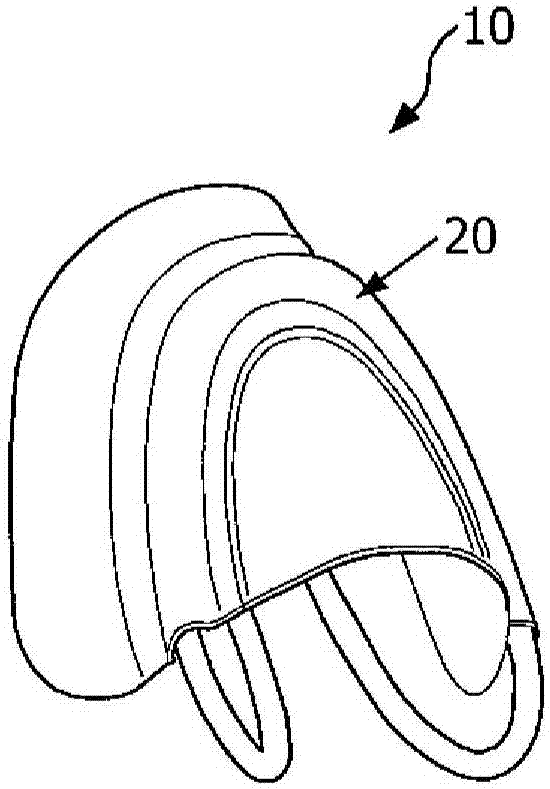
[0044] By providing a system and method for tightly attaching the device to the nasal septum without applying excessive pressure on the tissue, the described system and method overcome the above-mentioned problems. The nasal septum has several benefits for measuring SpO2 and PPG signals because the nasal septum is an extremely thin and well-perfused part of the body and can be detected according to the transmission geometry, in contrast to the reflection geometry utilized by the forehead probe. The nasal septum as a measurement site also has the benefit of being one of the last well-perfused sites when the patient enters a state of shock. Therefore, several systems and methods for stably fixing the blood oxygen sensor to the nasal septum are described herein.
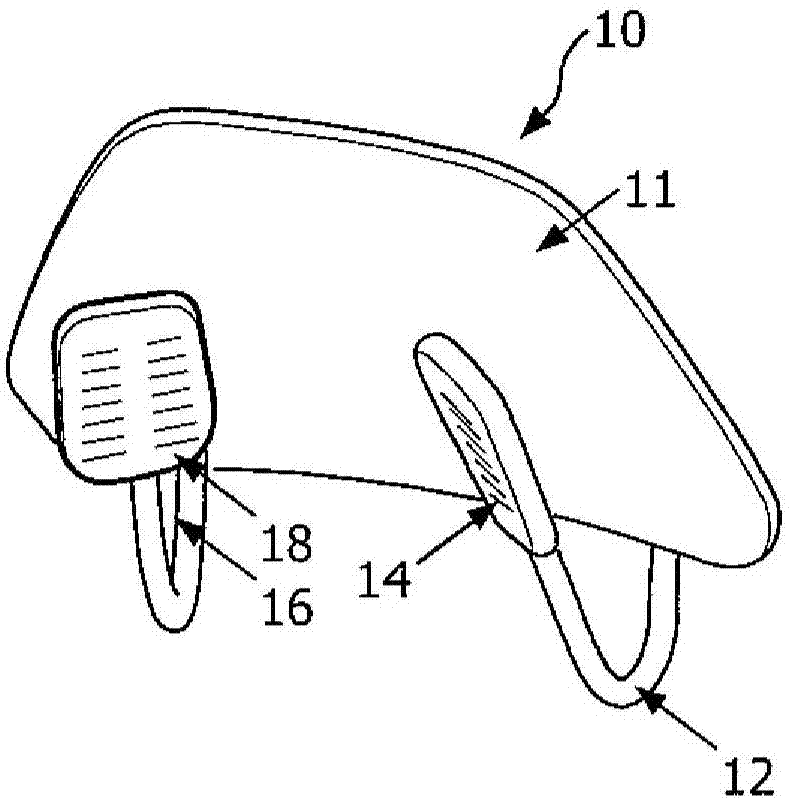
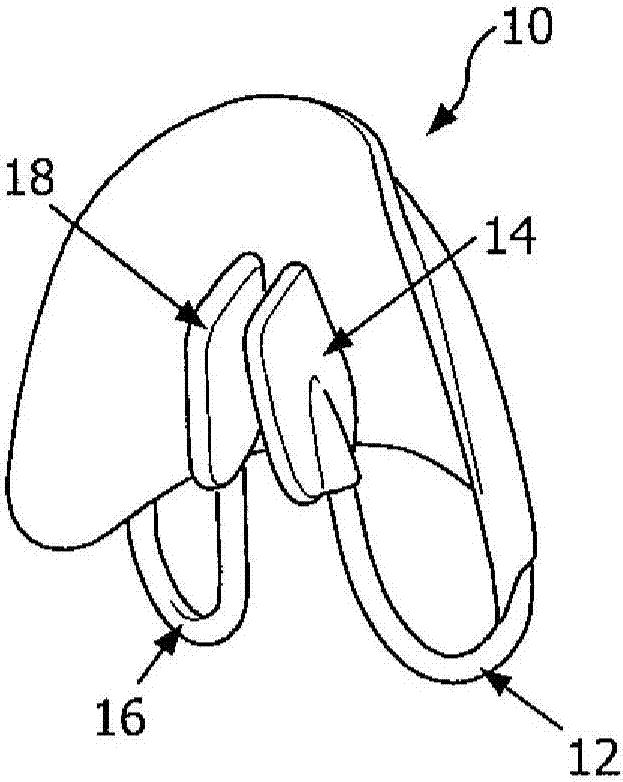
[0045] Figure 1A to Figure 1D Illustrated is a septal pulse oximeter 10 according to one or more aspects described herein, which can be attached to the nasal septum of a patient in a stable manner. Figure 1A The oximeter ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com