Pain is the single most common symptom for which patients seek medical treatment and there is currently no objective method available for its measurement.
The inappropriate desire for opiate drugs probably accounts for a significant fraction of pain therapy prescription drug demand.
Yet absent any objective method of establishing the existence of “pain”, the physician has no objective standards by which to prohibit such demand, and frequently feels ethically bound to take claims of pain at face value, or risk accusation of ineffective care and inhumane treatment.
For example, patient complaints of subjective numbness are often not detectable on clinical examination because present diagnostic methods are not sensitive enough to detect the early stage sensory impairments of such neurological disorders as nerve root entrapment or peripheral neuropathy.
As a result, patients with these types of neurological disorders cannot be diagnosed until the disorder progresses to a detectable level.
Basic psychophysical methods for the estimation of pain sensibility have a long history of questionable clinical relevance.
No studies have been able to demonstrate a relationship between pain threshold and the underlying pain state; in fact, pain threshold measurement procedures are unable to quantitatively demonstrate analgesic states engendered by clinically proven drugs as, for example, morphine (for review, see Chapman et al.
Furthermore, the method suffers from major disadvantages when transferred to the clinical situation where the test subject, who may suffer excruciating pain of endogenous pathological origin, is less able to attend to the minor sensory nuances of the pain threshold.
Tolerance methods using these techniques, unlike threshold methods, also evoke some not inconsiderable anxiety and apprehension on the part of the subject, which may resemble the anxiety of the pain-suffering patient.
However, studies have shown that tactile stimulation interferes with that aspect of cutaneous tolerance limit responsive to internal pain interference and thus methods that utilize a contact stimulus invalidate pain tolerance level results.
Therefore, this apparatus cannot be used to accurately measure pain tolerance.
However, most radiant heat pain stimulators have been designed to measure the pain threshold level and thus are prone to the disadvantages inherent in such measurement.
Thus, pain tolerance results obtained with the instrument are invalid.
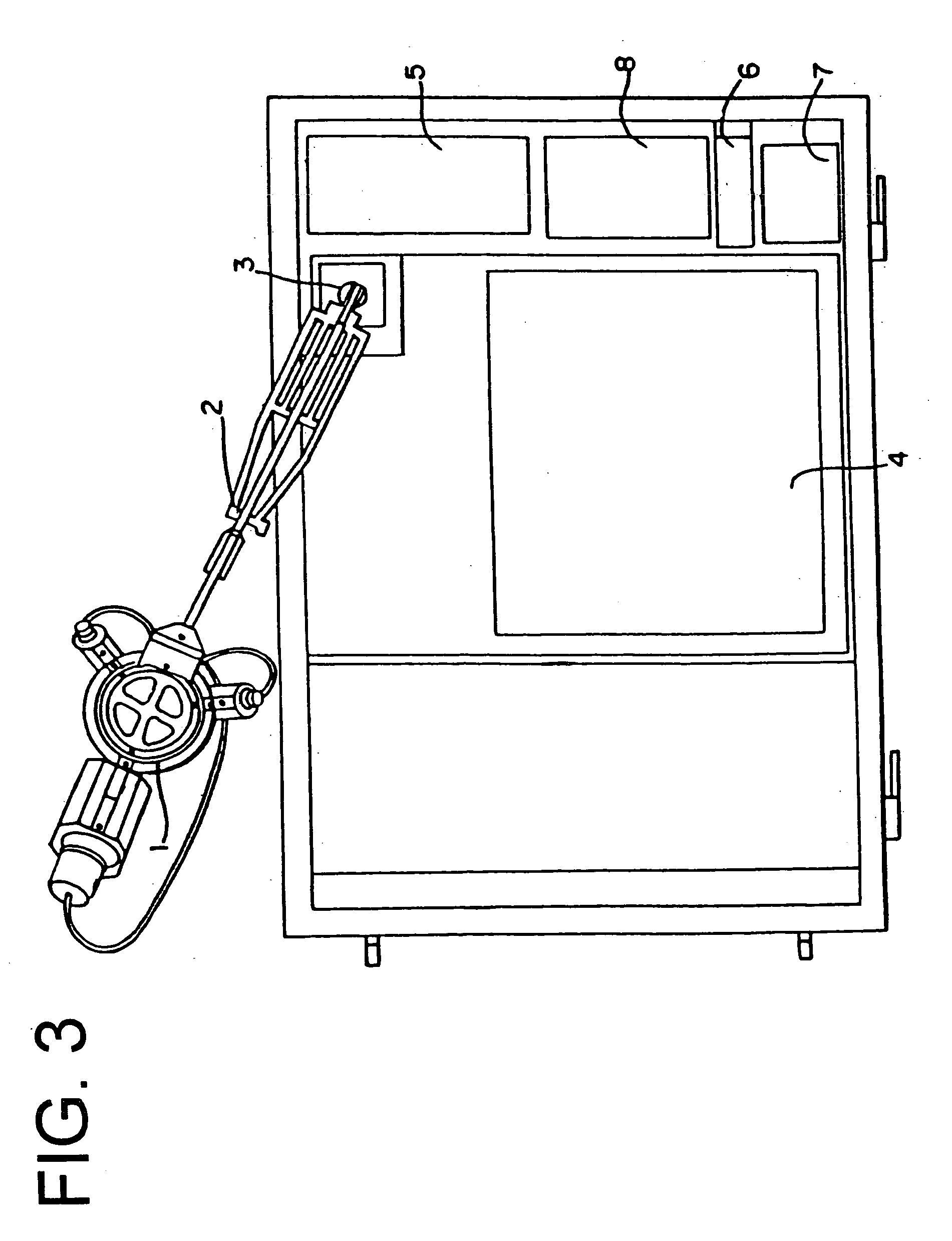
The concept prototype was a nonportable, electromechanical device that did not allow for automatic data acquisition.
Unfortunately, available sensor response characteristics are largely inadequate to this task.
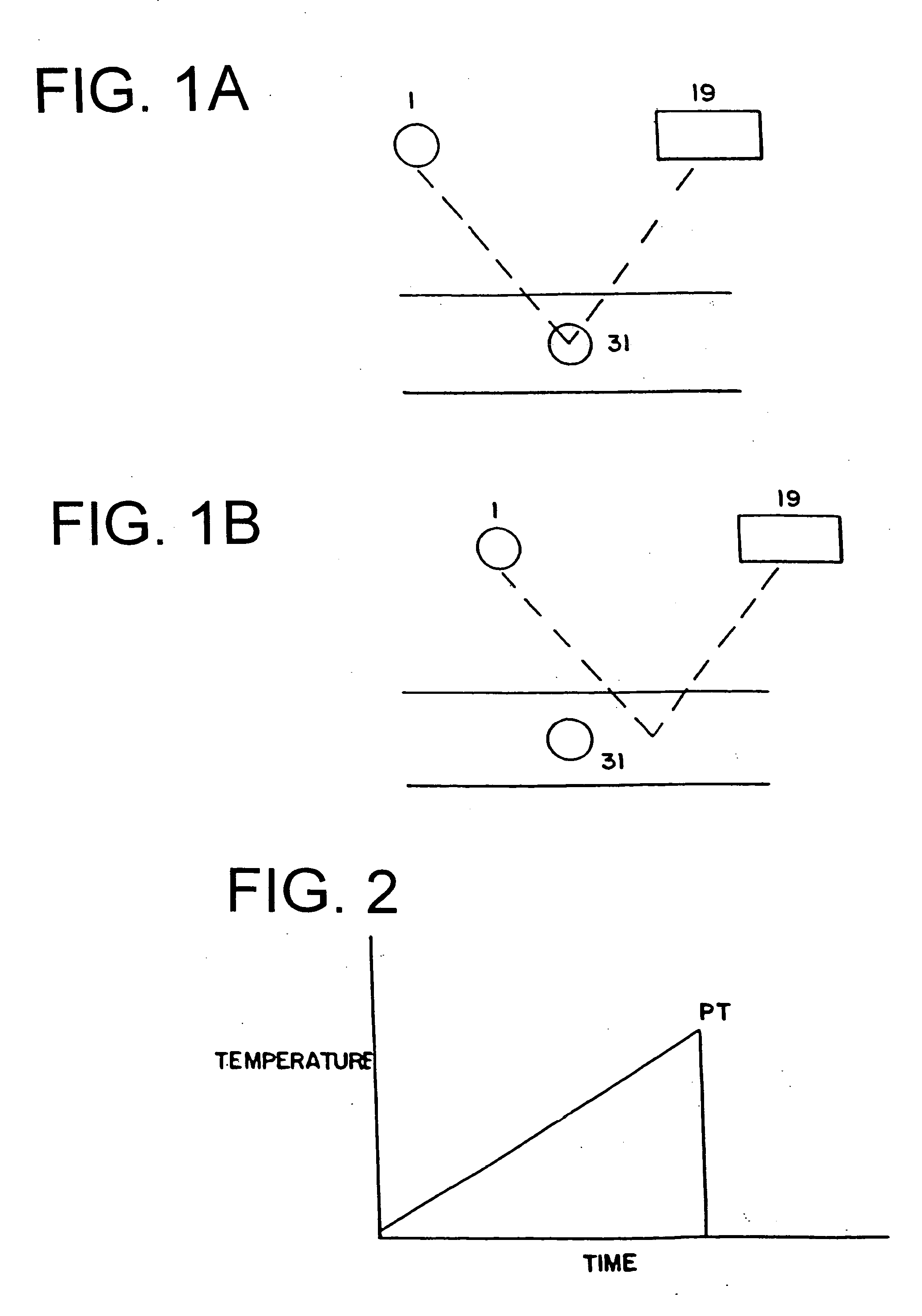
Thus, should a temperature sensor within the target be used to feedback control, for example, a motor-drive positioning mechanism on which a radiant heat projector (emitter) is mounted, whereby feedback from the sensor is used to control projector position, either toward or away from the target, it is found that accurate, rapid and responsive positioning of the emitter by the motor drive cannot be achieved because the sensor response time is invariably too slow, having too much inertia or resistance to change.
Verbal descriptor scales are commonly employed for pain assessment by asking the patient to rate their present pain on a numerical rating scale from one to one hundred or some other number: for instance, the NRS-101 asks the patient to scale their pain between one and a hundred and one but verbal enquiry has the serious disadvantage that the questioner (nurse or doctor) inevitably conveys expectation by voice, tone, facial expression, and demeanor, which will inevitably influence the patient's response.
However, when used to ask the patient to rate their present degree of pain without regard to any earlier response they may have made, this property of category scales proves somewhat of a disadvantage—since it is hoped in this situation that the patient's present response will be uninfluenced by prior responses.
These numbers are of course completely arbitrary in quantity though not in rank order, and hence parametric statistics cannot be used to compare scores.
The software driving this accessory is inherent to the thermode program and cannot in its present form be modified to stand alone as a patient assessment tool.
The Medoc device is hardware limited, in that it administers only one PQ test (the COPAS), and only in conjunction with the sensory testing protocol, and only by employing the ‘slide switch’ interface.
The BPM device is likewise by design and construction limited to its present purpose and takes several minutes to complete all the questionnaire forms.
 Login to View More
Login to View More  Login to View More
Login to View More