Straight intramedullary fracture fixation devices and methods
a fixation device and intramedullary technology, applied in the field of devices, tools and methods for providing bone reconstruction and reinforcement, can solve the problems of multiple traumas and resultant fractures, large number of non-life-threatening fractures, and significant bone fractures
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
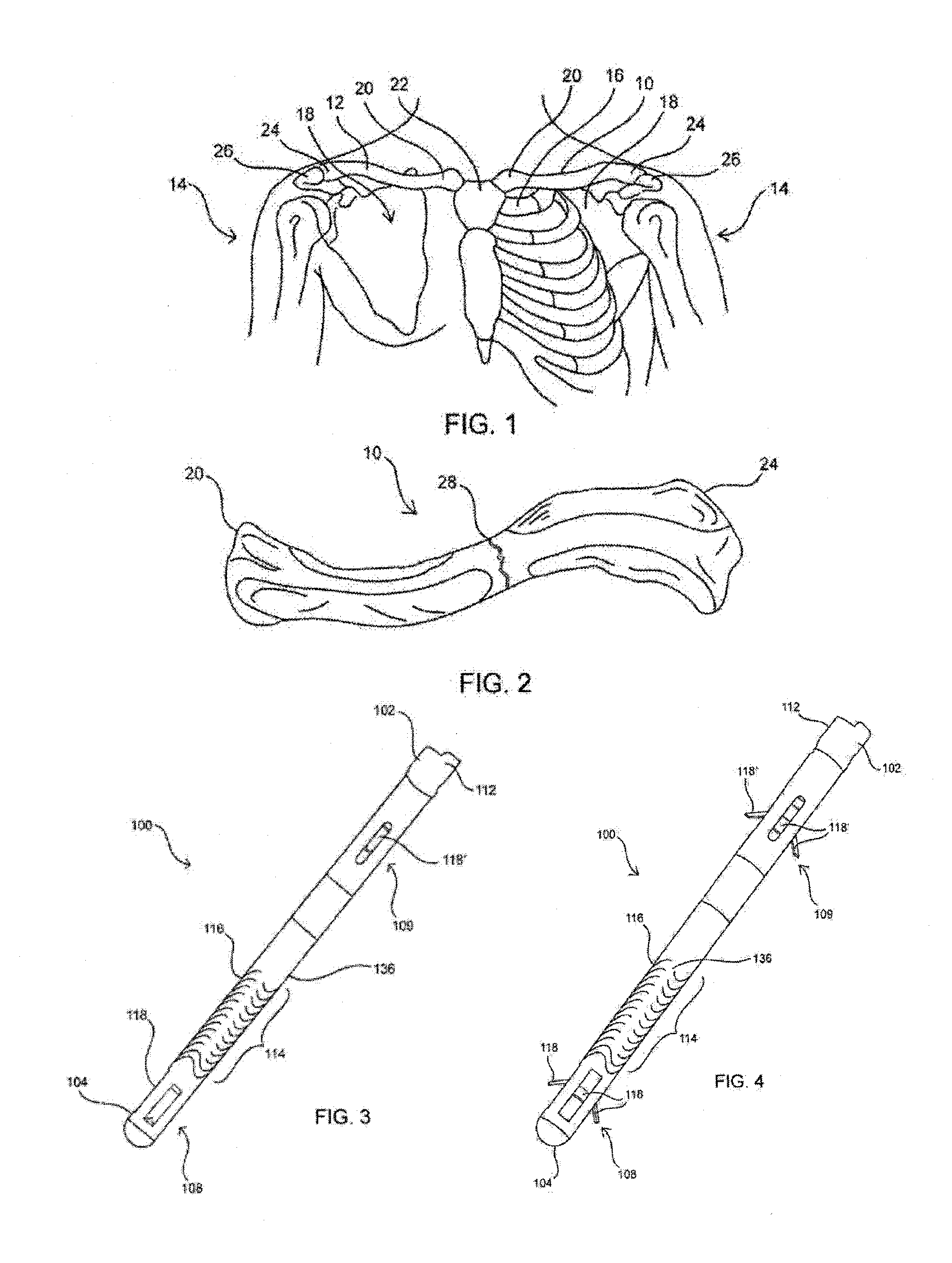
first embodiment
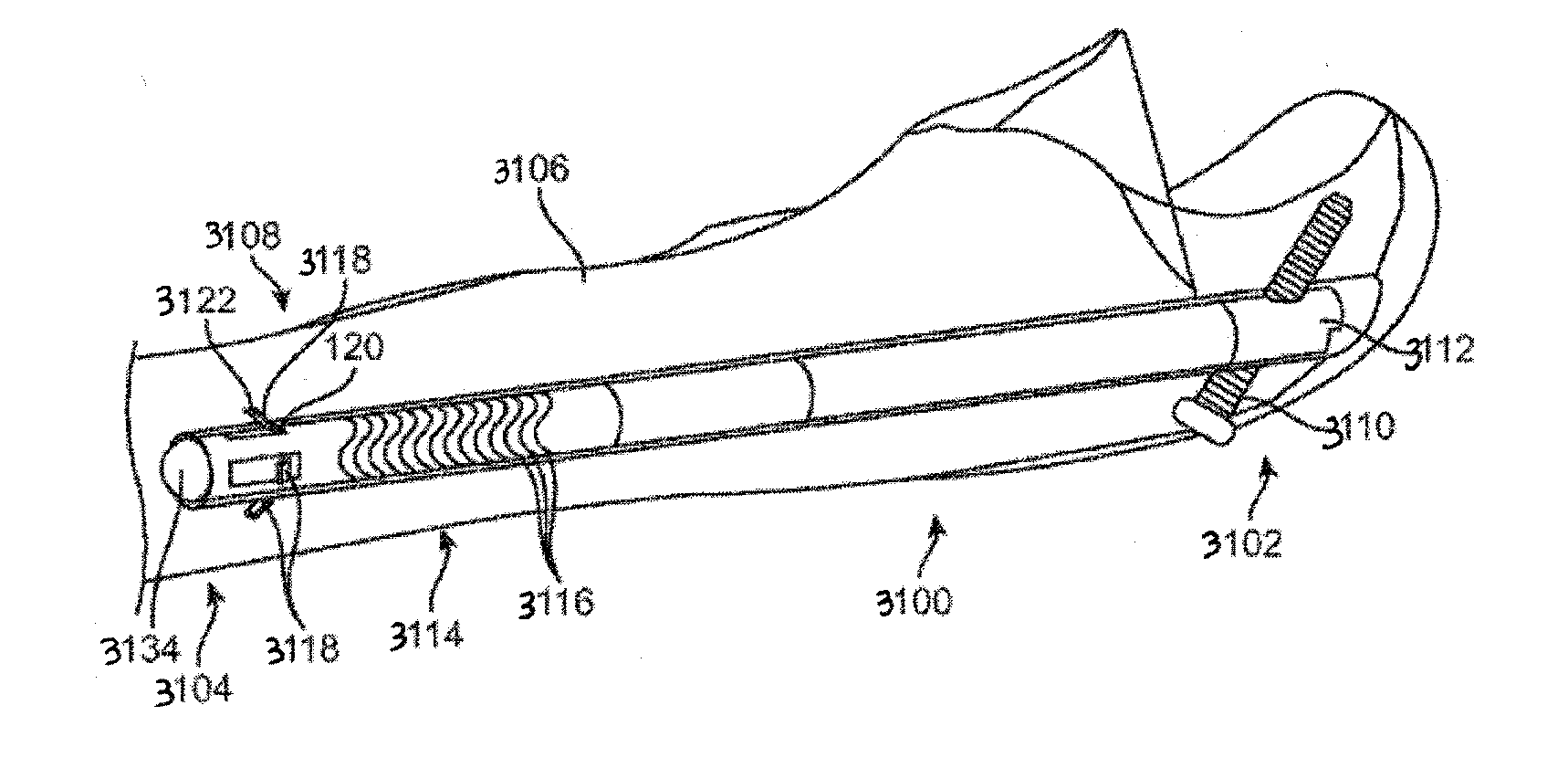
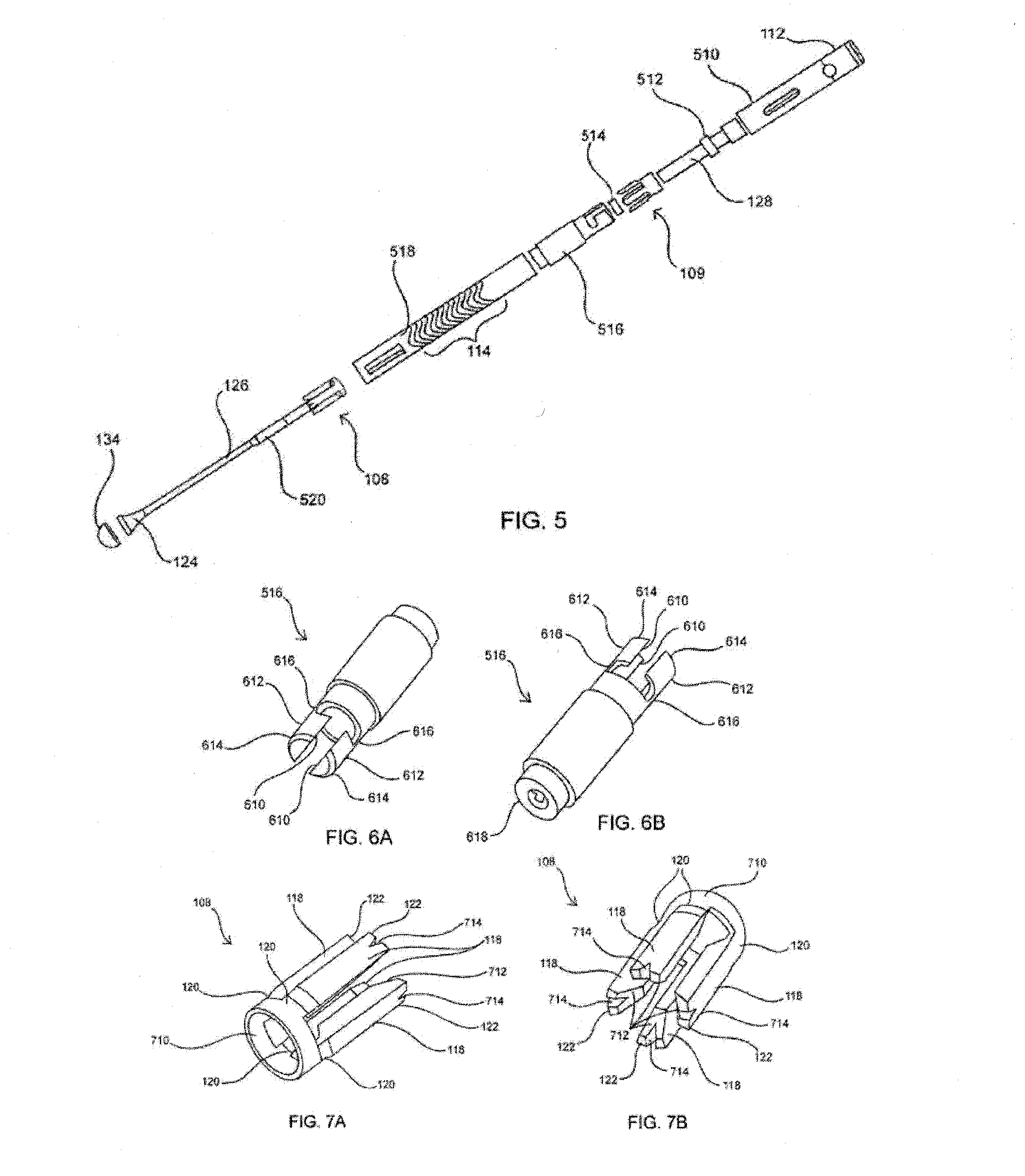
[0250]In a first embodiment, to implant bone fixation device 100 in clavicle 12, an incision is first made at the fracture 28, and tissue is retracted if needed to access the fracture. Fracture 28 is then distracted to gain access to the medial end of the lateral portion of the bone. A channel may then be drilled axially through the lateral portion of the bone from fracture site 28 outward toward the lateral end 24 until it surfaces at the lateral end as shown. A guidewire, such as a K-wire, may first be driven anterior to posterior thereby tenting the posterior skin and the drill guided over the guidewire anterior to posterior in the lateral clavicle segment.
[0251]A second incision may be made where the channel exits lateral end 24 of clavicle 12 in order to access the exit point. A guide wire may then be placed through the second incision and into the lateral exit point of the channel created in the lateral portion of clavicle 12. The guide wire may then be fed medially through th...
second embodiment
[0254]In a second embodiment, to implant bone fixation device 100 in clavicle 12, an incision is first made at the fracture 28. The patient may be positioned in the “beach chair” position or any other suitable position for surgery. The incision is made at the front (anterior side) of the patient adjacent to the fracture. Tissue is retracted if needed to access the fracture and the fracture 28 may then be distracted or elevated to gain access to each of the segments of the bone. The medial segment and lateral segment are then both prepared for the insertion of the device by creating a channel within them.
[0255]Any suitable combination of tools may be used to create the channels in both the medial segment and the lateral segment of the clavicle. The tools may include hand tools or power tools. The tools may also include awls, drill bits, guidewires, or any other suitable tools to create a channel within bone. The awls may be curved awls, straight awls, and / or malleable awls (i.e. the ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com