Lamina implant and method
a technology of lamina implants and implants, applied in the field of lamina replacement, can solve the problems of reducing the usefulness of spinal surgery, creating an unnatural state of the neck, and high risk of adjacent level segment instability,
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
[0017]The detailed description set forth below in connection with the appended drawings is intended as a description of presently-preferred embodiments of the invention and is not intended to represent the only forms in which the present invention may be constructed and / or utilized. The description sets forth the functions and the sequence of steps for constructing and operating the invention in connection with the illustrated embodiments. It is to be understood, however, that the same or equivalent functions, features, and sequences may be accomplished by different embodiments that are also intended to be encompassed within the spirit and scope of the invention.
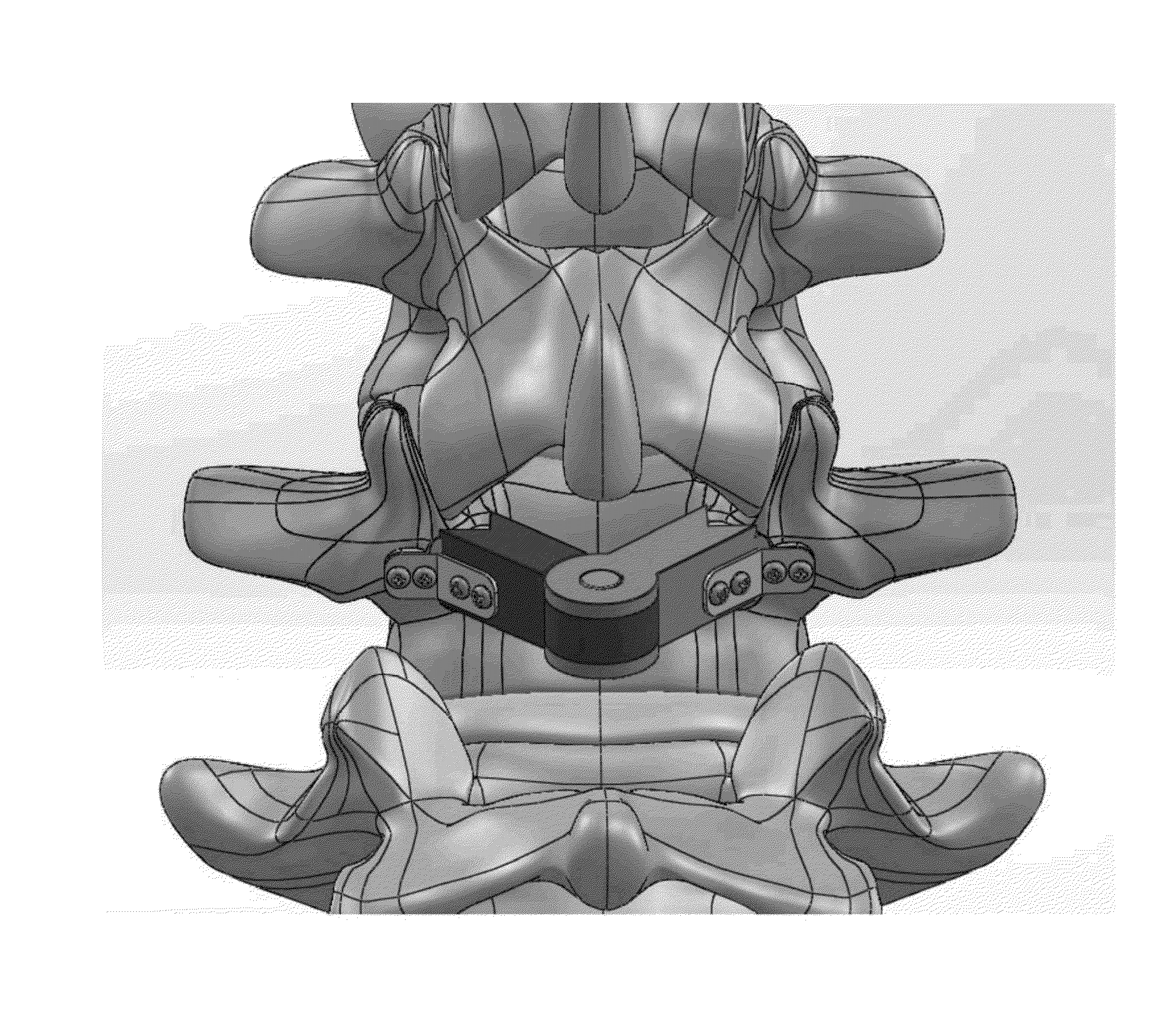
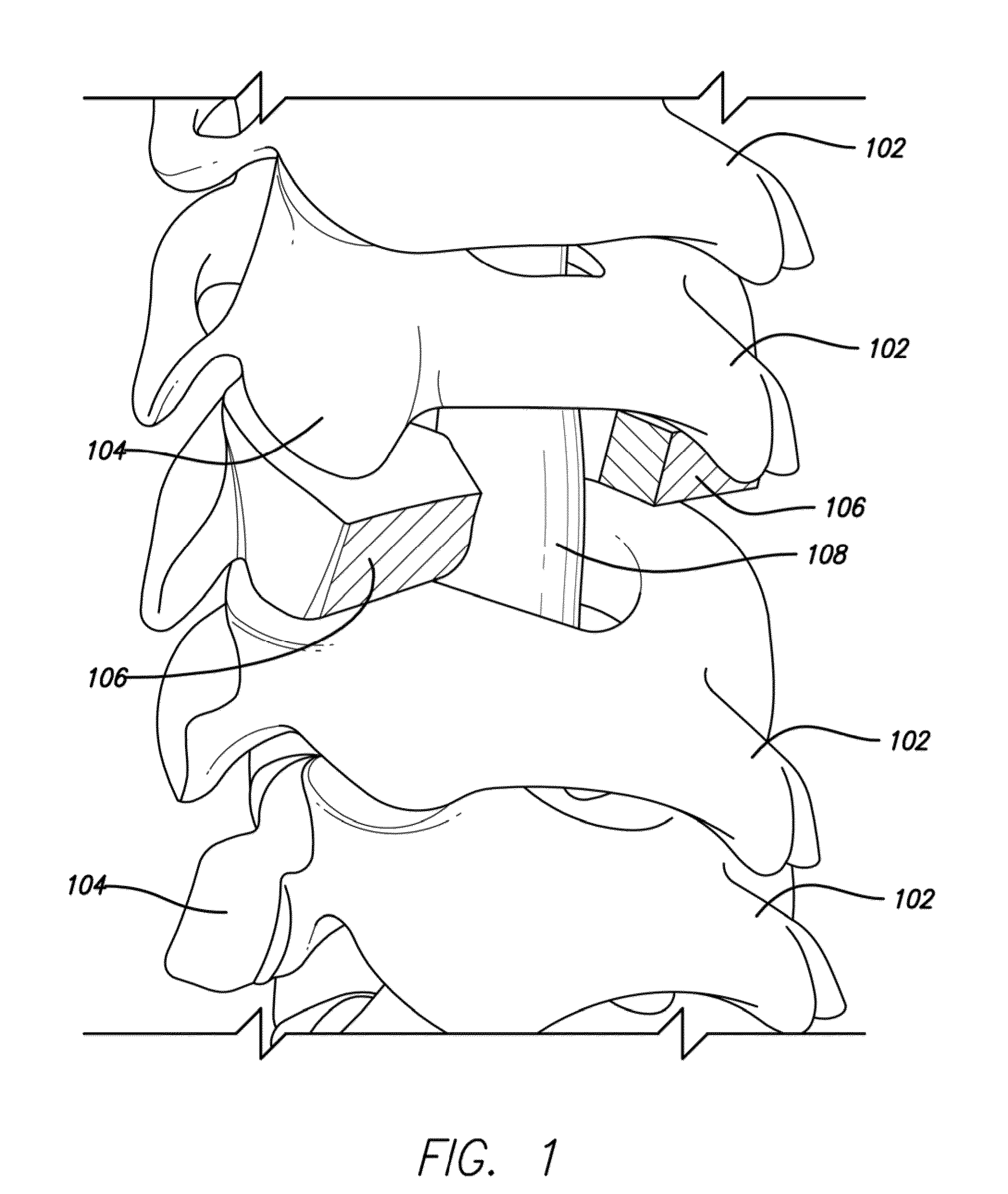
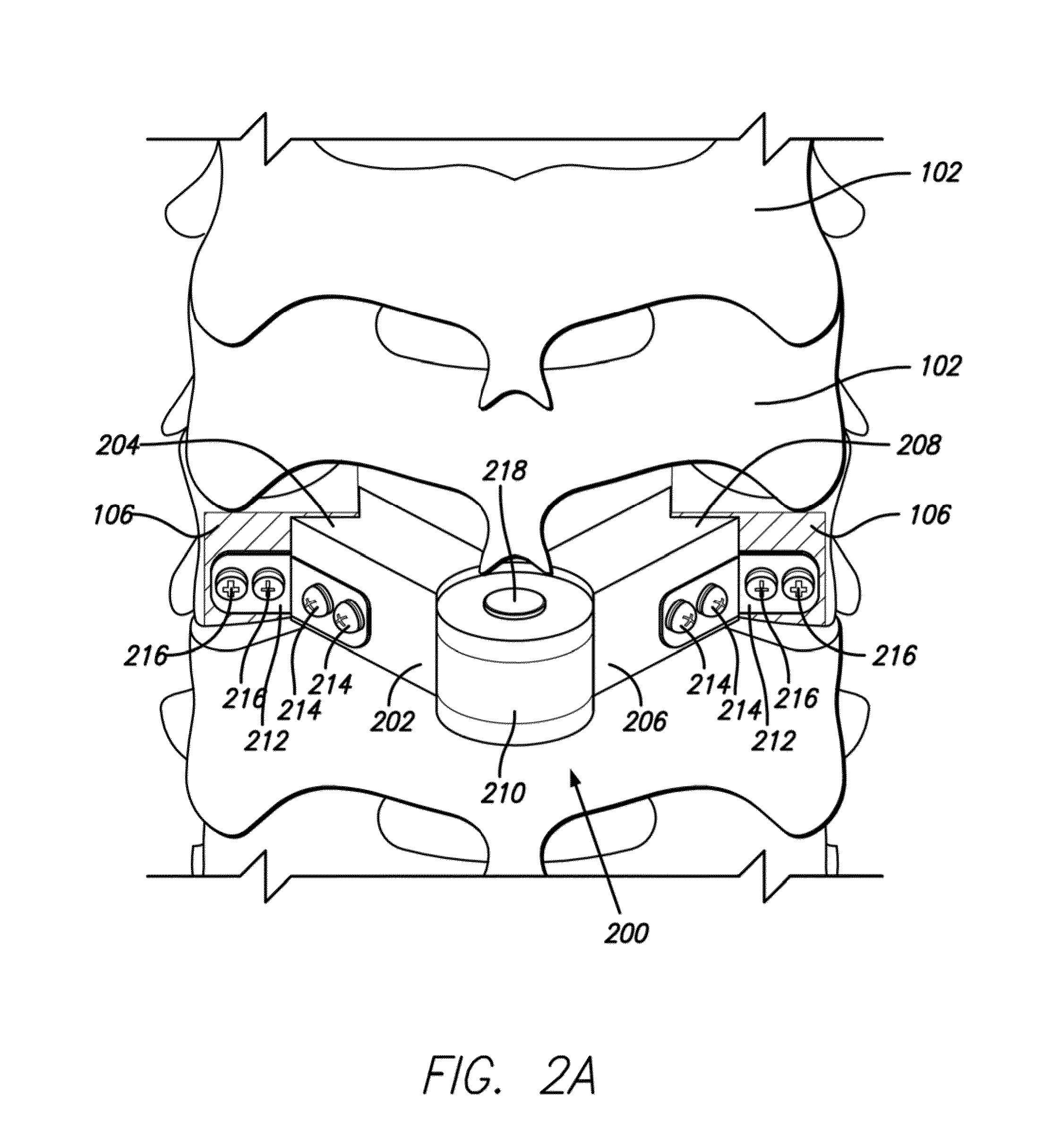
[0018]The present invention represents a novel implant and technique for the restoration of the lamina after cervical decompression or lumbar decompression. As seen in FIG. 1, when a surgeon performs a cervical or lumbar laminectomy by removing the lamina 102 of a spine 100, a gap is formed. In one embodiment of the present ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com