Implantable prosthesis
a prosthesis and implant technology, applied in the field of implantable prostheses, can solve the problems of recurrence of defects, postoperative pain for patients, and tension at the anchoring locations between fabric and tissu
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
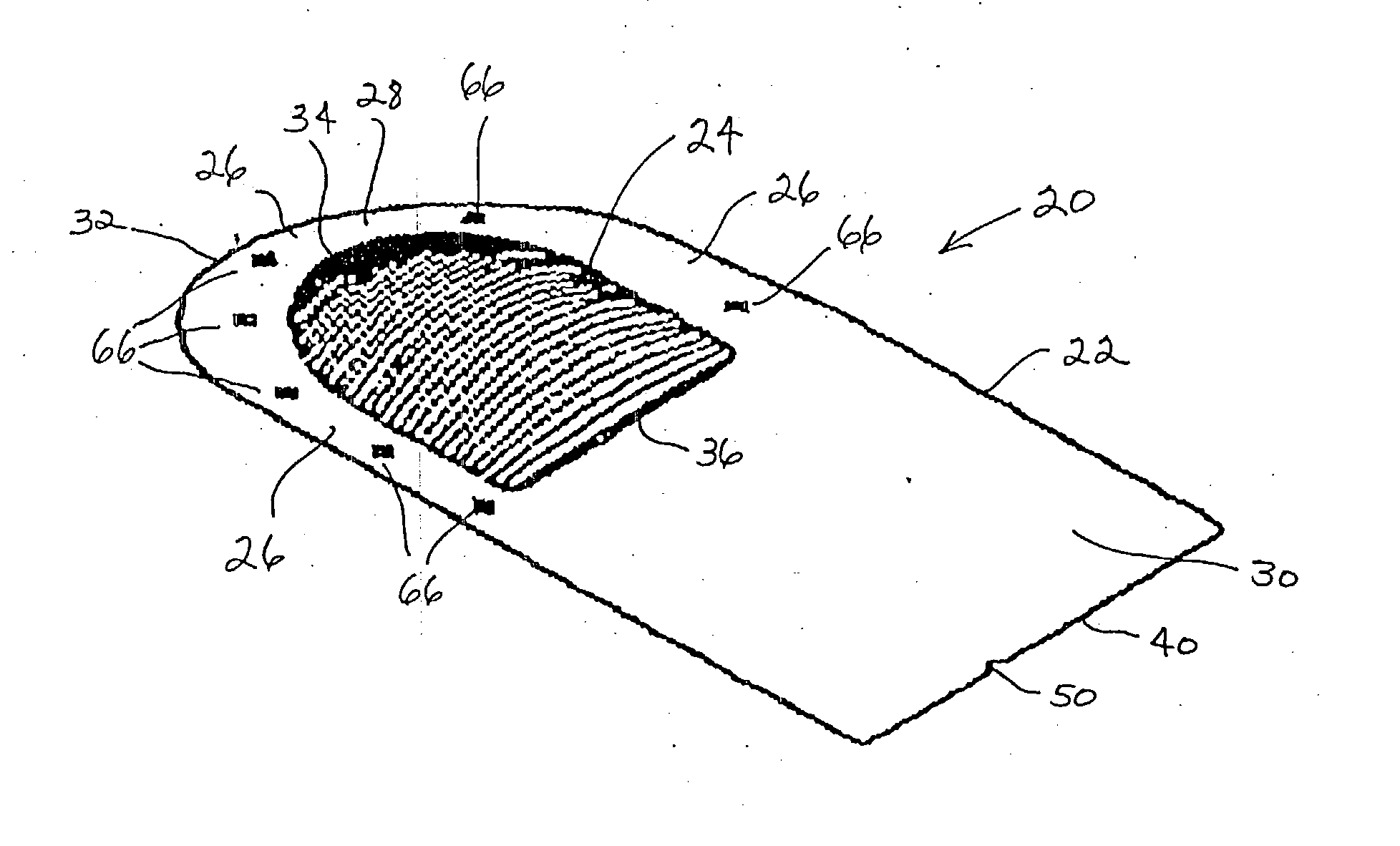
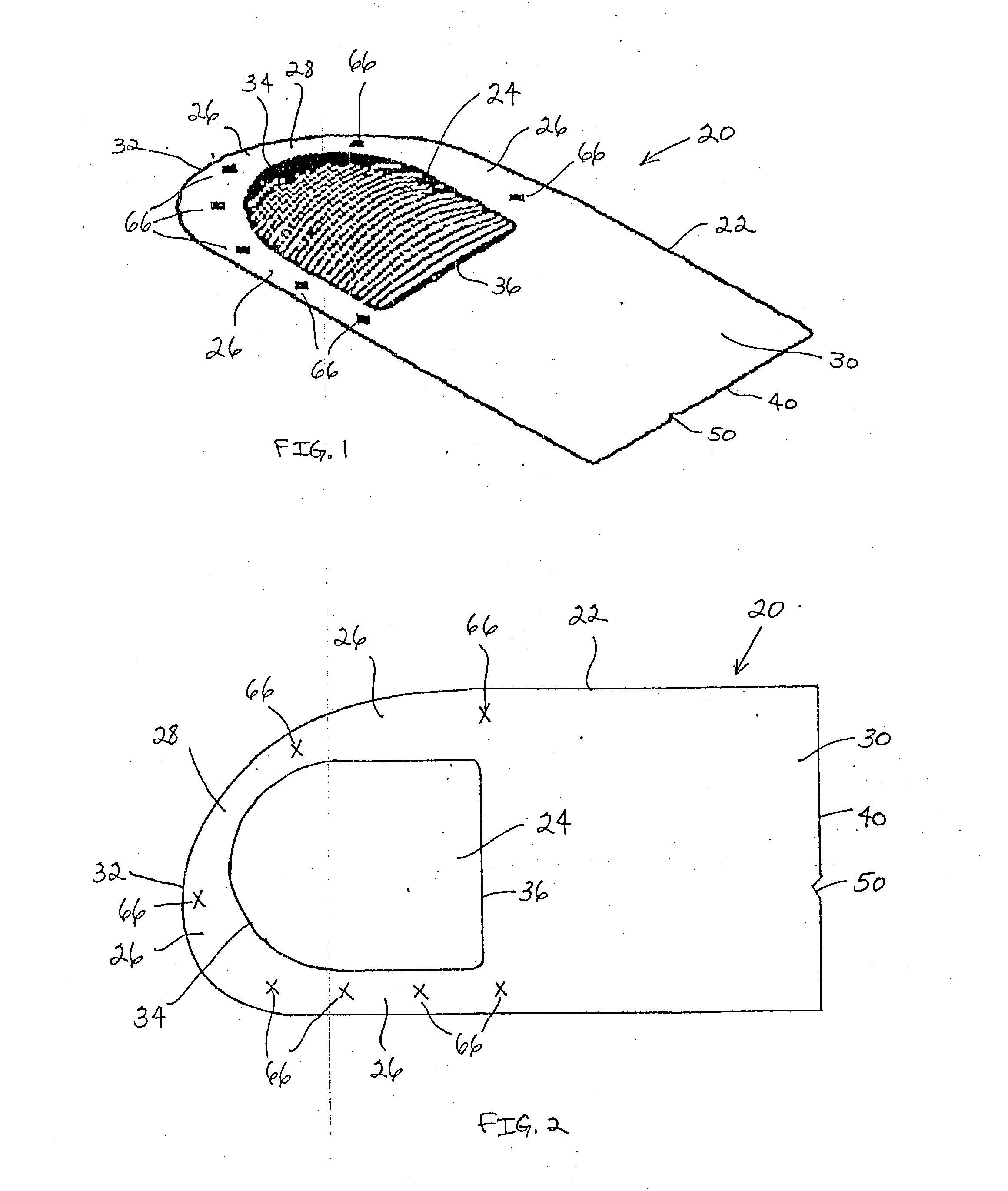
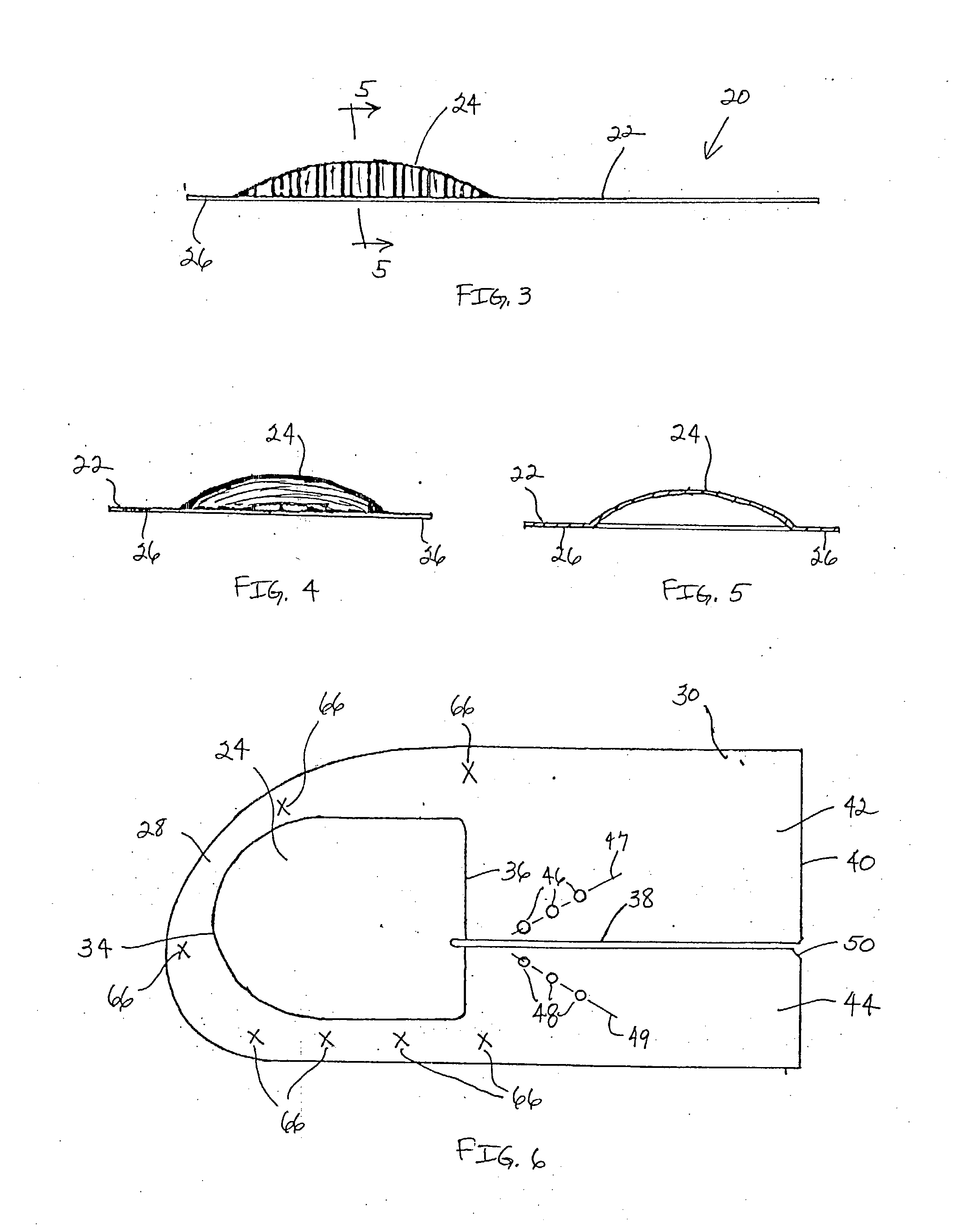
[0027] FIGS. 1-5 illustrate one embodiment of an implantable prosthesis for repairing an anatomical defect, such as a soft tissue or muscle wall defect. The prosthesis is configured to reduce the likelihood that an applied force at the repair site, such as due to intraabdominal pressure or tissue shrinkage, can lead to detrimental effects associated with tension at the anchoring locations between the prosthesis and host tissue and / or contraction of the prosthesis. In this regard, the prosthesis may be configured to limit the amount of tension at the anchoring locations caused by the application of a force or pressure to the prosthesis and / or contraction of the prosthesis. Alternatively, the prosthesis may be configured to compensate for contraction of the prosthesis due to tissue shrinkage at the repair site. The prosthesis may be configured to both limit tension at the anchoring locations and compensate for tissue shrinkage. The prosthesis may facilitate a reduction in postoperativ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com