Nasal airway management device
a management device and nasal passage technology, applied in the field of nasal passage management devices, can solve the problems of not maintaining an airway or adequately breathing, putting enormous pressure on ensuring timely, sedated patients, critically ill patients and coding patients,
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
[0026]Some embodiments of the invention are discussed in detail below. In describing embodiments, specific terminology is employed for the sake of clarity. However, the invention is not intended to be limited to the specific terminology so selected. A person skilled in the relevant art will recognize that other equivalent components can be employed and other methods developed without departing from the broad concepts of the invention. All references cited herein are incorporated by reference as if each had been individually incorporated.
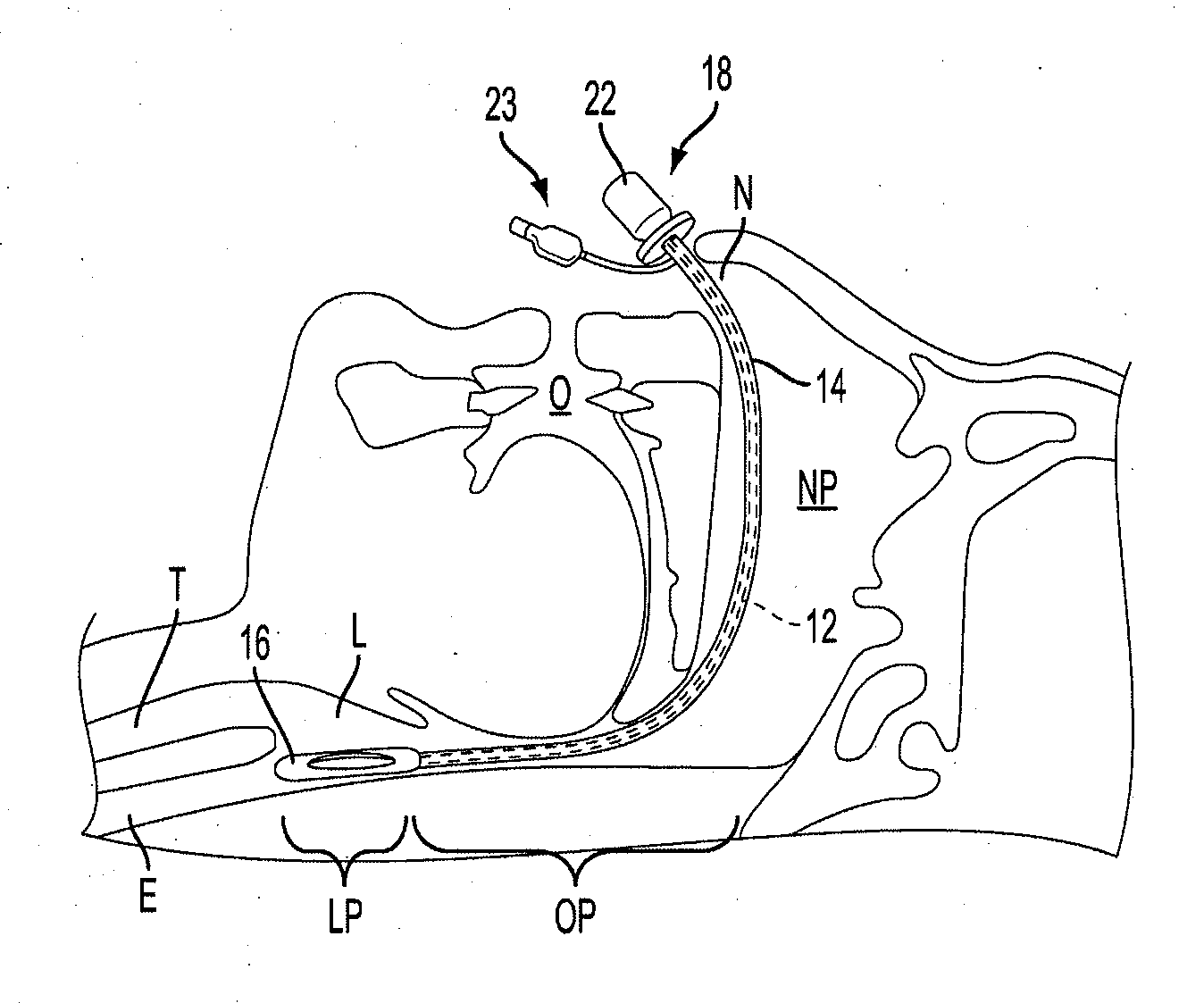
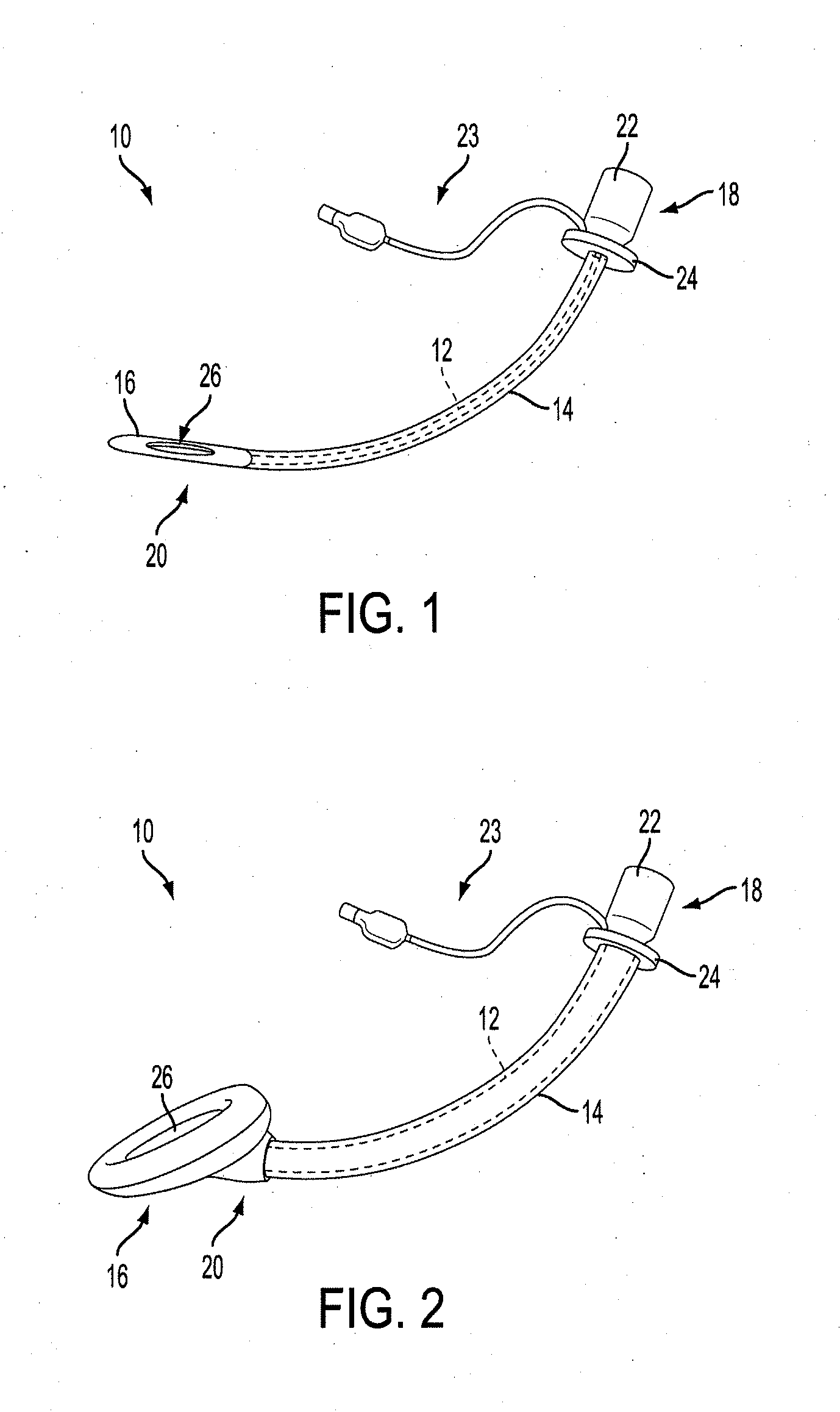
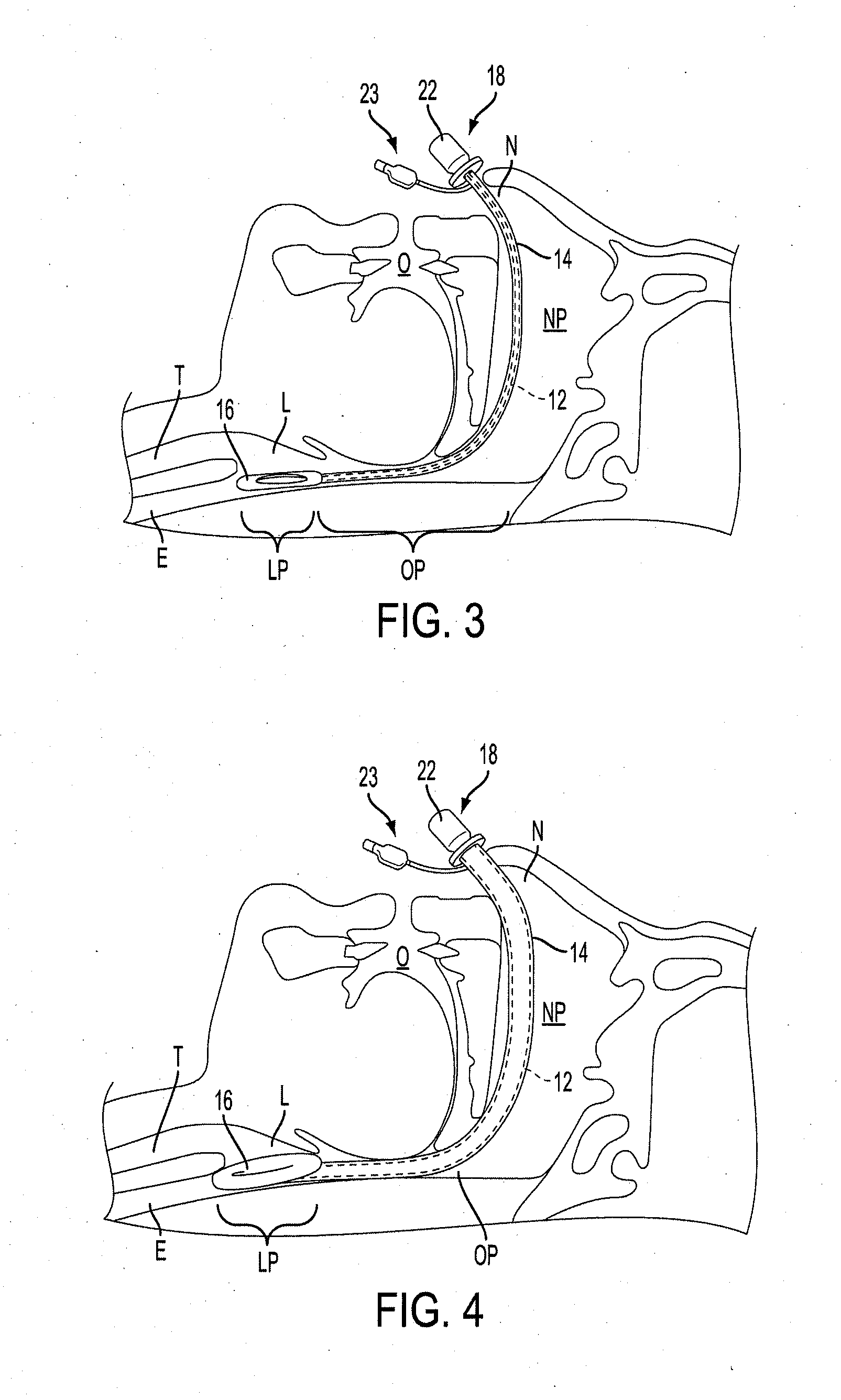
[0027]FIGS. 1 and 2 depict perspective views of a nasal airway management device 10 according to an embodiment of the invention. The device 10 includes a hollow flexible tube 12 defining a lumen extending between a proximal end 18 and a distal end 20. An inflatable outer sleeve 14 may surround and extend along the length of the tube 12. An inflatable supraglottic laryngeal cuff 16 may be attached at or near the distal end 20 of the tube 12. Both oute...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com