Three-dimensional medical implant for regeneration of soft tissue
a three-dimensional, medical implant technology, applied in the field of medical technology, can solve the problems of increasing the number of such devices in the market, difficulty in providing a scaffold that fits the surgeons' needs in terms of tissue regeneration, ease of use and problem-free healing, and difficulty in combining different scaffold characteristics or even different materials into one scaffold, etc., to achieve adequate pliability and mechanical rigidity, rapid tissue ingrowth, and the effect of good mechanical rigidity
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
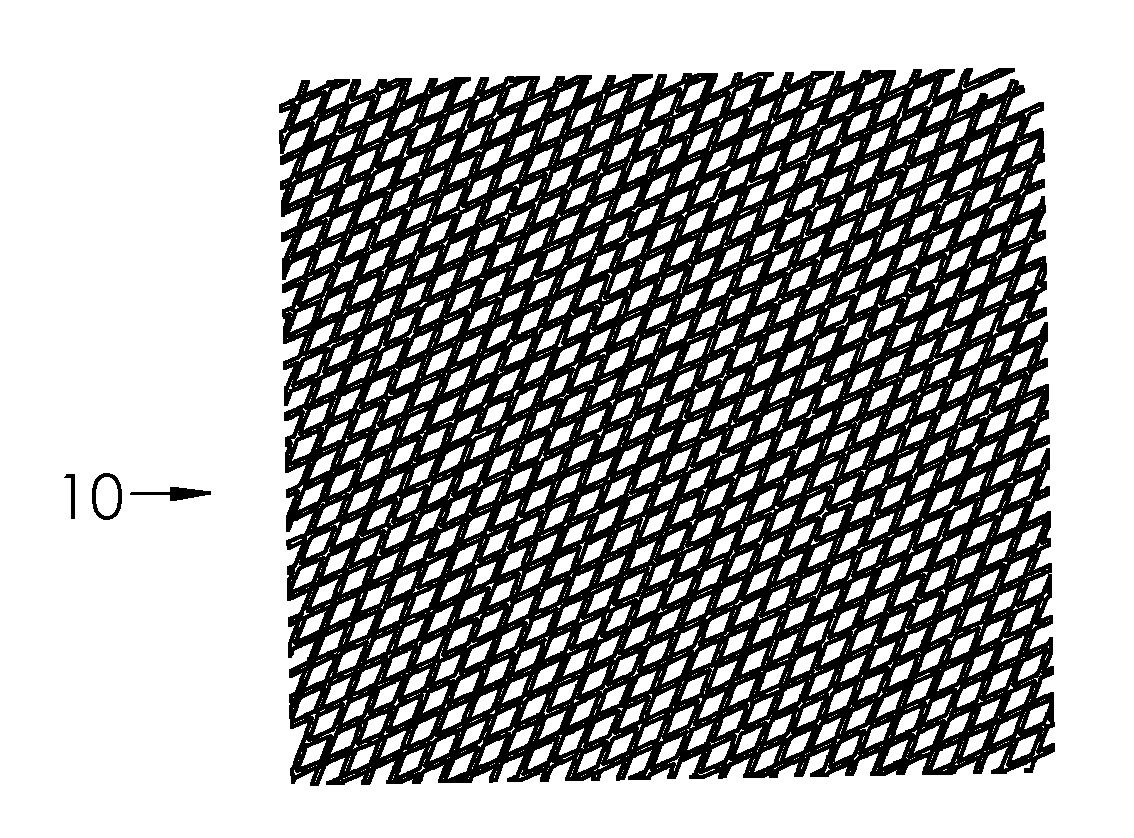
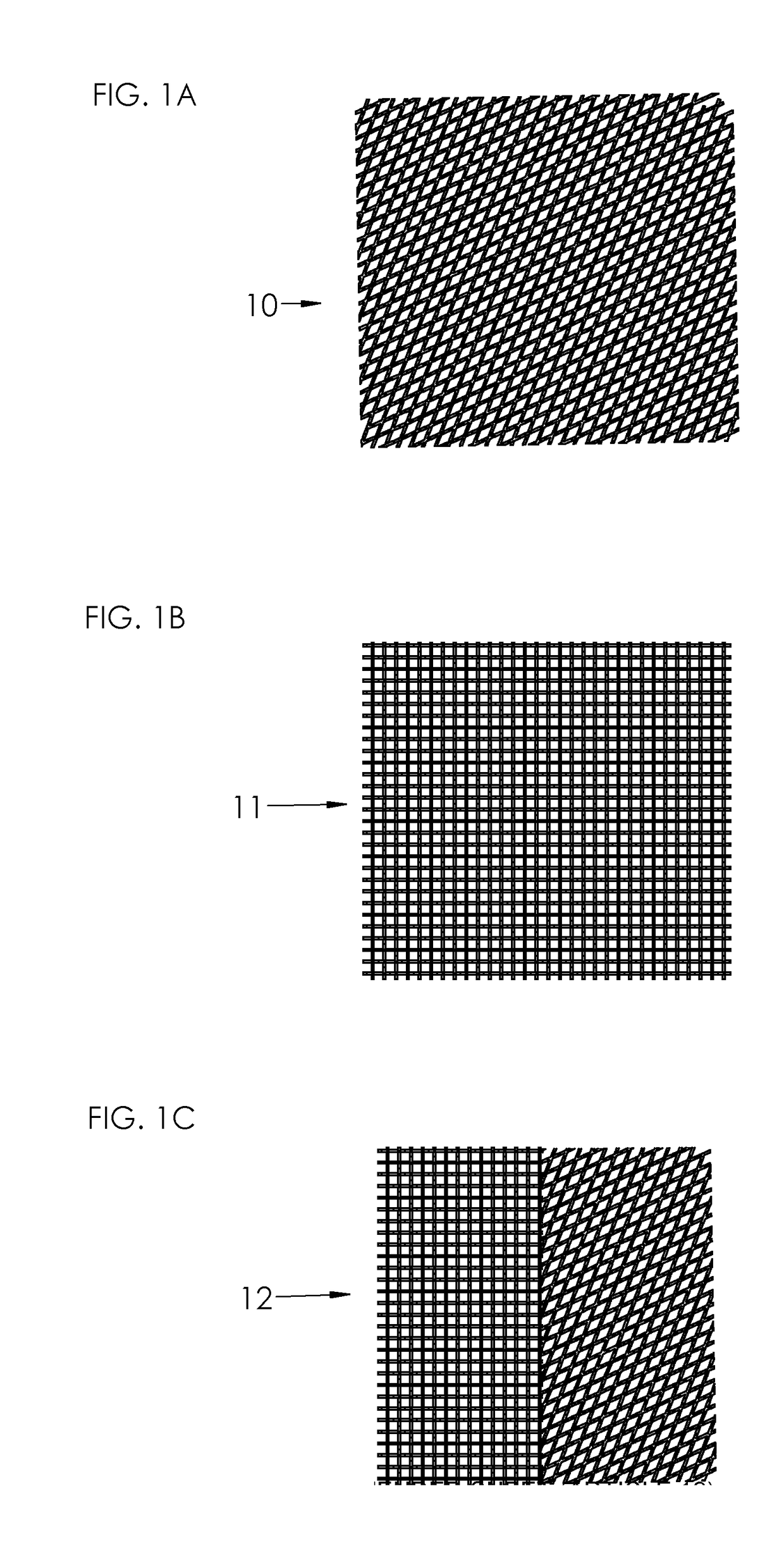
[0037]FIG. 1A illustrates schematically a mesh 10 which has rhombic or diamond-shaped openings, which may be obtained by warp knitting using atlas type pattern or interlaced pillar pattern. The mesh as such is previously known in the art.
[0038]FIG. 1B illustrates schematically a mesh 11 which has square-shaped openings, which may be obtained by open woven structure or warp knitting using double marquisette combined with pillar stitch. The mesh as such is previously known in the art.
[0039]FIG. 1C illustrates schematically a mesh 12 which is a combination of a mesh 10 and a mesh 11.
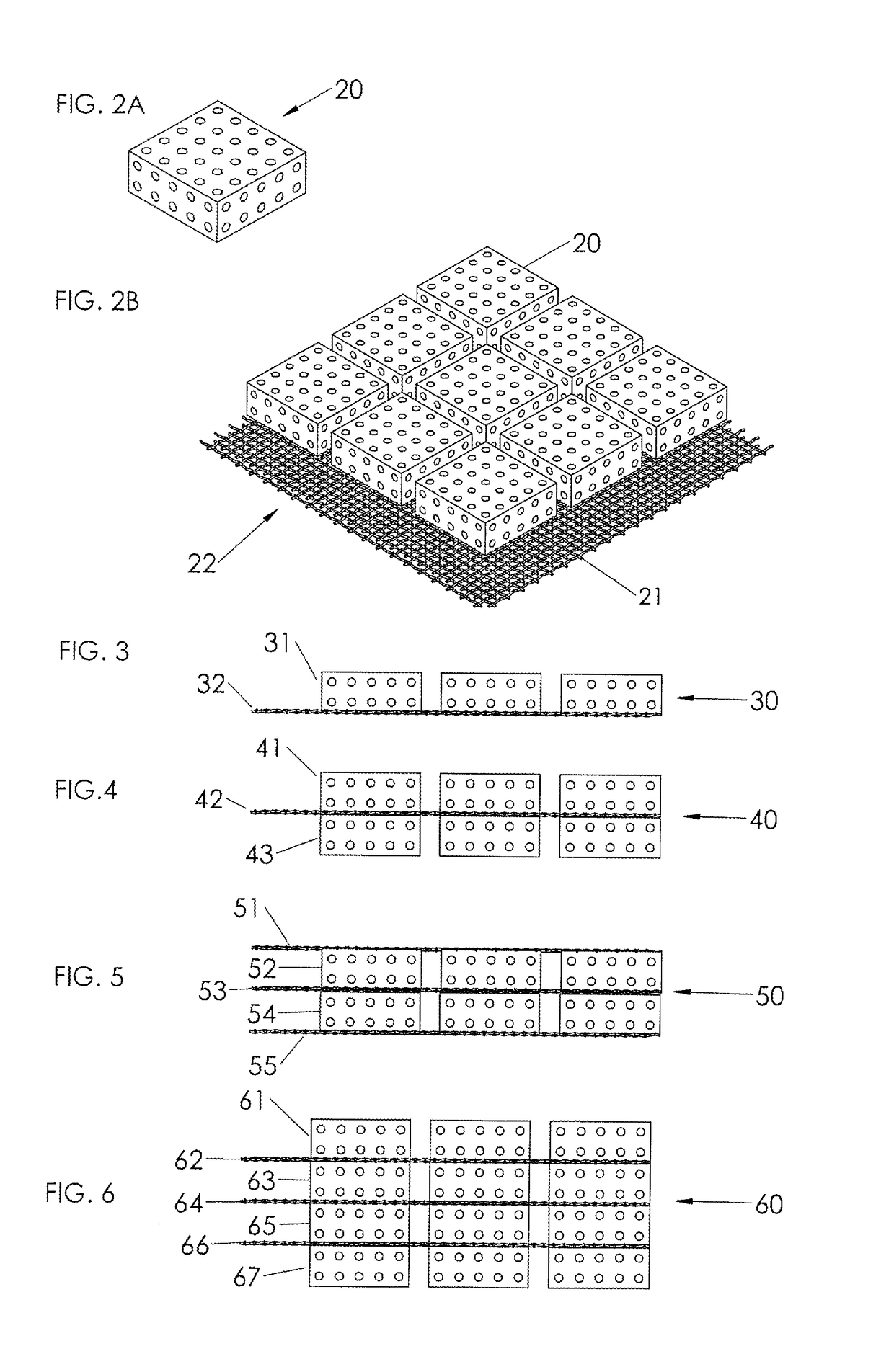
[0040]FIG. 2A illustrates schematically a perspective view of a volume-building component 20 according to the present disclosure consisting of a scaffold component. The dotted pattern of the volume-building component is not to be construed as illustrating holes or pores in the material, but is solely meant to illustrate any type of volume-building component, irrespective of the structure or composition of t...
PUM
| Property | Measurement | Unit |
|---|---|---|
| distance | aaaaa | aaaaa |
| distance | aaaaa | aaaaa |
| melting point | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com