Method and apparatus for non-invasive monitoring of respiratory parameters in sleep disordered breathing
A non-invasive, breathing effort technology that can be used in respirator, app, drug devices, etc., to solve problems such as differences in obstructive sleep apnea, limiting average mask pressure, etc.
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
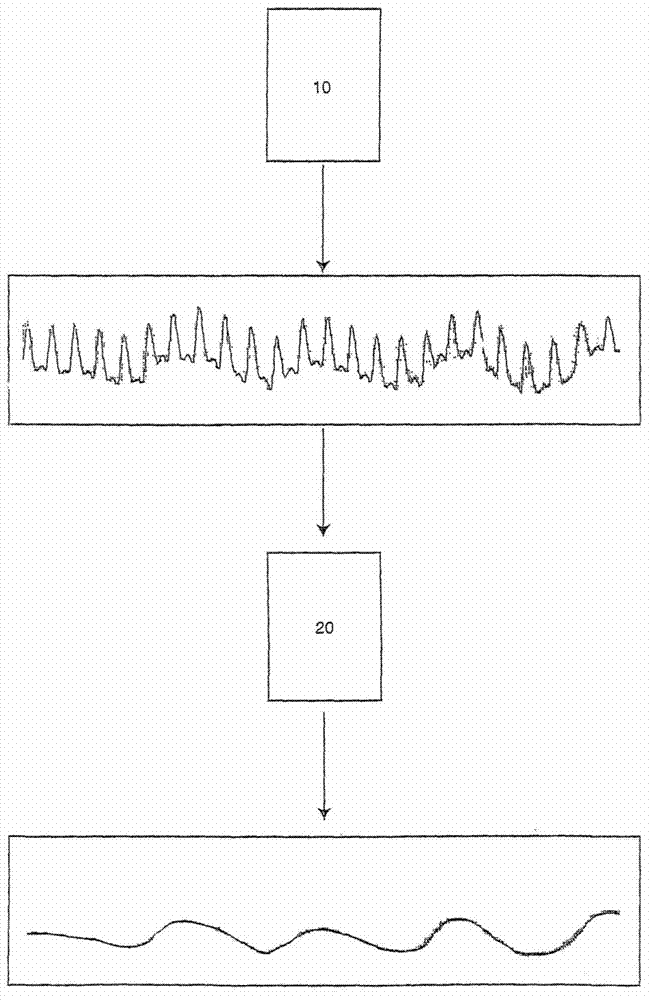
[0039] Pulse oximetry plethysmography (sometimes called "pulse oximetry" or "photoplethysmography") is the standard method for obtaining blood oxygenation data in a non-invasive and continuous manner. Oximeters use two wavelengths of light to determine hemoglobin saturation. Absorption by the pulsatile arterial blood volume produces a waveform that represents an alternating current (AC) signal. Absorption by non-pulsatile blood, venous and capillary blood, and tissue absorption is represented by a direct current (DC) signal. See "Use of Pulse Oximetry to Recognize Severity of Airflow Obstruction in Obstructive Airway Disease, Correlation with Pulsus Paradoxus" by Hartert et al., Chest 1999:115:475-481. The pulse oximeter signal obtained by Harter et al. figure 1 shown in .
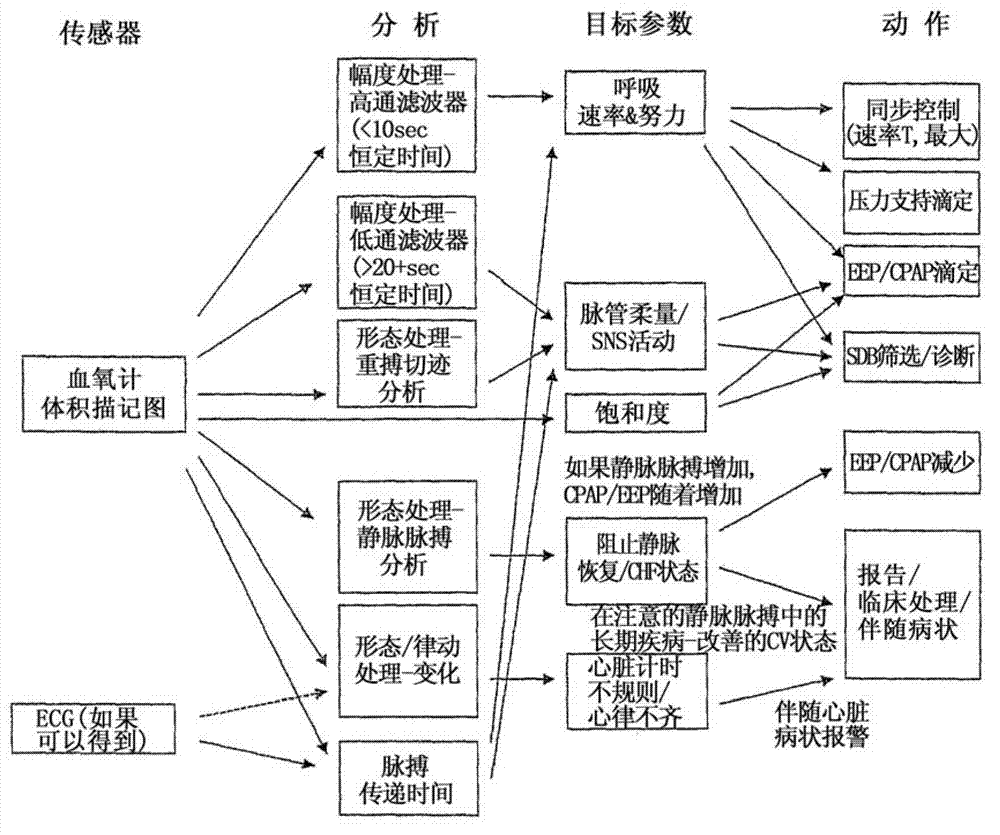
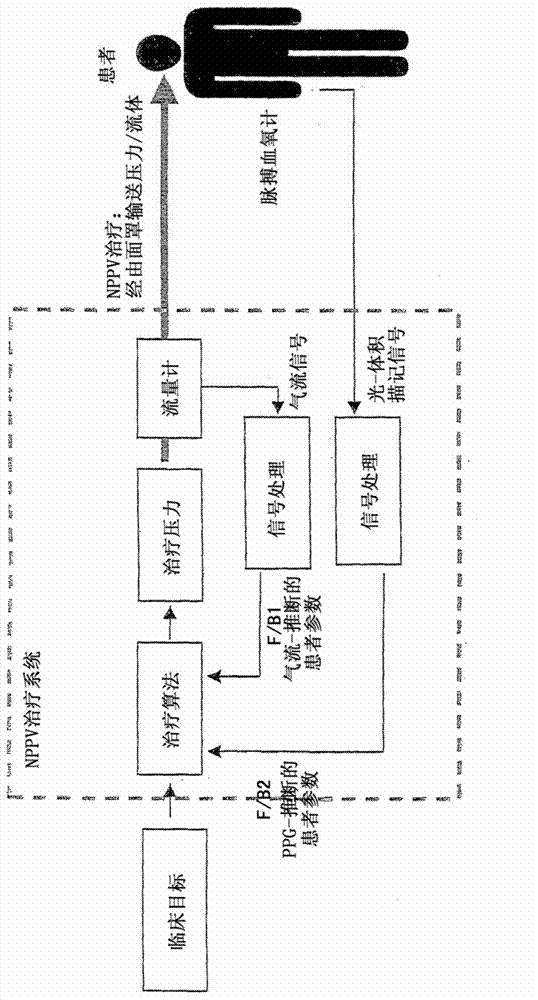
[0040] Current pulse oximeters are primarily used to monitor SpO2 and heart rate, but according to an embodiment of the present invention, pulse oximeters are used in respiratory therapy devices as indi...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com