Method and apparatus for performing catheter-based annuloplasty using local plications
a technology of annuloplasty and local plication, which is applied in the field of mitral valve insufficiencies treatment techniques, can solve the problems of many types of ailments, high cost of ventricular assist devices, and incongestive heart failure, so as to avoid complicated surgical procedures and improve the quality of life
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
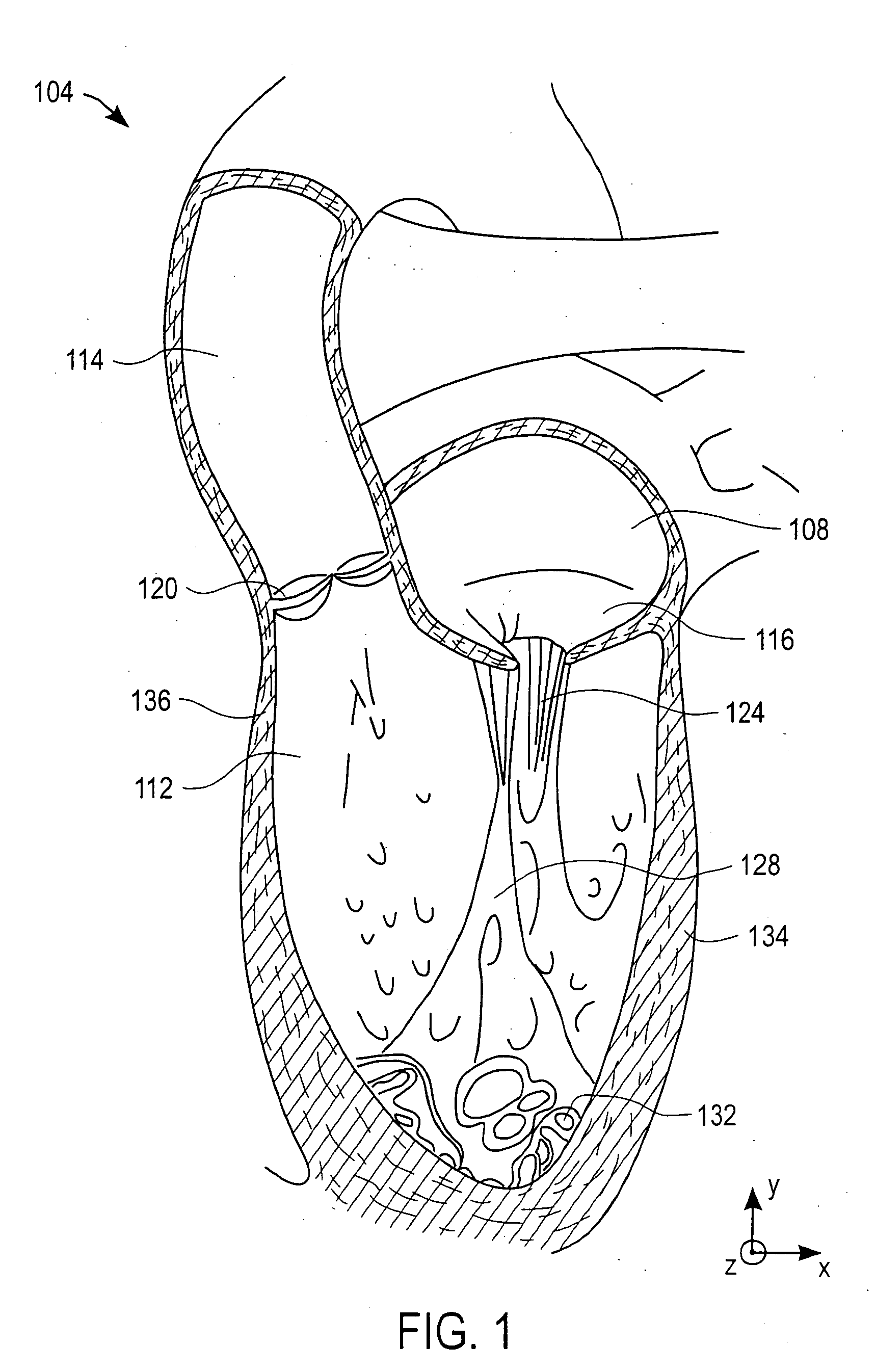
[0094] Invasive, open-heart surgical procedures are generally effective in the treatment of mitral valve leakage. However, open-heart surgical procedures may be particularly hazardous to some patients, e.g., frail patients or patients who are considered as being very ill, and undesirable to other patients, e.g., patients who are asymptomatic and do not wish to undergo a surgical procedure. As such, open-heart surgical procedures to correct mitral valve leakage or, more generally, mitral valve insufficiency, are not suitable for many patients who would likely benefit from reducing or eliminating the mitral valve leakage.
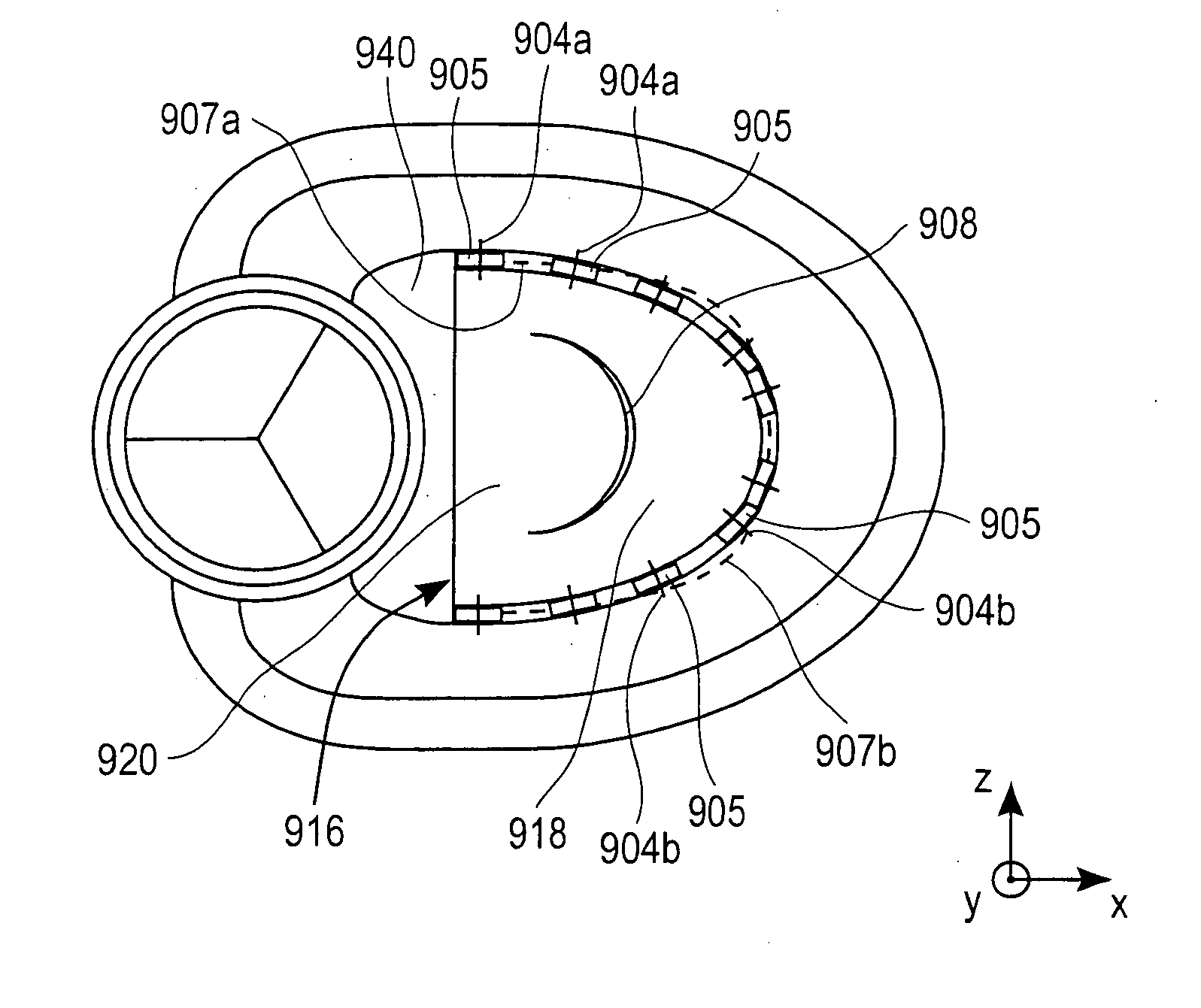
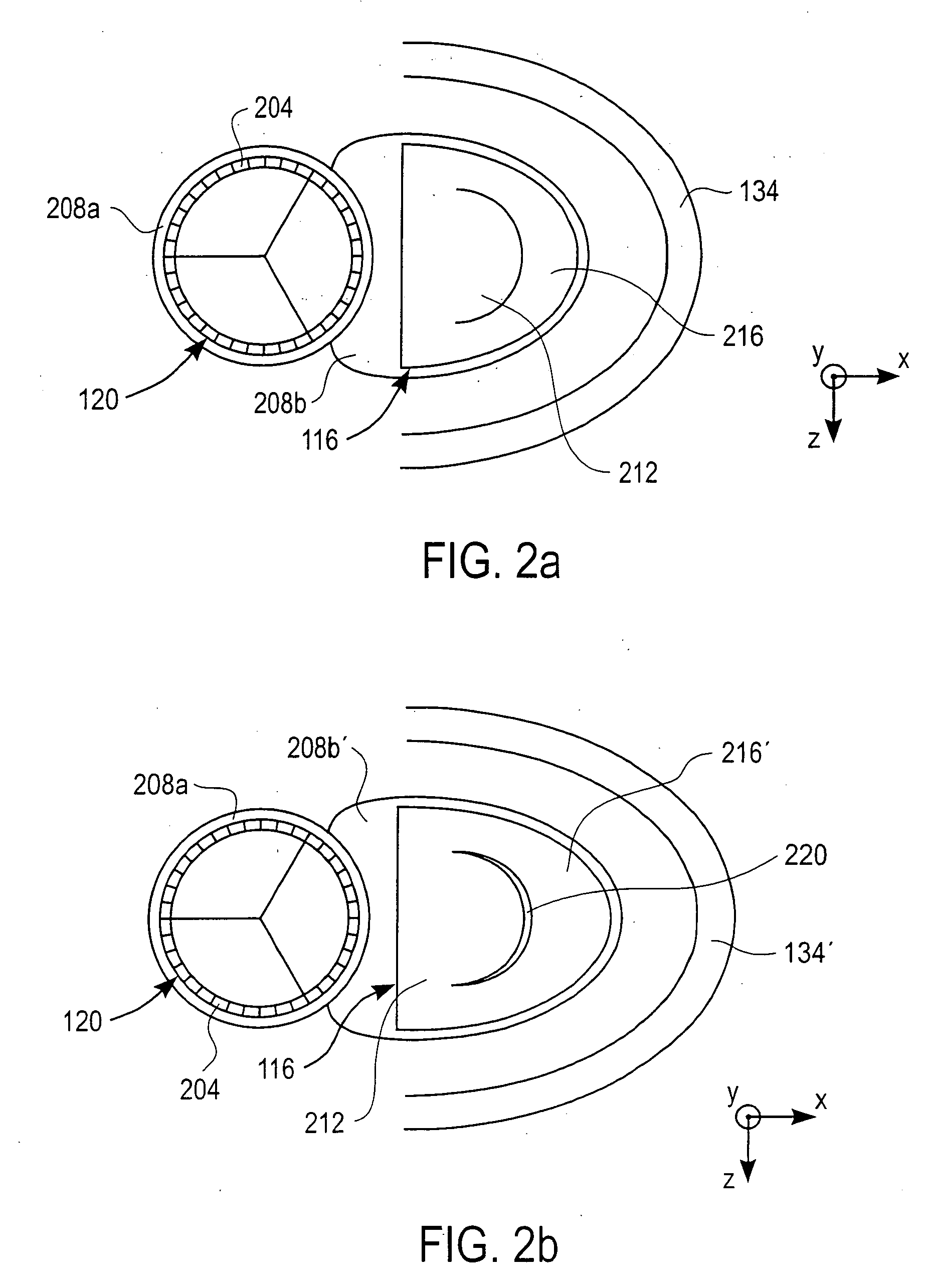
[0095] A catheter-based annuloplasty procedure enables annuloplasty to be performed on a patient without requiring that the patient undergo open-heart surgery, or be placed on cardiopulmonary bypass. Catheters may be introduced into the left ventricle of a heart through the aorta to position a guide wire and plication implants on the ventricular side of a mitral valv...
PUM
| Property | Measurement | Unit |
|---|---|---|
| distance | aaaaa | aaaaa |
| distance distance | aaaaa | aaaaa |
| tension | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com