Minimally-invasive devices and methods for treatment of congestive heart failure
a congestive heart failure, minimally invasive technology, applied in the direction of surgical forceps, catheters, applications, etc., can solve the problems of inability to pump at a sufficient rate to maintain adequate blood circulation throughout the body, inability to perform highly invasive and traumatic procedures, and shortening of breath, so as to facilitate the reduction of left ventricular volume, reduce pain and trauma to the patient, and reduce the risk of infection and neurological events.
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
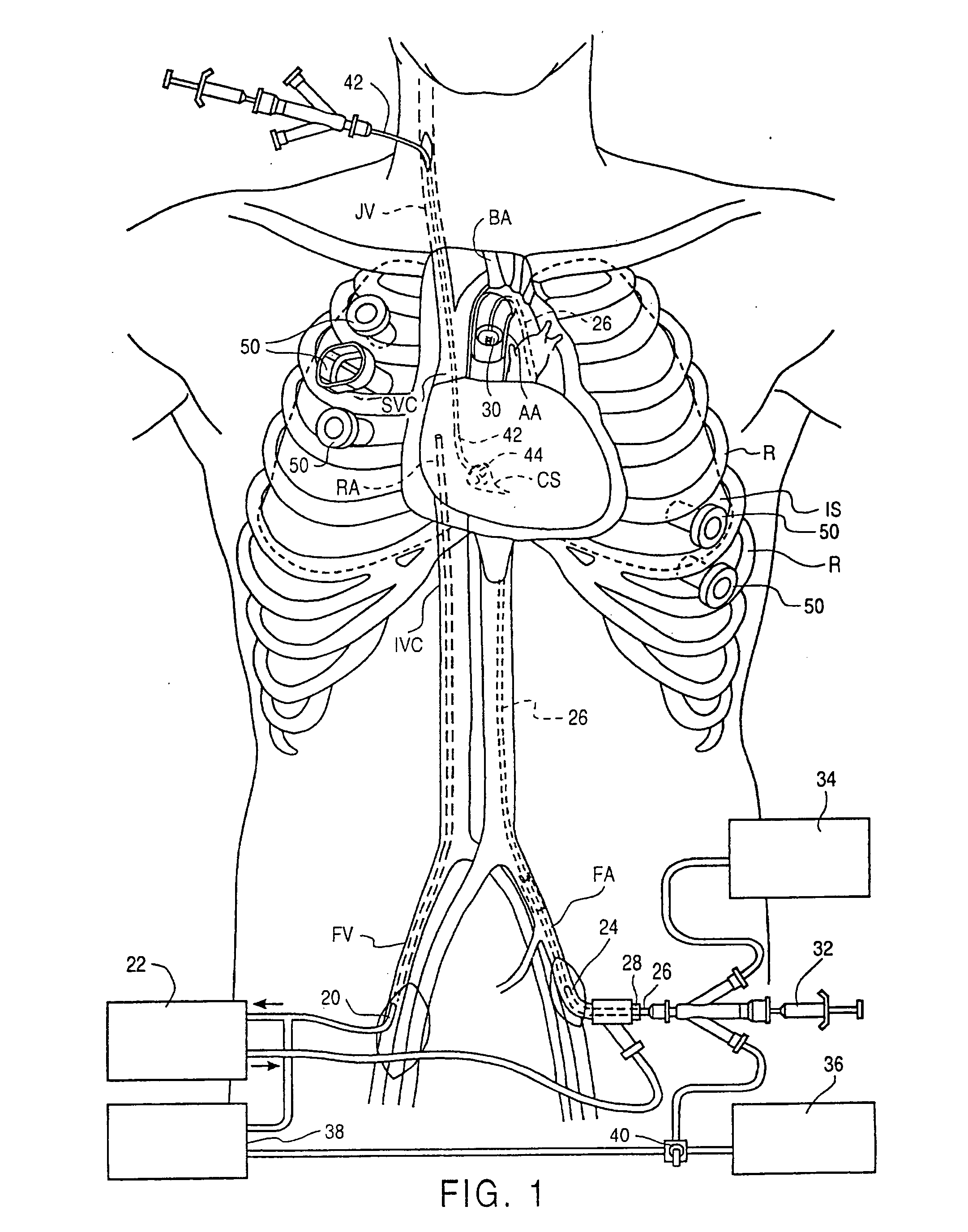
[0042] Referring to FIG. 1, an endovascular cardiopulmonary bypass (CPB) system useful in the method of the invention is illustrated as it is used in a patient. Additional aspects of such endovascular CPB systems suitable for use in the methods of the invention are described in the following patent applications, which are incorporated herein by reference: Ser. No. 08 / 282,192, filed Jul. 28, 1994, now U.S. Pat. No. 5,584,803, Ser. No. 08 / 612,341, filed Mar. 7, 1996, and Ser. No. 08 / 486,216, filed Jun. 7, 1995, now U.S. Pat. No. 5,766,151. The system includes a venous drainage cannula 20 placed into a femoral vein FV (or other suitable peripheral vein) and preferably having sufficient length to extend into the inferior vena cava IVC, the right atrium RA or the superior vena cava SVC. Venous drainage cannula 20 is connected to an extracorporeal CPB system 22, which filters and oxygenates the blood withdrawn from the patient. The system further includes an arterial return cannula 24 pla...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com