Femoral and humeral stem geometry and implantation method for orthopedic joint reconstruction
a stem and humeral technology, applied in the field of orthopaedic implants, can solve the problems of instability of the shoulder joint, disruption of the soft tissue, and difficulty in so as to facilitate the insertion of the proximal body portion, facilitate the reaming of bone, and improve the conformance and fixation of the stem implan
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
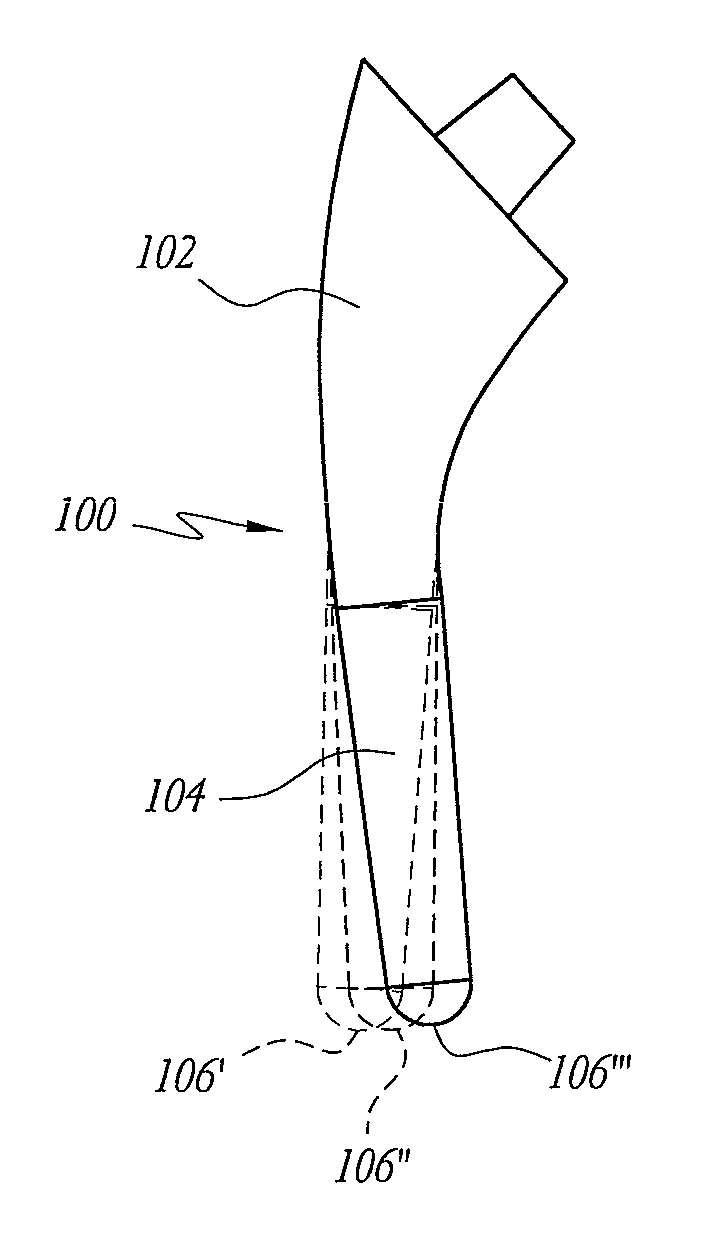
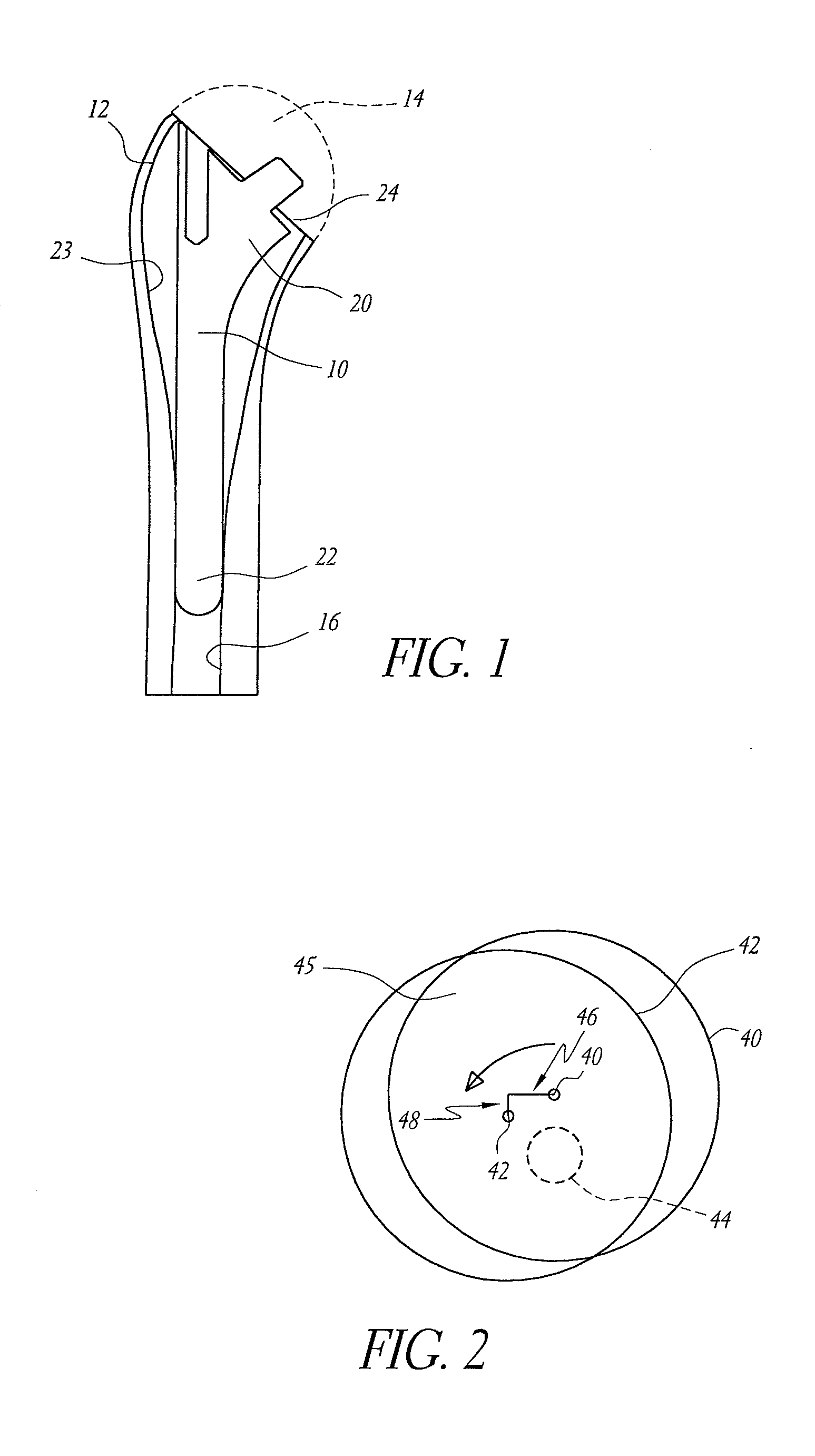
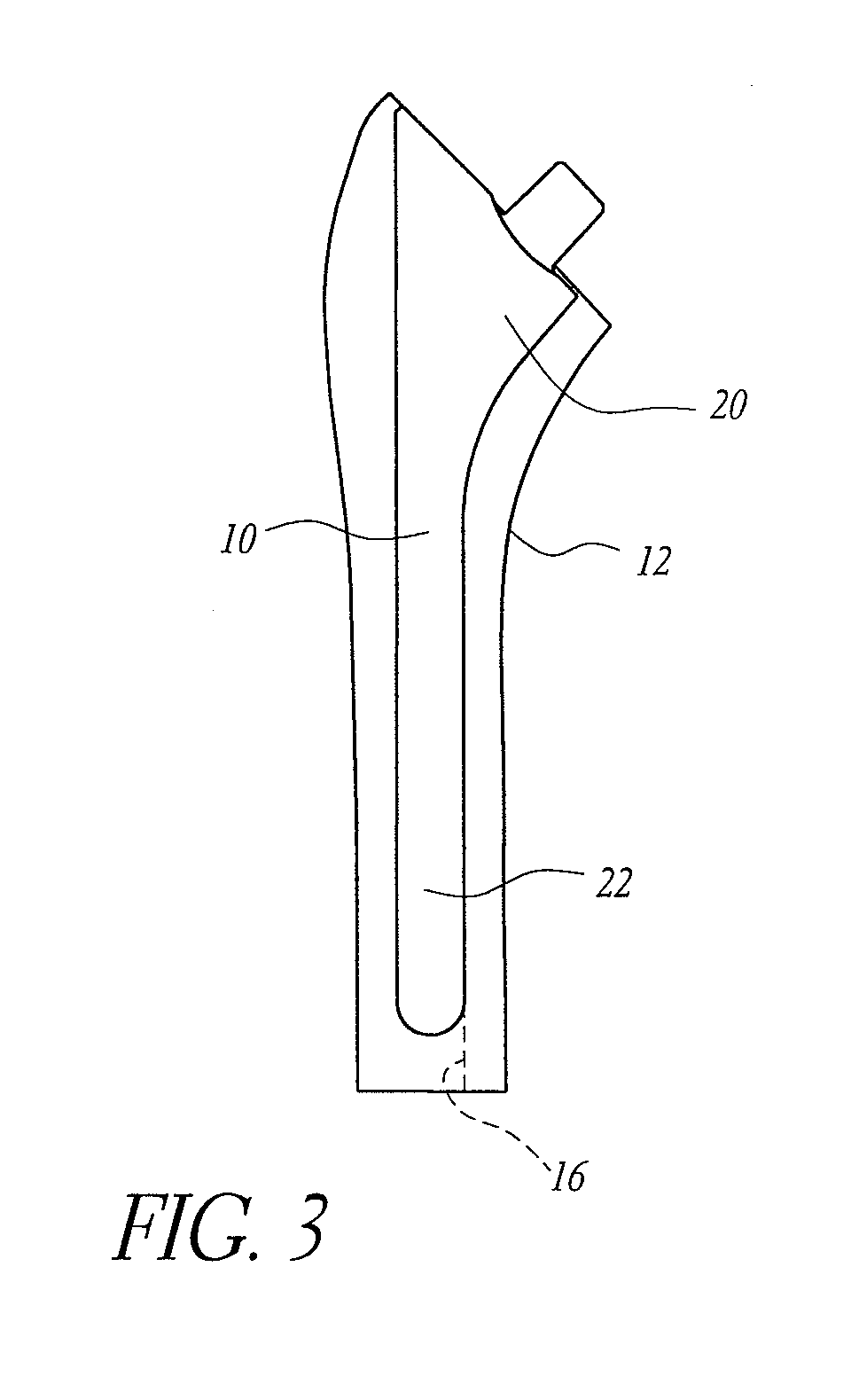
[0050] As used herein, the term “stem” is a broad term that is used to designate a device that is implanted into the bone for the purpose of supporting a functional component of a joint replacement and resisting the loads applied to the functional component. For example, a stem can be a device implanted into a humerus or femur to support a modular prosthetic humeral or femoral head (i.e. the supported structure). In other embodiments, the supported structure can be an integral part of the stem, as with a monolithic stem and head. Femoral and humeral stems typically include distal and proximal sections as well as a taper or other coupling device to which the functional component is attached. Additionally, femoral stems typically include a neck section that extends the distance between the proximal section and the head. The neck is not embedded in the bone, but sits proud. As used herein, the term “neck” can refer to the portion of a femoral stem that does not reside within the femur ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com