Absorbable anchor for hernia mesh fixation
a technology of anchors and hernia meshes, applied in the field of surgical fasteners, can solve the problems of reducing lifting ability, bowel impaction, and failure to teach how to generate enough spring action from the device to overcome the high radial force generated by tissue, and achieves reasonable “kill” times, reduce lifting ability, and weaken mechanical properties
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
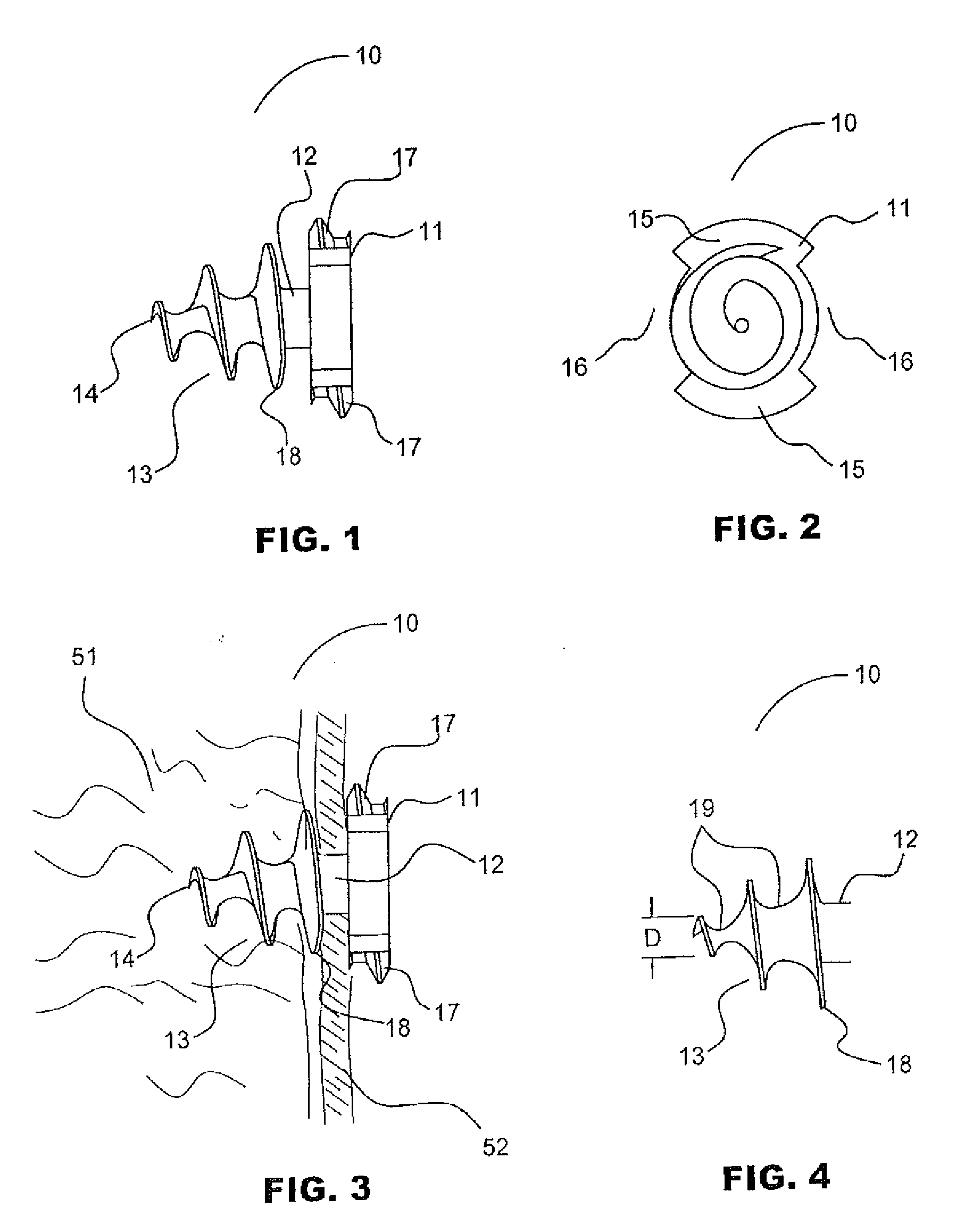
[0070]Turning now to FIGS. 1, 2 and 3, depictions of the anchor of the current invention, generally designated as 10. Anchor 10 comprises three sections, head section 11, mesh retention section 12, and threaded tissue-snaring section 13. Head section 11 comprises two opposing threaded sections 15 with head threads 17 and two opposing open or slotted sections 16. The distal surface of head section 11 is formed onto the proximal end of mesh retention section 12.
[0071]Mesh retention section 12 may, alternately, be tapered or right-cylinder shaped or may be omitted, which would allow the proximal end of threaded tissue-snaring section 13 to abut the distal end of head section 11. Unlike the embodiment of anchor 10 with no mesh retention section 12, either the conical or cylindrical configuration mesh retention section 12 locks mesh 52 on to anchor 10 when mesh 52 is screwed past the proximal-most tissue-snaring thread 18 since there is no thread located in mesh retention section 12 that...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com