Replacement mitral valve with annular flap
a technology of annular flap and mitral valve, which is applied in the field of prosthesis, annuloplasty rings, and replacement mitral valves, can solve the problems of reducing the efficiency of heart blood pumping, debilitating and life-threatening conditions, and inhibiting the valves' ability to control blood flow, etc., and achieves the effect of increasing the surface area of the prosthesis
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
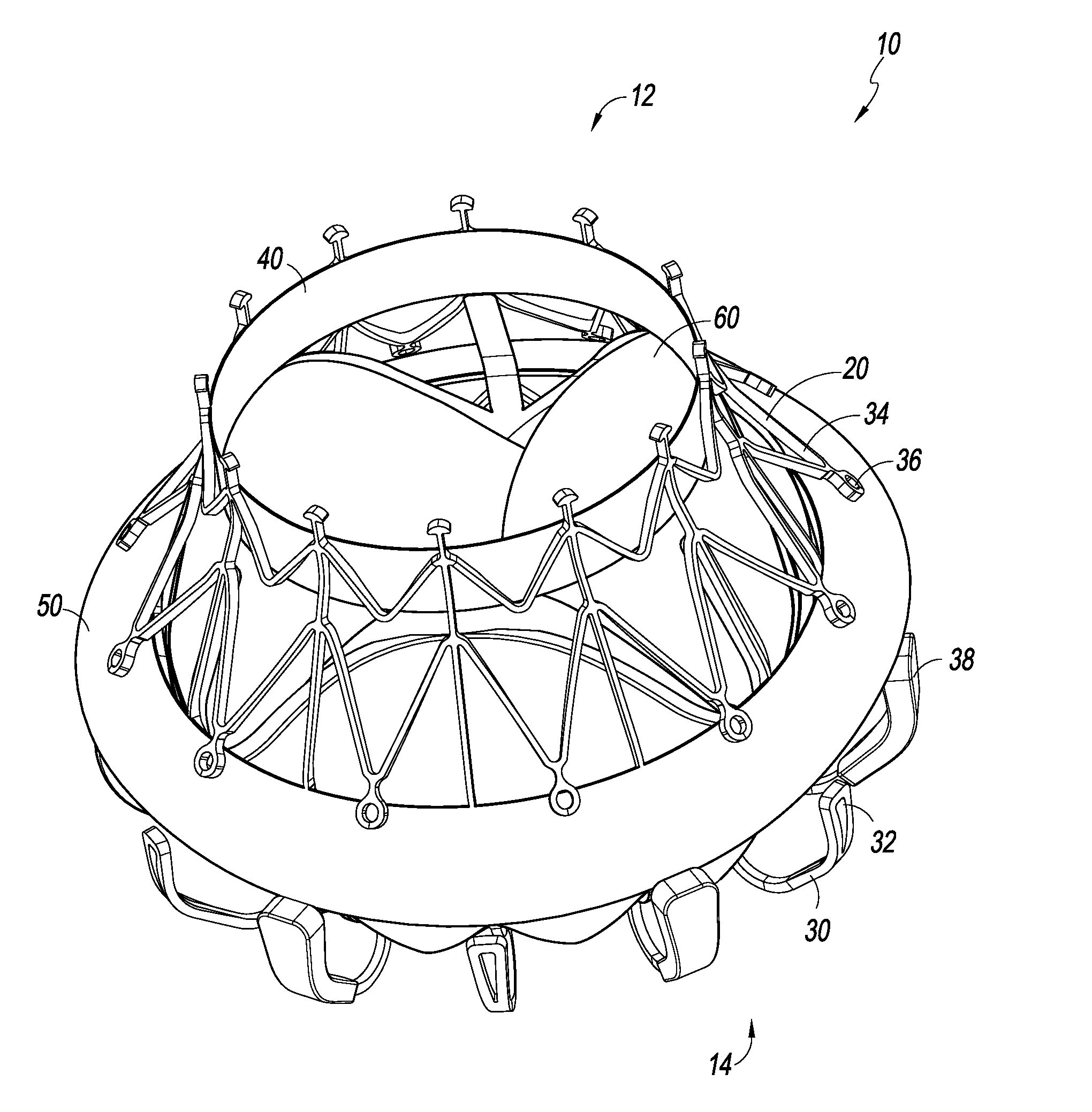
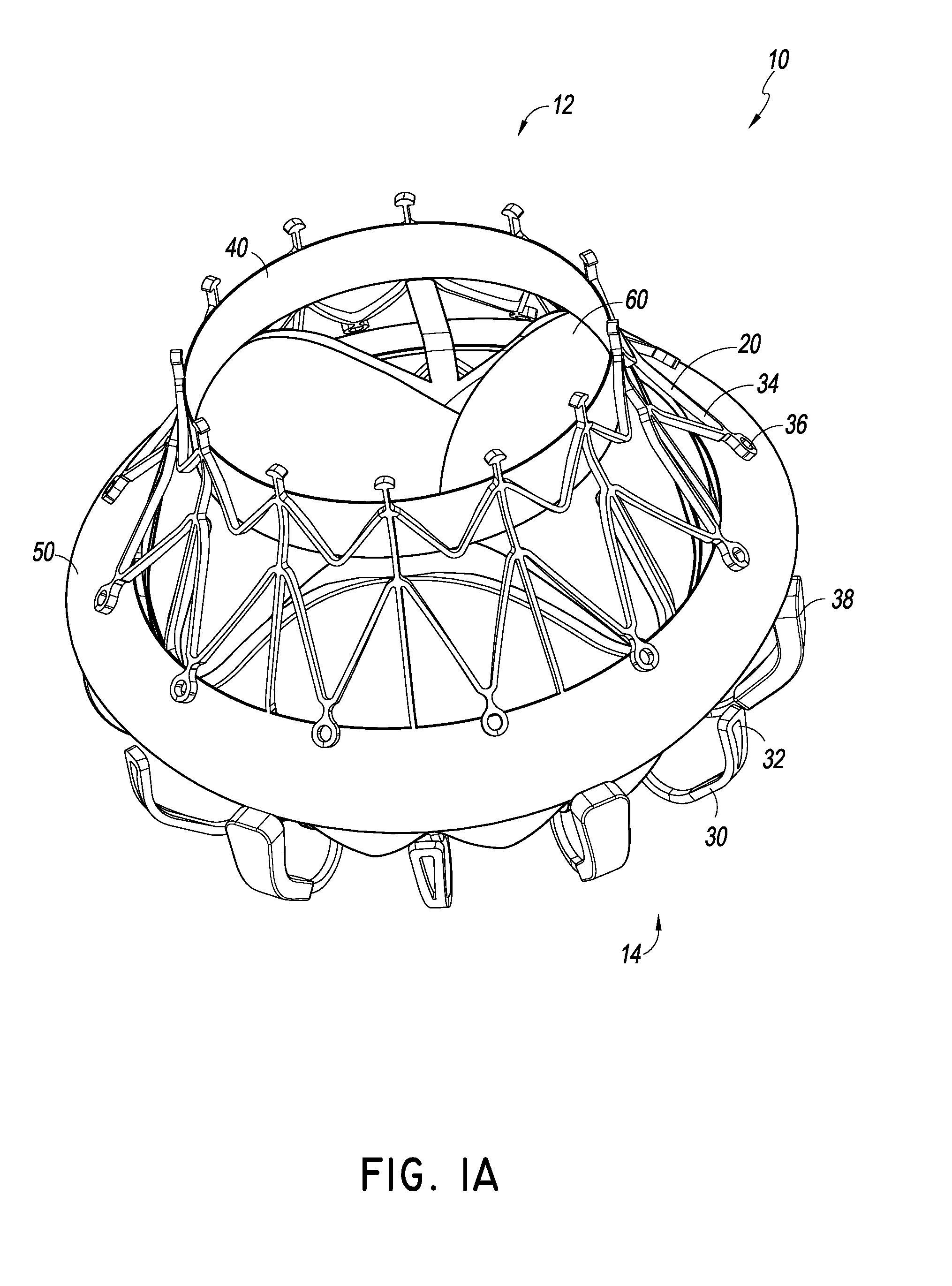
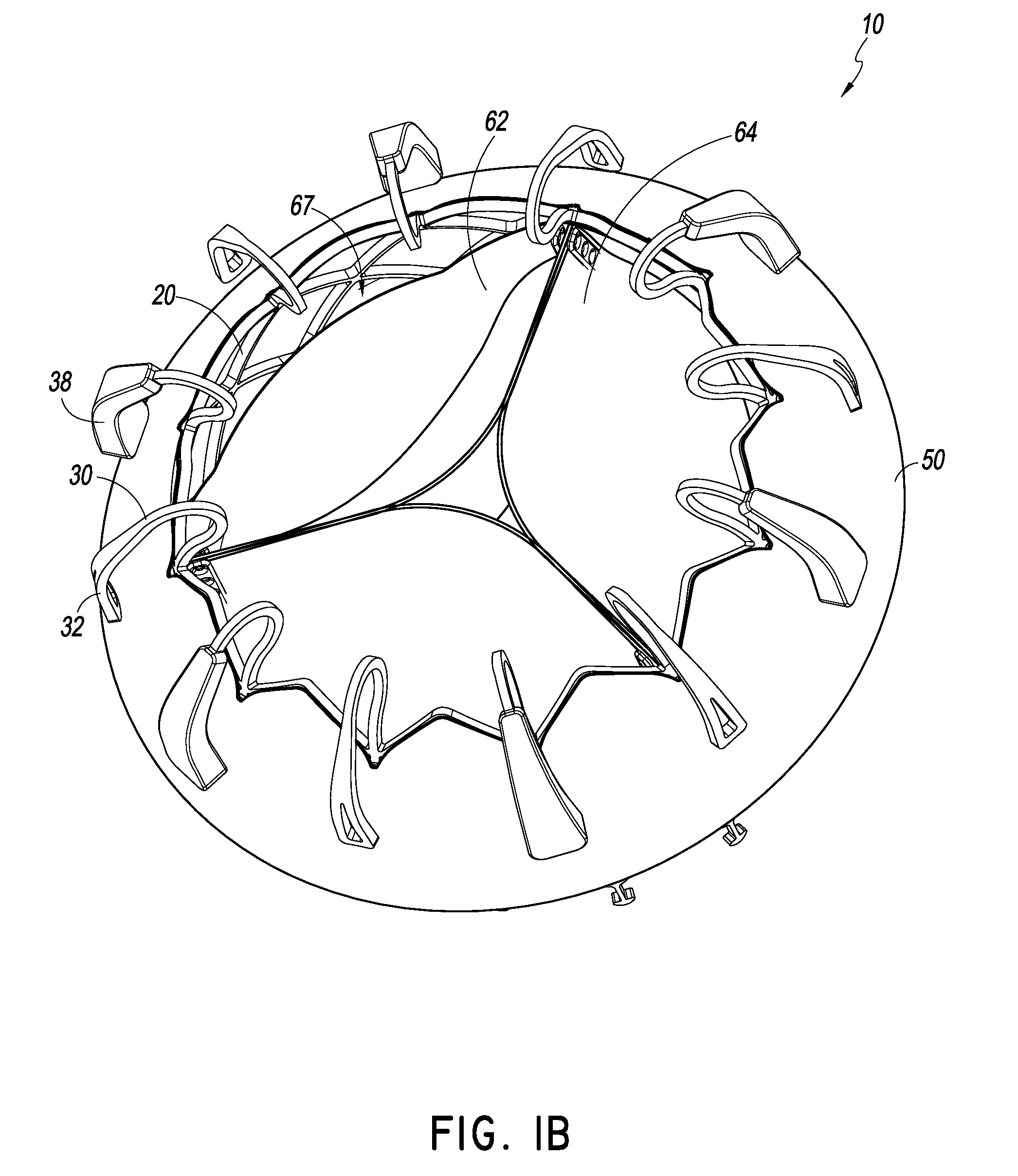
[0026]The embodiment of FIGS. 1A-4 illustrates a prosthesis 10. The prosthesis 10 can have components, features, and / or functionality similar to those described in any of U.S. Publication Nos. 2014 / 0277390, 2014 / 0277422, and 2014 / 0277427, the entire contents of all which are incorporated by reference herein. With reference first to the embodiments of FIGS. 1A-4, the prosthesis 10 can include a frame 20, anchors 30, 34, a band 40, an annular flap or sail 50 and a valve body 60. The prosthesis 10 can include a proximal end 12 and a distal end 14 with openings defined at both ends 12, 14 such that fluid can flow therethrough. In some embodiments, the proximal end 12 can be placed in the left atrium while the distal end 14 can be placed in the left ventricle such that prosthesis 10 can function as a replacement for a mitral valve. As will be discussed in greater detail below and as discussed in U.S. Publication Nos. 2014 / 0277390, 2014 / 0277422, and 2014 / 0277427, the prosthesis 10 can all...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com