Determining the size of the air fistula in the thoracic drainage therapy
a technology for determining the size of the air fistula which is applied in the direction of suction devices, intravenous devices, other medical devices, etc., can solve the problems of air accumulation in the pleural space, and no standard treatment recommendations concerning the regulation of the vacuum in the thoracic drainage system, and achieve the effect of optimal treatmen
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example 1
Closing Fistula
[0091]In a patient 1 with an air fistula, the thoracic drainage system Thopaz™ was used. A vacuum of 10 mbar was initially set. This resulted in a volumetric flow of 100 ml / min. From this, a fistula size F=2.15 was calculated using the above equation (see step 33). The vacuum was then increased by 5 mbar to 15 mbar. After one hour, the volumetric flow was measured again. This was now 120 ml / min. From this, a fistula size F=2.13 was calculated. The fistula had therefore functionally decreased in size. The vacuum of 15 mbar was therefore maintained for a further 3 hours.
example 2
Opening Fistula
[0092]In a patient 2, an initial vacuum of 10 mbar was likewise set. In this patient also, this resulted in a volumetric flow of 100 ml / min, from which a fistula size F=2.15 was calculated. The vacuum was again increased by 5 mbar to 15 mbar, and the volumetric flow was measured after one hour. This was now 240 ml / min, corresponding to a fistula size F=2.56. The vacuum was therefore lowered by 10 mbar to just 5 mbar, and this value was maintained for a further 3 hours.
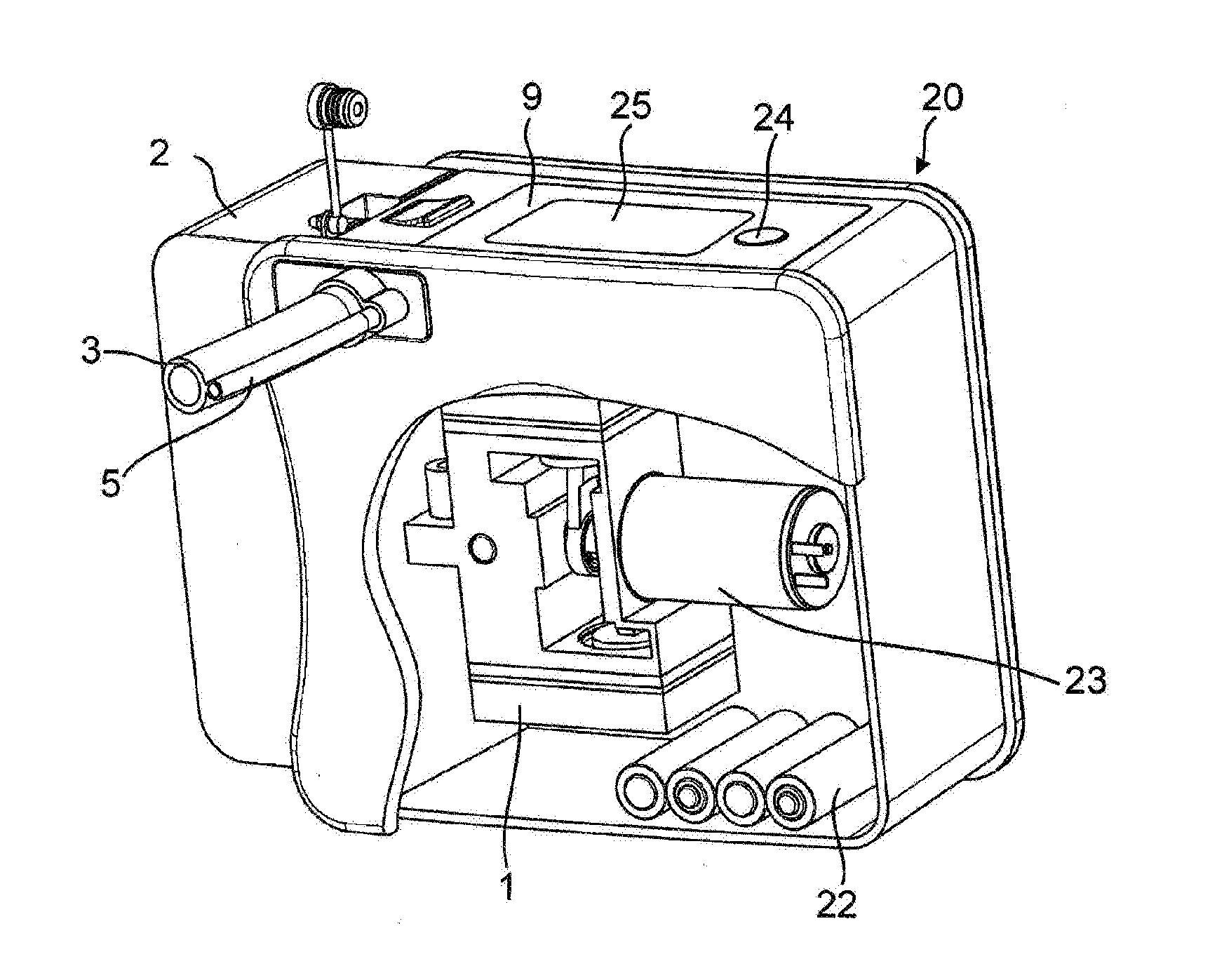
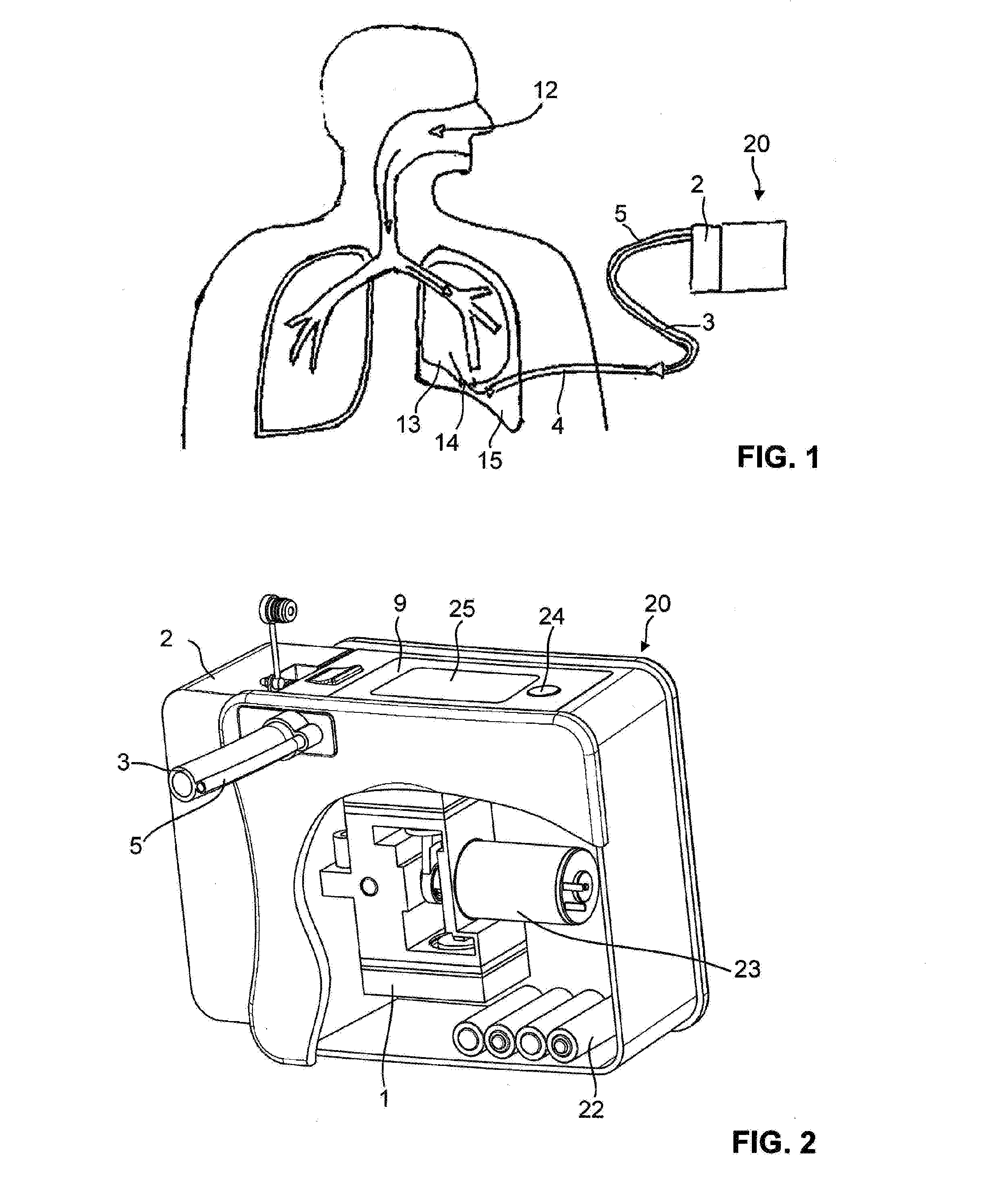
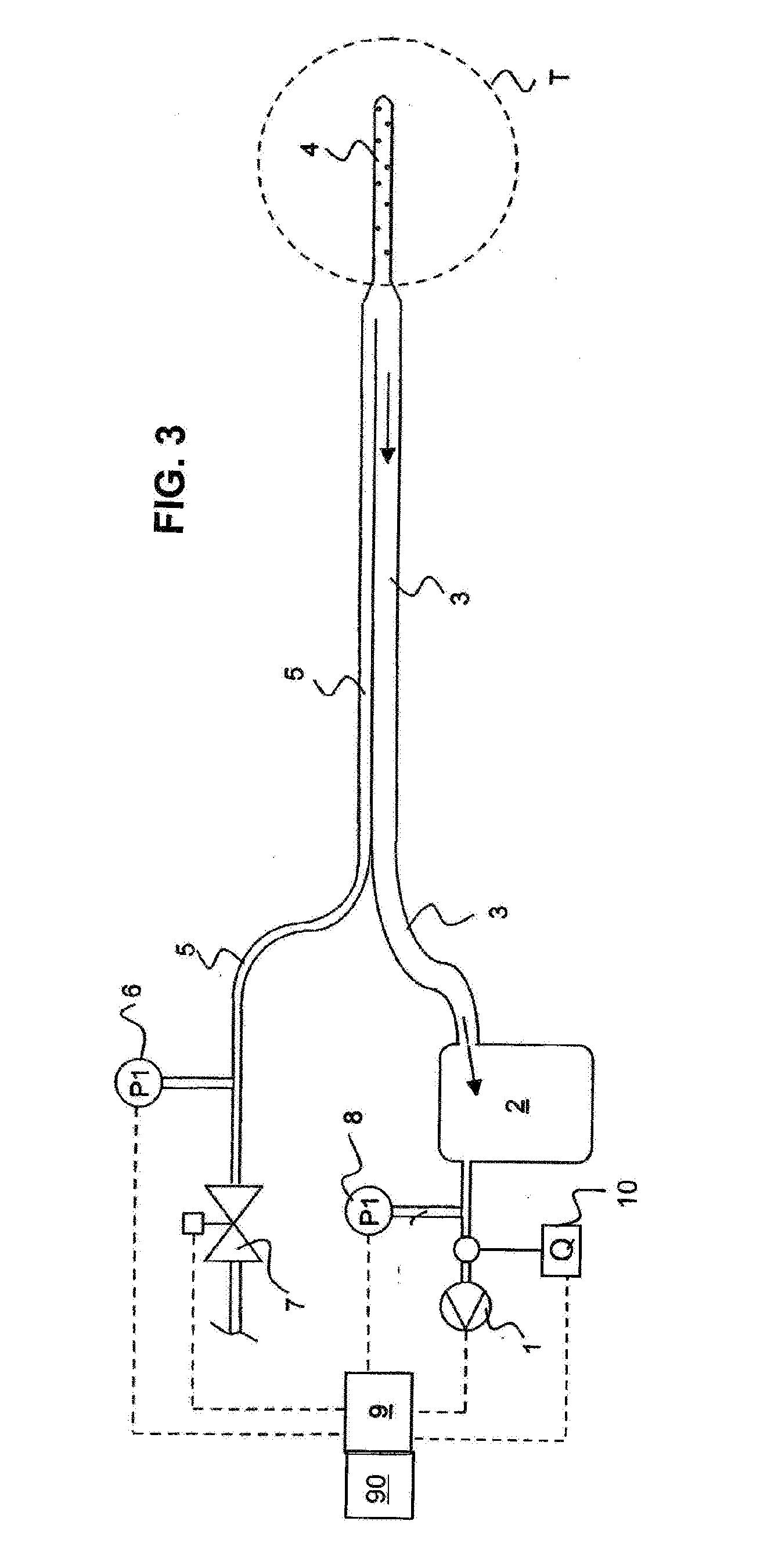
[0093]It is clear that many modifications can be made to the appliances and methods that have been described above by way of example. Thus, the suction device can be any other kind of suction device than the electrical suction pump in FIG. 2, e.g. an attachment for a central hospital vacuum system, as long as the vacuum level can be adjusted by a suitable pressure control. Accordingly, the thoracic drainage system can also be of a completely different construction than that shown in FIGS. 2 and 3. A grea...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com