Endovascular stapler
a technology of endovascular and stapler, which is applied in the direction of surgical staples, surgical forceps, blood vessels, etc., can solve the problems of type 1 endoleak with aneurysm sac reperfusion, enlargement and rupture, and insufficient coverage of renal artery orifices,
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
second embodiment
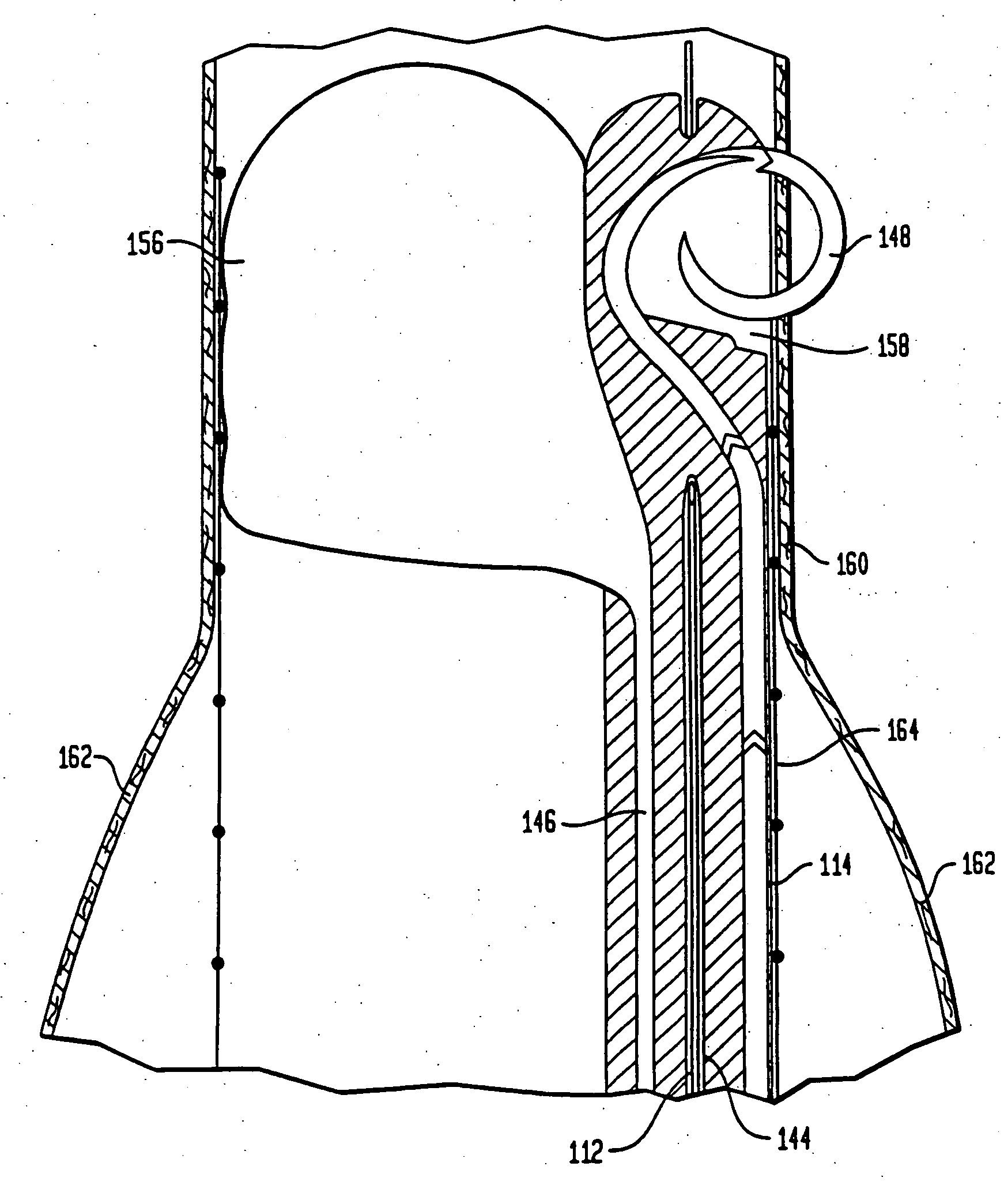
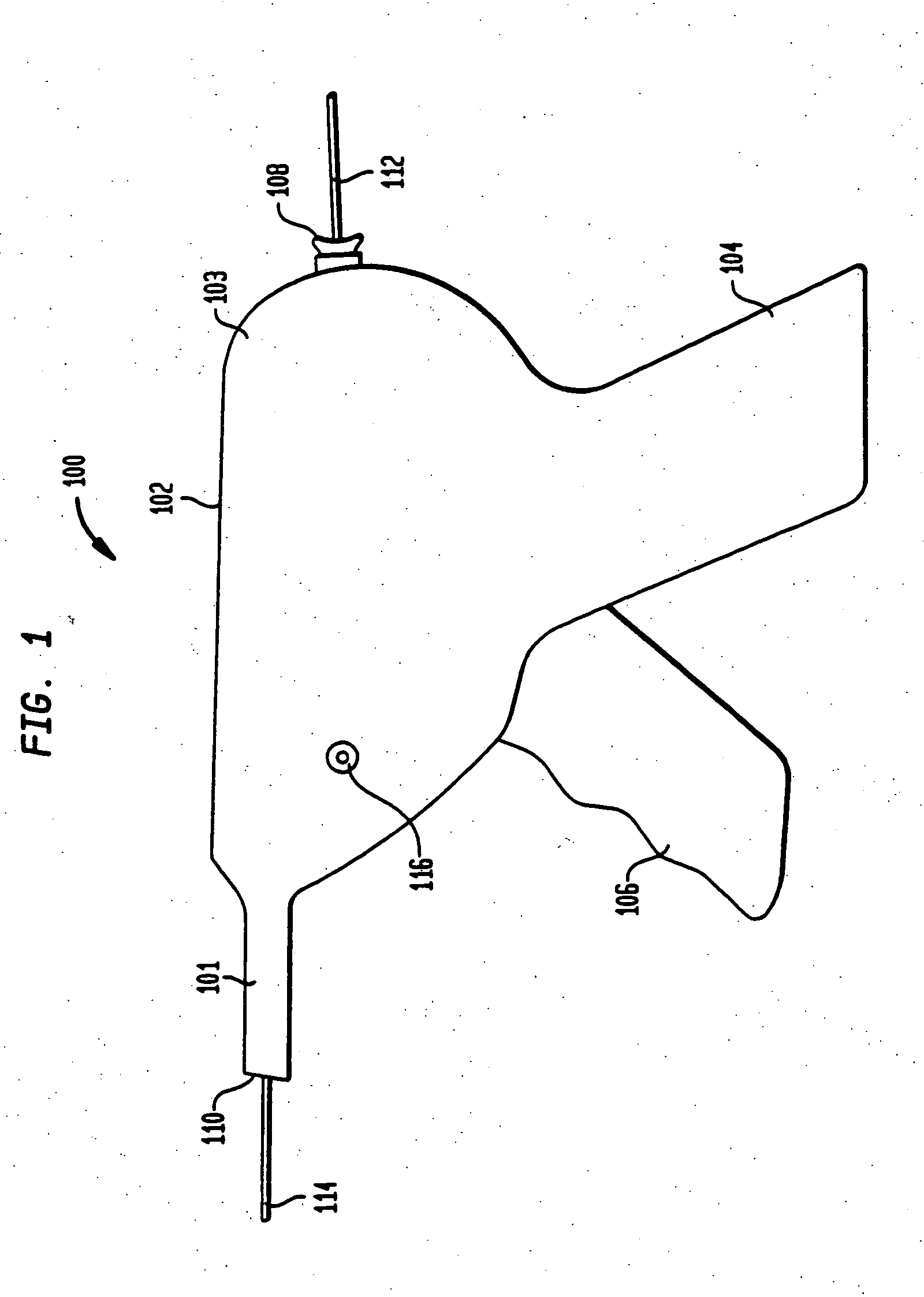
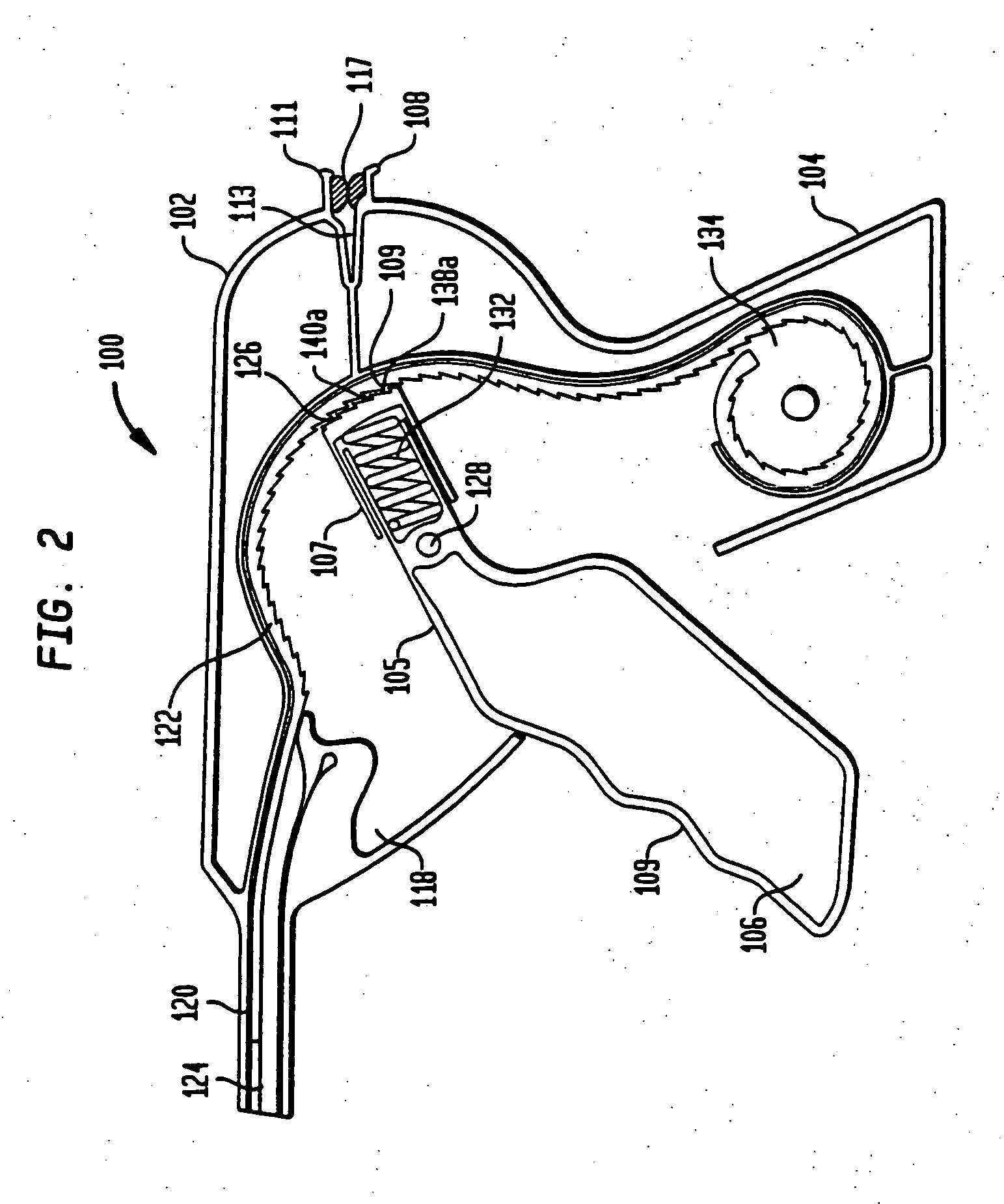
[0197]FIG. 14 depicts a cross-sectional view of a portion of the staple housing 214 of an endovascular stapler (not shown) in accordance with the present invention. In this embodiment, a single staple 248, formed in the shape of an elongated W may be applied to secure a graft 264 against a vessel, shown in FIG. 14 as an aortic wall 260. Typically, the chief function of a stapler in accordance with this embodiment is for use to arrest device migration of a previously placed endograft. Other embodiments employing multiple elongated W-shaped staples may also be used to arrest device migration of a previously implanted endograft or to affix a new endograft. Still further embodiments permit the withdrawal of portions of the stapler which may then be replaced with other portions pre-loaded with a staple for a subsequent firing.
[0198]FIG. 13 depicts a partially cut-away perspective view of a stapler housing 214 and a noncompliant balloon 256 inserted within an aortic wall 260 in preparatio...
first embodiment
[0202] As with the first embodiment, a guide wire channel 244 is also located within the staple housing 214. The guide wire channel 244 permits the use of a guide wire 212 in an “over the wire” system, to properly place the staple exit area 258.
[0203]FIG. 14 also depicts a portion of a noncompliant balloon 256. The noncompliant balloon 256 of the second embodiment may be completely exterior of the staple housing 214. The noncompliant balloon 256 is intended to be inflated such that the staple housing 214 will be pushed against the stent graft 264 such that the stent graft may be firmly apposed against the aortic wall 260.
[0204] Also included within the staple housing 214 is an elongated W-shaped staple 248. As shown in FIG. 15, the staple 248 includes two U-shaped sections 316 connected by a bridge 318. Each of the U-shaped sections 316 of the staple 248 sits against the front surface 320 of the actuator 306. At the extreme ends of the staple 248, the front surface 320 extends out ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com