Skin Marking Tool for Radiological Imaging Material
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
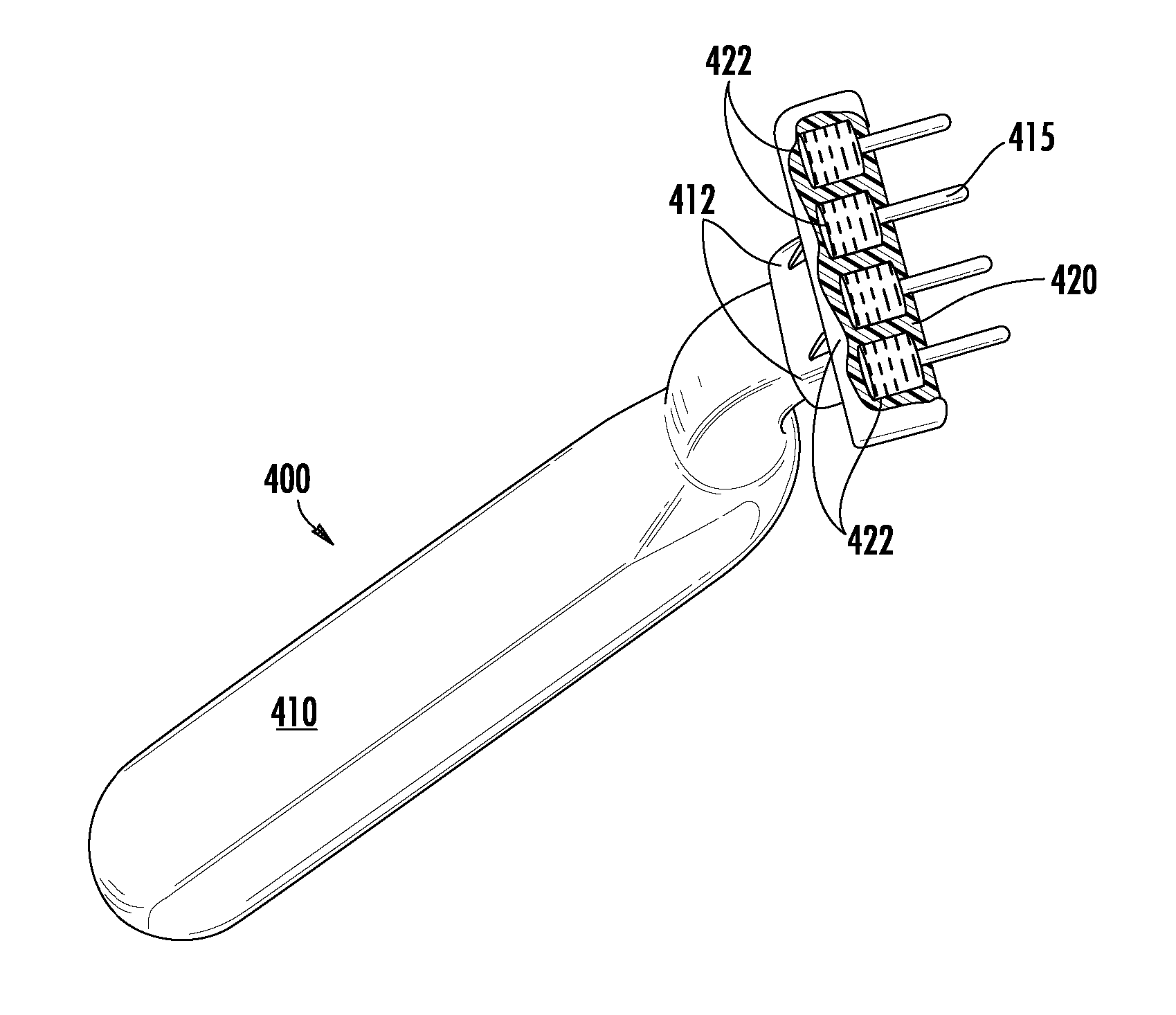
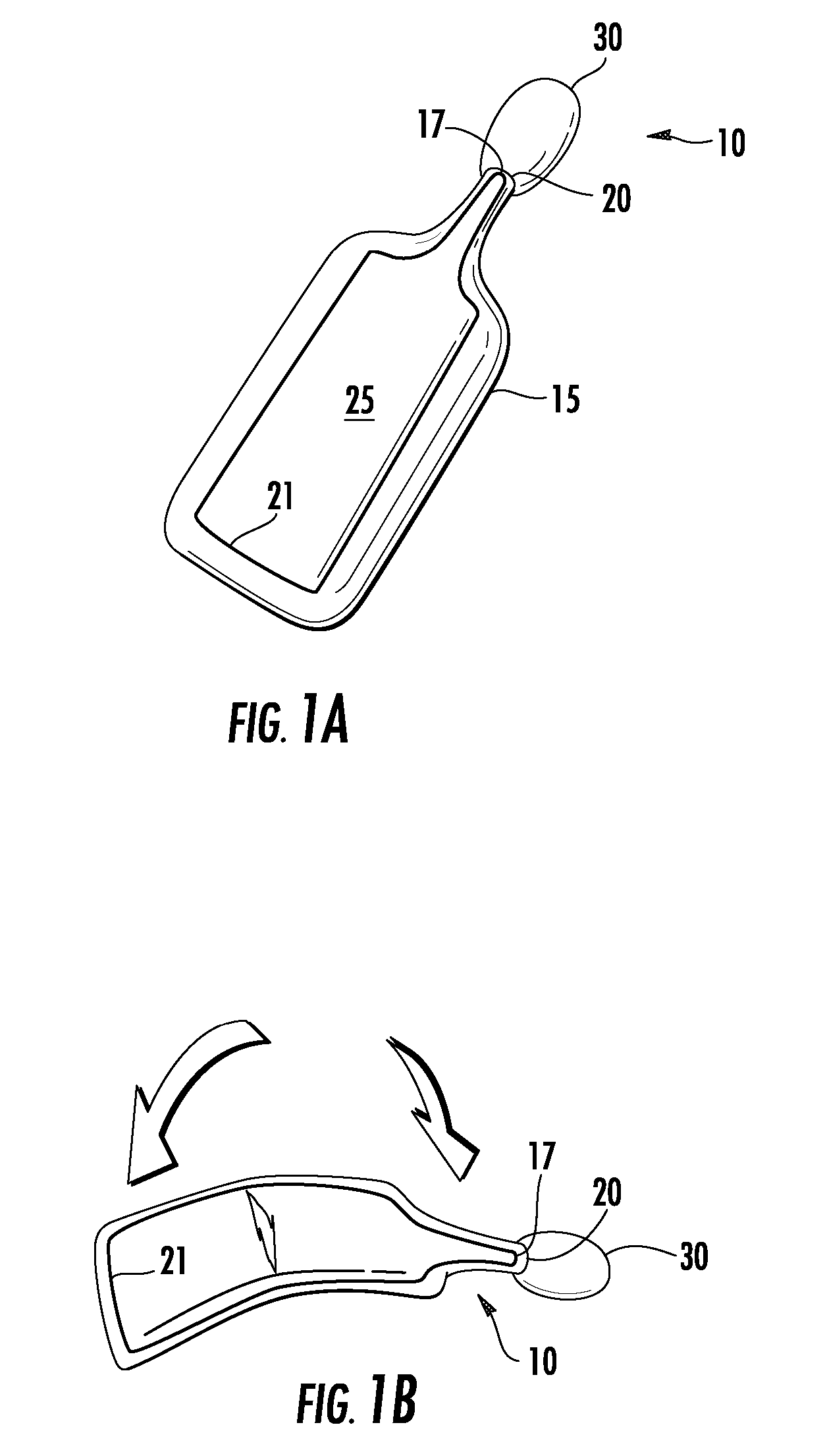
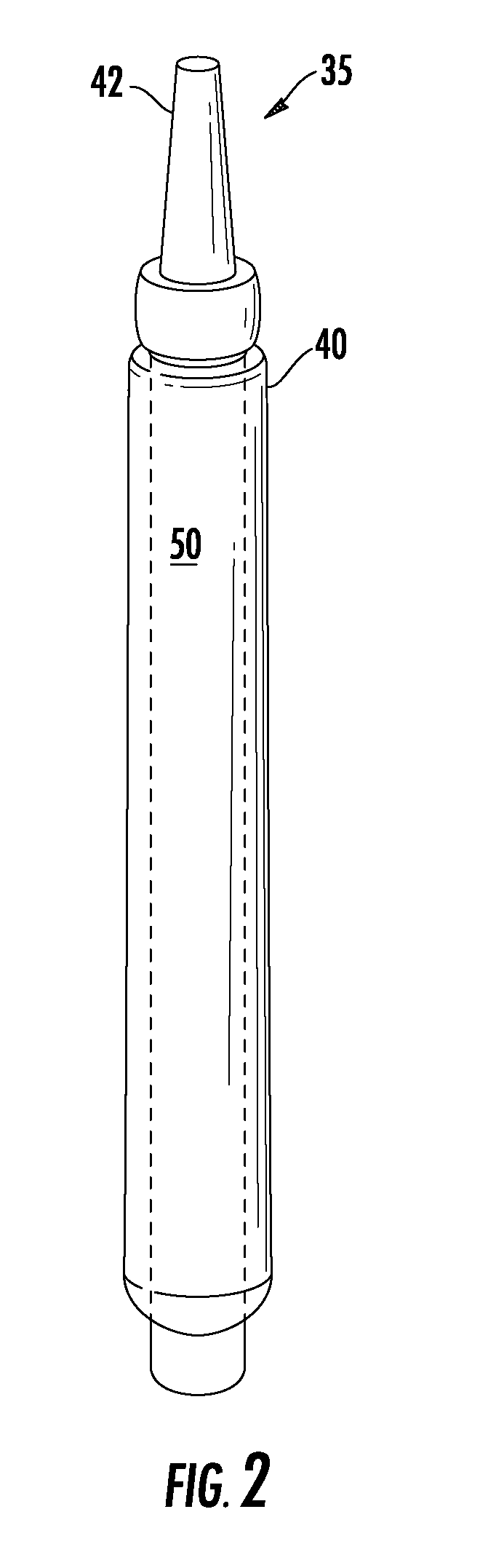
[0035]The invention is a device and method for marking a patient's body with a suitable substance to identify a location of medical interest, such as the site of a patient's injury. The marking substance, or imaging material, is selected to show up on medical images associated with that patient so that a radiologist or clinician evaluating the images can easily determine the exact site of medical interest. The imaging material further marks the patient's skin to assist the person preparing the image in the first place.
[0036]The invention is intended to be used in any setting where medical images are used for diagnosis. Accordingly, the term “medical image” is used in its broadest sense and includes, but is not limited to X-rays, CT scans, fluoroscopy, and MRI technology.
[0037]The invention includes the use of specialized substances, referred to herein as “imaging materials” that show up on a medical image to mark the area of medical interest without obscuring the view of important f...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com