Stable glucagon formulations for the treatment of hypoglycemia
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
formulation examples
III. Formulation Examples
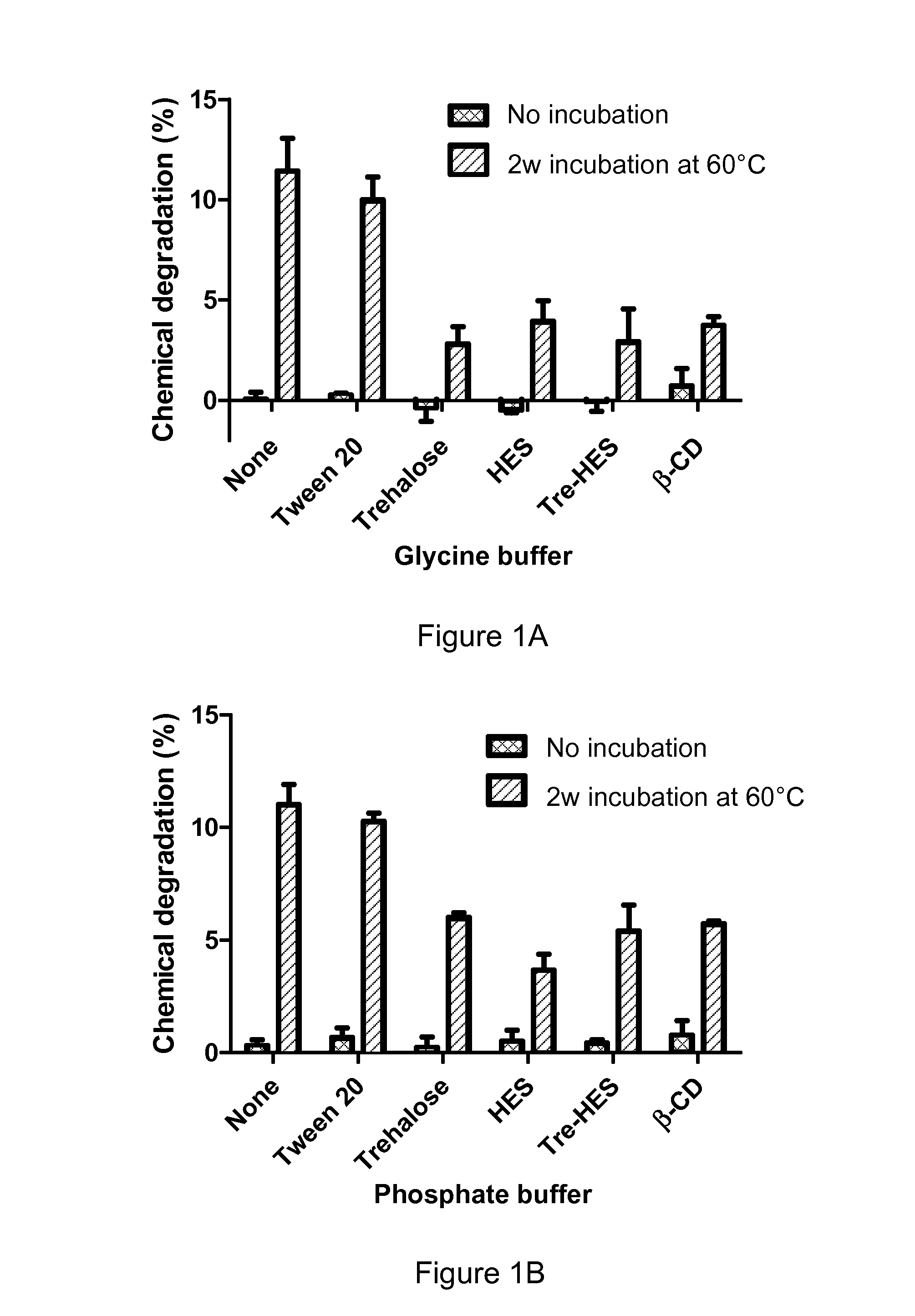
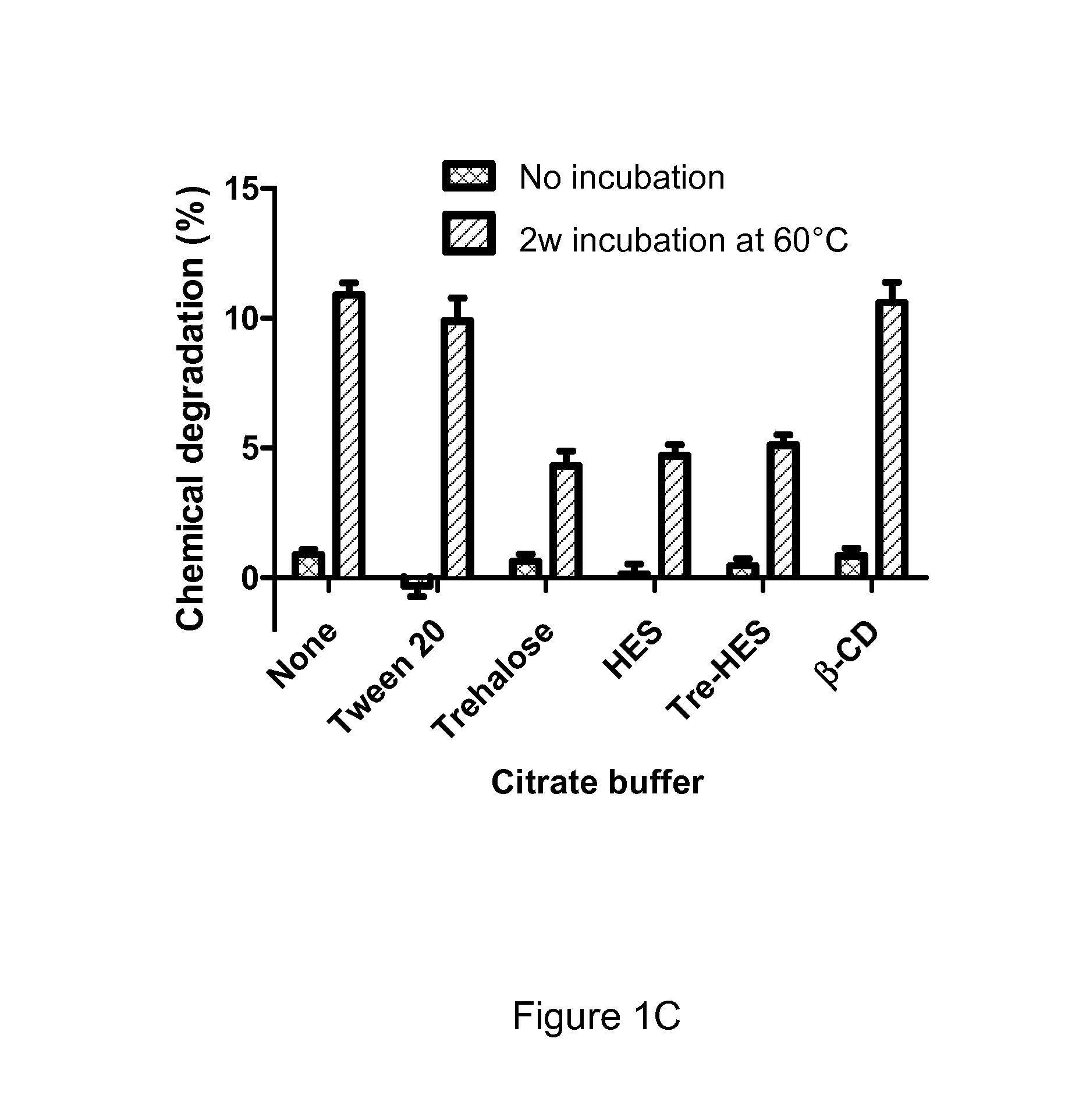
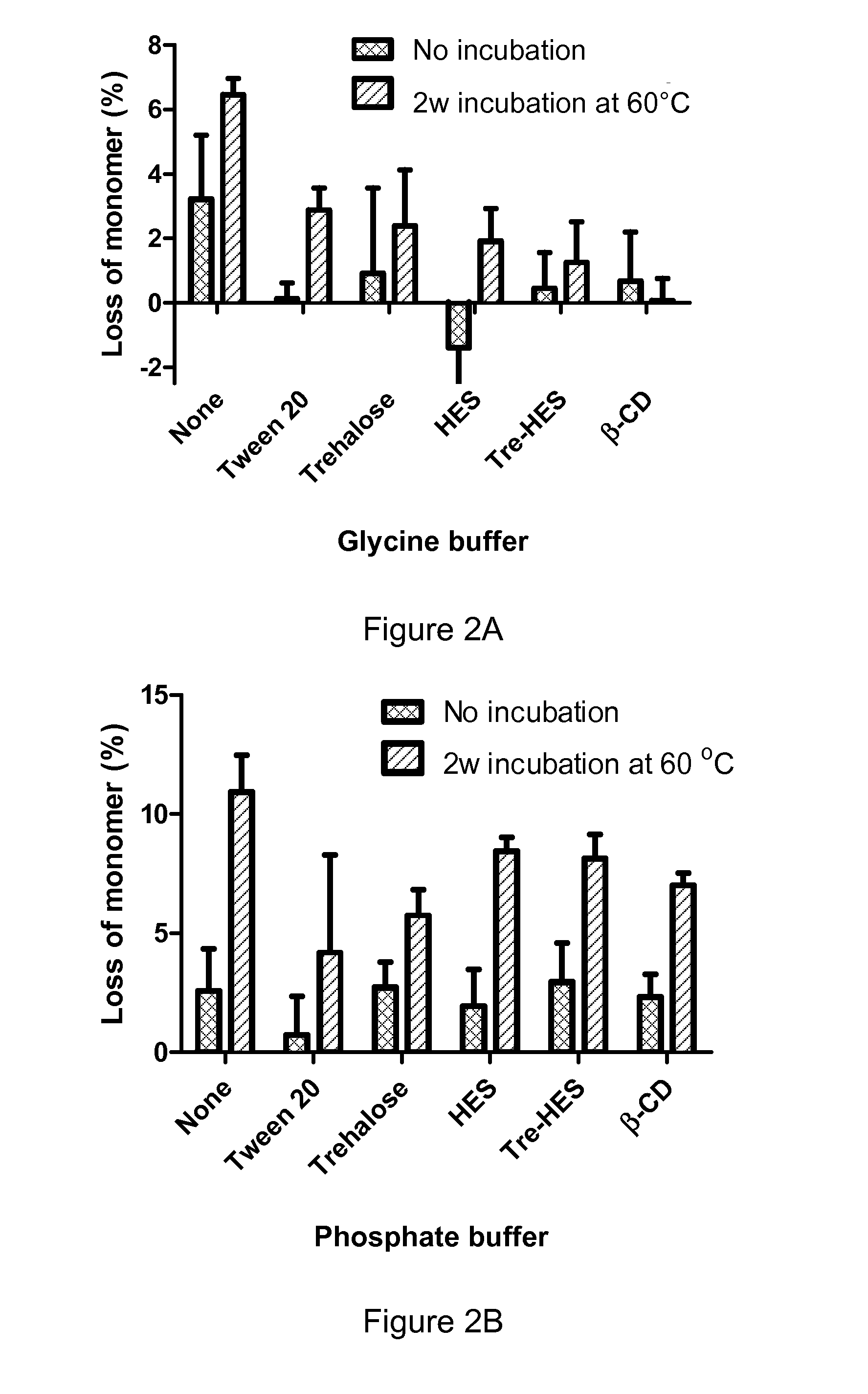
[0079]The present invention will be described in greater detail by way of specific examples. The following examples are offered for illustrative purposes, and are not intended to limit the invention in any manner. Those of skill in the art will readily recognize a variety of noncritical parameters which can be changed or modified to yield essentially the same results.
example 1
Preparation of Glucagon Solutions for Use in Freeze-Drying
[0080]Various solutions were prepared to contain glucagon at a concentration of 10 mg / mL. The solutions contained, alternatively, glycine, citrate or phosphate at 5 mM, generally providing a buffer establishing pH of 3. The solution also contained a sugars, alone or in combination, in amounts equal to the w / v amount of glucagon (1:1) or at 200% (2:1) of the amount of glucagon. The sugars were trehalose, HES, and β-cyclodextrin β-CD. Some solutions also contained Tween 20 at 0.10% w / v as a surfactant. The various formulations mixed to substantial homogeneity in amounts as described in Table 1 below:
TABLE 1Glucagon mixtures for subsequent lyophilization.GycineCitratePhosphateTween-GlucagonBufferBufferBufferTrehaloseHESβ-CD20Formulation(mg / ml)(mM)(mM)(mM)(mg / ml)(mg / ml)(mg / ml)(mg / ml)155000000255000000.01355001000045500010005550055006550000100750500000850500000.0195050100001050500100011505055001250500010013500500001450050000.01155...
example 2
Preparation of Dry Glucagon Powder by Freeze-Drying
[0082]The above formulations of Table 1 were pipetted (0.3 mL) into 3-ml lyophilization vials (13-mm ID). The formulations were lyophilized in a FTS Durastop freeze-drier (Stoneridge, N.Y.). Samples were frozen to about −40° C. at a ramp of 2.5° C. / min and maintained for 2 hours (h) to allow sufficient freezing. The sample temperature was then increased to about −5° C. at a ramp of 2° C. / min and held for 2 h as an annealing step. The temperature was then decreased to about −30° C. at a ramp of 1.5° C. / min and the vacuum was turned on at 60 mTorr. The primary drying was set for 24 h. The temperature was gradually increased to about 40° C. at a ramp of 0.5° C. / min and held for additional 10 h. After drying was complete, the vials were capped under vacuum using XX stoppers from the West Pharmaceutical company (product #10123524). None of the formulations showed any evidence of cake collapse following freeze-drying. These formulations w...
PUM
| Property | Measurement | Unit |
|---|---|---|
| Stability | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com