Calibrated Systems, Devices and Methods for Preventing, Detecting, and Treating Pressure-Induced Ischemia, Pressure Ulcers, Pneumonia and Other Conditions
a technology of pressure ulcers and systems, applied in the field of systems, devices and methods for the detection of compromised tissue perfusion and other issues, can solve the problems of affecting the treatment of pressure ulcers, and affecting the treatment effect of patients, so as to reduce or eliminate physical contact, improve the effect of blood circulation and airflow
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
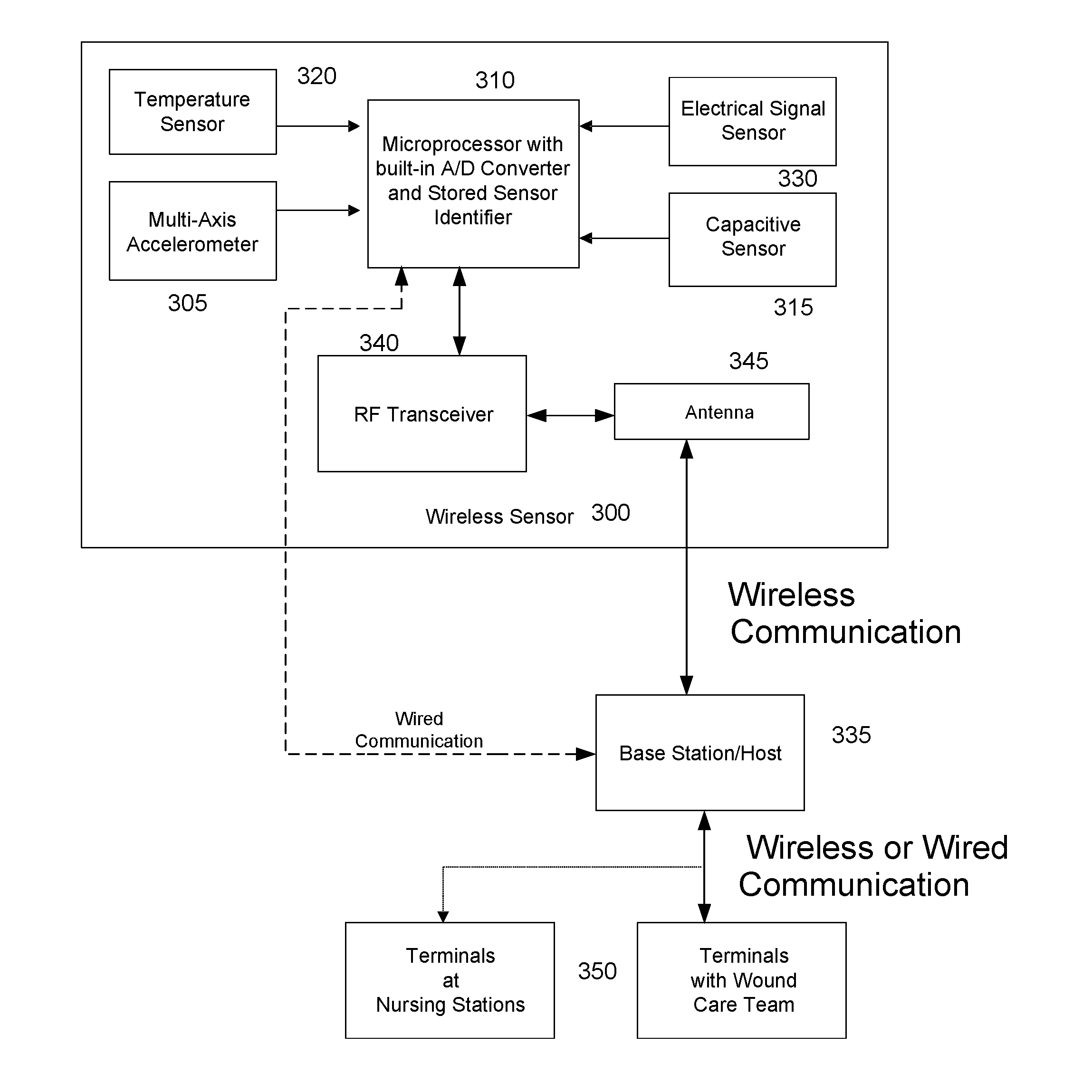
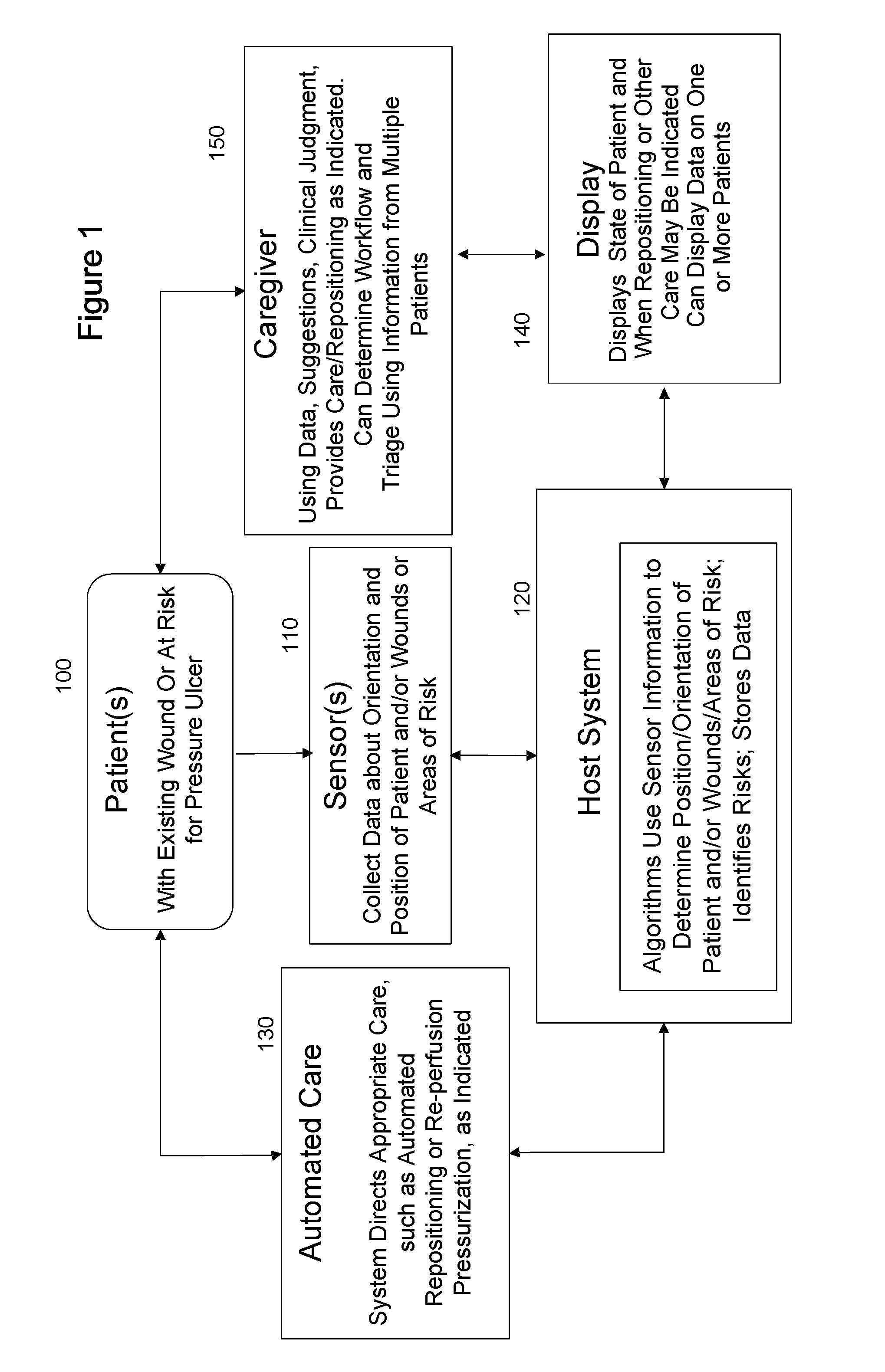
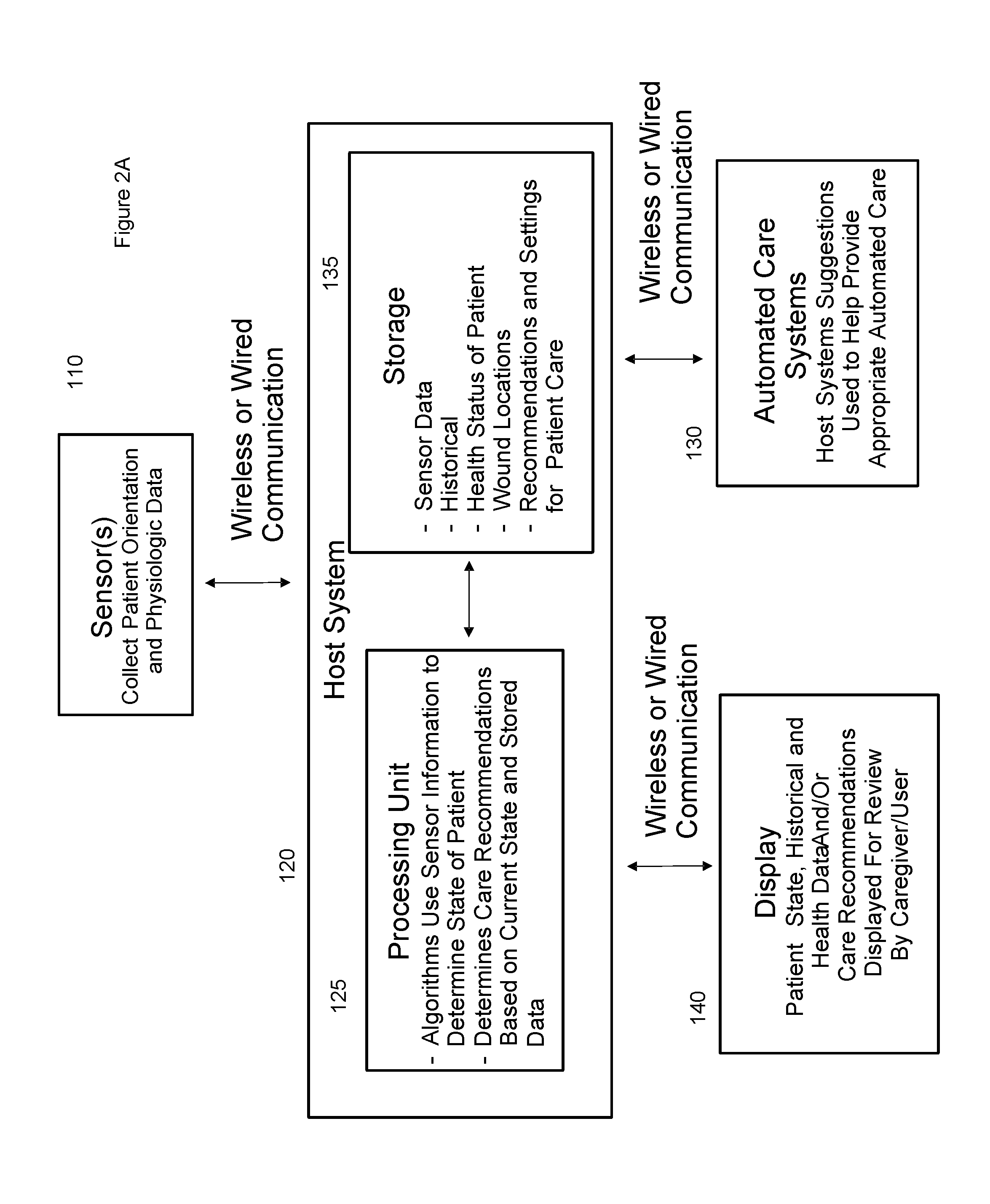
[0048]Referring first to FIG. 1, an embodiment of a system in accordance with an aspect of the invention is illustrated in flow diagram form. A patient 100 requiring monitoring, and in at least some instances having an existing wound or being at risk for developing a pressure ulcer, is associated with one or more sensors 110. The sensors collect data about the orientation, position, and movement of the patient and / or wounds and / or areas of compromised tissue perfusion and / or areas of risk. The sensors communicate with a host system 120, typically a computer running at least one program for processing the incoming sensor information to determine the position or orientation or movements of a patient, wounds or areas of compromised tissue perfusion or areas of risk on the patient. The program also uses historical and other data to analyze the sensor data and identify risks. In at least some embodiments, the data, including both the sensor data and the analytical data, is stored for fut...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com