Method for internal compression hemostasis after minimally invasive breast lump rotary varicotomy and hemostatic balloon
A breast lump, compression hemostasis technology, applied in the direction of surgery, medical science, etc., can solve the problems of gauze and chest belt displacement, rebleeding in tissue defect areas, hemorrhagic shock of patients, etc., to achieve accurate position, durable and reliable hemostasis effect Effect
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
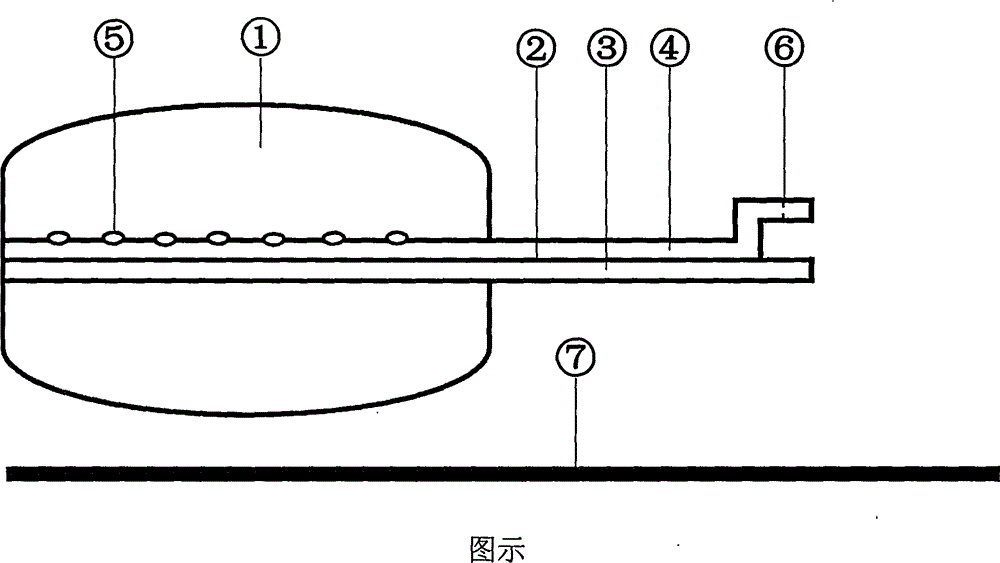
[0009] The present invention consists of three parts: a liquid-fillable balloon ①, a double-lumen catheter ② and a catheter core ⑦. The front end of the injection catheter lumen ④ is located in the balloon, and there is a side hole ⑤ in it, and the end is equipped with a self-closing liquid injection cap ⑥; the front end of the drainage catheter lumen ③ is flush with the front end of the balloon, and the end is open . The above-mentioned main structure is made of medical silica gel or medical rubber. Catheter core ⑦ is made of polyethylene material, should have certain hardness and elasticity, and its diameter is slightly smaller than the diameter of drainage catheter lumen ③, and length is about 3 centimeters longer than the latter.
[0010] After minimally invasive rotary breast mass resection, insert the catheter core ⑦ into the drainage catheter lumen ③. At this time, the fluid-inflatable balloon ① is still in a non-filled state, and the front end of the double-lumen cath...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com