Braided stent to be implanted in a blood vessel
a braided stent and blood vessel technology, applied in the field of braided stents to be implanted in blood vessels, can solve the problems of correspondingly reversed length reduction upon expansion of braided stents, and affecting the effect of length
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
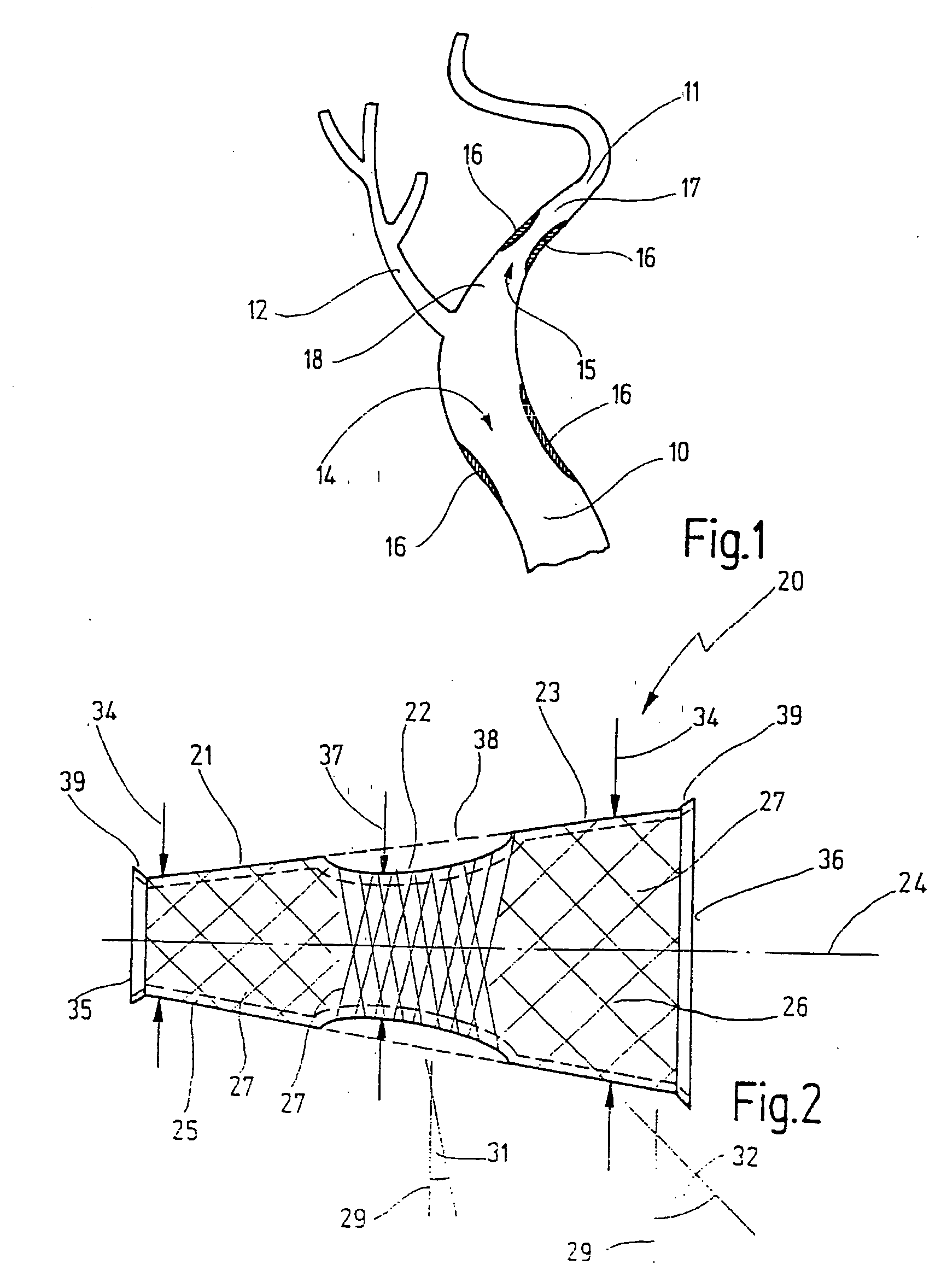
[0069]FIG. 1 shows the geometric situation at the carotid bifurcation in a human. The common carotid artery 10 merges here into the internal carotid artery 11, with the external carotid artery 12 branching off. A stenosis 14 in the common carotid artery and a stenosis 15 in the internal carotid artery 11 are indicated by hard, brittle areas 16. It will be noted that the internal carotid artery 11 has a smaller internal diameter in an area 17 in the distal direction from the stenosis 15 than it does in an area 18 in the proximal direction from the stenosis 15.
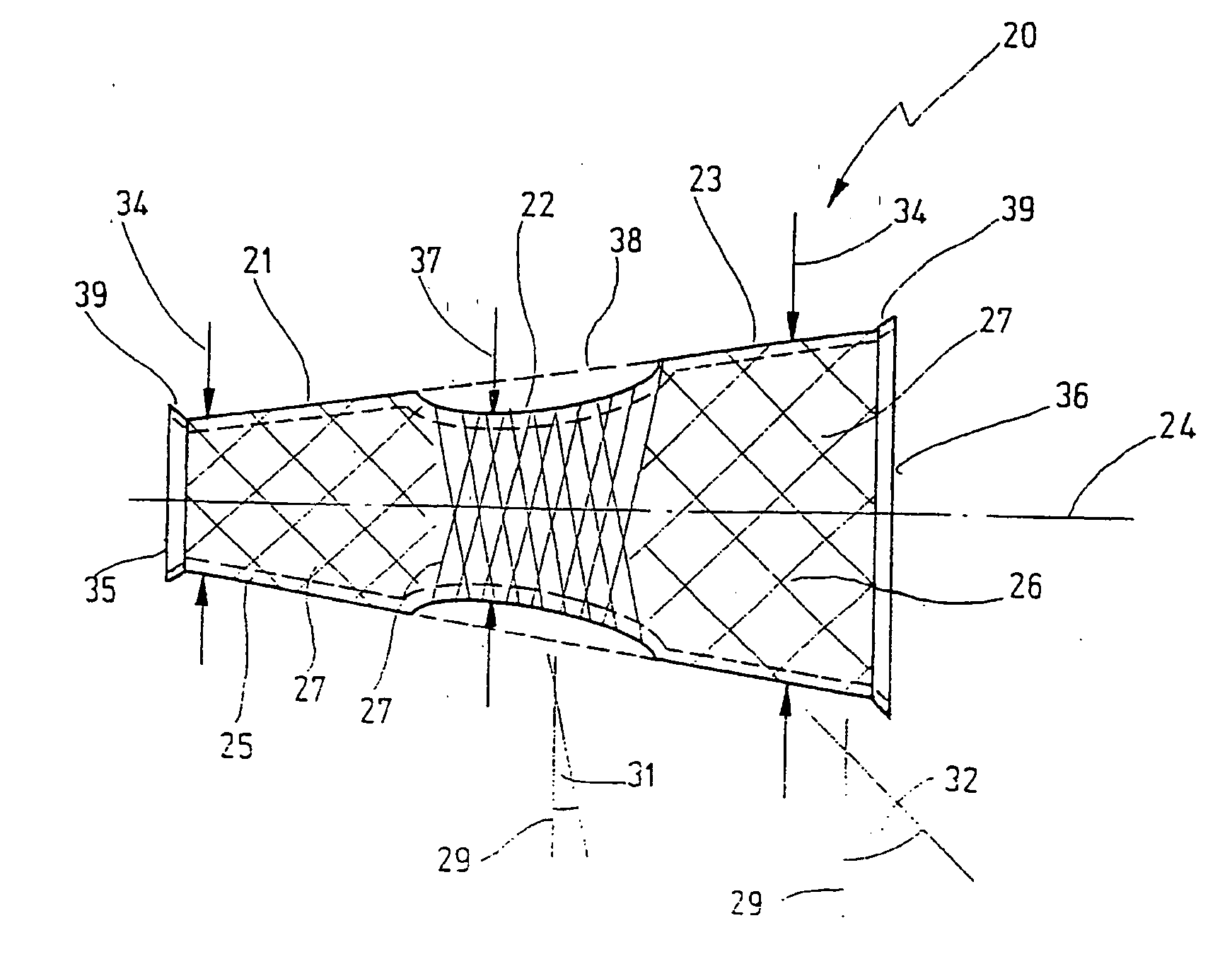
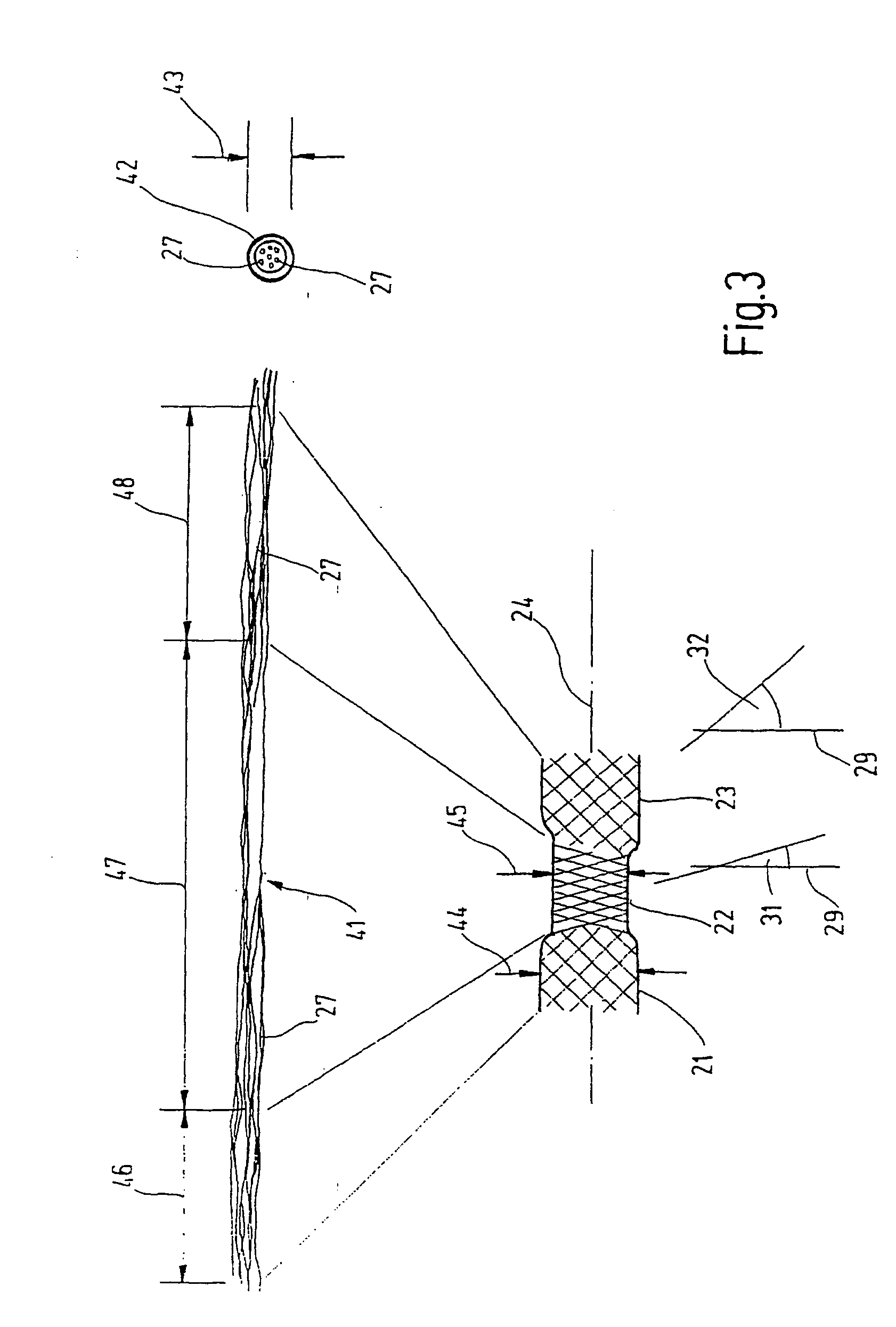
[0070]FIG. 2 shows a braided stent 20 according to the invention which is intended to be inserted into the area of the stenosis 15 in FIG. 1. The braided stent 20 has a distal portion 21, a central portion 22 and a proximal portion 23 arranged one after the other in the longitudinal direction 24 of the braided stent 20.
[0071] The braided stent 20 has a hollow body whose circumferential surface indicated by 25 is made from a br...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com