Apparatus And Method For Cardiac Ablation
a technology of cardiac ablation and apparatus, applied in the field of medical devices, can solve the problems of life-threatening arrhythmias, inability to treat dysrhythmias of the heart with drugs, and high cost of both procedures
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
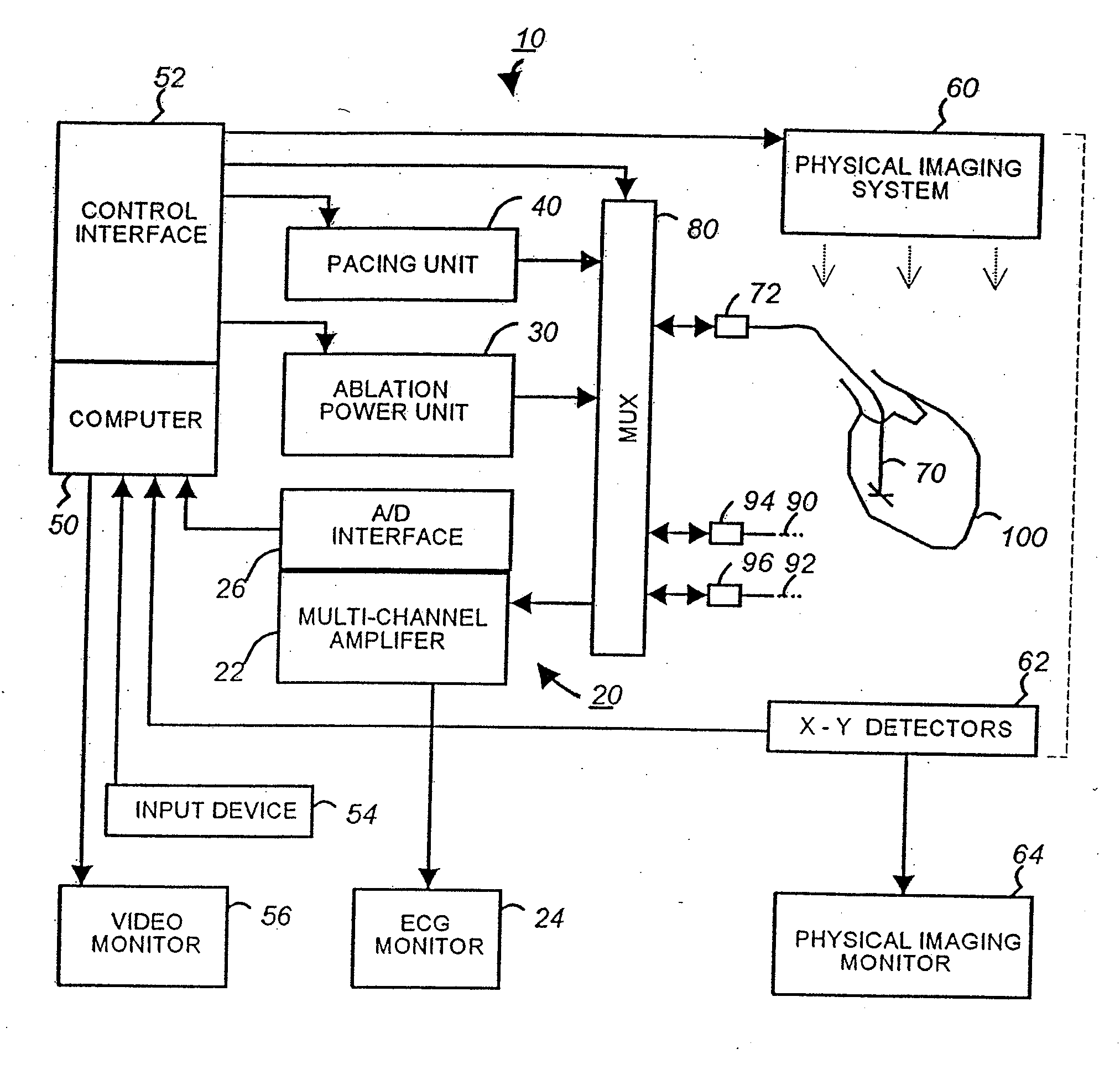
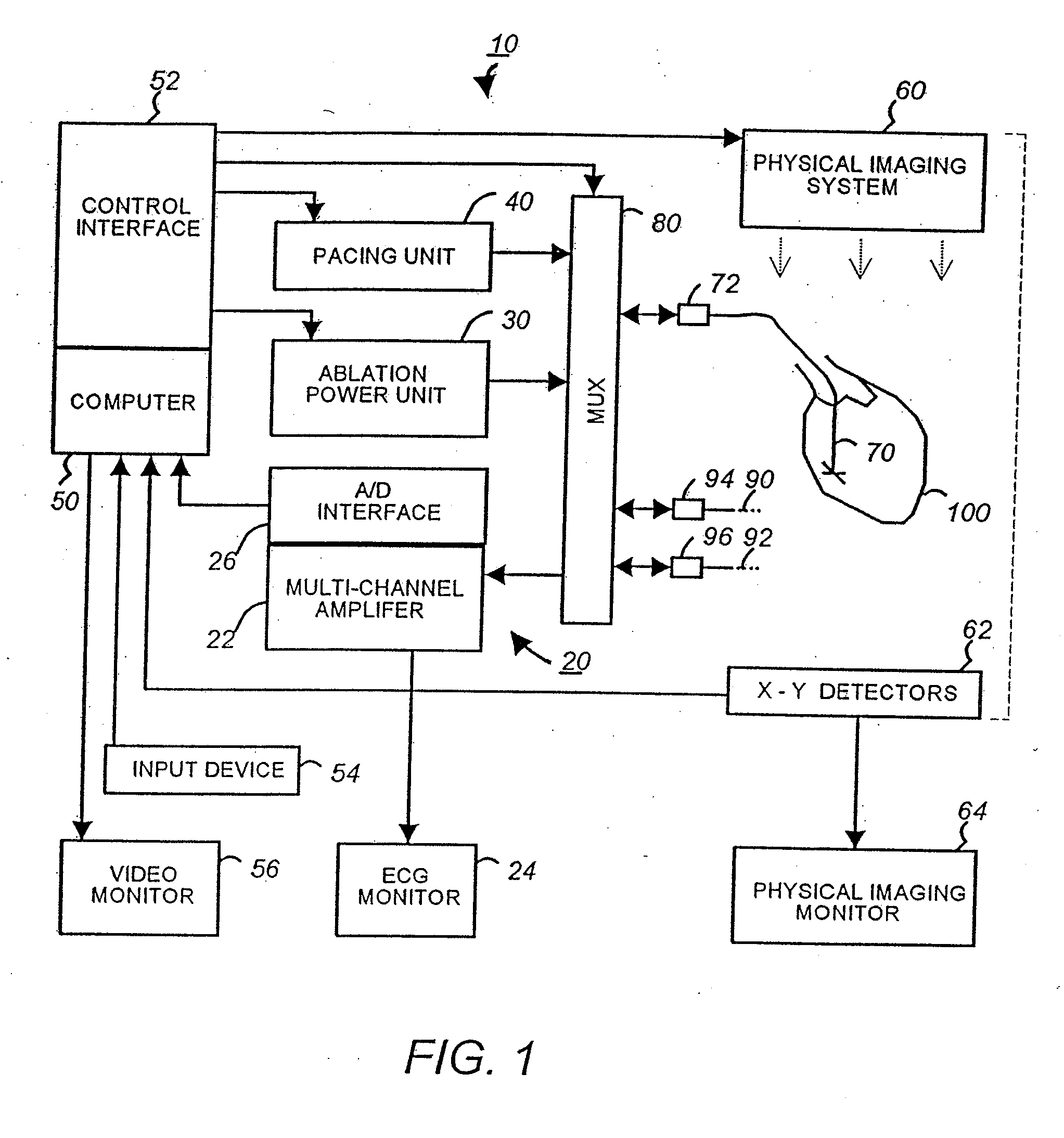
[0055]FIG. 1 is a schematic block diagram of a multi-electrode catheter mapping and ablation system 10 according to a preferred embodiment of the present invention.
[0056] The system 10 essentially comprises of three functioning units, namely a mapping unit 20, an ablation unit 30 and a pacing unit 40. A computer 50 controls the operation of each of the units and their cooperations via a control interface 52. The computer receives operator inputs from an input device 54 such as a keyboard, a mouse and a control panel. The output of the computer may be displayed on a video monitor 56 or other output devices (not shown).
[0057] In the preferred embodiment the system 10 also includes a physical imaging system 60. The physical imaging system 60 is preferably a 2-axis fluoroscope or an ultrasonic imaging system. The physical imaging system 60 is controllable by the computer 50 via the control interface 52. In one implementation, the computer triggers the physical imaging system to take “...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com