Patents
Literature
143 results about "Cardiac Ablation" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
A procedure intended to eliminate or modify a focus or re-entry circuit that causes an arrhythmia in the heart. (ACC)
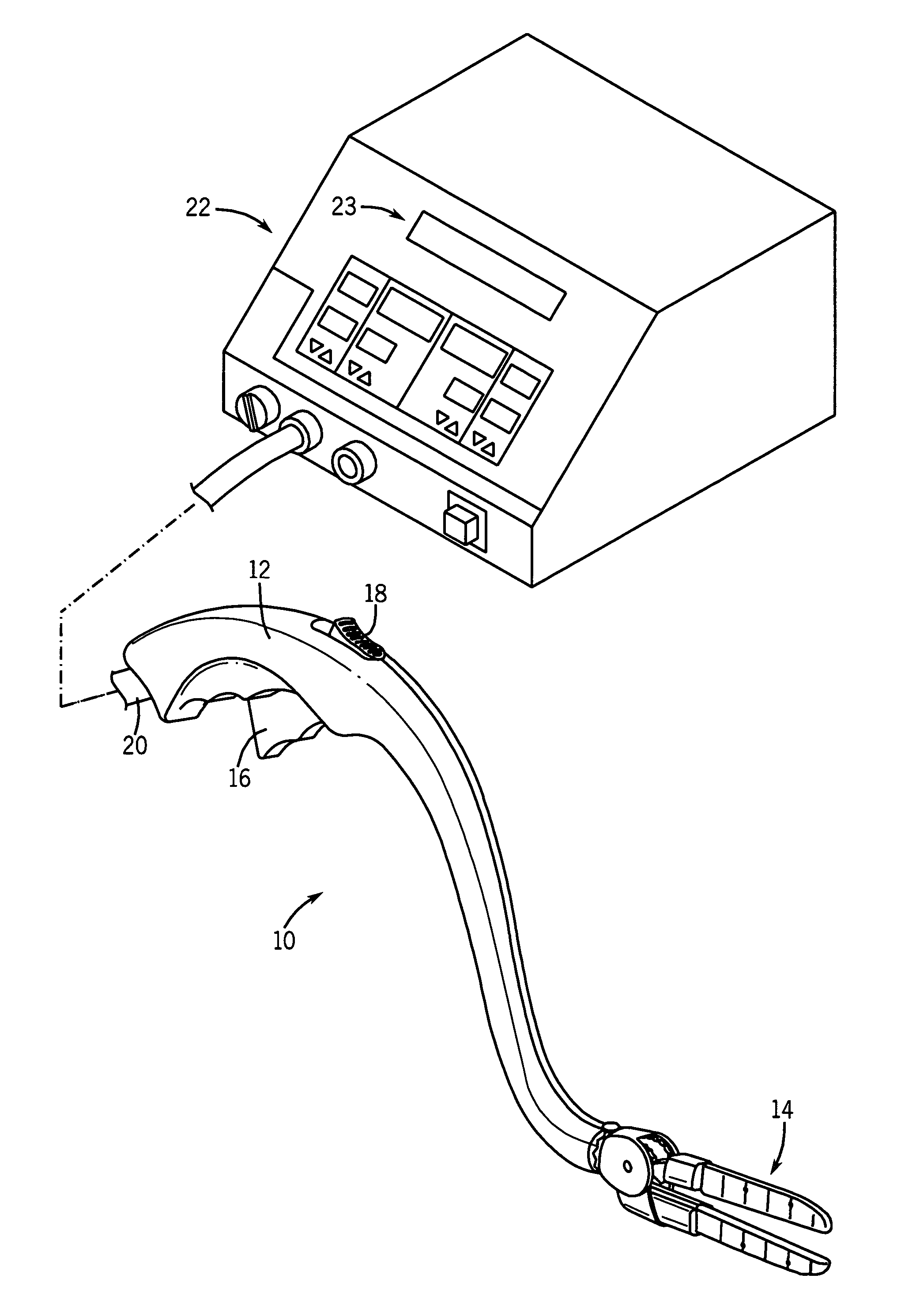
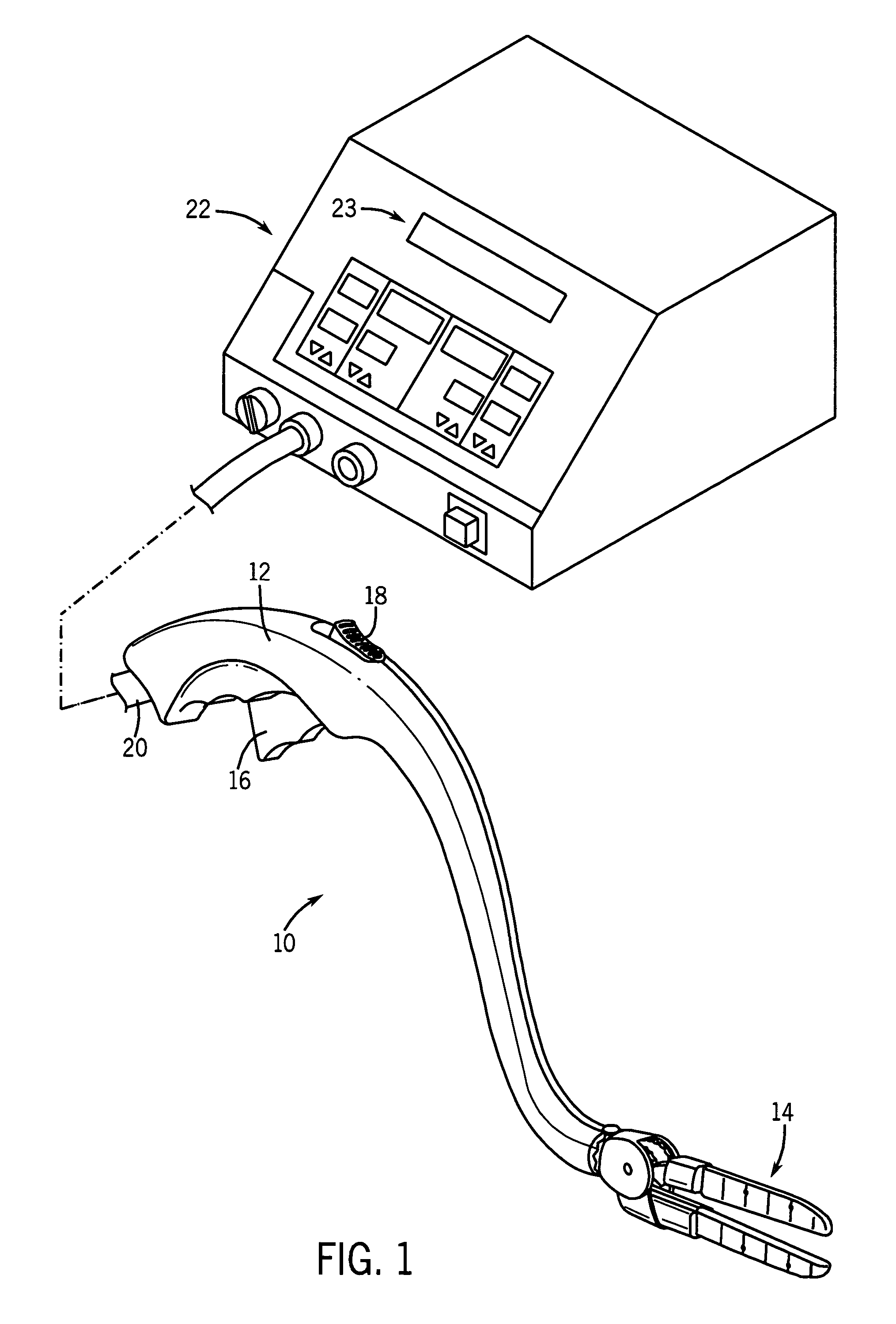
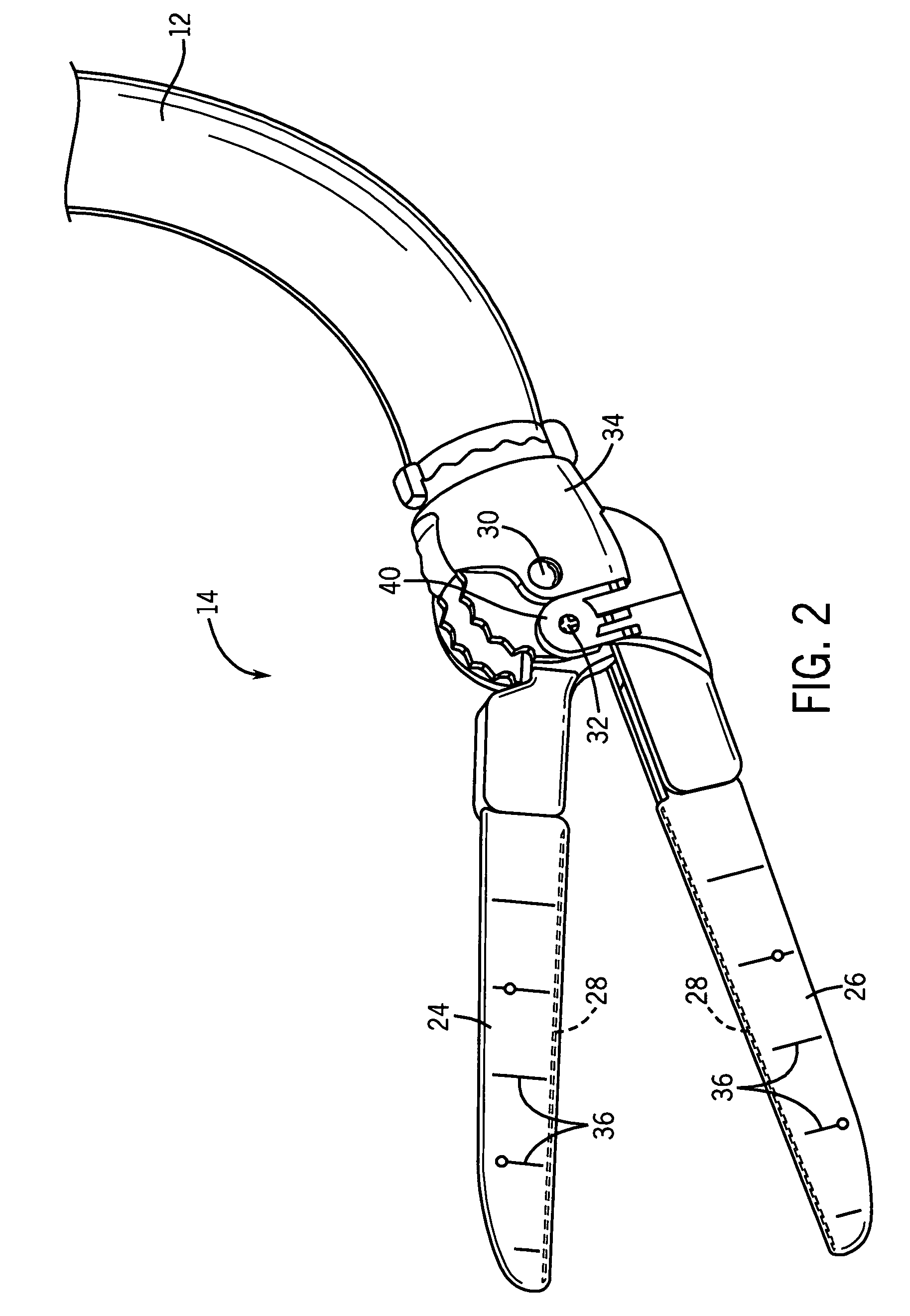
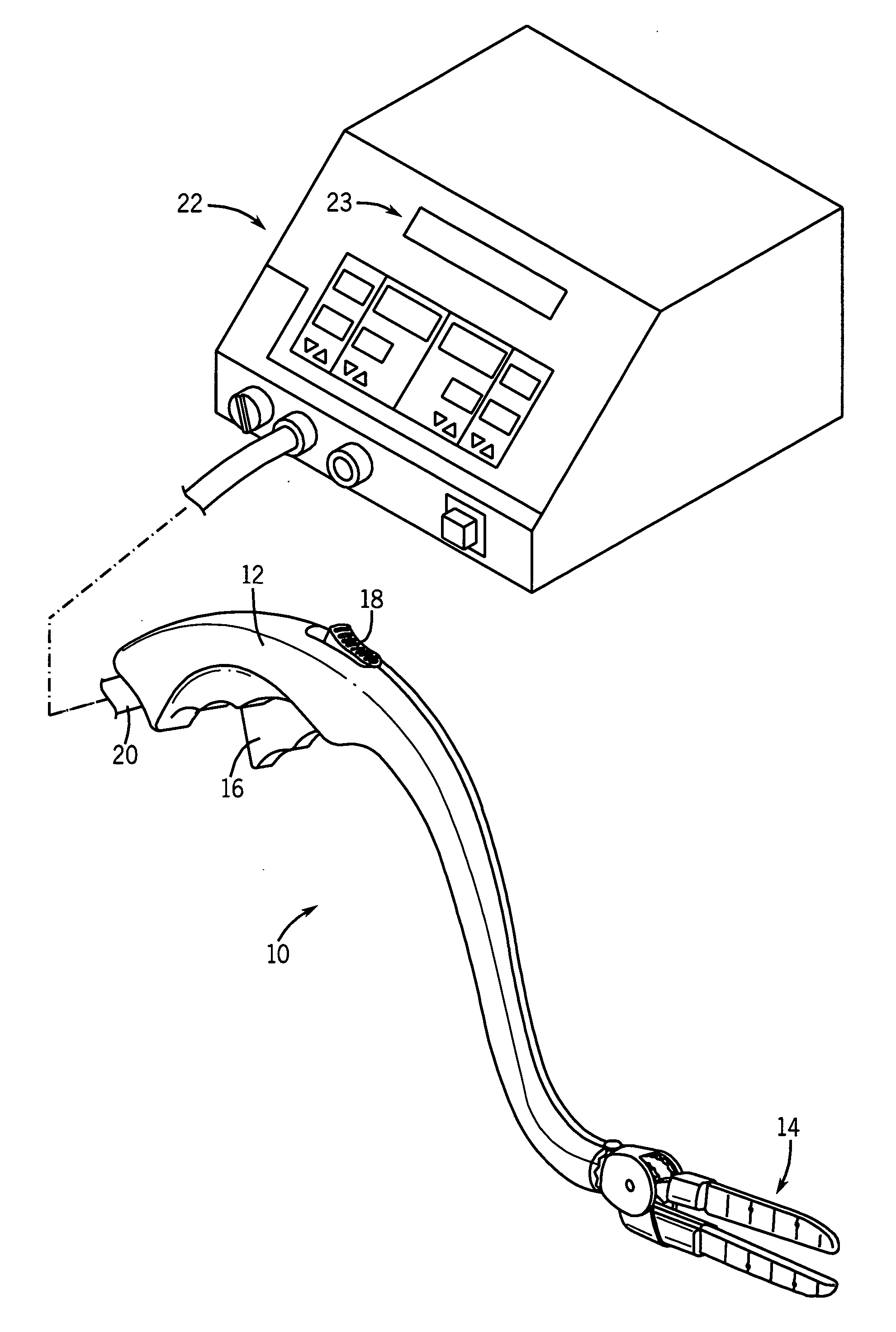
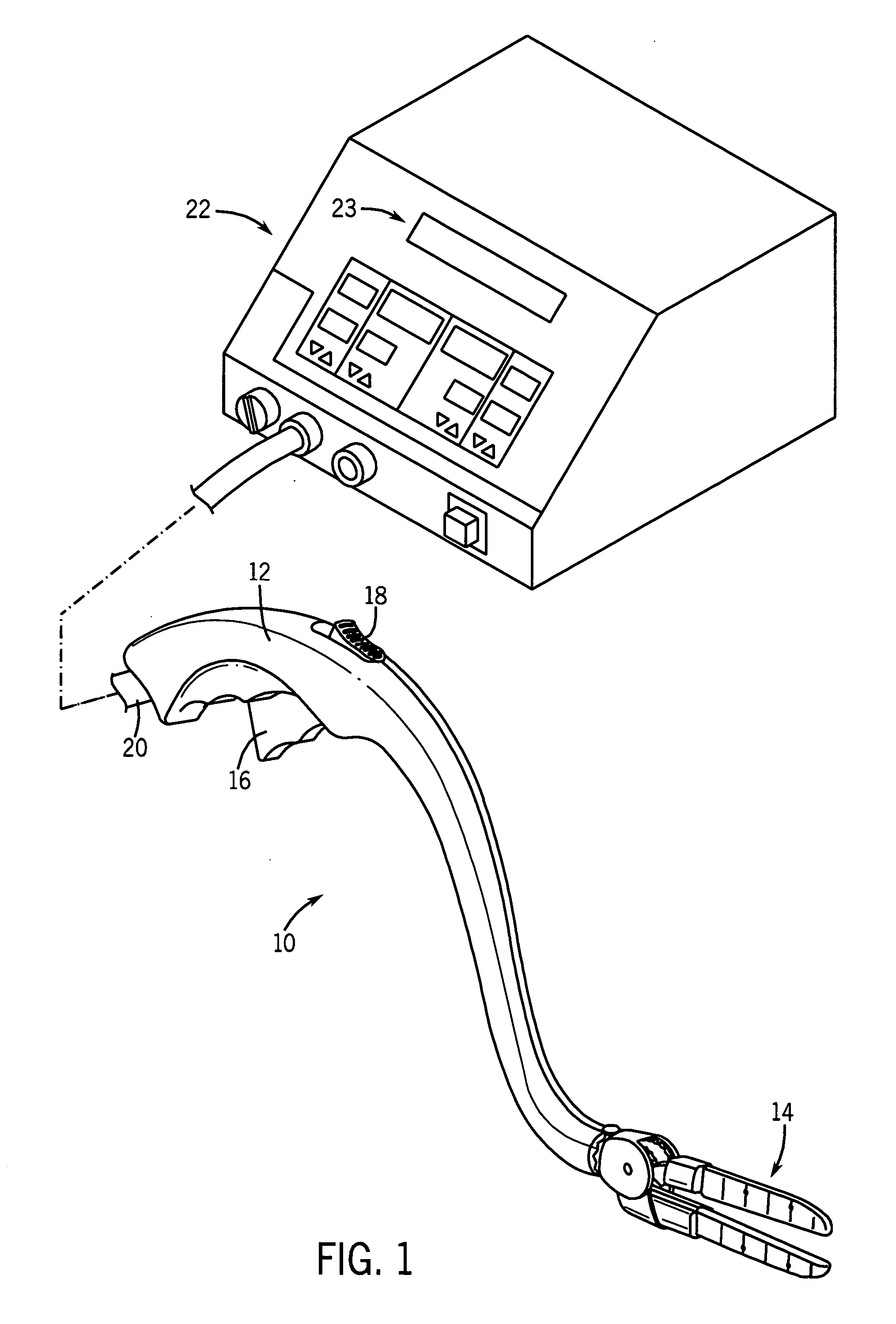
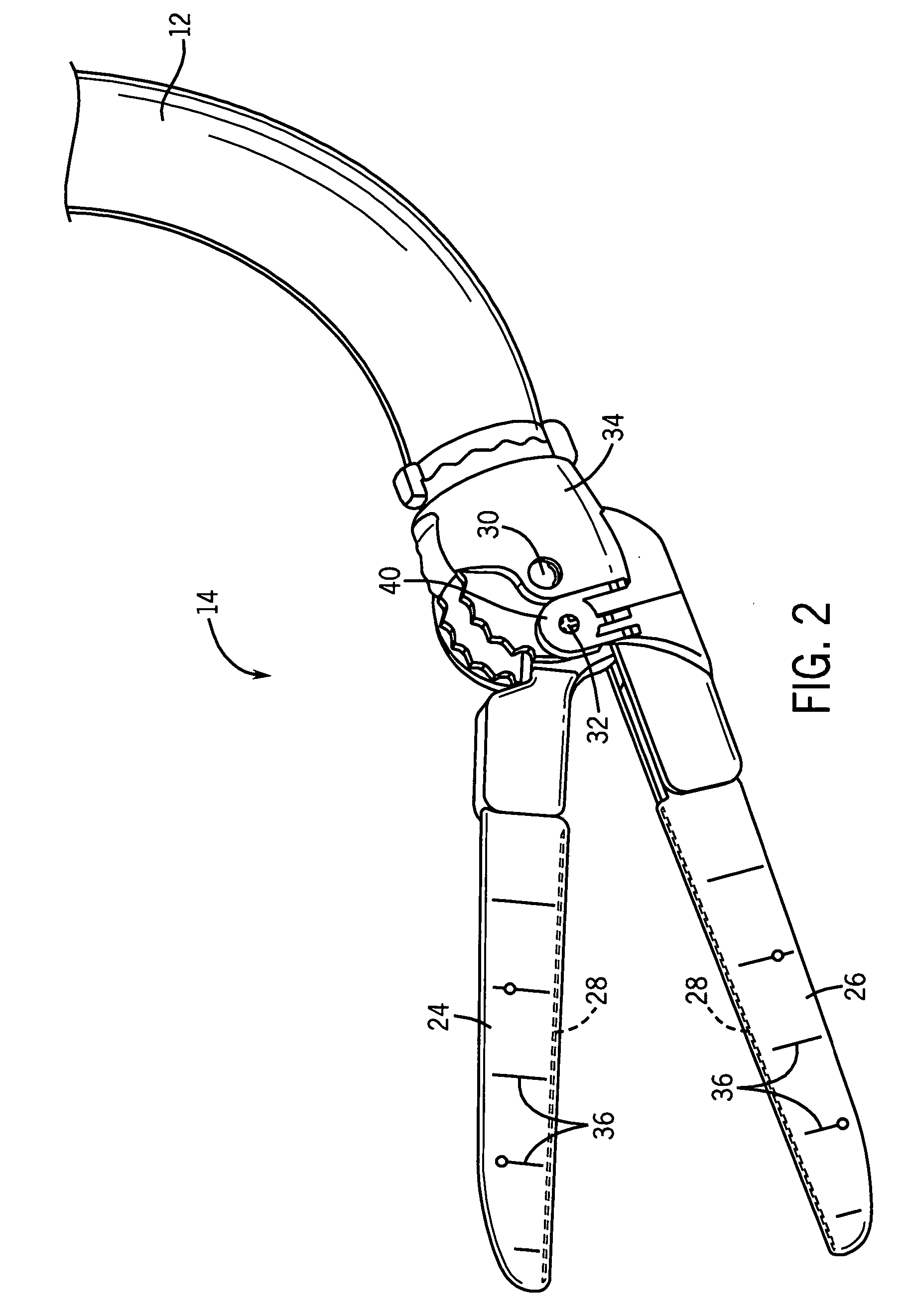
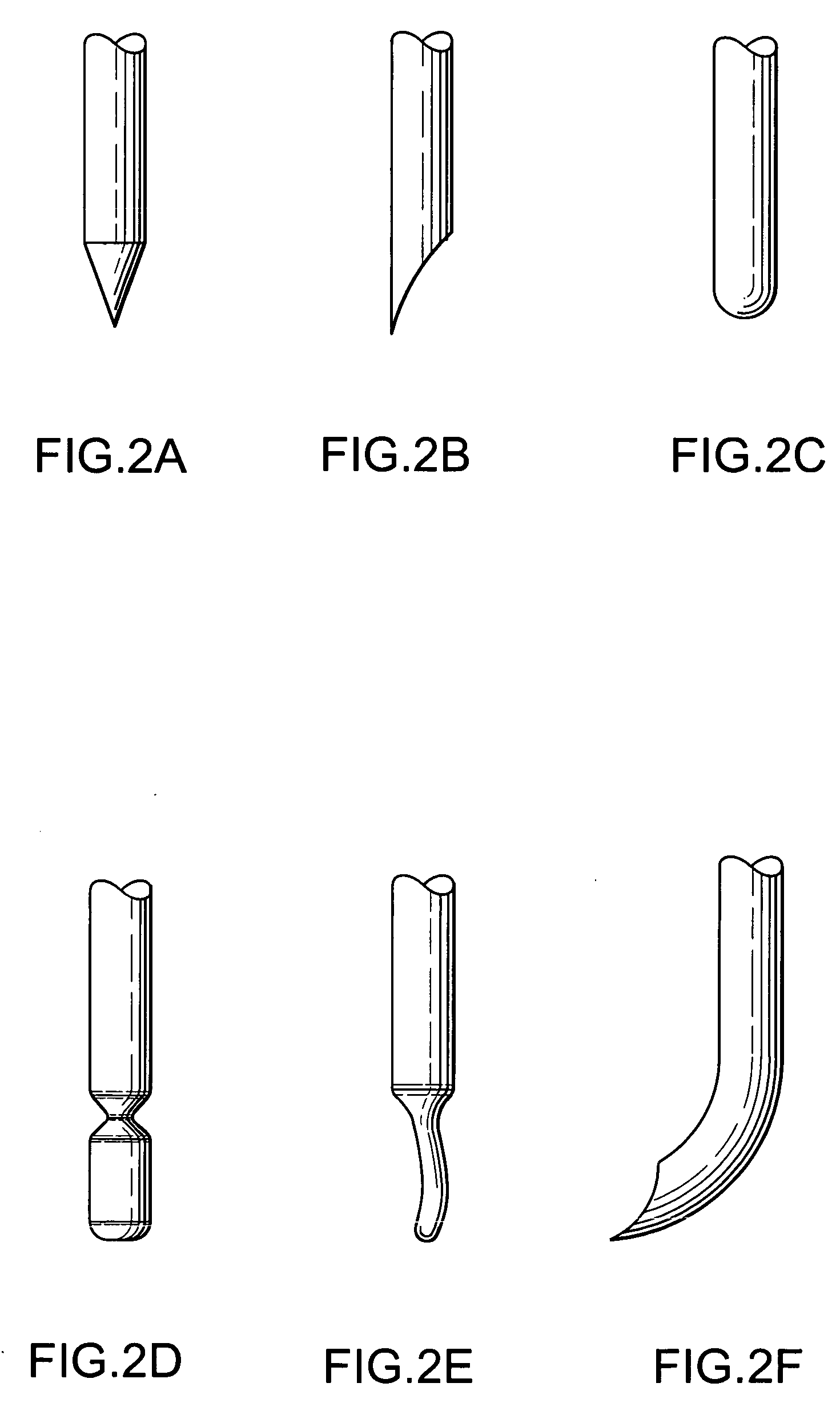
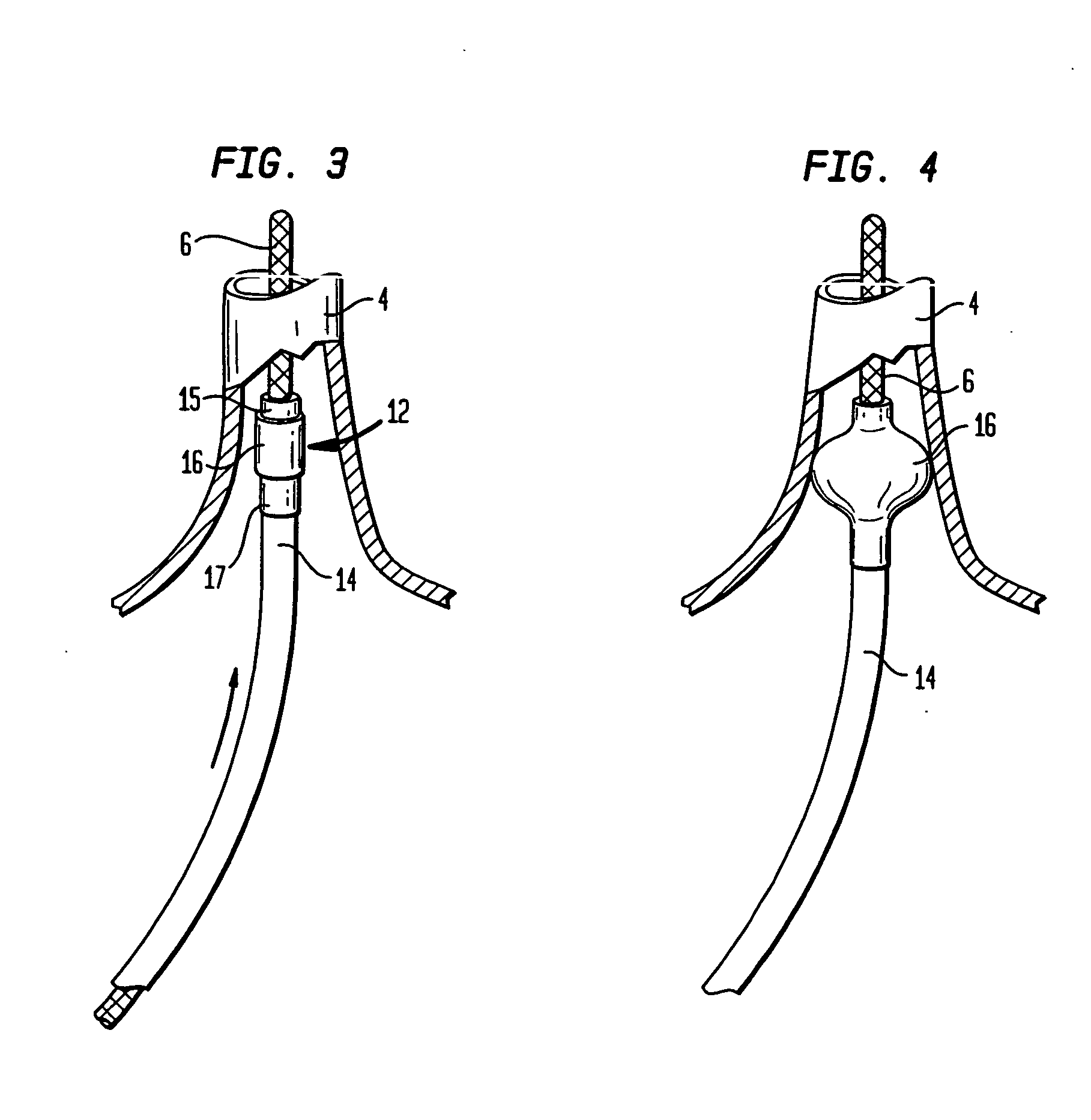
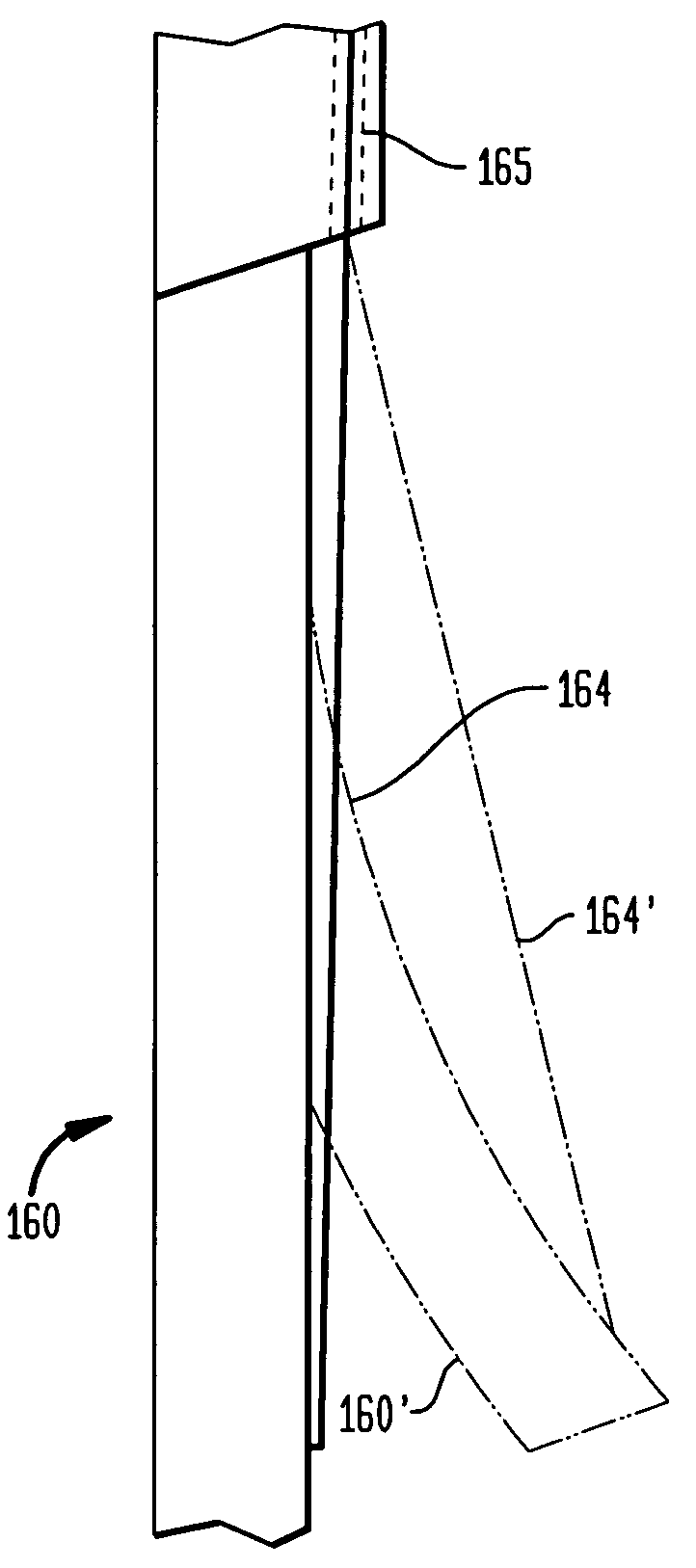
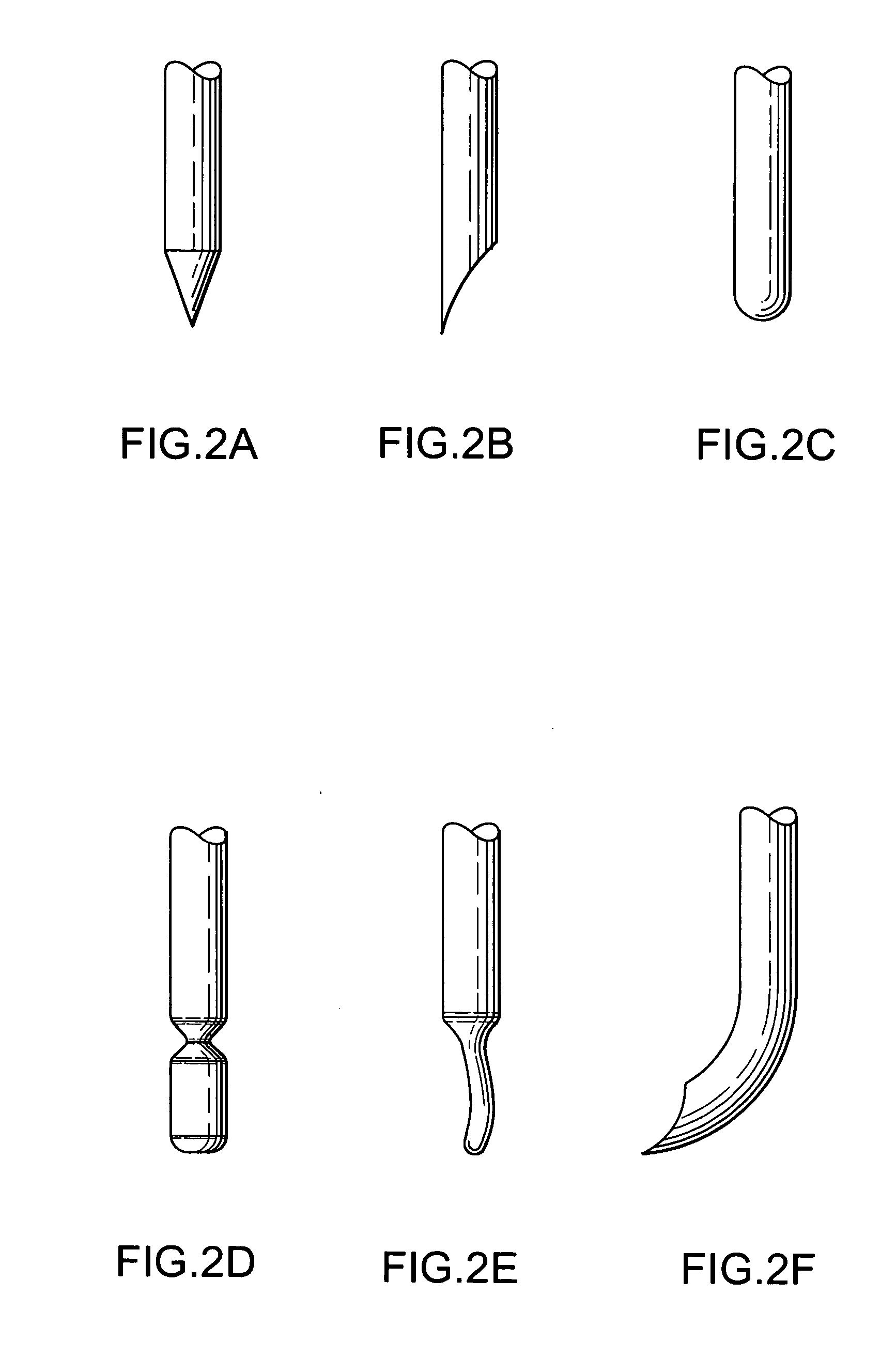
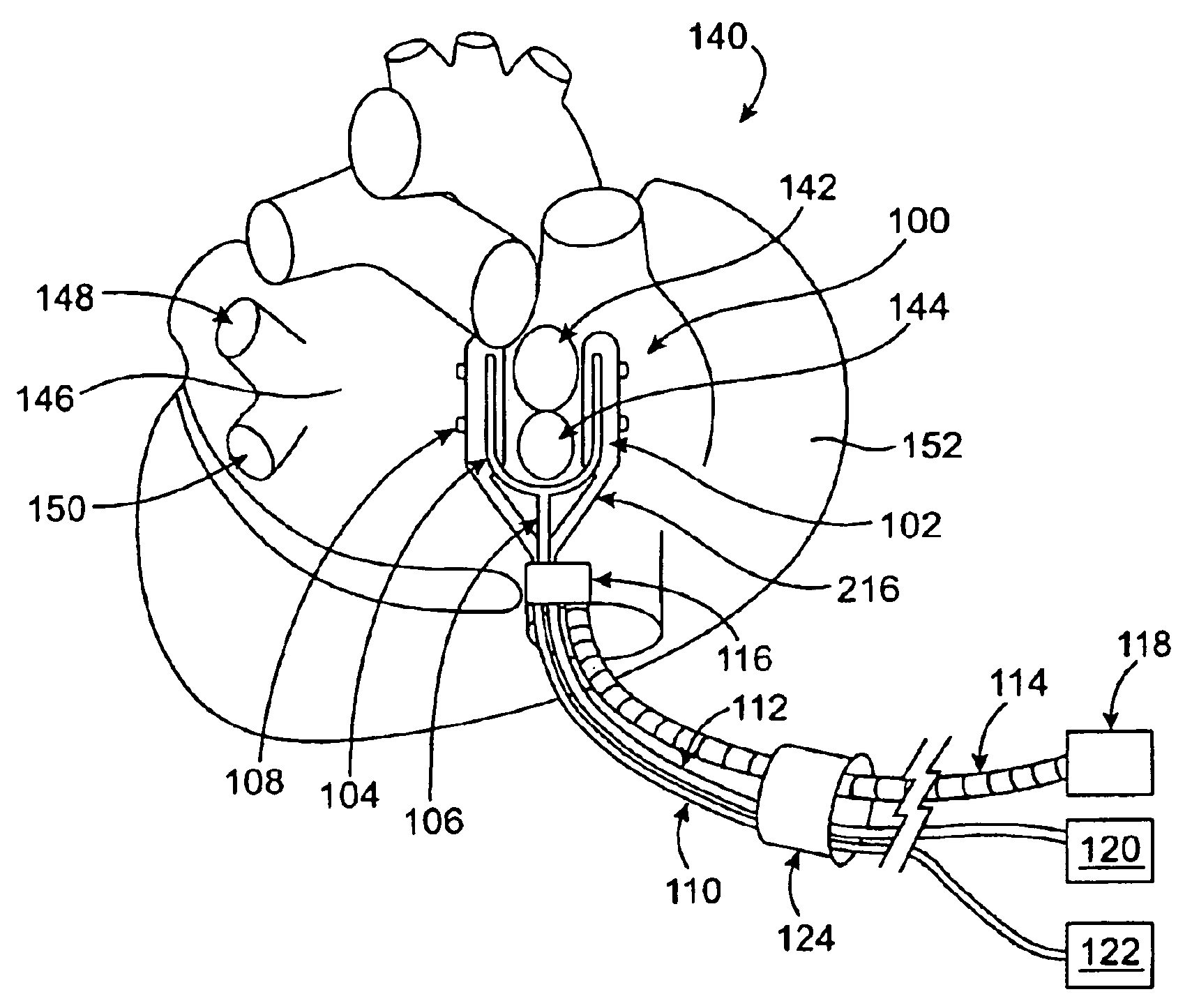
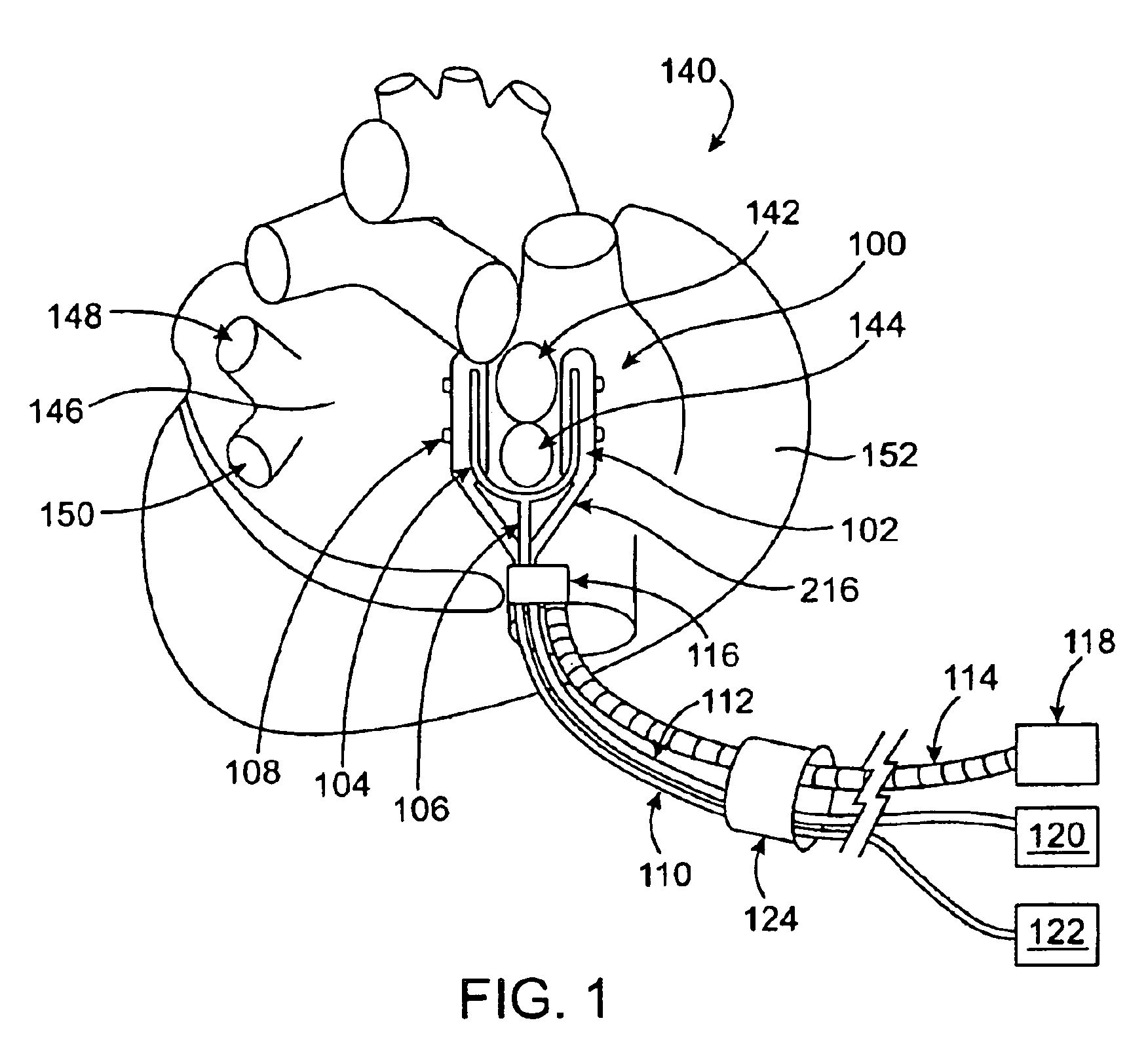
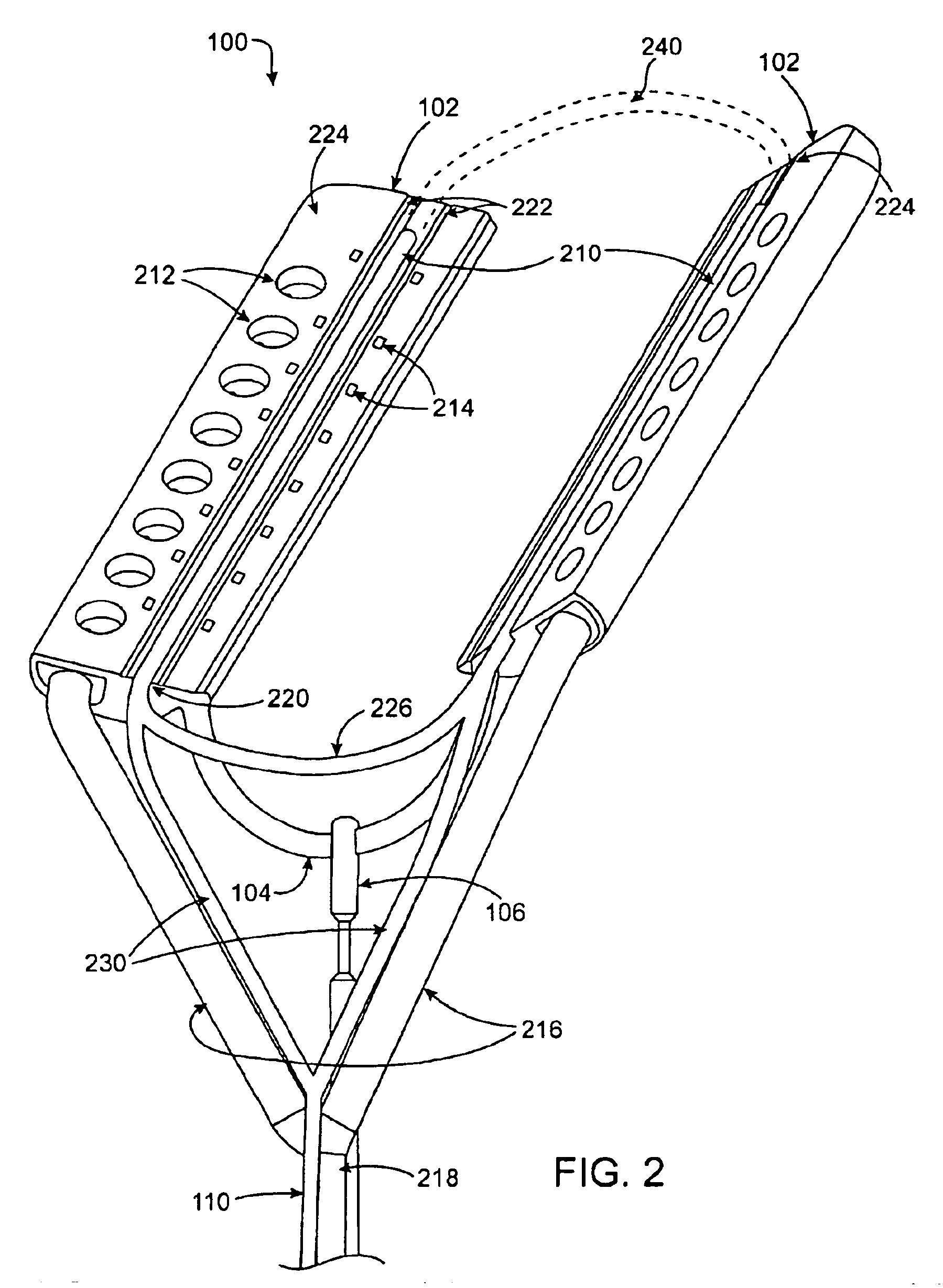
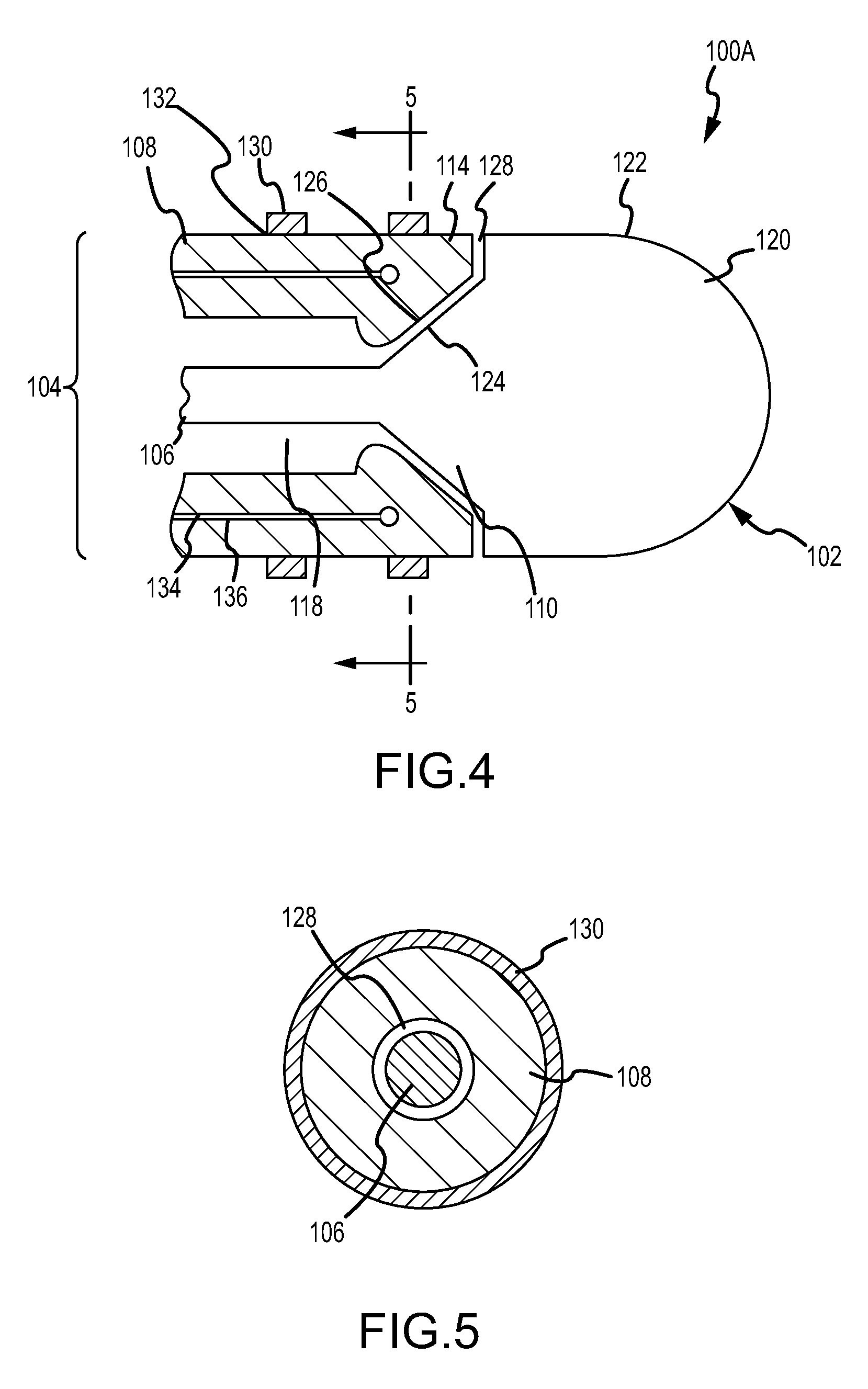
Device and method for determining tissue thickness and creating cardiac ablation lesions
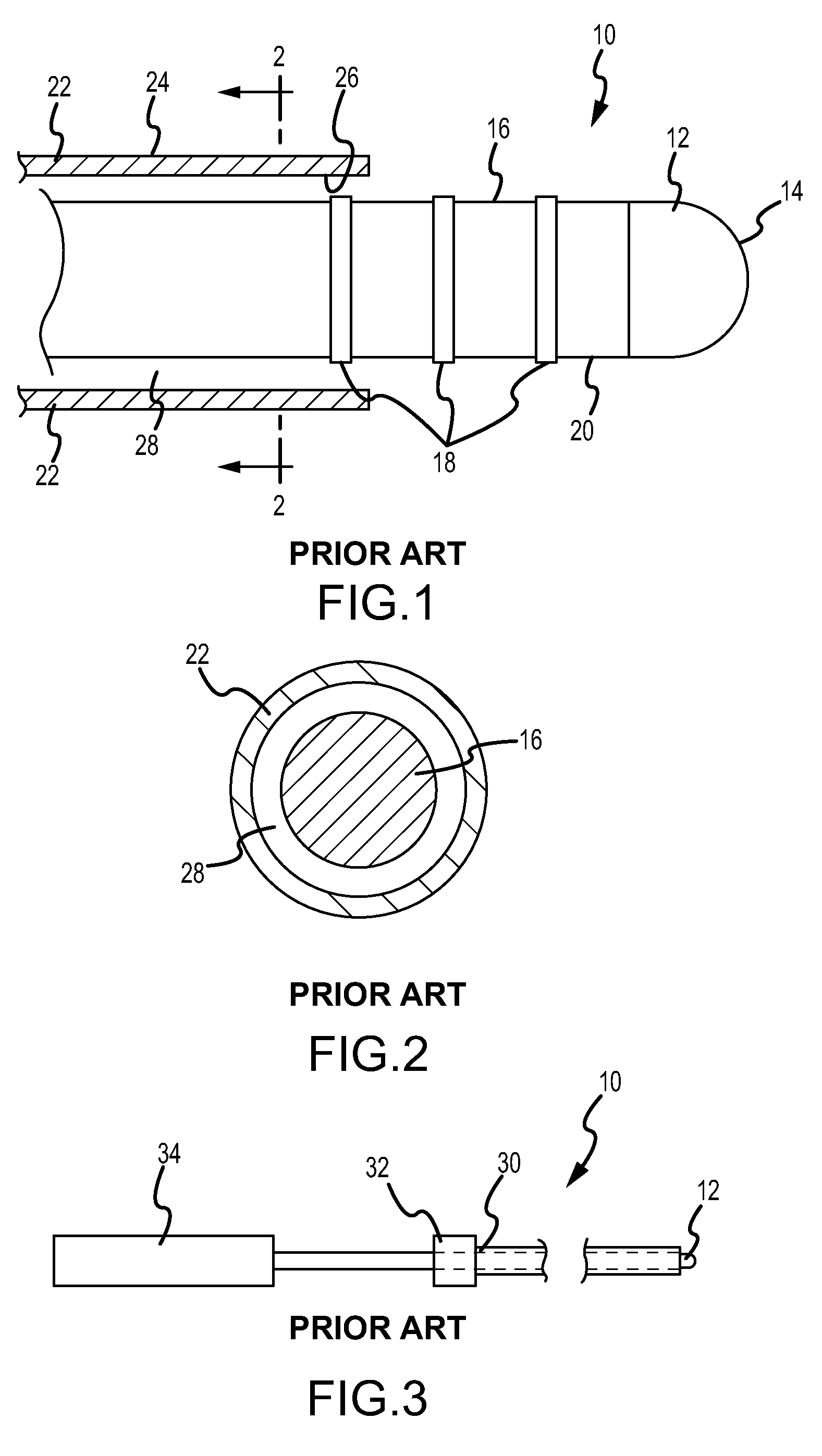
A tissue ablation device has a handle and an ablation head coupled to the handle. The ablation head has a first jaw, a second jaw, and an ablative element coupled to at least one of the first and second jaws. A thickness measurement device may be coupled to the ablation device to indicate the distance separating the first and second jaws. Further, a force measurement device may be coupled to the ablation device to measure the force being applied by the first and second jaws to a piece of tissue. Further, a strain measurement device may be coupled to the ablation device to indicate the strain resulting in a piece of tissue disposed between the first and second jaws when a stress is applied to the tissue.
Owner:MEDTRONIC INC
Device and method for determining tissue thickness and creating cardiac ablation lesions
A tissue ablation device has a handle and an ablation head coupled to the handle. The ablation head has a first jaw, a second jaw, and an ablative element coupled to at least one of the first and second jaws. A thickness measurement device may be coupled to the ablation device to indicate the distance separating the first and second jaws. Further, a force measurement device may be coupled to the ablation device to measure the force being applied by the first and second jaws to a piece of tissue. Further, a strain measurement device may be coupled to the ablation device to indicate the strain resulting in a piece of tissue disposed between the first and second jaws when a stress is applied to the tissue.
Owner:MEDTRONIC INC
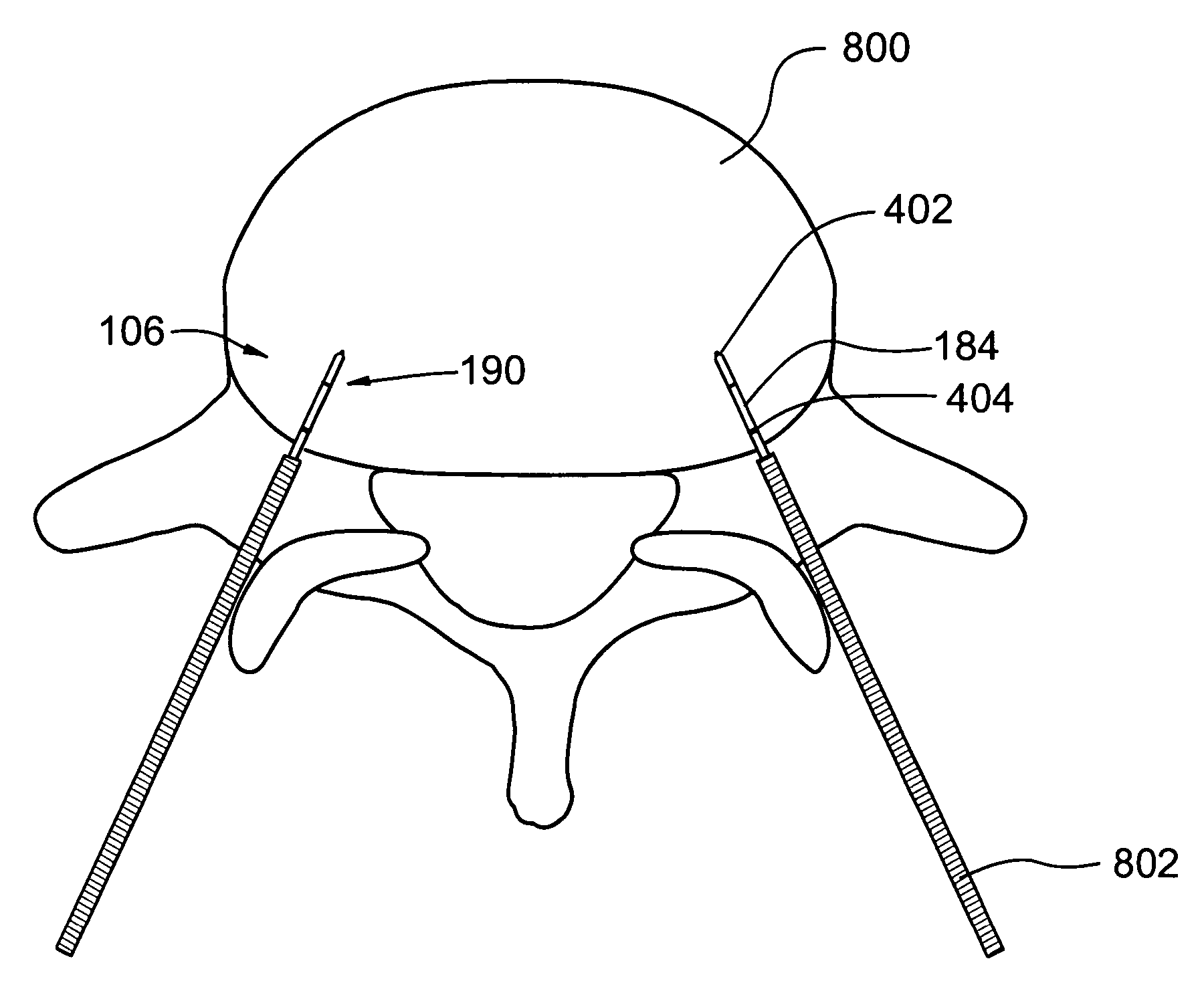
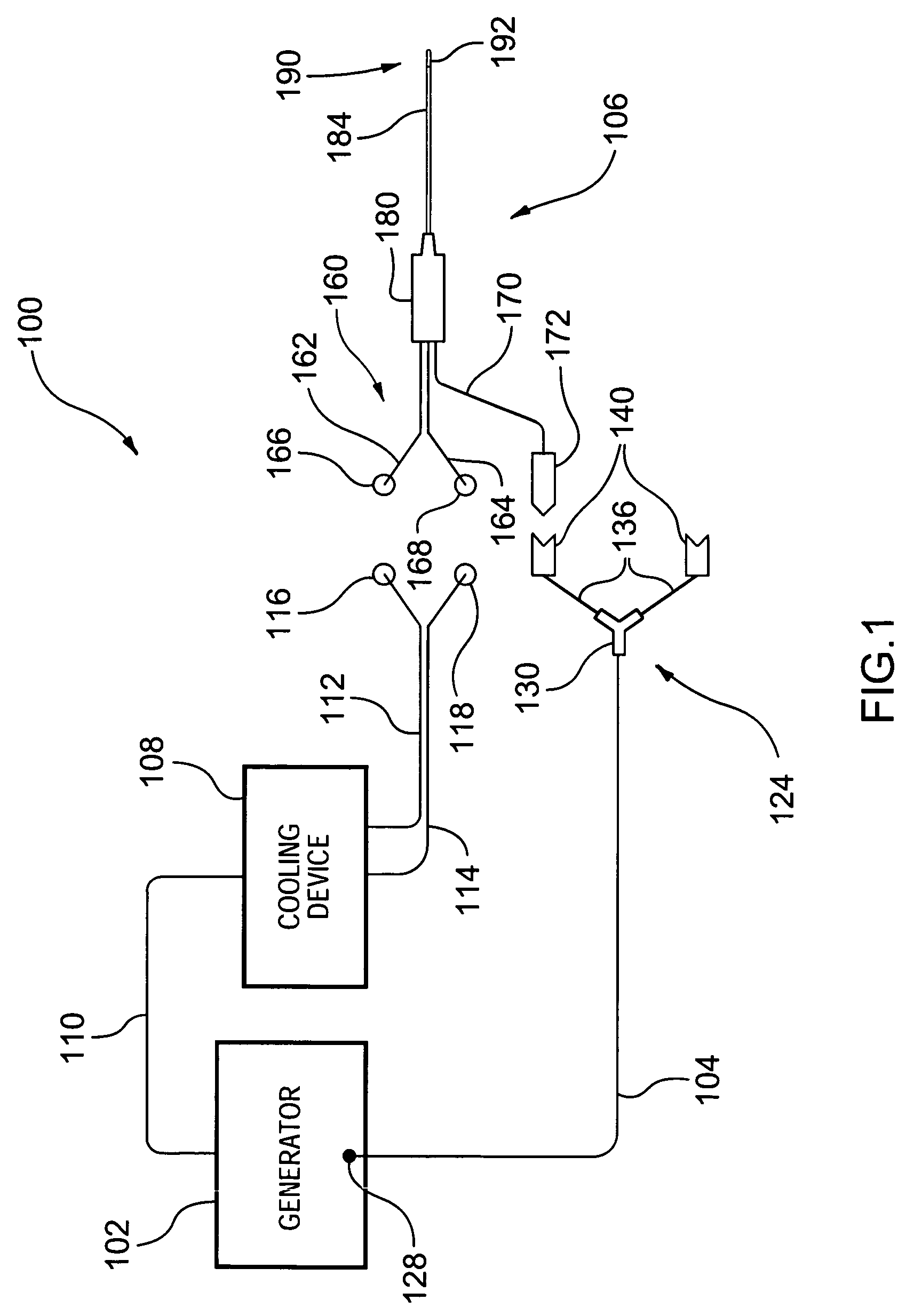
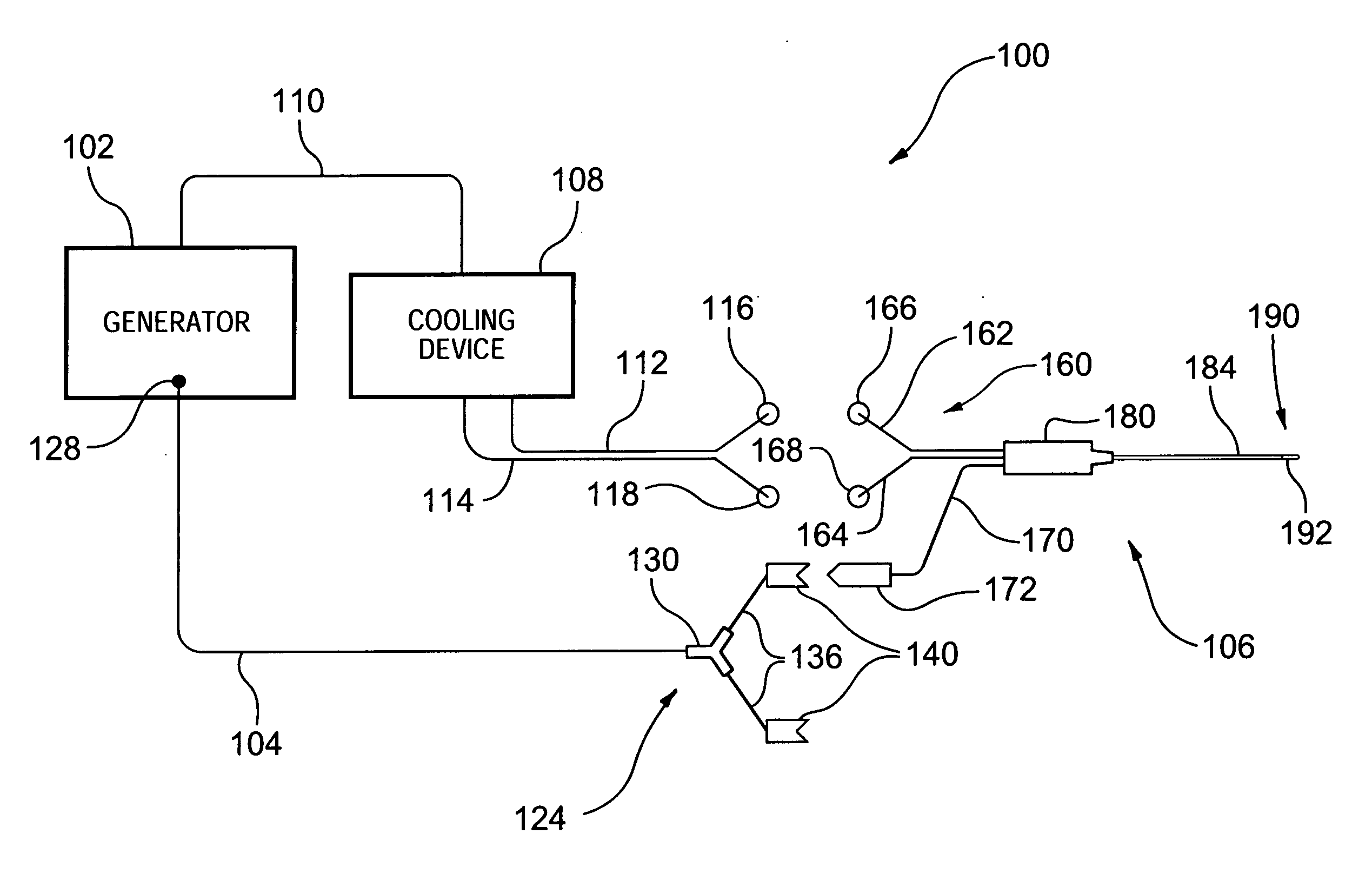
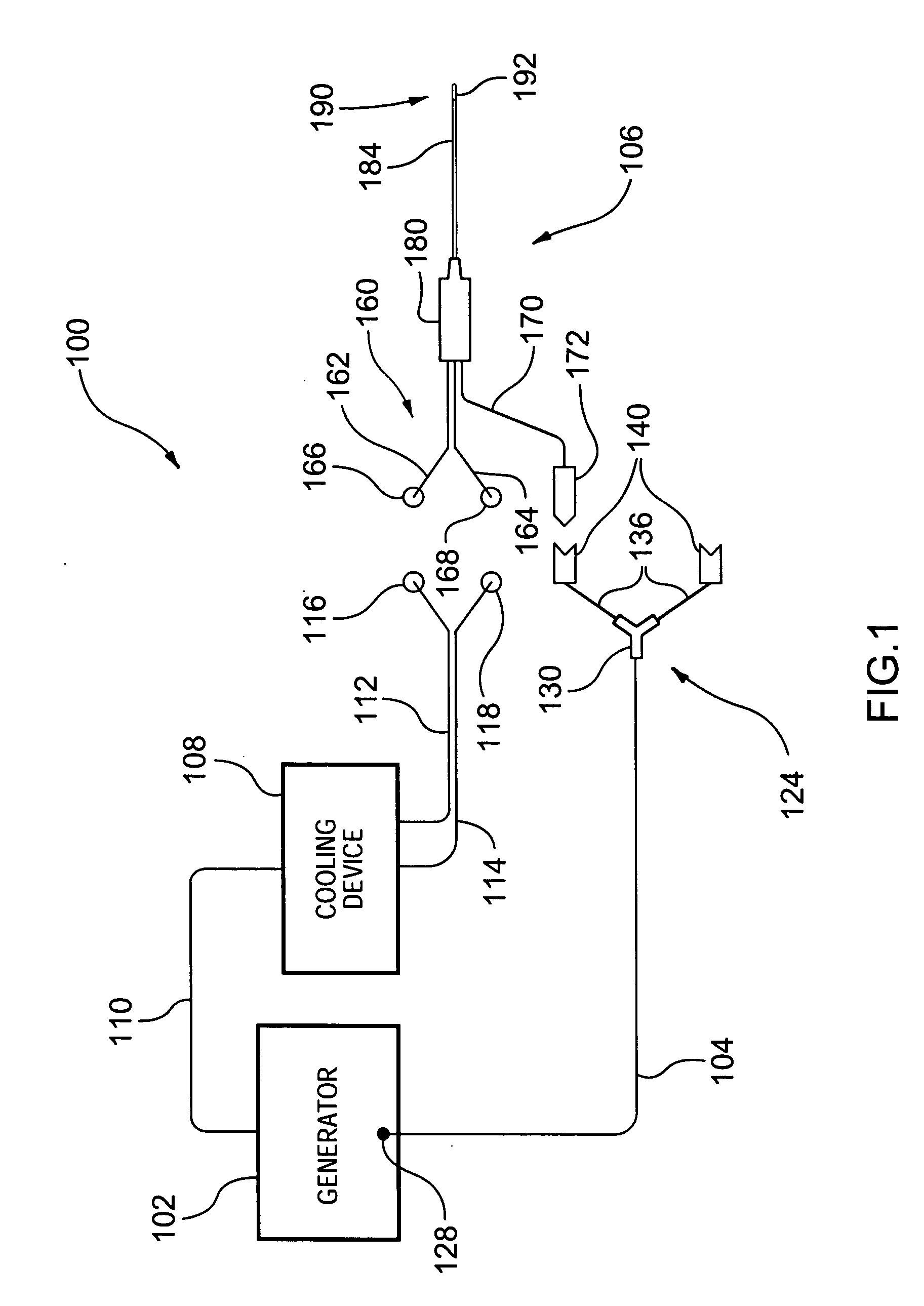
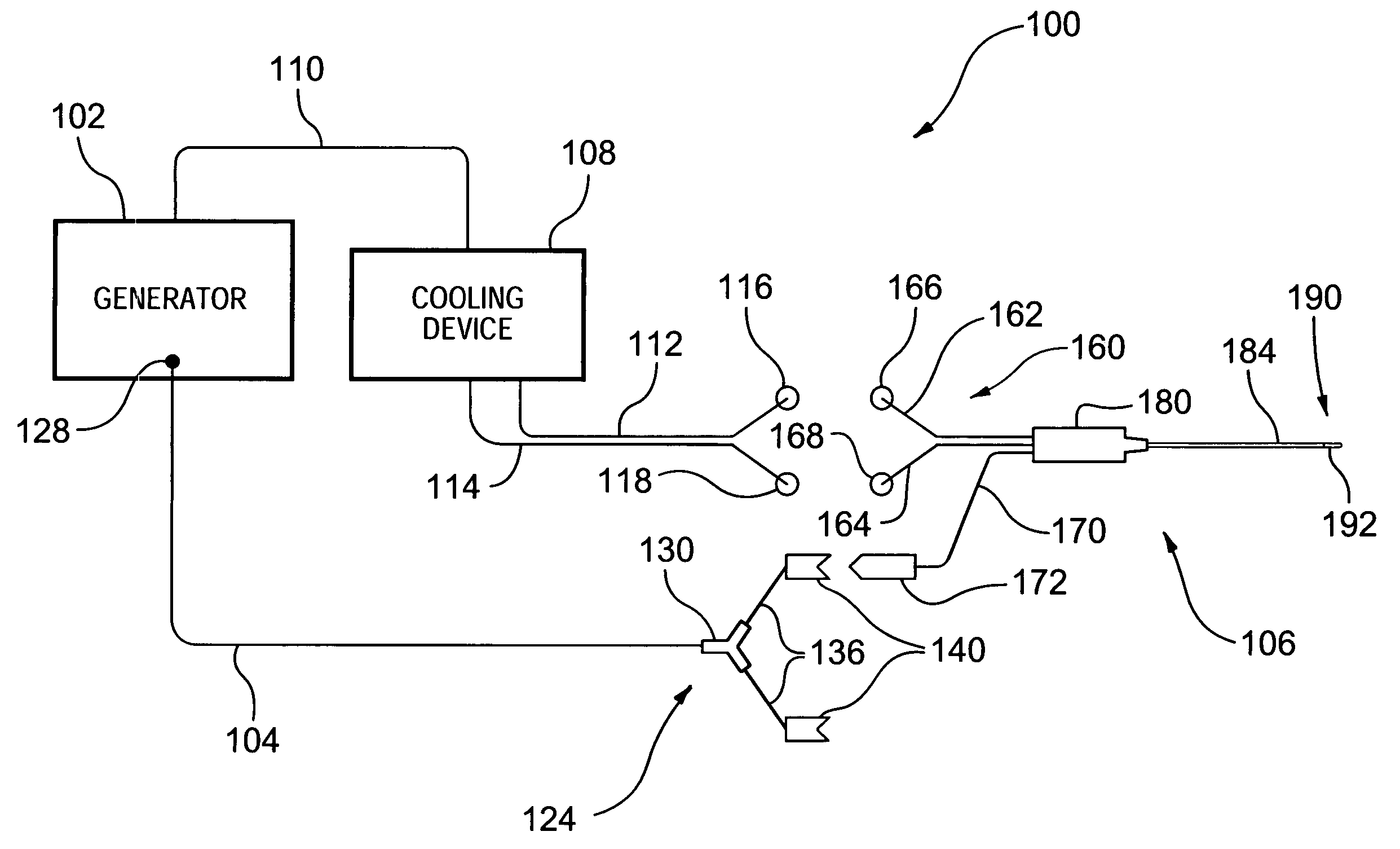
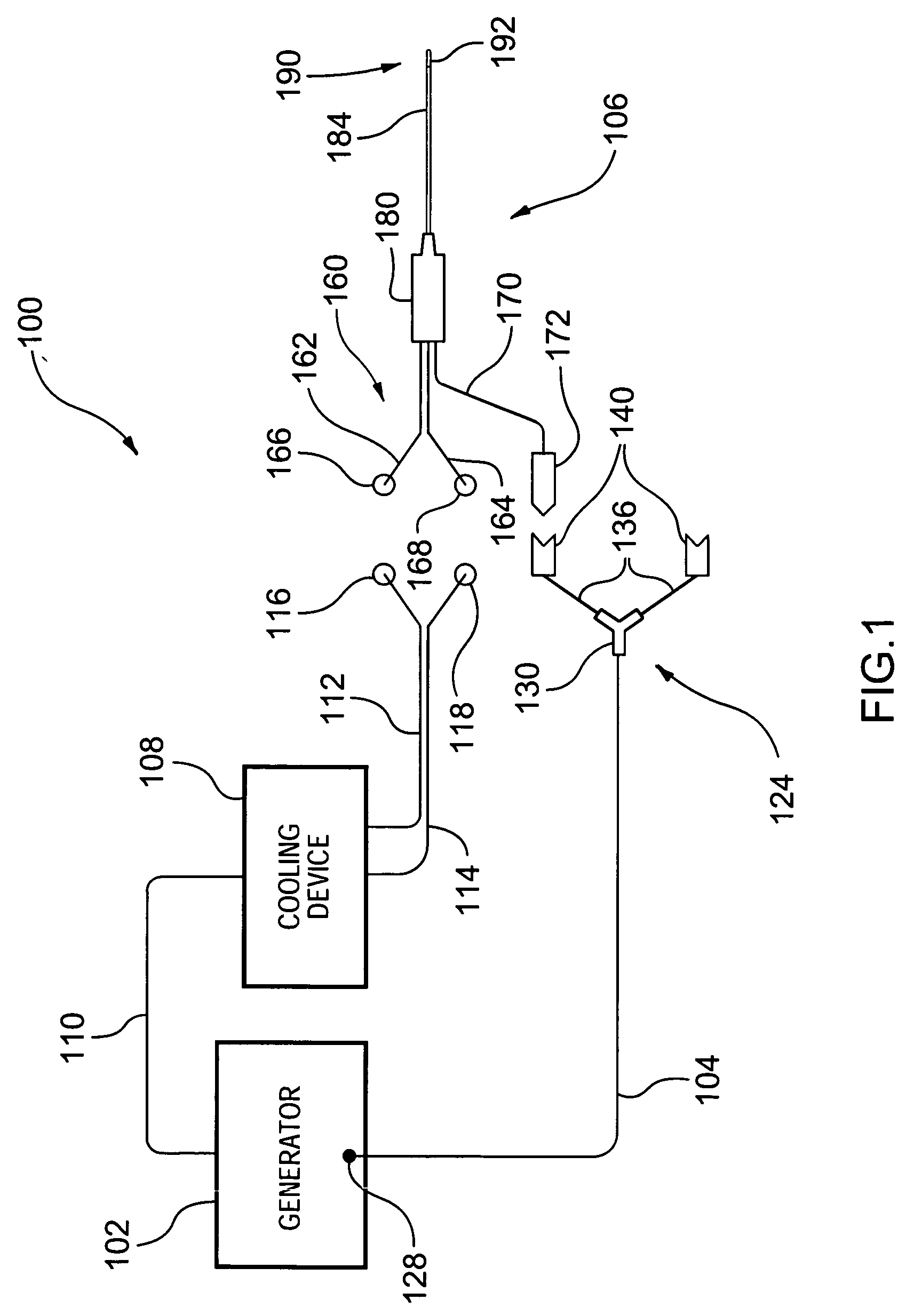
Electrosurgical tissue treatment method
A medical probe assembly, system, and methods for the use thereof to treat tissue are described. The system optionally comprises an energy source, two internally-cooled probe assemblies, and one or more cooling devices to provide cooling to at least one of the probe assemblies. The probe assemblies may be configured in a bipolar mode, whereby current flows preferentially between the probe assemblies. The probe assemblies and system described herein are particularly useful to deliver radio frequency energy to a patient's body. RF energy delivery may be used for various applications, including the treatment of pain, tumor ablation and cardiac ablation.
Owner:AVANOS MEDICAL SALES LLC
Thermal treatment methods and apparatus with focused energy application
InactiveUS7083614B2Minimize reflectionCollapse of structureUltrasonic/sonic/infrasonic diagnosticsUltrasound therapyMedicineAcoustic energy
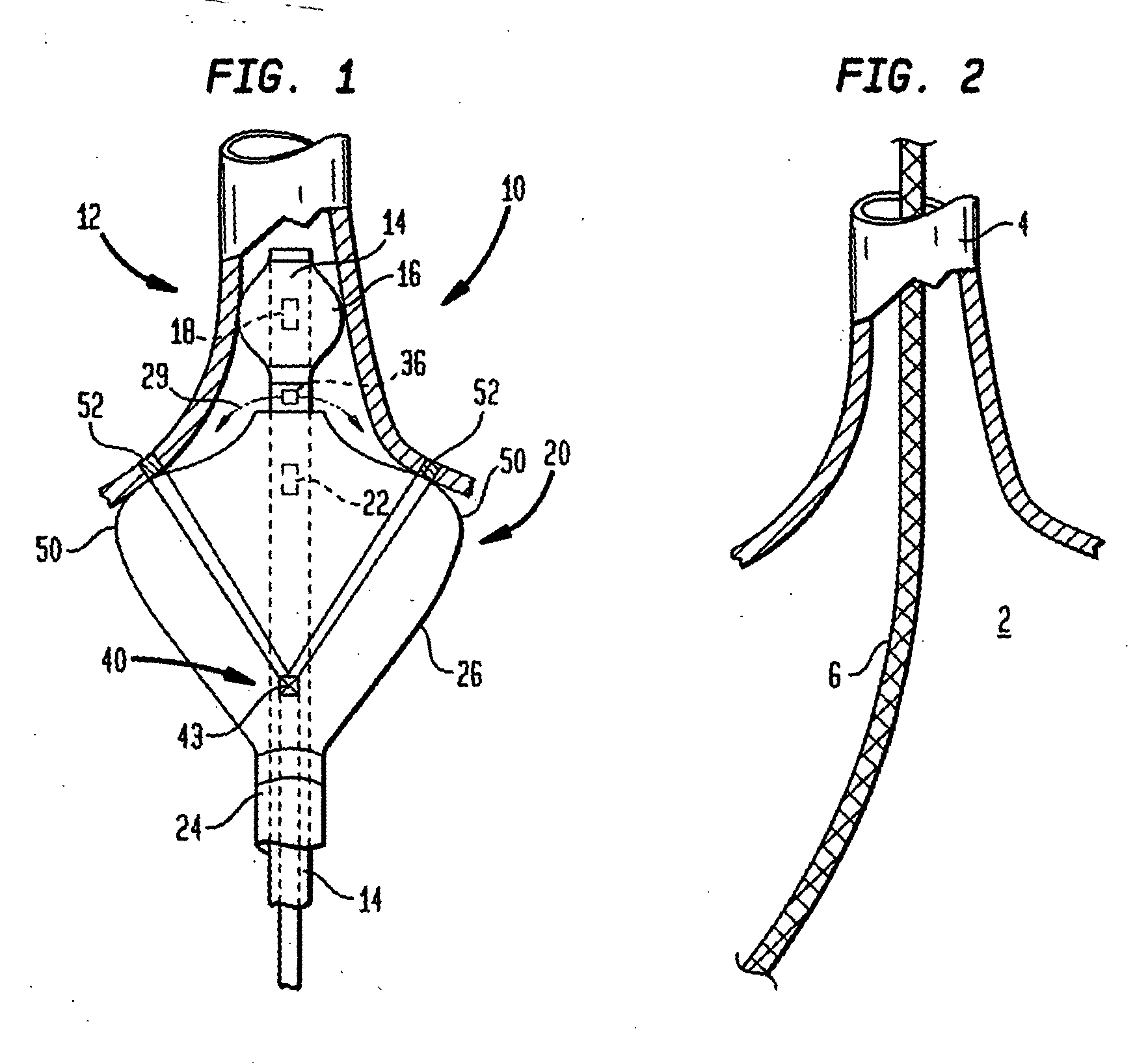
A collapsible ultrasonic reflector incorporates a gas-filled reflector balloon, a liquid-filled structural balloon an ultrasonic transducer disposed within the structural balloon. Acoustic energy emitted by the transducer is reflected by a highly reflective interface between the balloons. In a cardiac ablation procedure, the ultrasonic energy is focused into an annular focal region to ablate cardiac tissue extending in an annular path along the wall. Devices for stabilizing the balloon structure and for facilitating collapse and withdrawal of the balloon structure are also disclosed.
Owner:BOSTON SCI SCIMED INC +1
Guided cardiac ablation catheters
InactiveUS20050065504A1Improve energy transferEnhance the imageUltrasound therapyLaproscopesLight sourceCardiac Ablation
Owner:CARDIOFOCUS INC
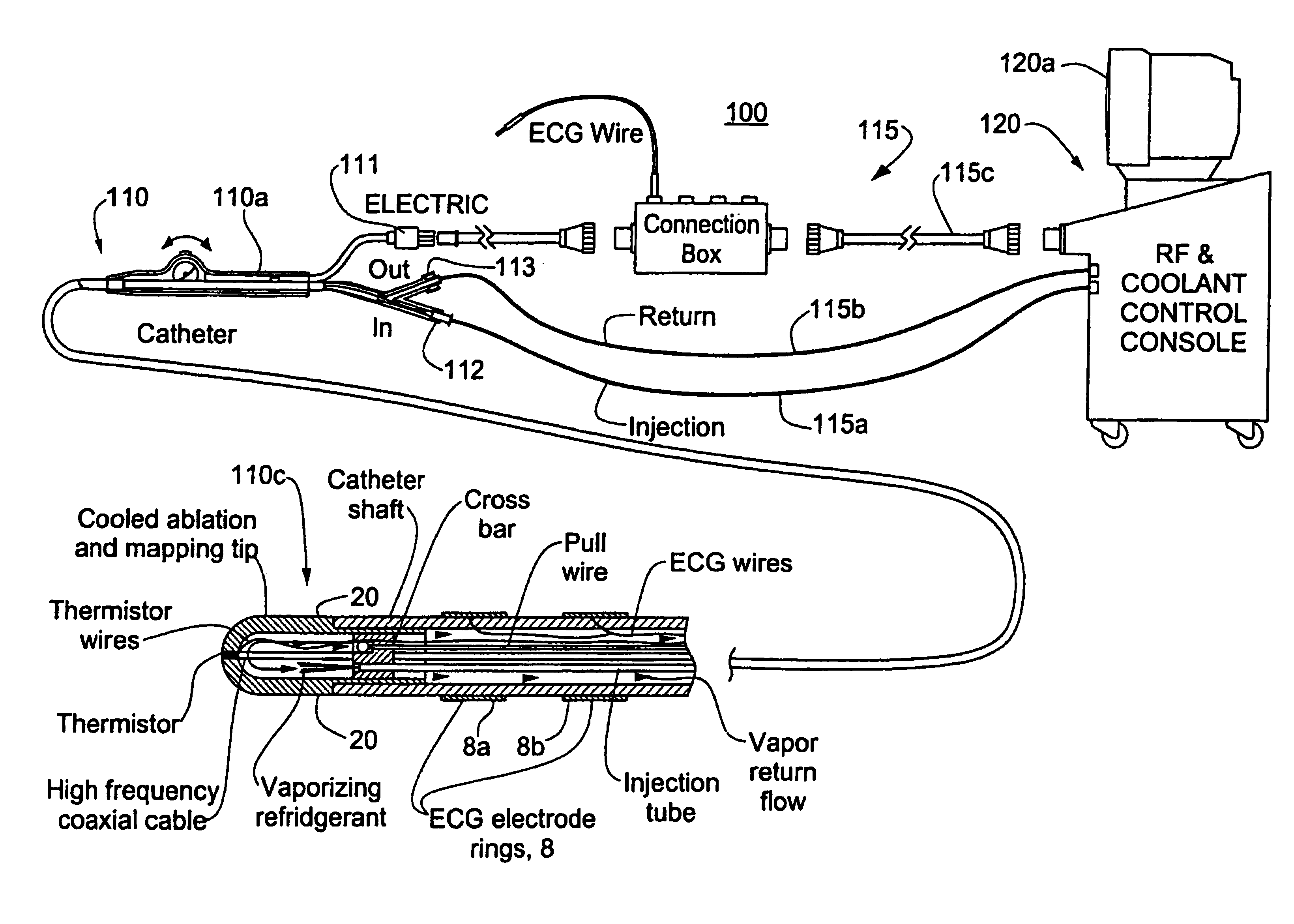
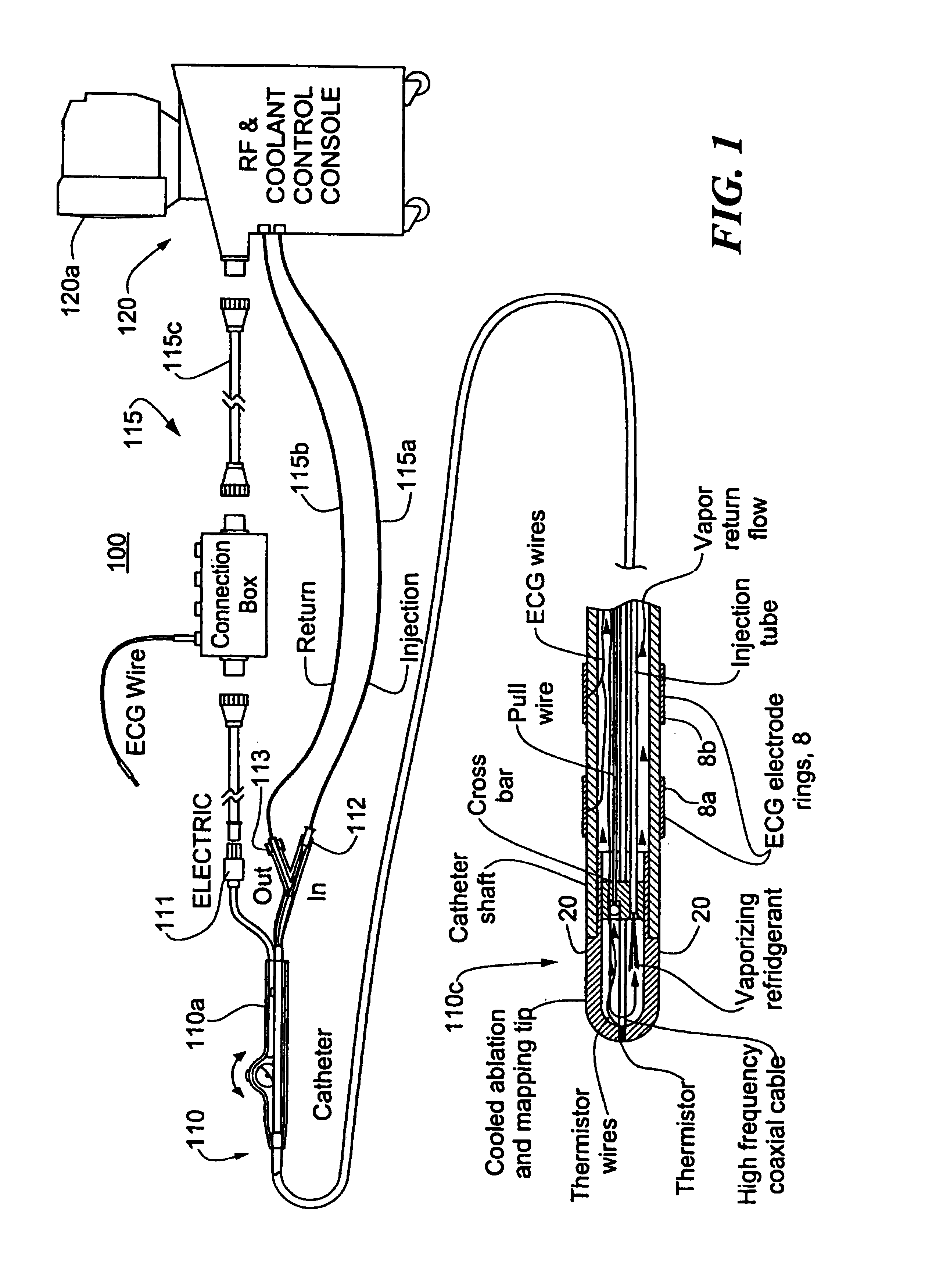
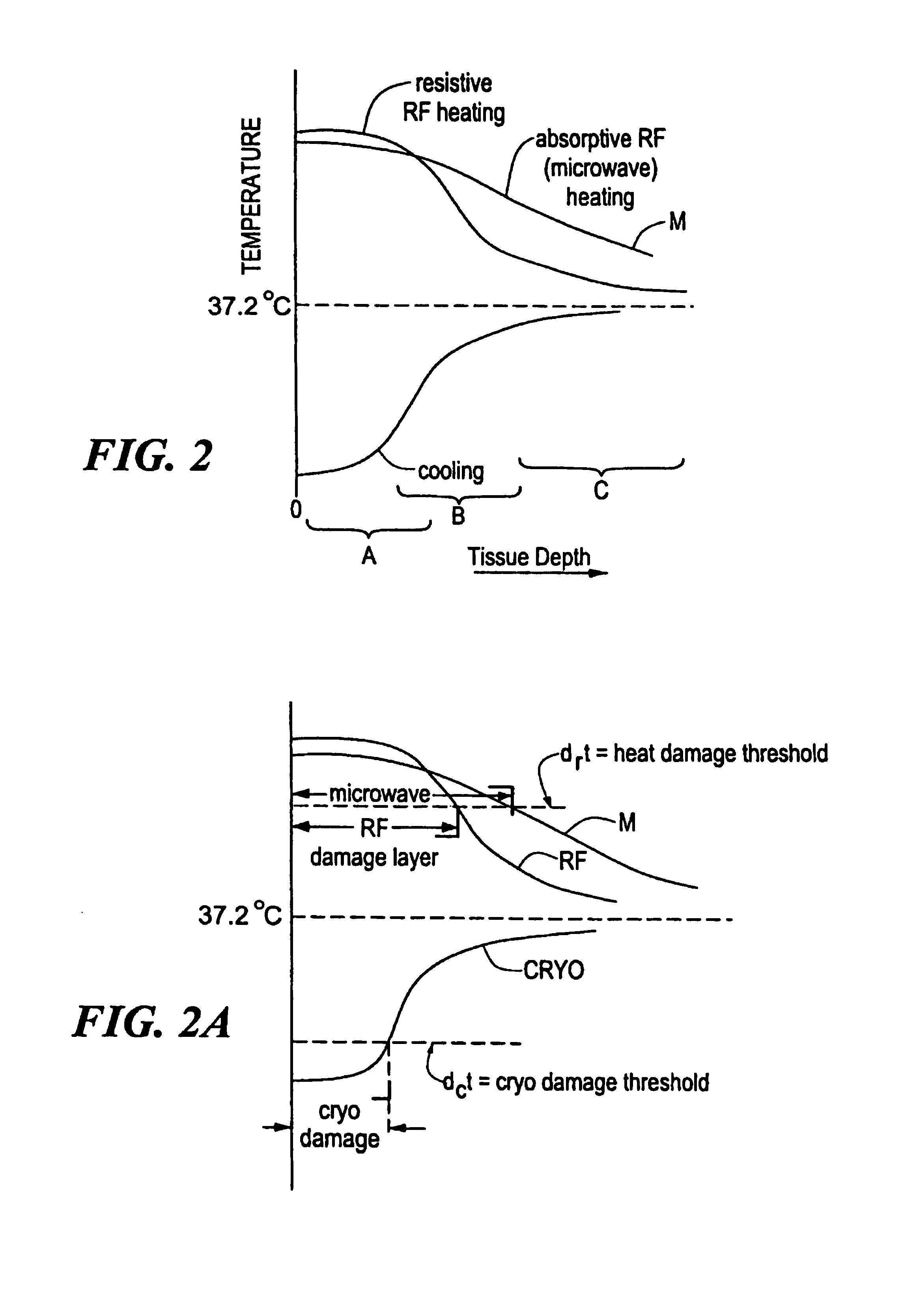
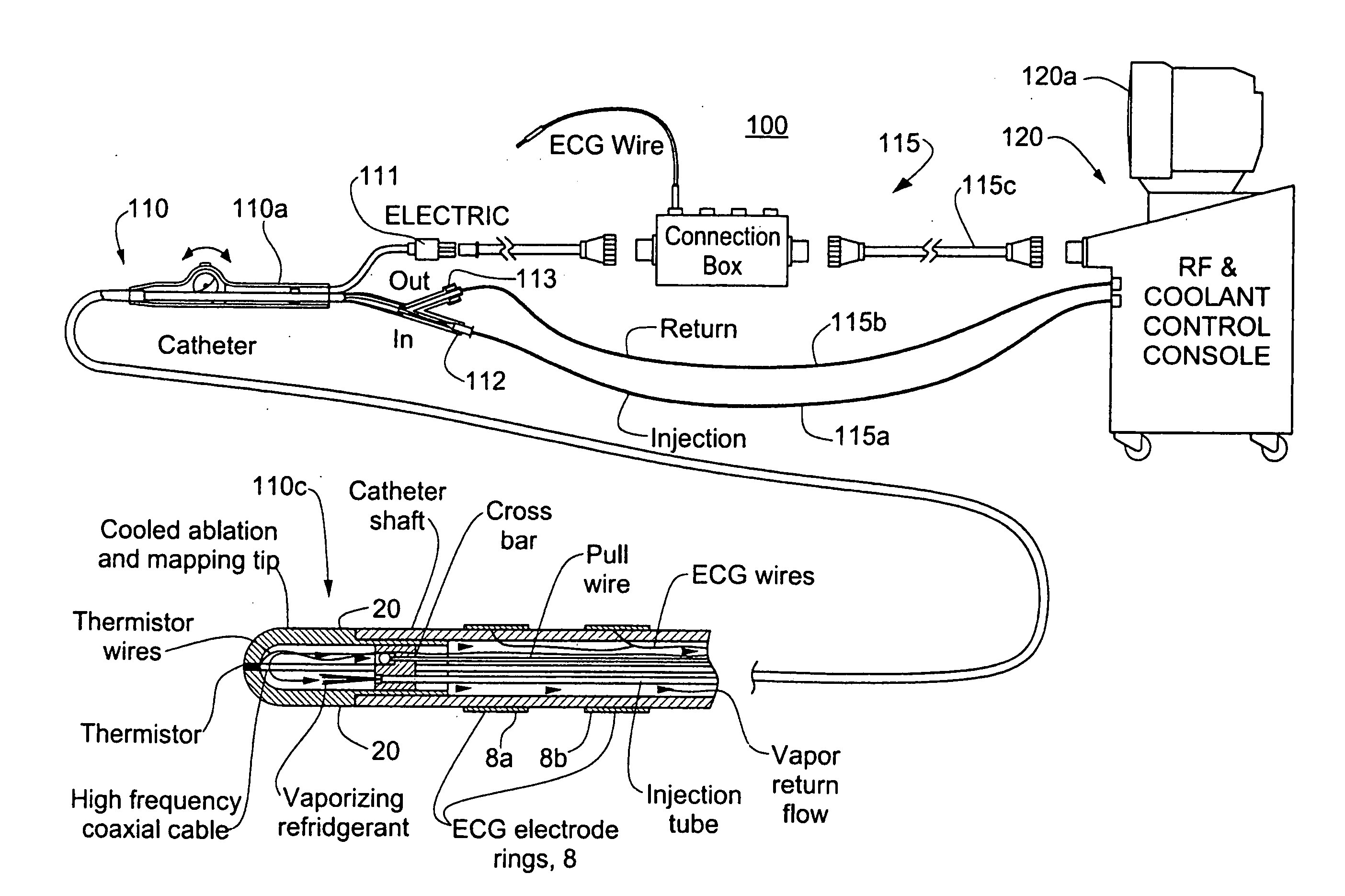
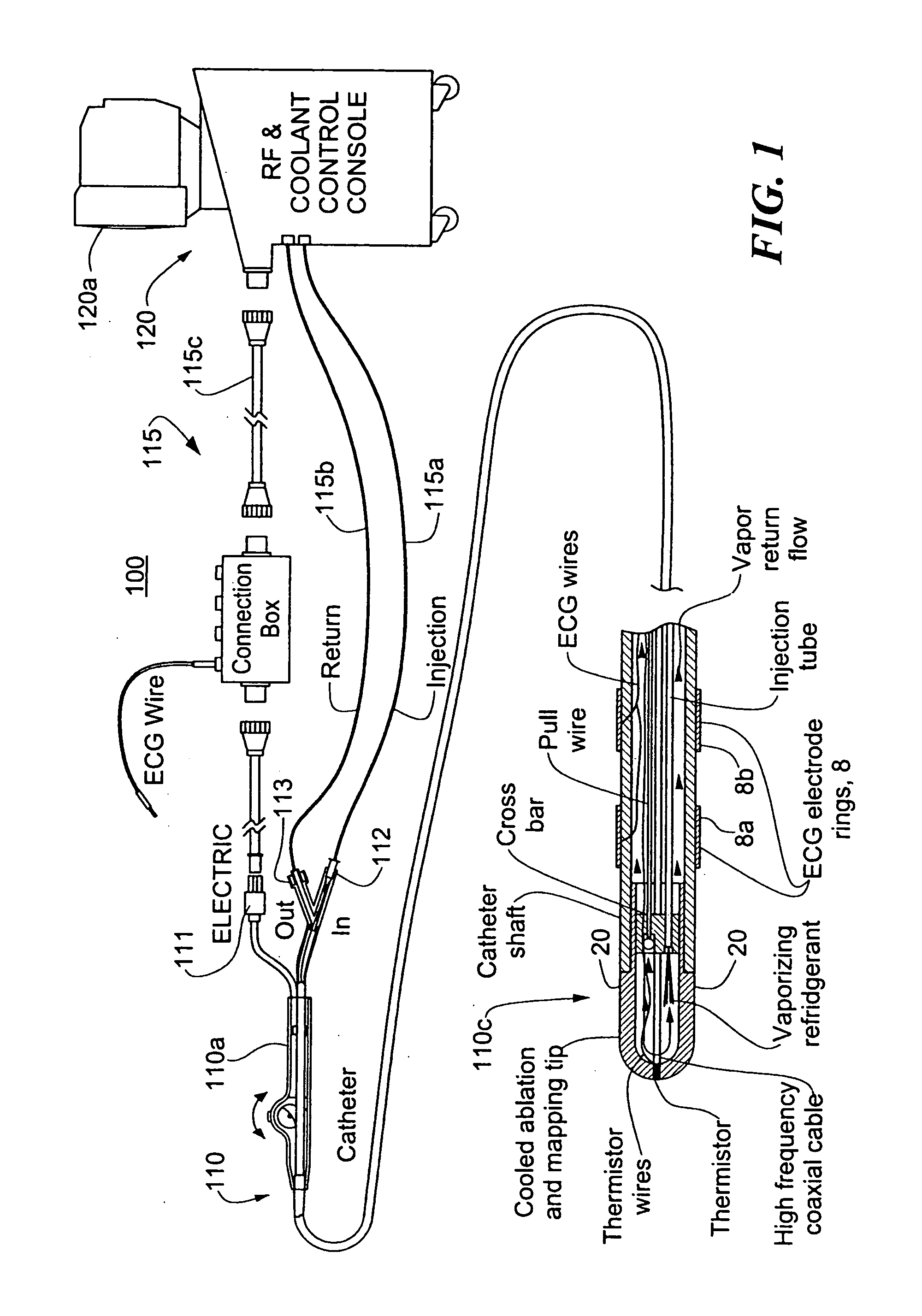
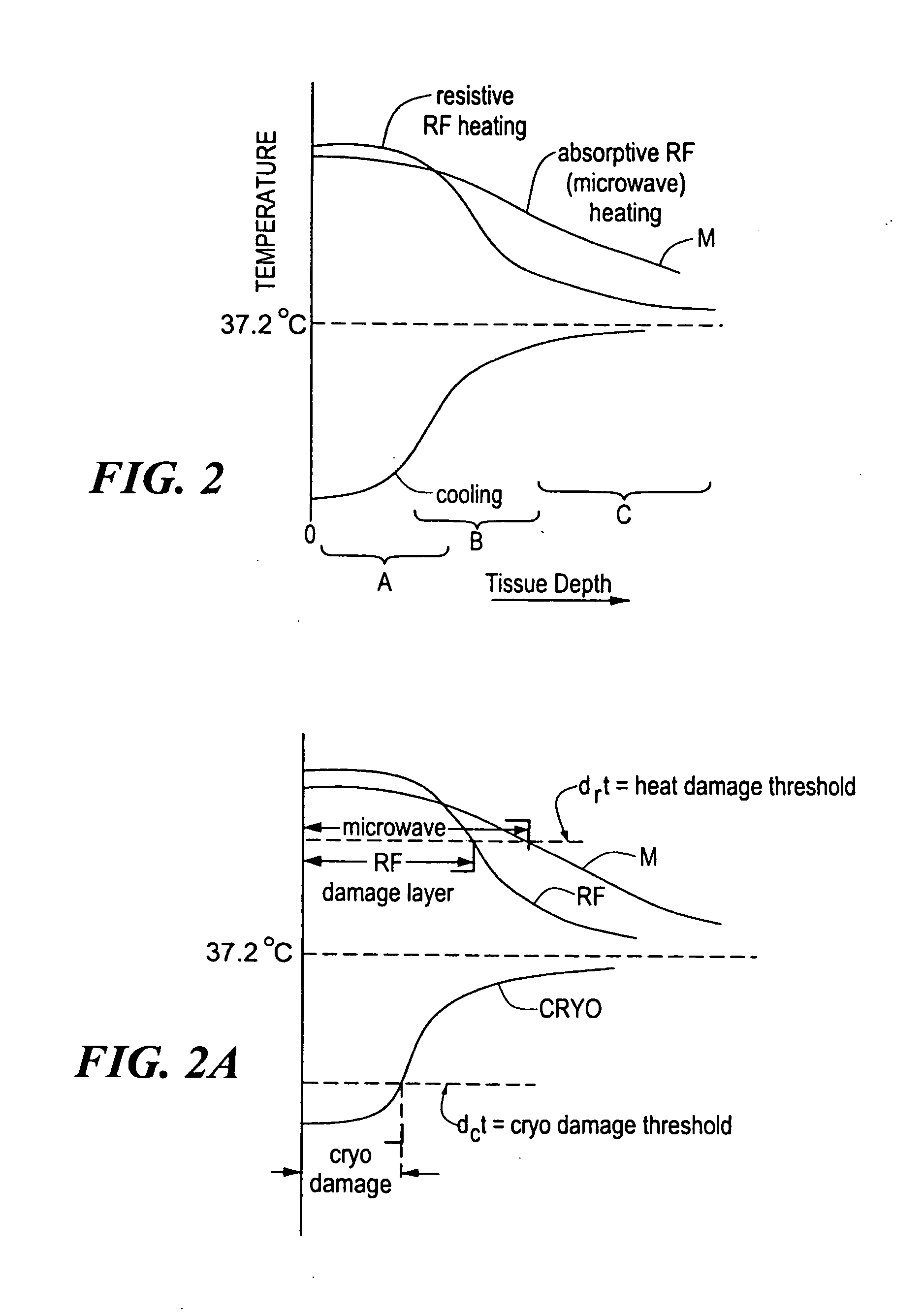
Catheter with cryogenic and heating ablation
InactiveUS7097641B1Improve versatilityEnhancing speed and placement lesionCatheterSurgical instruments for heatingTissue remodelingCelsius Degree
A catheter includes a cryoablation tip with an electrically-driven ablation assembly for heating tissue. The cryoablation tip may be implemented with a cooling chamber through which a controllably injected coolant circulates to lower the tip temperature, and having an RF electrode at its distal end. The RF electrode may be operated to warm cryogenically-cooled tissue, or the coolant may be controlled to conductively cool the tissue in coordination with an RF treatment regimen, allowing greater versatility of operation and enhancing the lesion size, speed or placement of multi-lesion treatment or single lesion re-treatment cycles. In one embodiment a microwave energy source operates at a frequency to extend beyond the thermal conduction depth, or to penetrate the cryogenic ice ball and be absorbed in tissue beyond an ice boundary, thus extending the depth and / or width of a single treatment locus. In another embodiment, the cooling and the application of RF energy are both controlled to position the ablation region away from the surface contacted by the electrode, for example to leave surface tissue unharmed while ablating at depth or to provide an ablation band of greater uniformity with increasing depth. The driver or RF energy source may supply microwave energy at a frequency effective to penetrate the ice ball which develops on a cryocatheter, and different frequencies may be selected for preferential absorption in a layer of defined thickness at depth in the nearby tissue. The catheter may operate between 70 and minus 70 degrees Celsius for different tissue applications, such as angioplasty, cardiac ablation and tissue remodeling, and may preset the temperature of the tip or adjacent tissue, and otherwise overlay or delay the two different profiles to tailor the shape or position where ablation occurs or to speed up a treatment cycle.
Owner:MEDTRONIC CRYOCATH LP
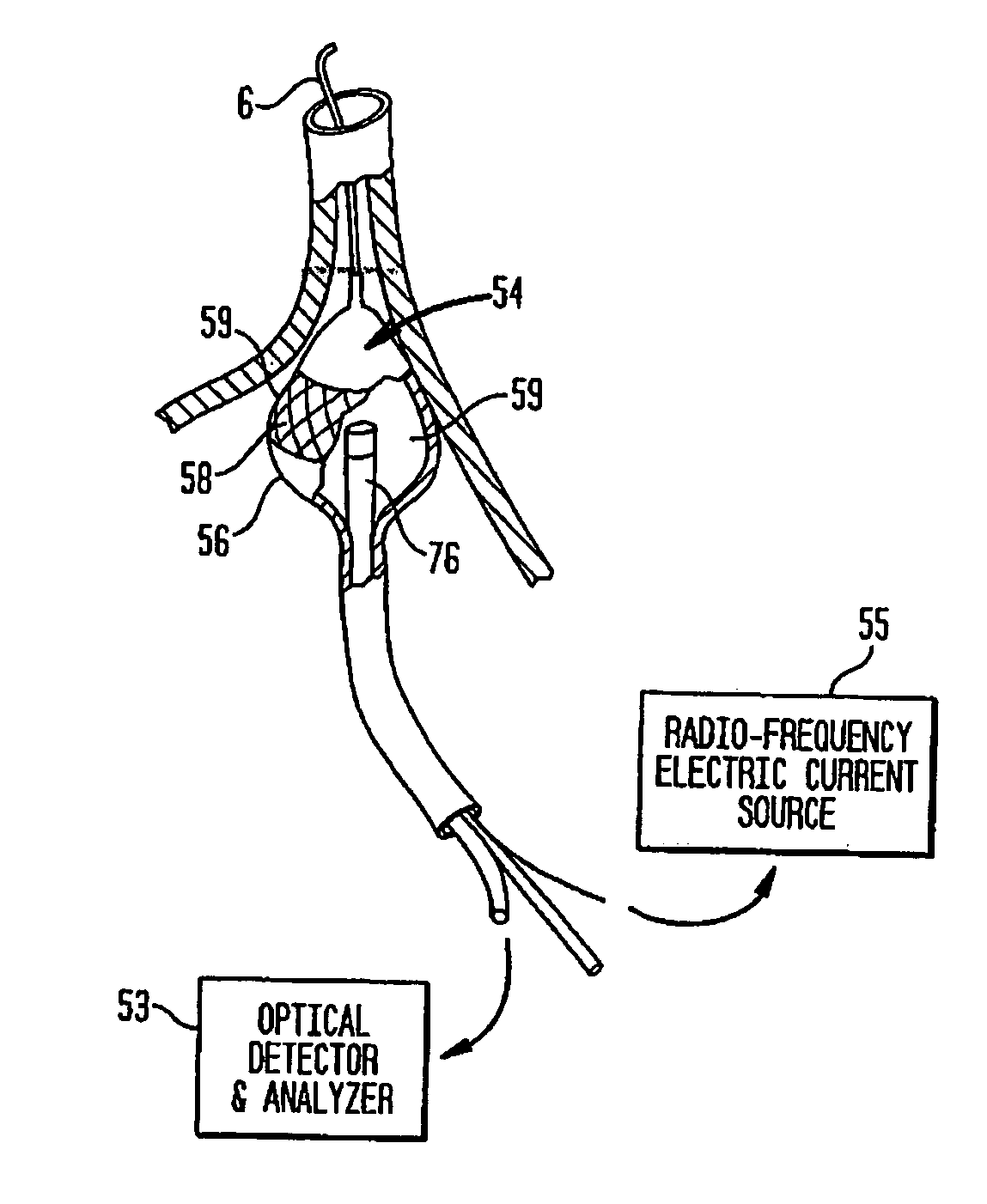
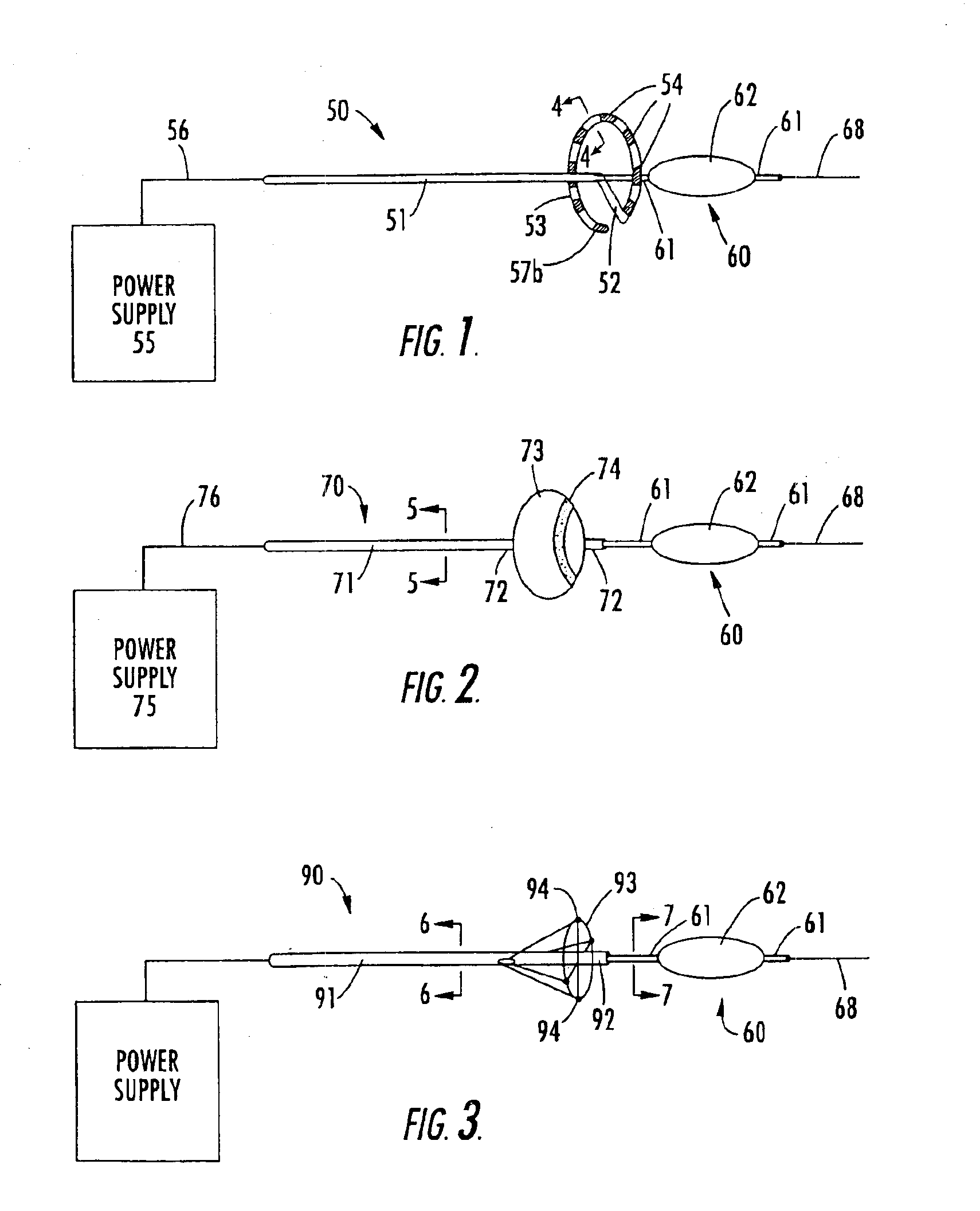
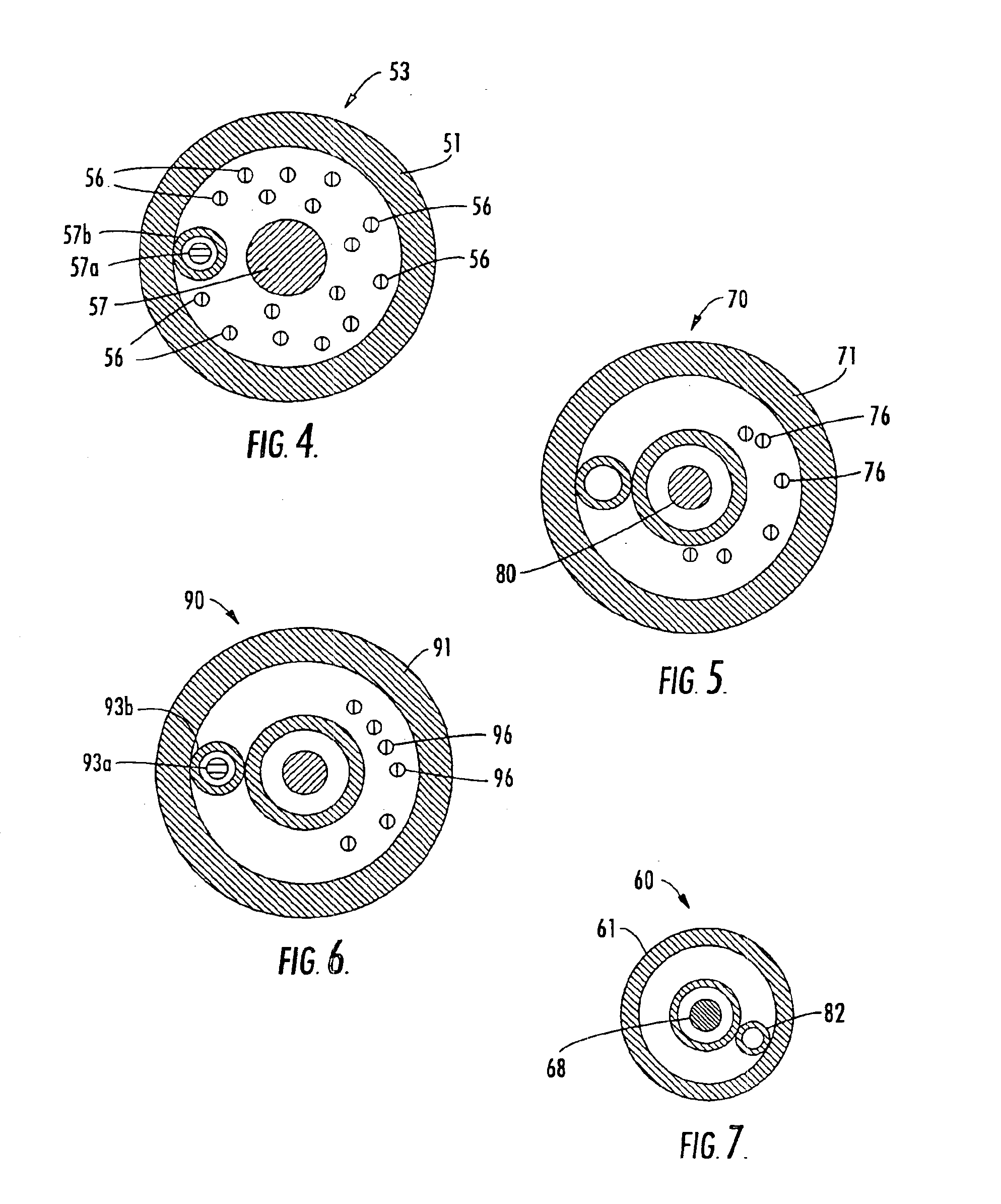
Coaxial catheter instruments for ablation with radiant energy
InactiveUS20050038419A9Rapid and effective photoablationLess timeStentsUltrasound therapyCoaxial catheterTarget tissue
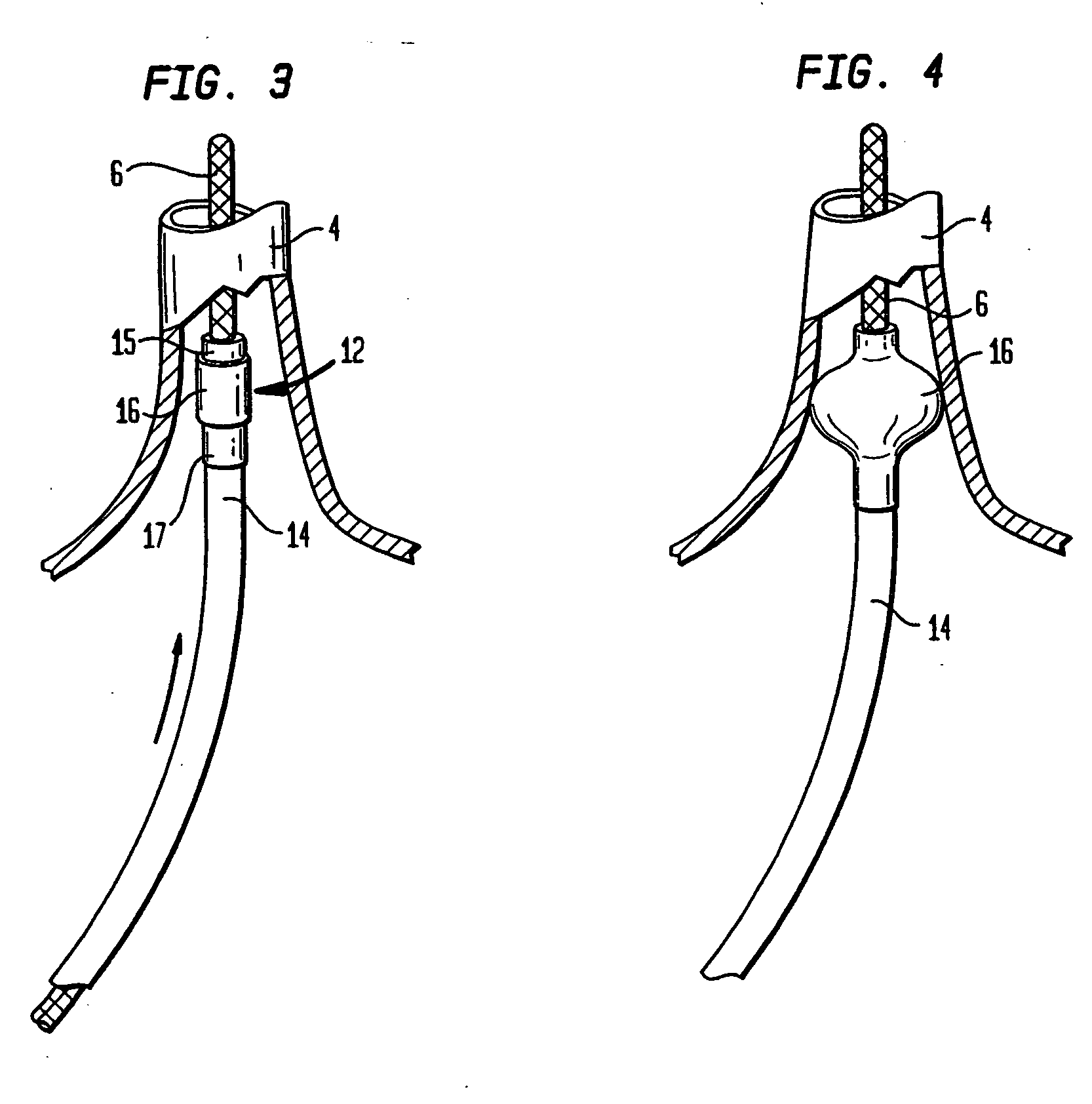
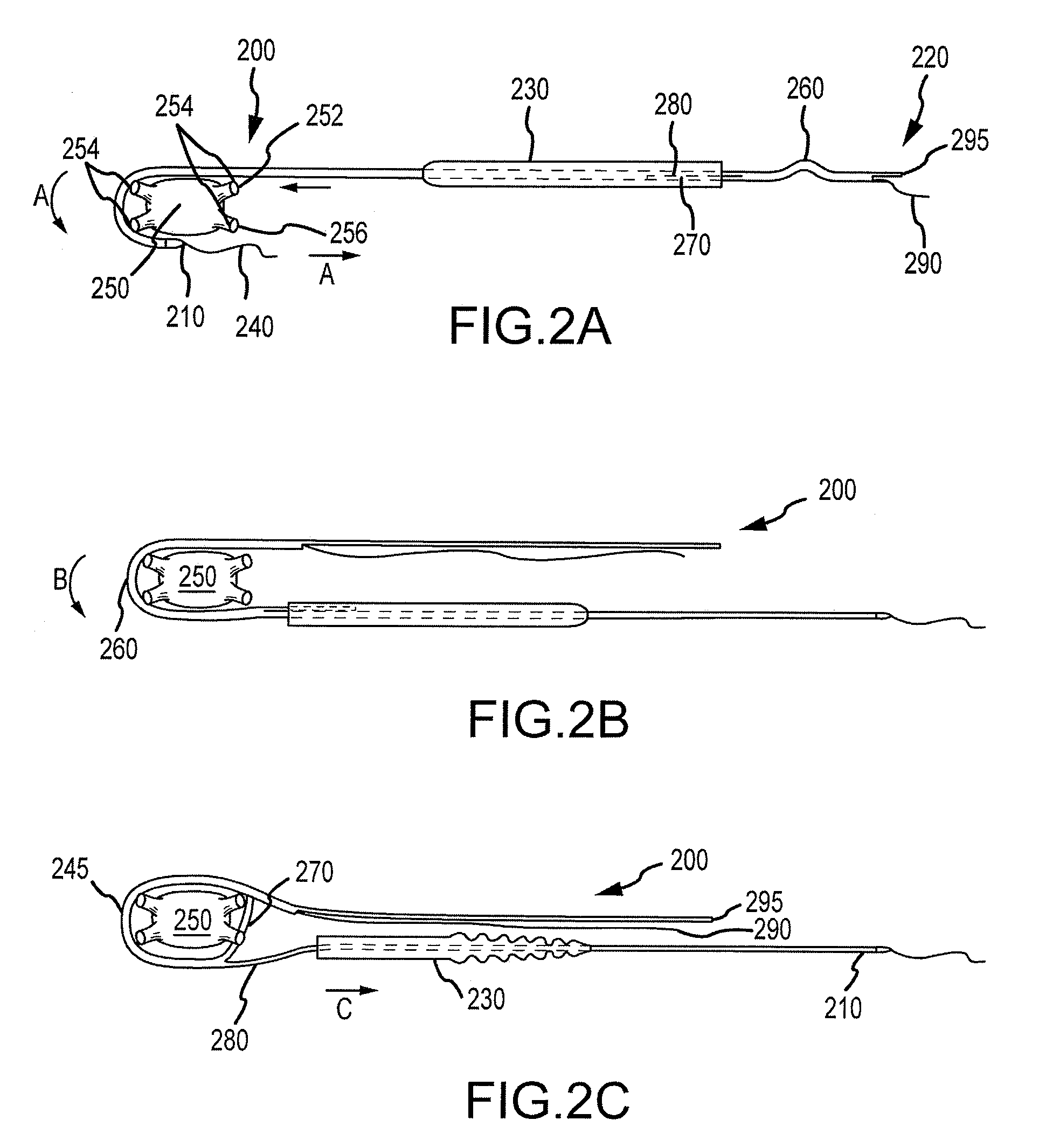
Ablation methods and instruments are disclosed for creating lesions in tissue, especially cardiac tissue for treatment of arrhythmias and the like. Percutaneous ablation instruments in the form of coaxial catheter bodies are disclosed having at least one central lumen therein and having one or more balloon structures at the distal end region of the instrument. The instruments include an energy emitting element which is independently positionable within the lumen of the instrument and adapted to project radiant energy through a transmissive region of a projection balloon to a target tissue site. The instrument can optionally include at least one expandable anchor balloon disposed about, or incorporated into an inner catheter body designed to be slid over a guidewire. This anchor balloon can serve to position the device within a lumen, such as a pulmonary vein. A projection balloon structure is also disclosed that can be slid over the first (anchor balloon) catheter body and inflated within the heart, to define a staging from which to project radiant energy. An ablative fluid can also be employed outside of the instrument (e.g., between the balloon and the target region) to ensure efficient transmission of the radiant energy when the instrument is deployed. In another aspect of the invention, generally applicable to a wide range of cardiac ablation instruments, mechanisms are disclosed for determining whether the instrument has been properly seated within the heart, e.g., whether the device is in contact with a pulmonary vein and / or the atrial surface, in order to form a lesion by heating, cooling or projecting energy. This contact-sensing feature can be implemented by an illumination source situated within the instrument and an optical detector that monitors the level of reflected light. Measurements of the reflected light (or wavelengths of the reflected light) can thus be used to determine whether contact has been achieved and whether such contact is continuous over a desired ablation path.
Owner:CARDIOFOCUS INC
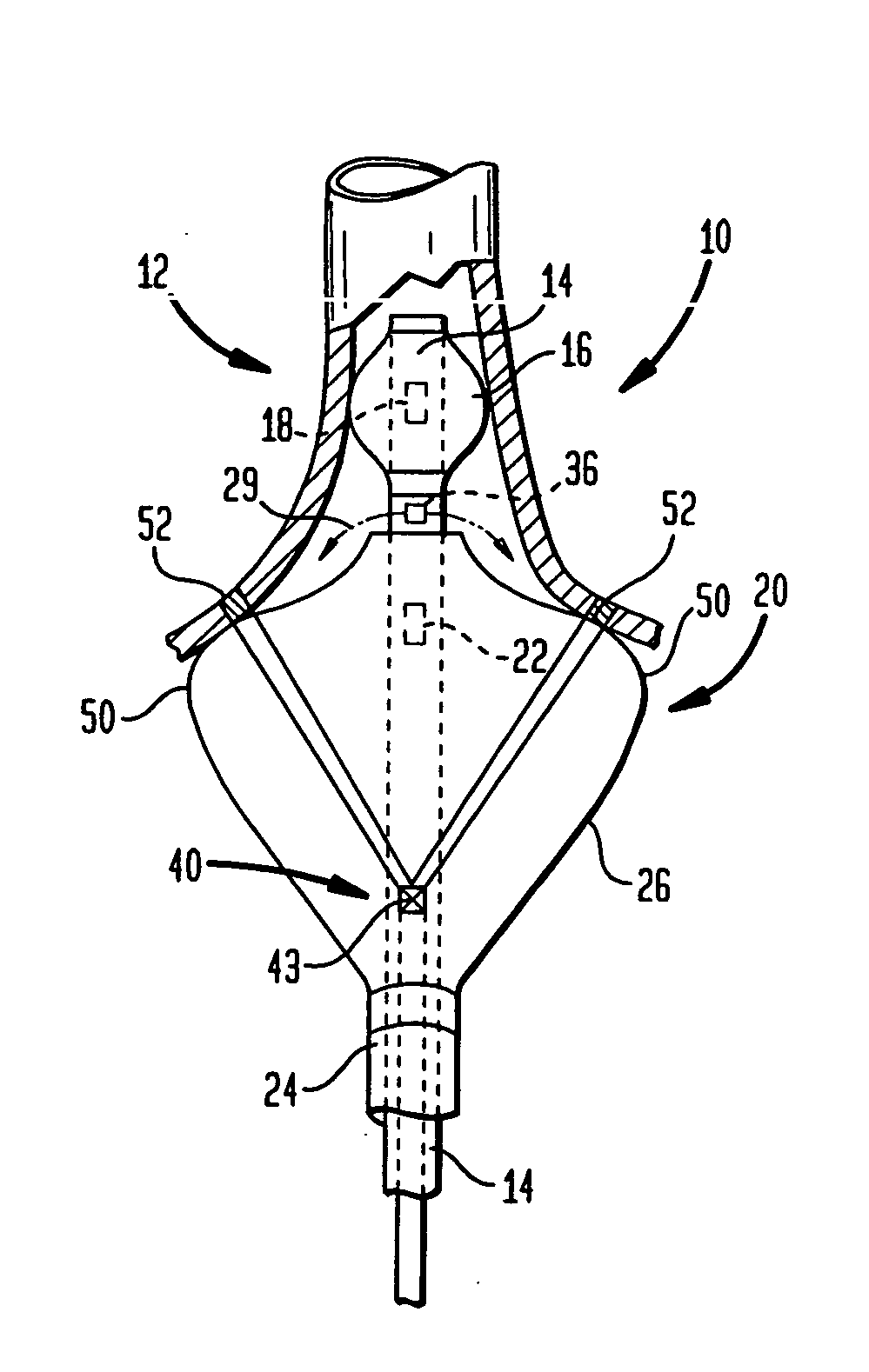
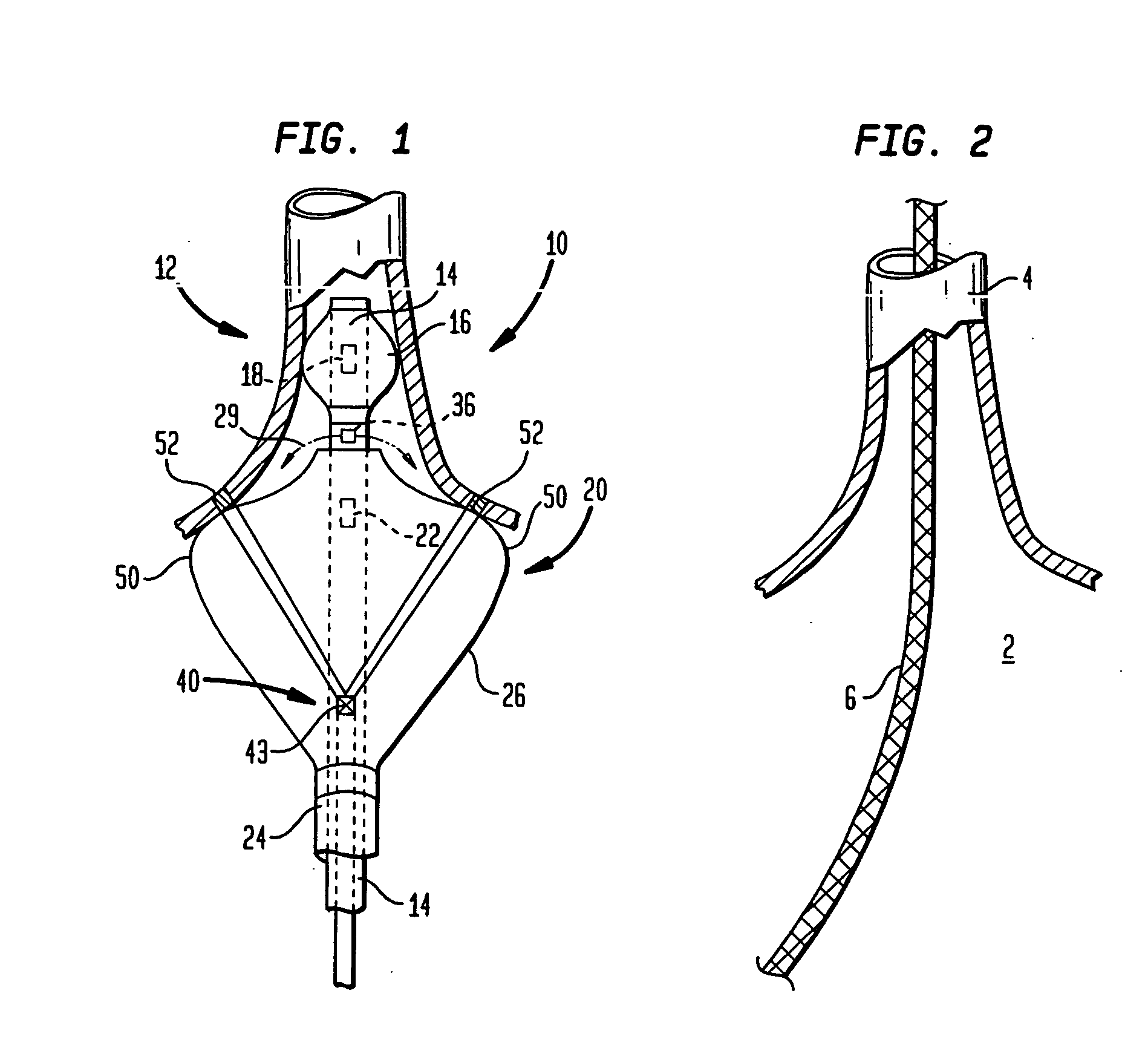
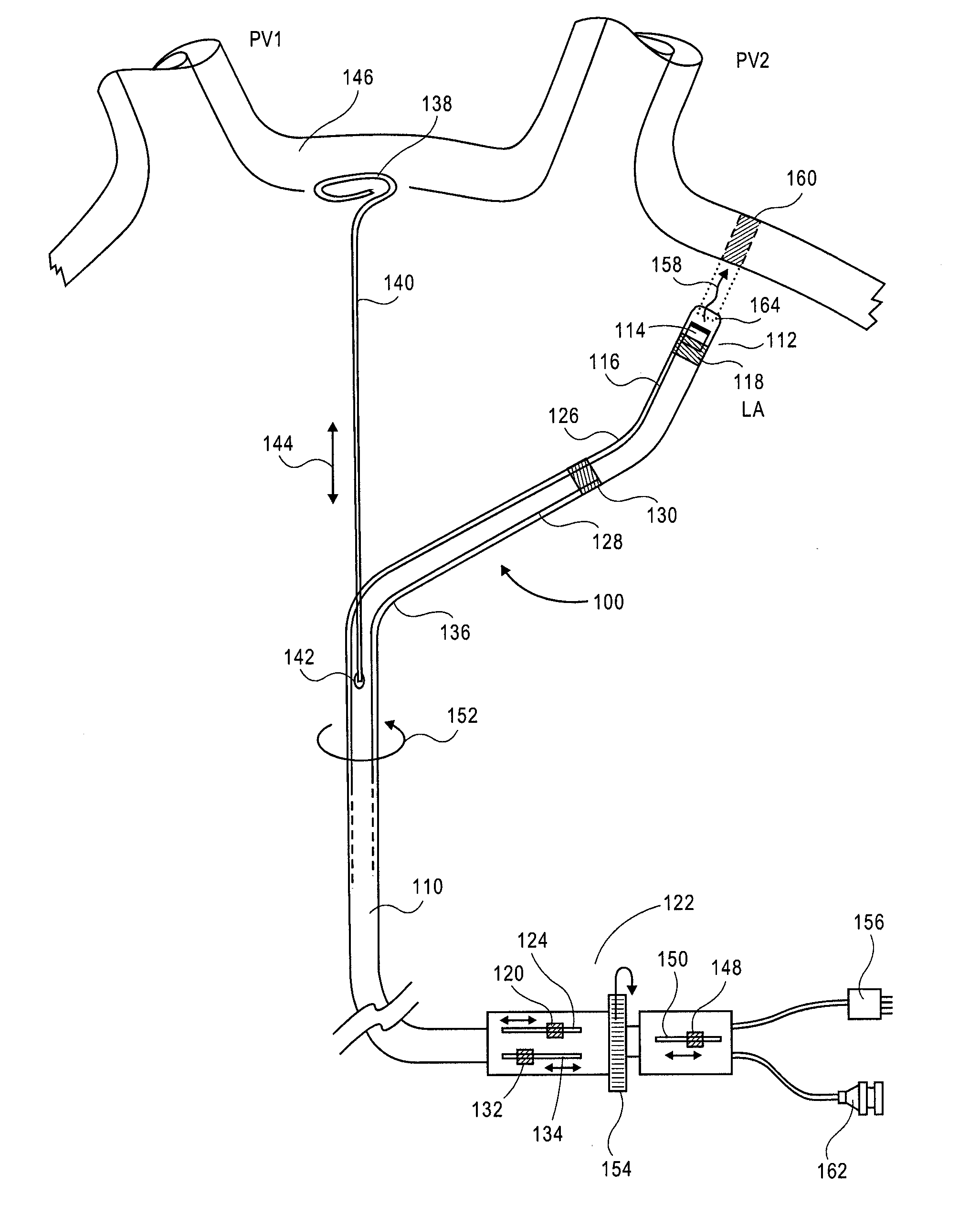
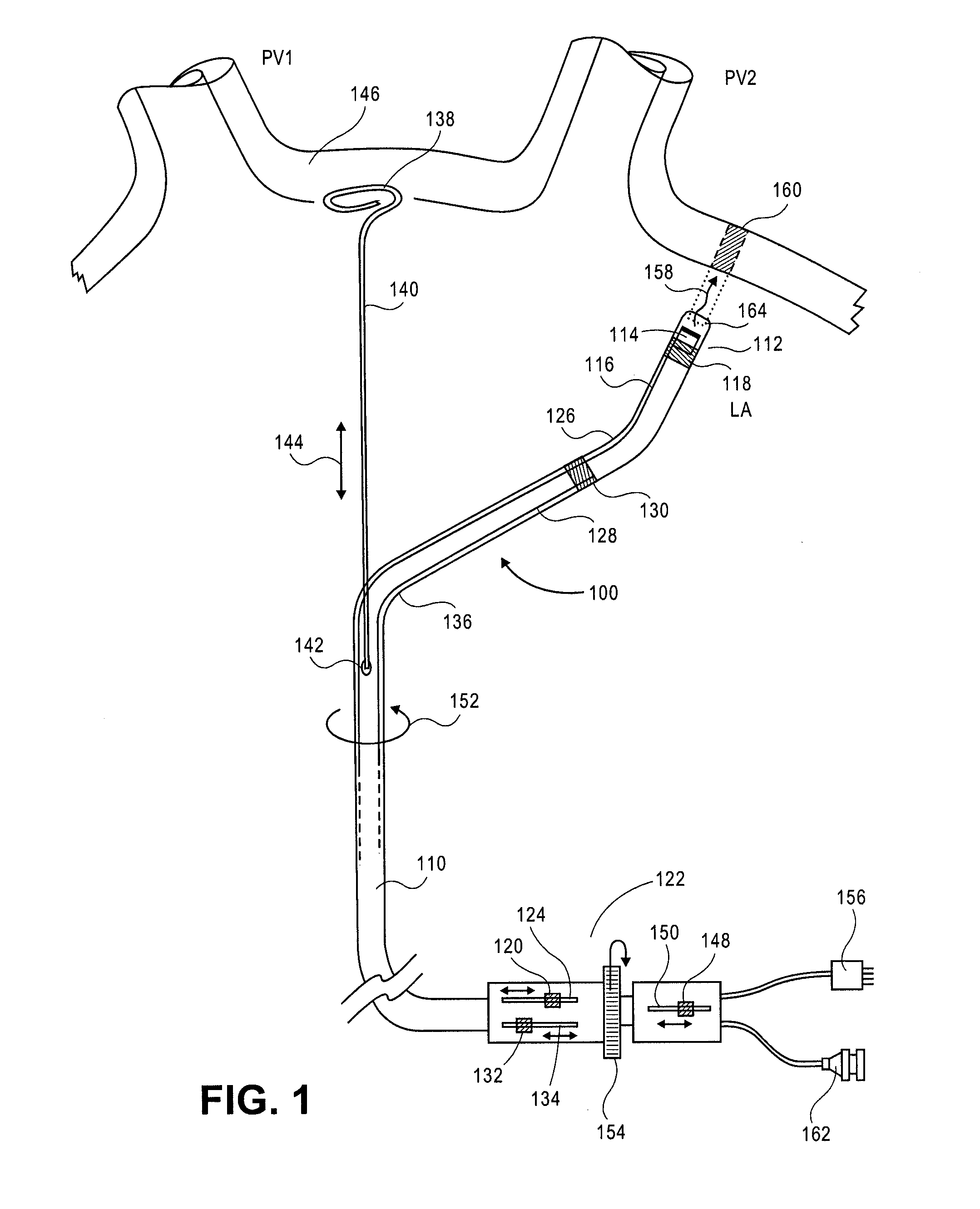
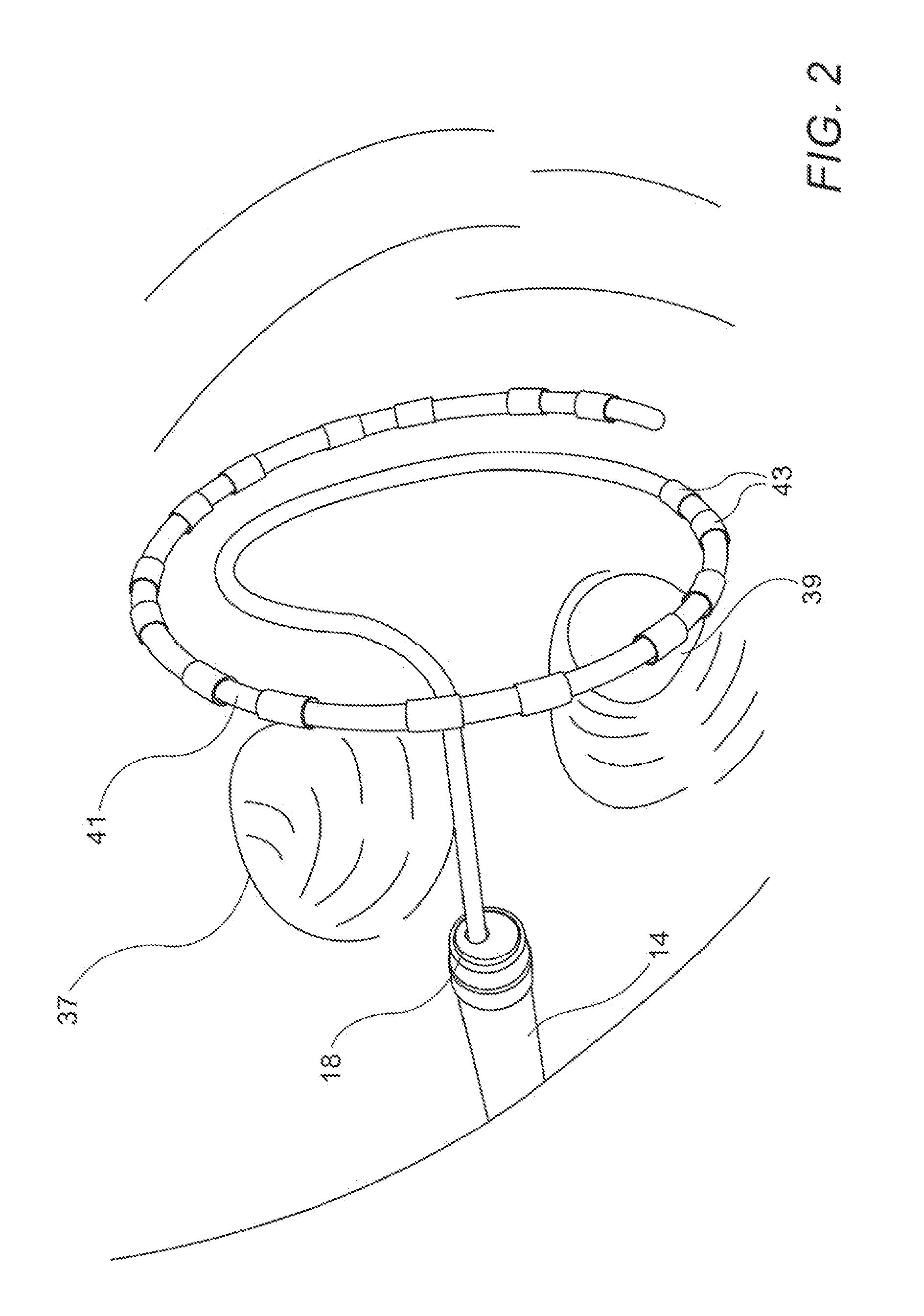
Ablation catheter, system, and method of use thereof
InactiveUS6893438B2Simple formatMechanically simpleElectrotherapySurgical instruments for heatingHeart chamberCardiac Ablation
A cardiac ablation apparatus for producing a circumferential ablation that electrically isolates a heart chamber wall portion from vessel such as a pulmonary vein extending into said wall portion comprises (a) an elongate centering catheter having a distal end portion; (b) an expandable centering element connected to said centering catheter distal end portion and configured for positioning within said vessel when in a retracted configuration, and for securing said elongate centering catheter in a substantially axially aligned position with respect to said vessel when said centering element is in an expanded configuration; (c) an ablation catheter slidably connected to said centering catheter said ablation element having a distal end portion, and (d) an expandable ablation element connected to said ablation catheter distal end portion. The ablation element is configured to form a circumferential ablation on the wall around the elongate centering catheter when the centering catheter is axially aligned with respect to the vessel. In a further embodiment, a non-expandable, compliant centering element is employed, such as an elastic finger. Systems incorporating such an apparatus and methods of use thereof are also disclosed.
Owner:UAB RES FOUND
Device for Ablating Body Tissue
A cardiac ablation system including an ablation catheter having an anchor adapted to support the ablation catheter within an atrium of a heart and an ultrasound emitter disposed radially outward from a rotation axis and from the anchor, and a control mechanism adapted to rotate the ultrasound emitter about the rotation axis and to provide ablation energy to the ultrasound emitter to ablate heart tissue.
Owner:AURIS HEALTH INC
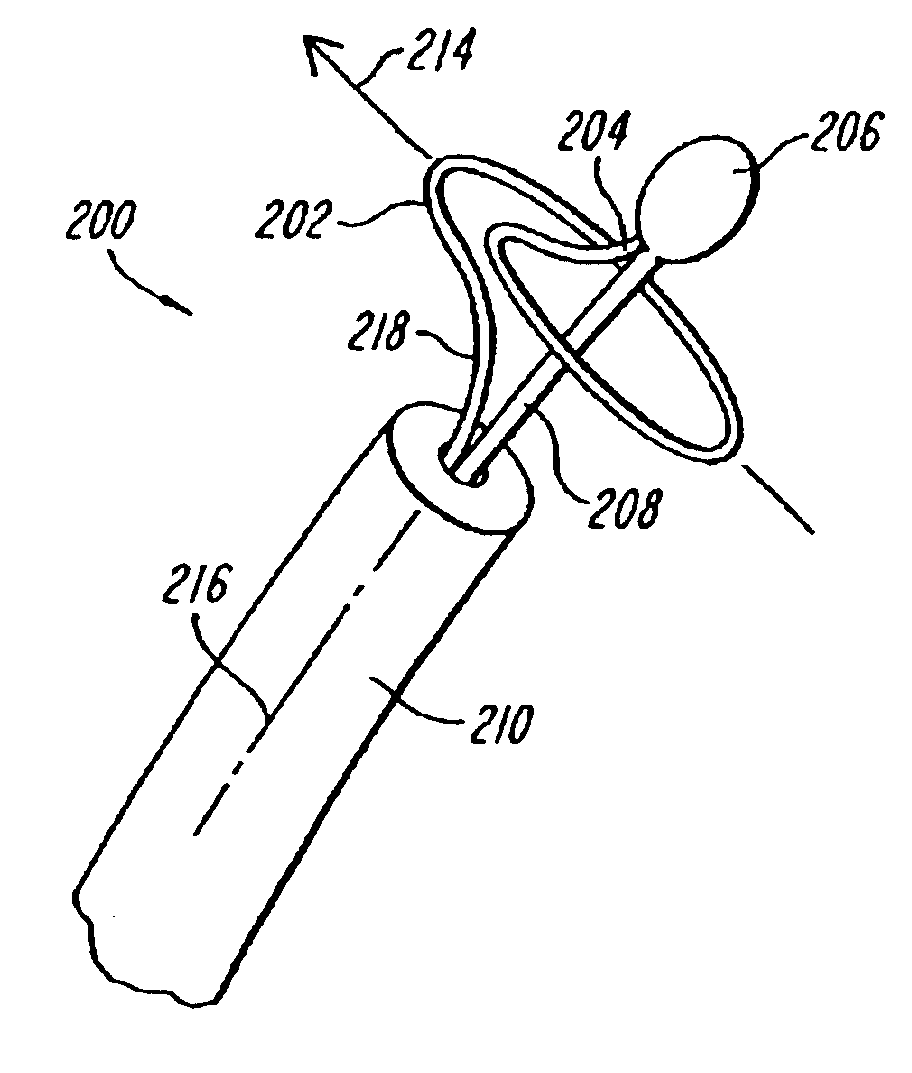
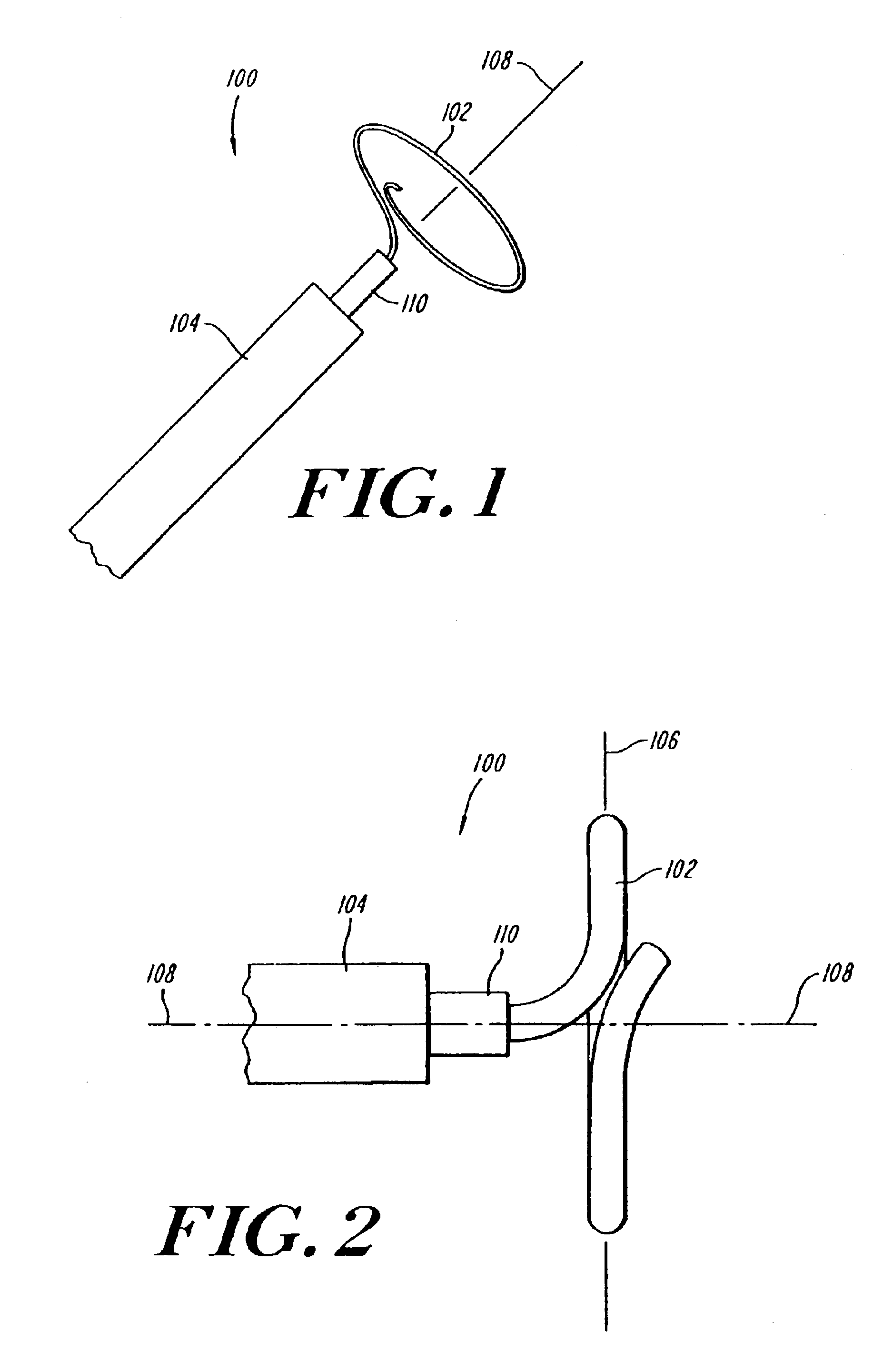
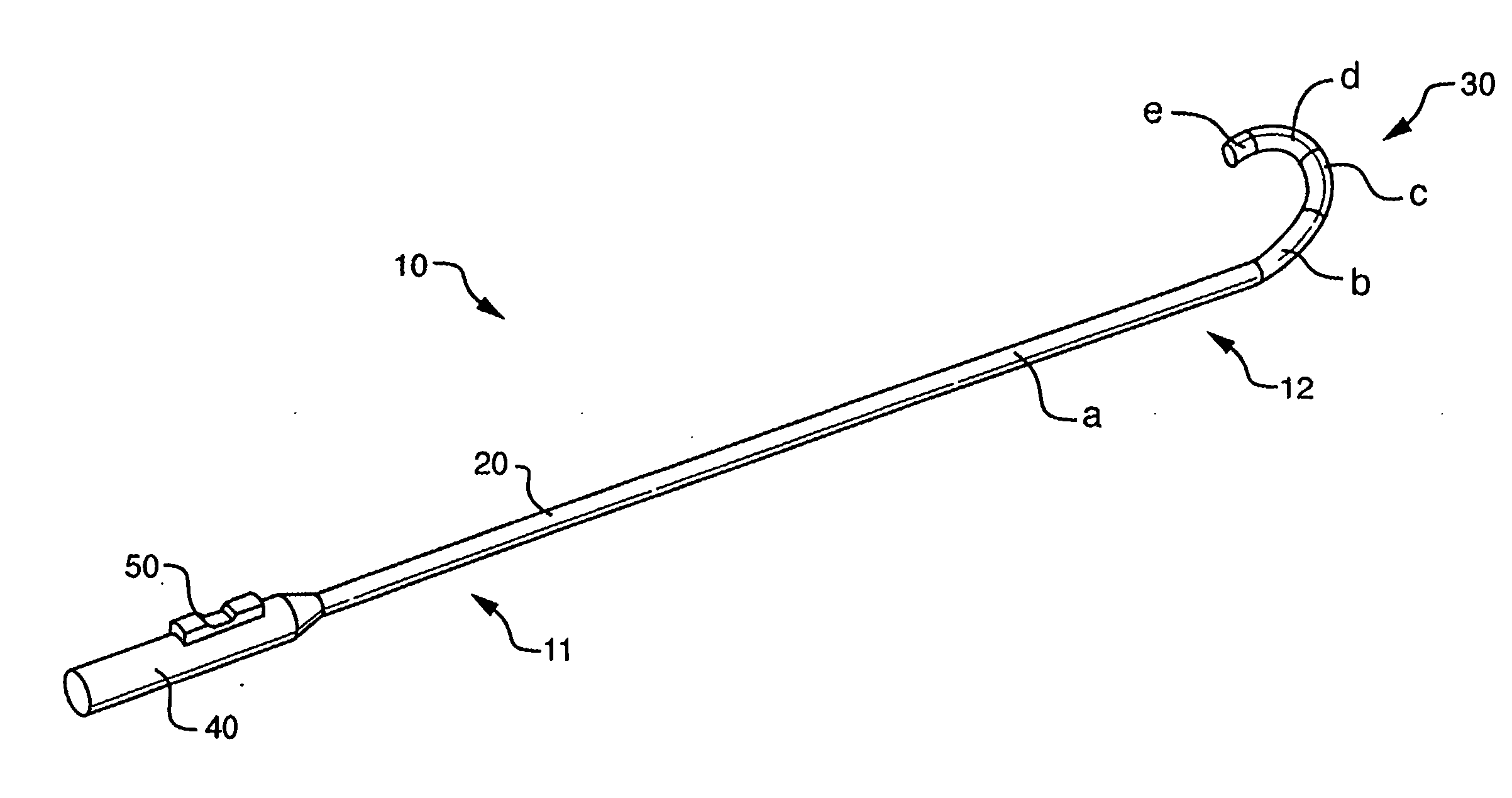
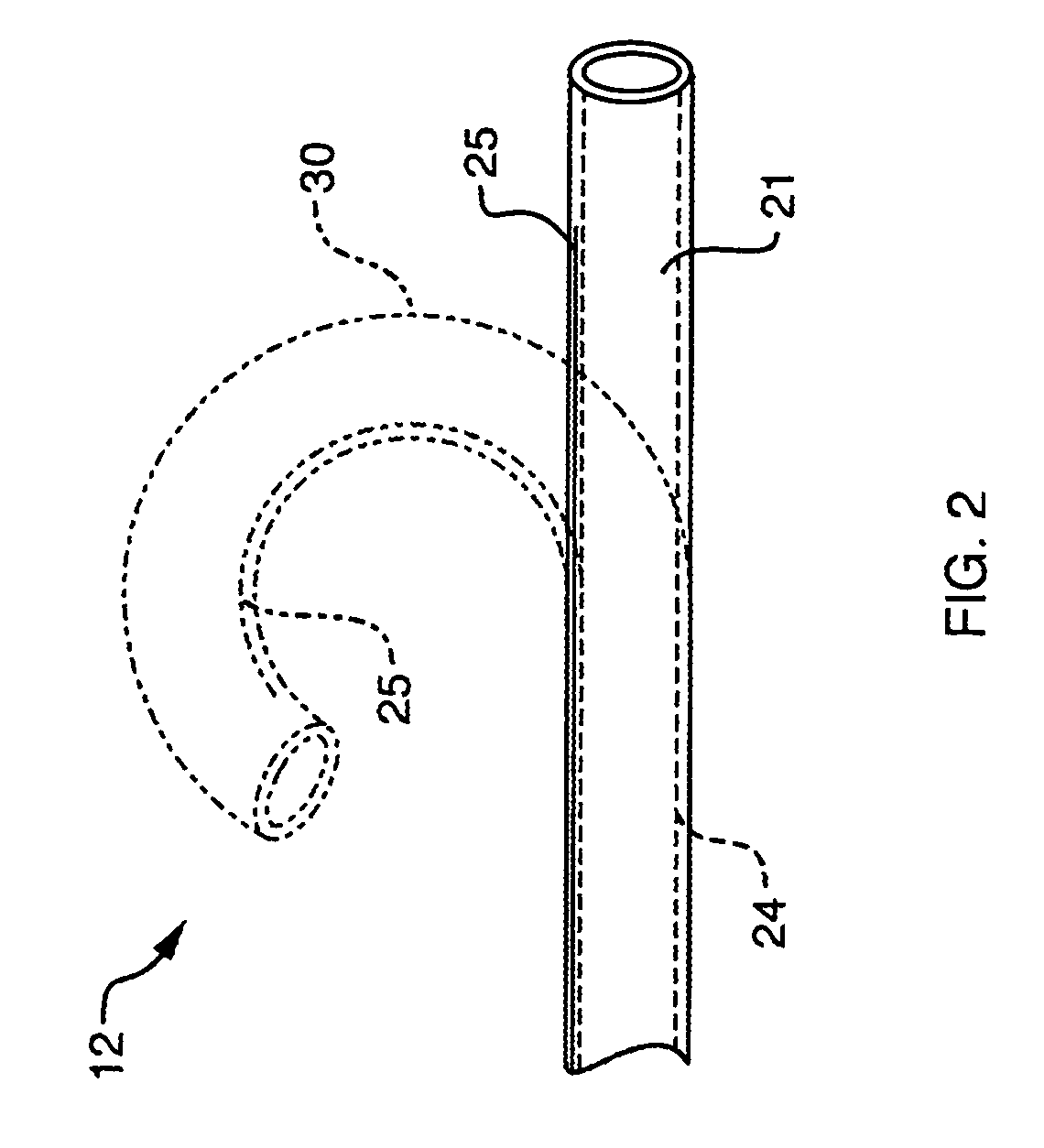
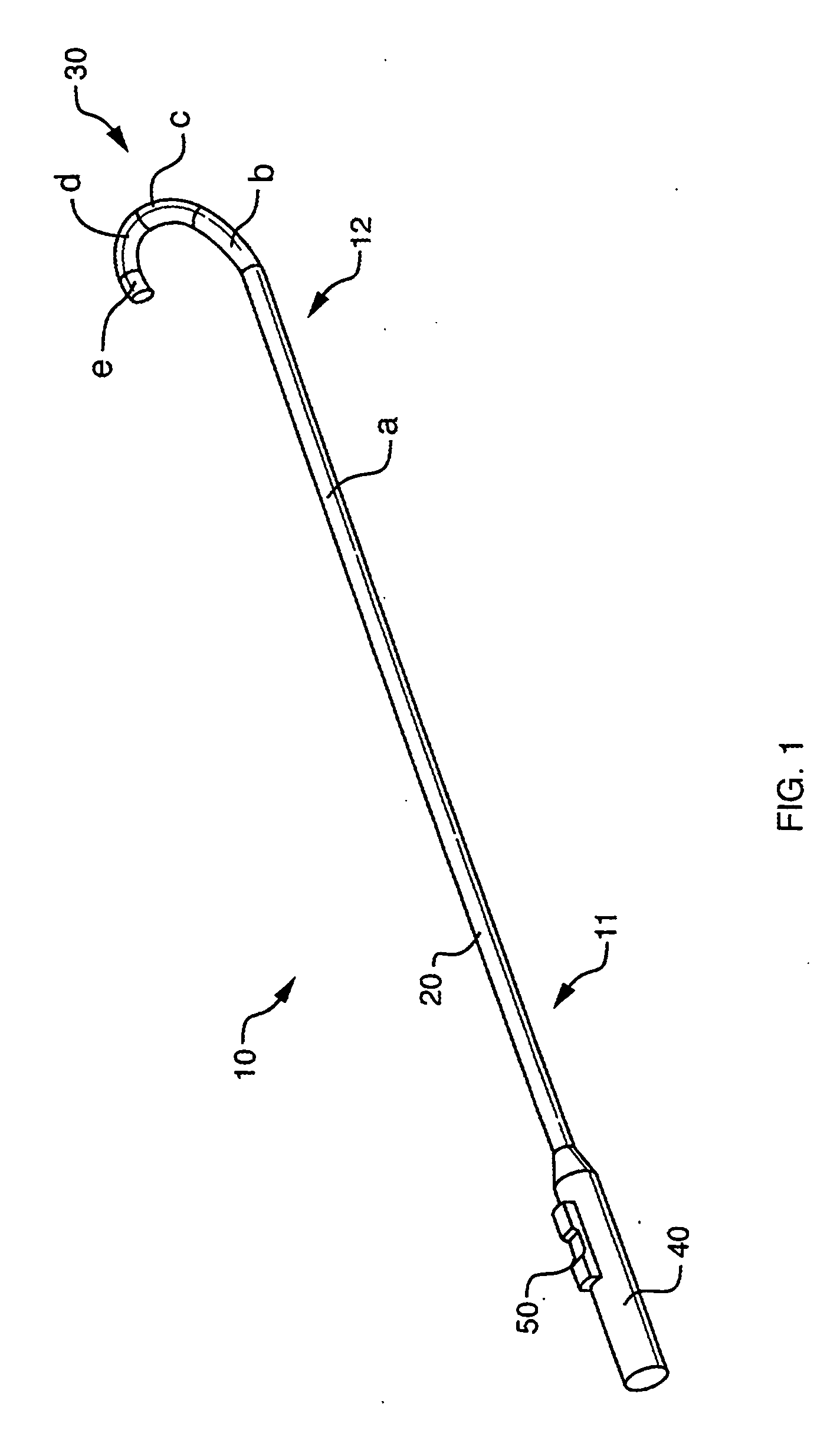
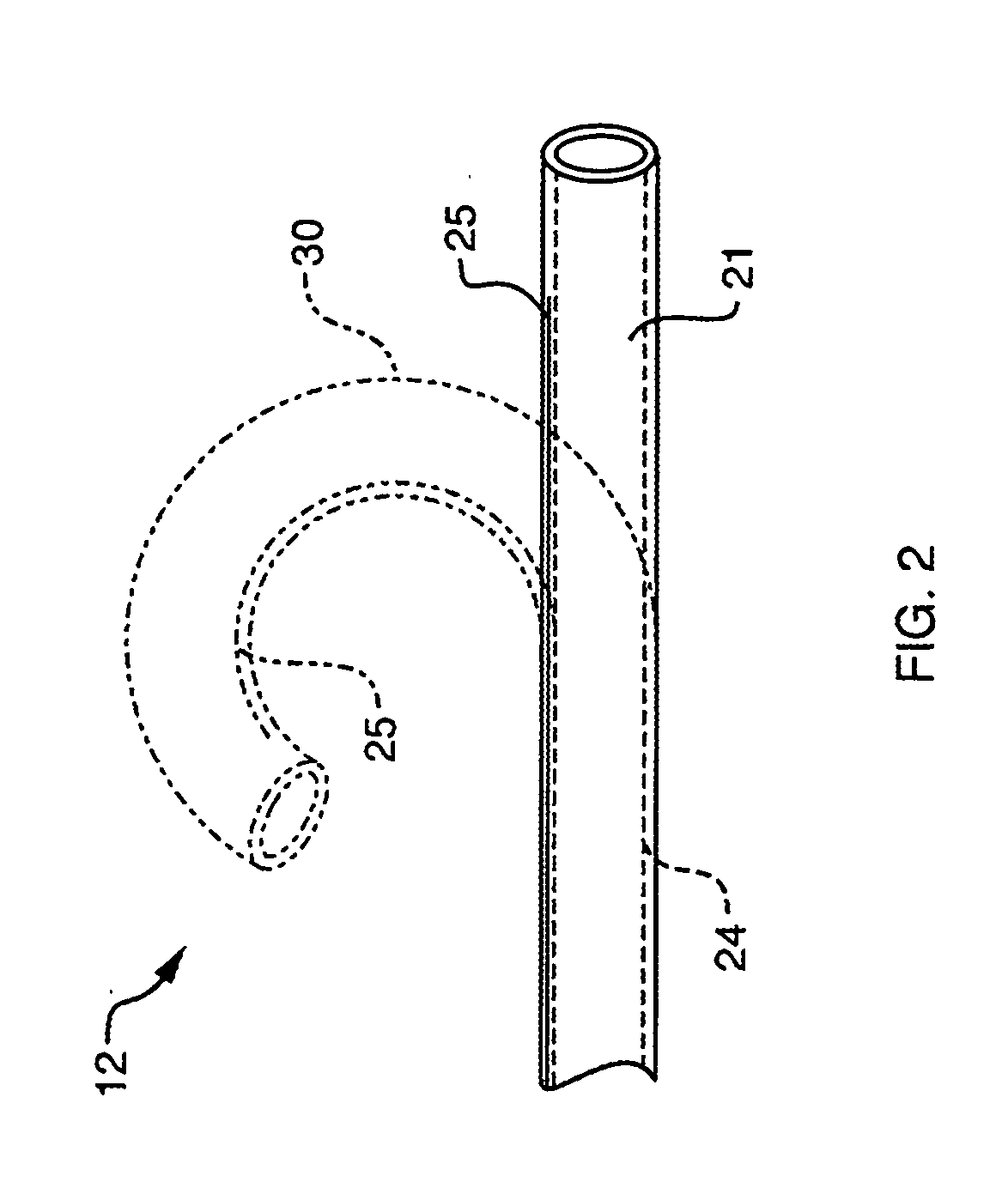
Coiled ablation catheter system
InactiveUS6960206B2Facilitate formation of lesionPromote formationStentsSurgical instruments for heatingVeinCardiac Ablation
A cardiac ablation catheter includes a coil-like ablating element that is deployable from an elongate, flexible sheath. The ablating element, while in the deployed position, has a shape with at least one revolution oriented in a plane that is orthogonal to a longitudinal axis of the sheath. The catheter system is well-suited to ablate a circumferential region of tissue about a pulmonary vein or the posterior wall of the left atrium proximate the pulmonary vein os. The treated tissue region electrically isolates the atria from the pulmonary vein.
Owner:THE GENERAL HOSPITAL CORP
Method for Ablating Body Tissue
A cardiac ablation method including the following steps: inserting a treatment catheter into an atrium of a heart, the treatment catheter including an ultrasound emitter; positioning the ultrasound emitter to face heart tissue within the left atrium outside of a pulmonary vein; emitting ultrasound energy from the ultrasound emitter while rotating the ultrasound emitter about a rotation axis; and ablating heart tissue with the ultrasound energy to form a lesion outside of a pulmonary vein.
Owner:AURIS HEALTH INC
Multi-electrode ablation sensing catheter and system
InactiveUS20100168557A1Enhanced informationMinimize impactElectrocardiographySurgical instruments for heatingCardiac AblationMedical treatment
The invention is directed to a multi-electrode ablation sensing catheter and system suitable for medical procedures such as cardiac ablation. In one embodiment of the invention, a catheter is provided having an elongated catheter shaft and a catheter tip having two or more closely spaced electrodes mounted on the catheter tip, where the electrodes are coupled to a plurality of electronic circuitries and are used for electrogram sensing, impedance sensing, and location sensing and orientation. In another embodiment of the invention, a catheter system is provided having a catheter with an elongated catheter shaft and a catheter tip with two or more closely spaced electrodes mounted on the catheter tip, and an RF generator circuitry, an electrogram sensing circuitry, an impedance sensing circuitry, and a location sensing and orientation circuitry.
Owner:ST JUDE MEDICAL ATRIAL FIBRILLATION DIV
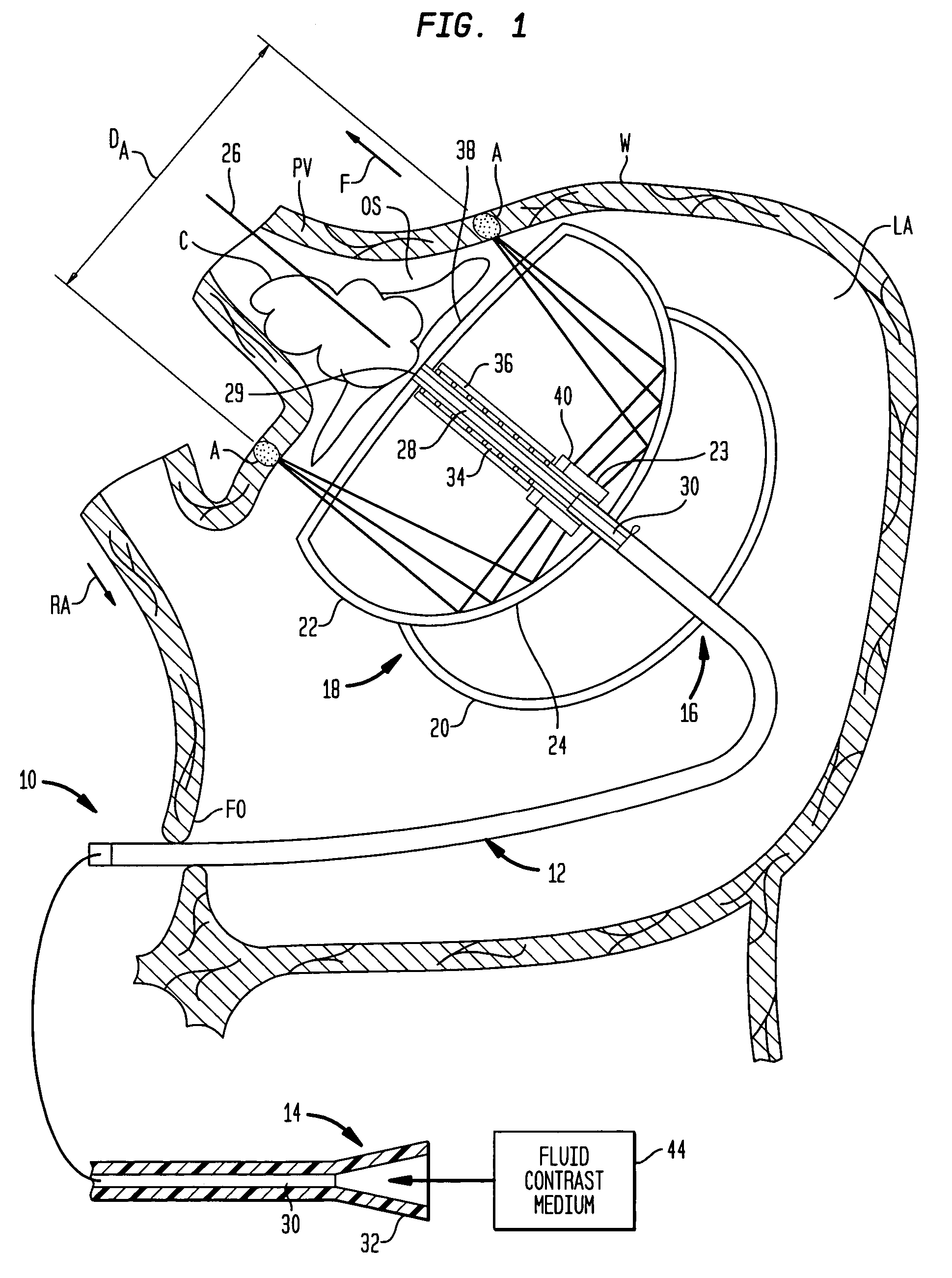
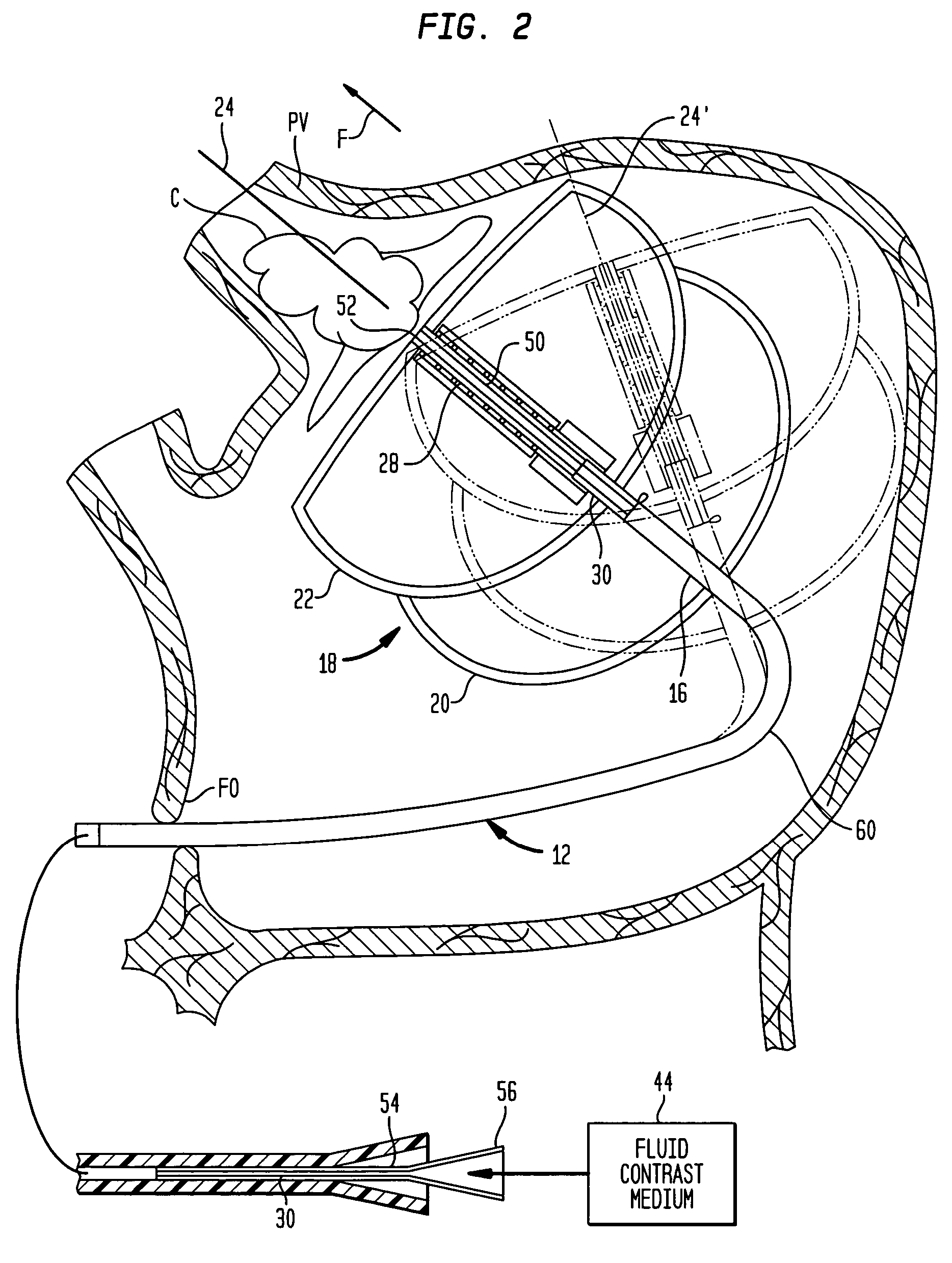
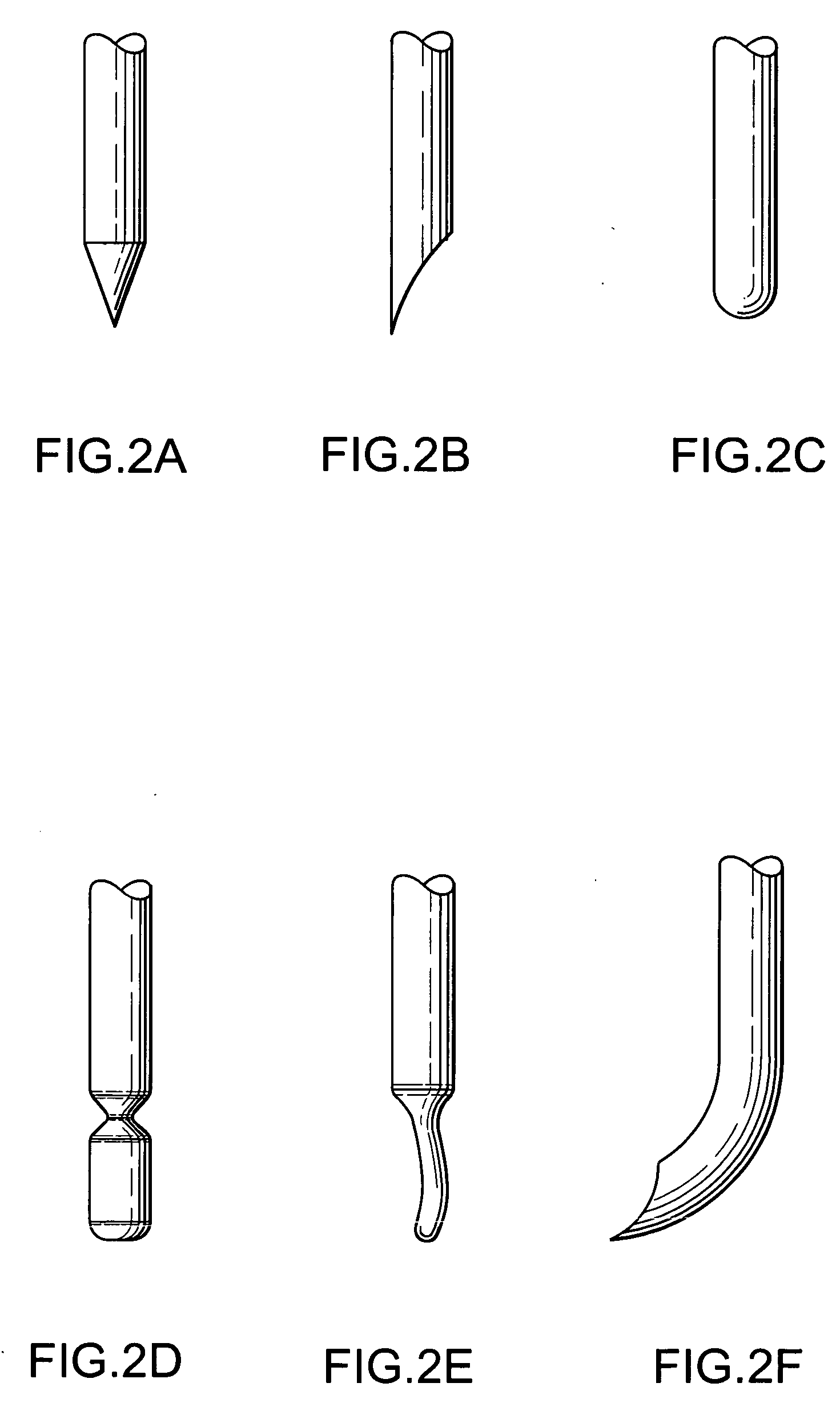
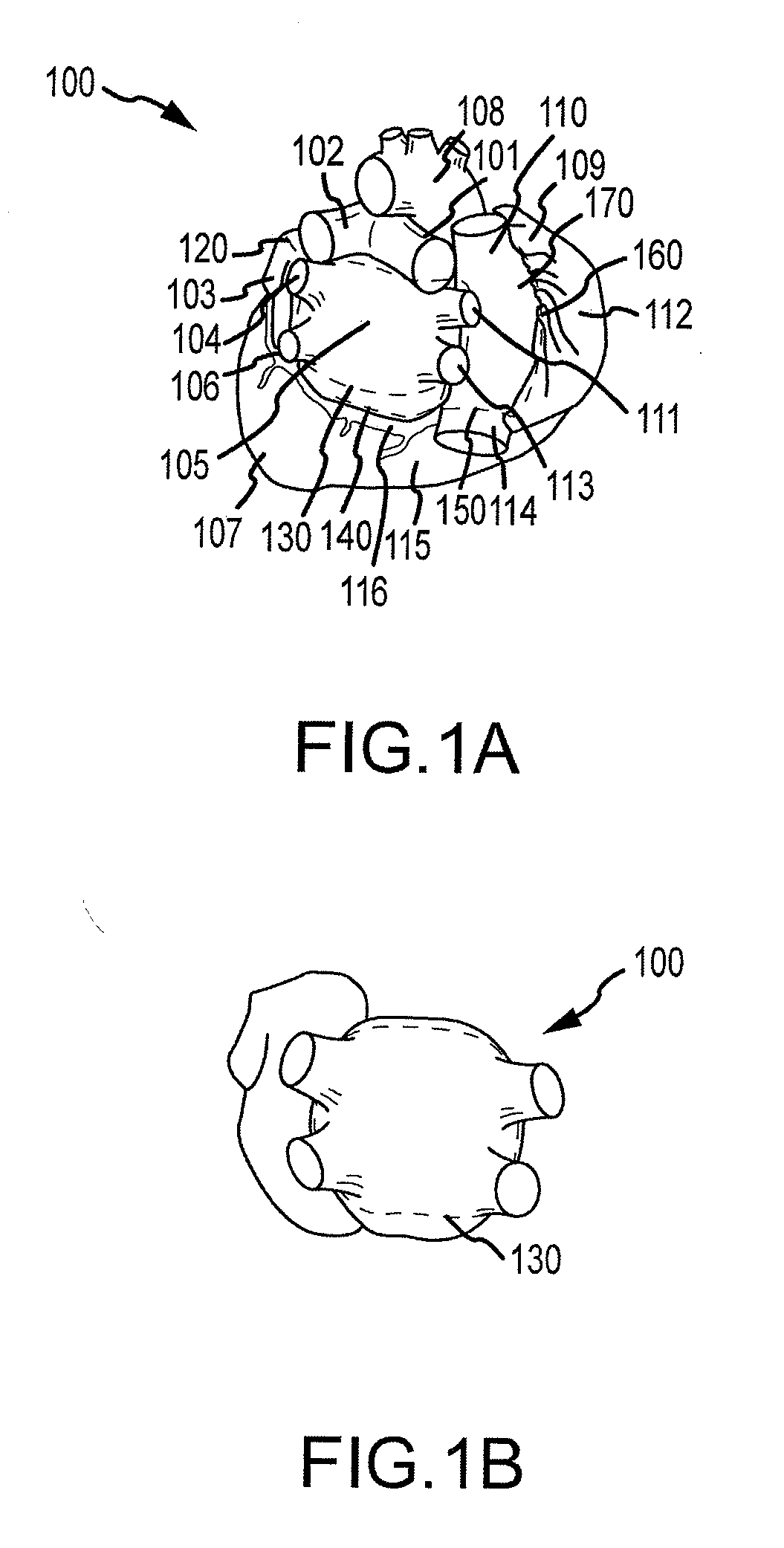
Cardiac ablation devices
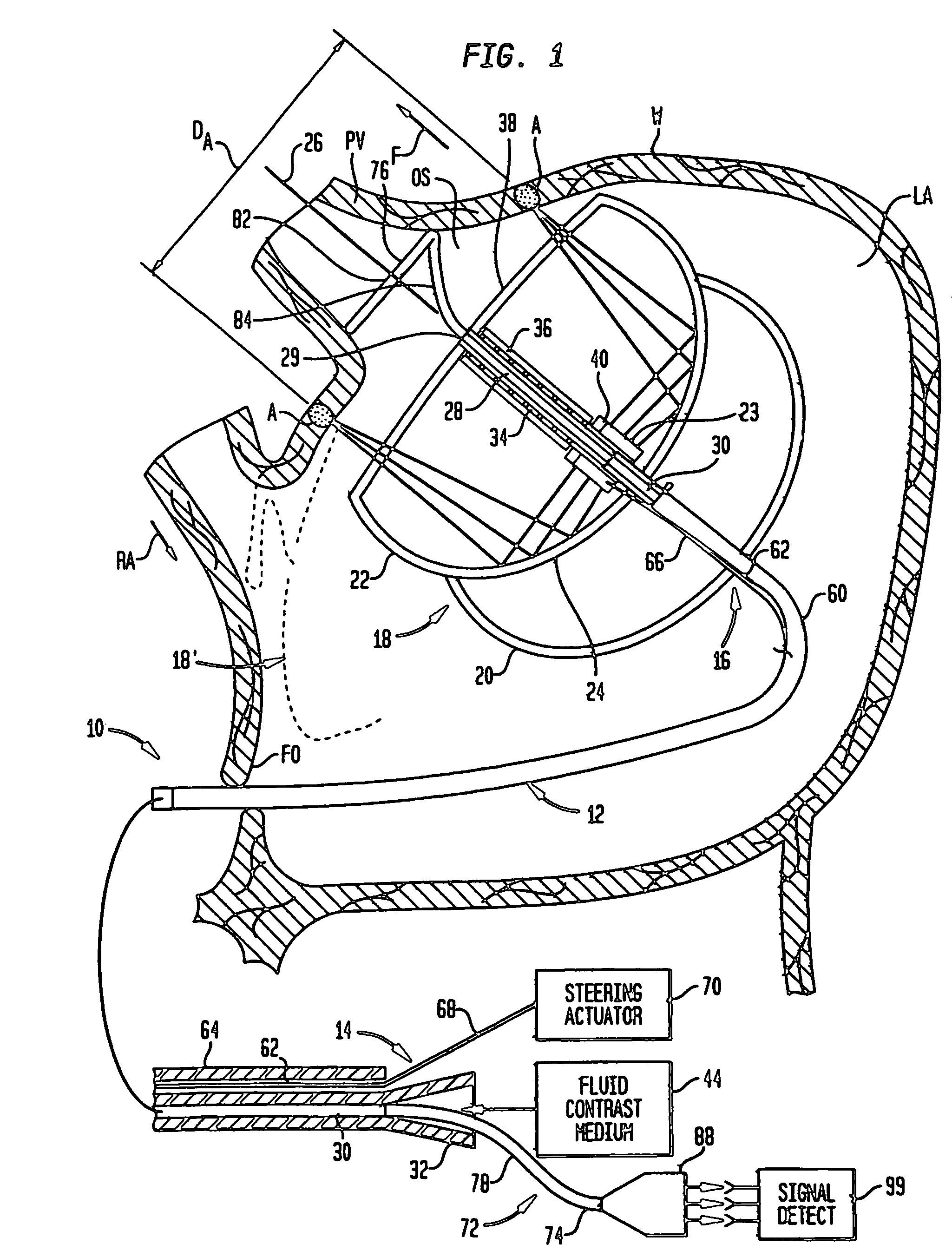
A cardiac ablation device treats atrial fibrillation by directing and focusing ultrasonic waves into a ring-like ablation region (A). The device desirably is steerable and can be moved between a normal disposition, in which the ablation region lies parallel to the wall of the heart for ablating a loop-like lesion, and a canted disposition, in which the ring-like focal region is tilted relative to the wall of the heart, to ablate only a short, substantially linear lesion. The ablation device desirably includes a balloon reflector structure (18, 1310) and an ultrasonic emitter assembly (23, 1326), and can be steered and positioned without reference to engagement between the device and the pulmonary vein or ostium. A contrast medium (C) can be injected through the ablation device to facilitate imaging, so that the device can be positioned based on observation of the images.
Owner:BOSTON SCI SCIMED INC
Bipolar tissue treatment system
InactiveUS20050177209A1Reduce the temperatureSurgical instruments for heatingTherapeutic coolingRadio frequency energyCardiac Ablation
A novel medical probe assembly, system, and methods for the use thereof to treat tissue are described. The system optionally comprises an energy source, two probe assemblies, and one or more cooling devices to provide cooling to at least one of the probe assemblies. The probe assemblies may be configured in a bipolar mode, whereby current flows preferentially between the probe assemblies. The probe assemblies and system described herein are particularly useful to deliver radio frequency energy to a patient's body. RF energy delivery may be used for various applications, including the treatment of pain, tumor ablation and cardiac ablation.
Owner:BAYLIS MEDICAL
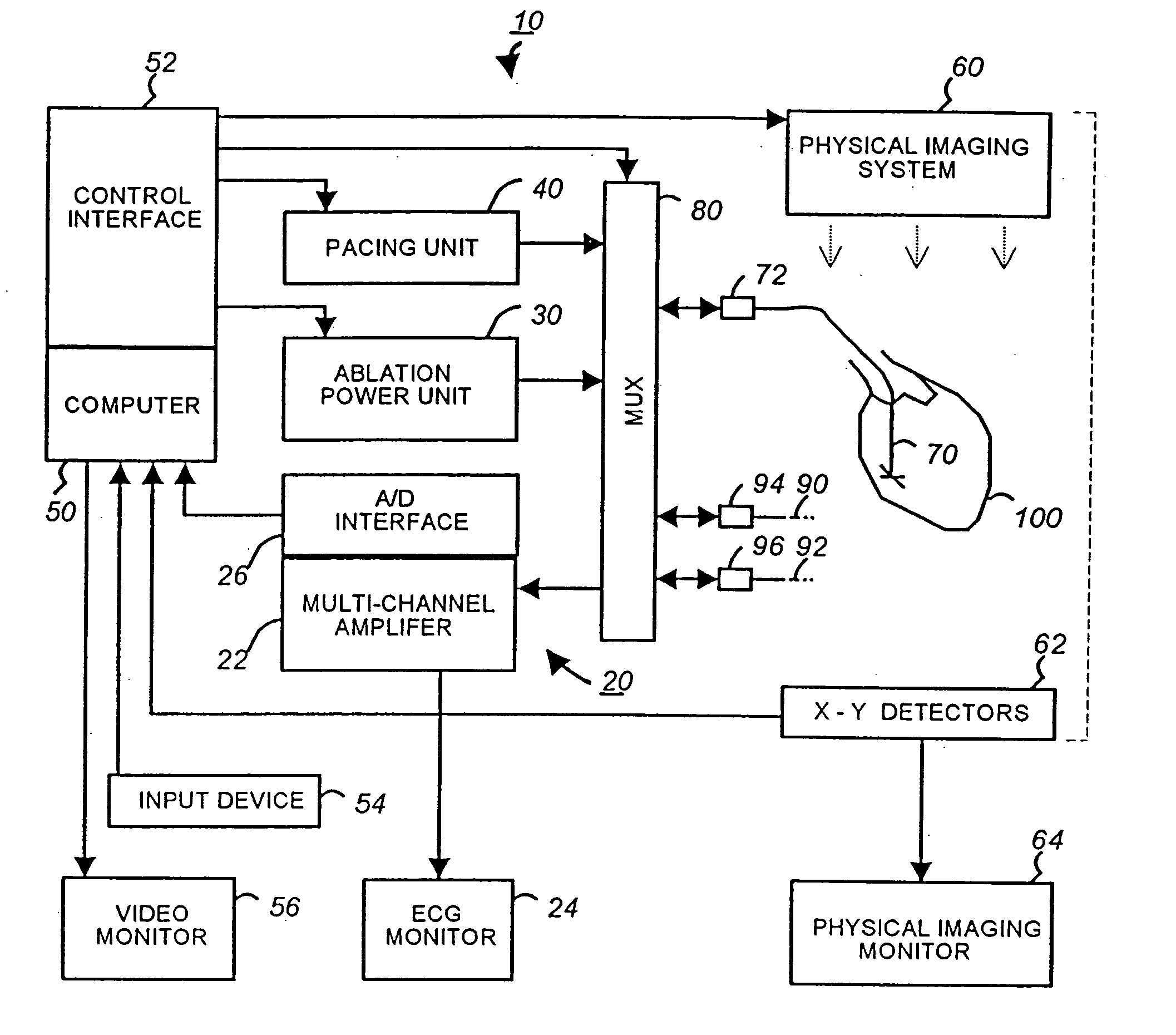
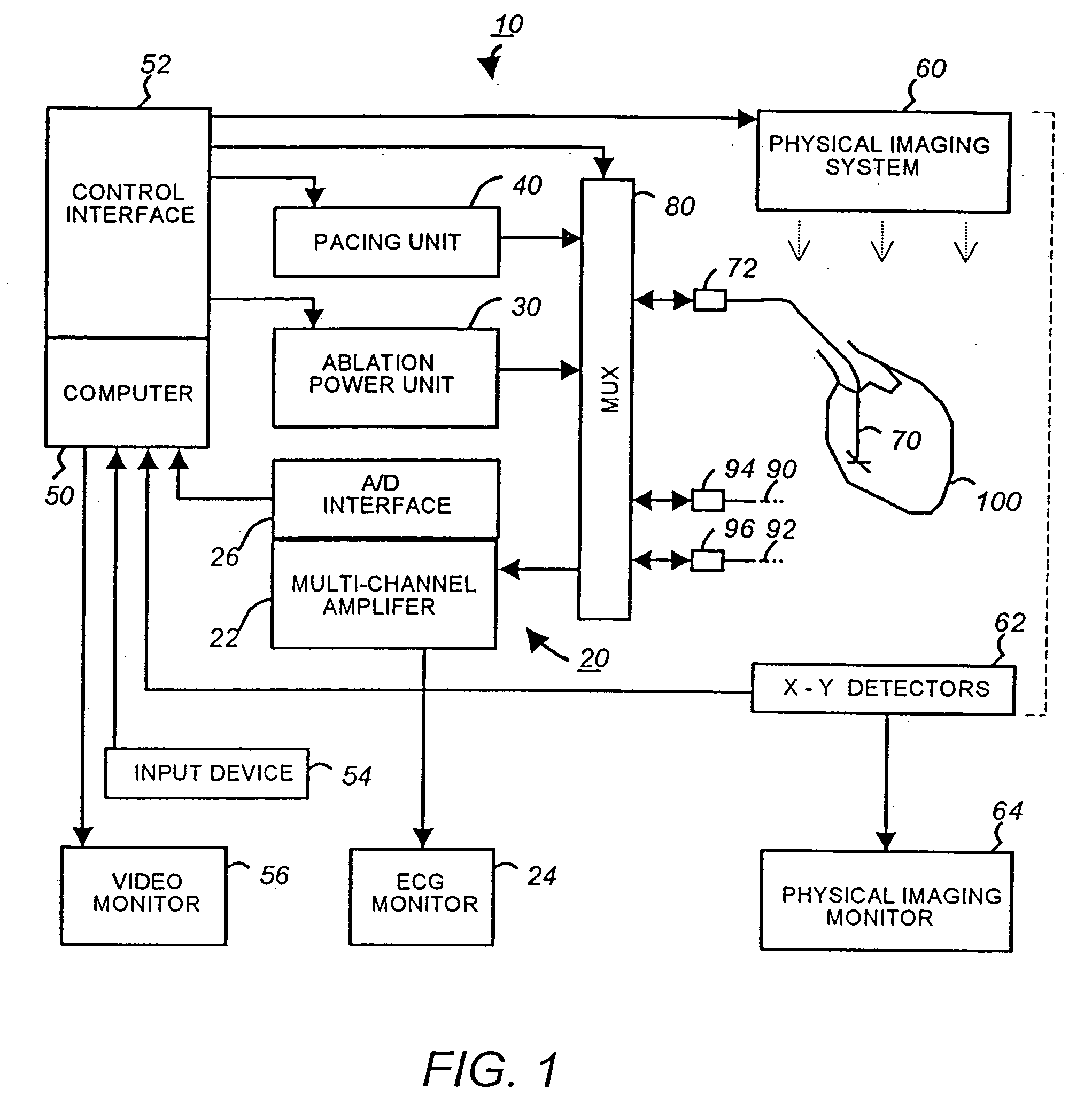
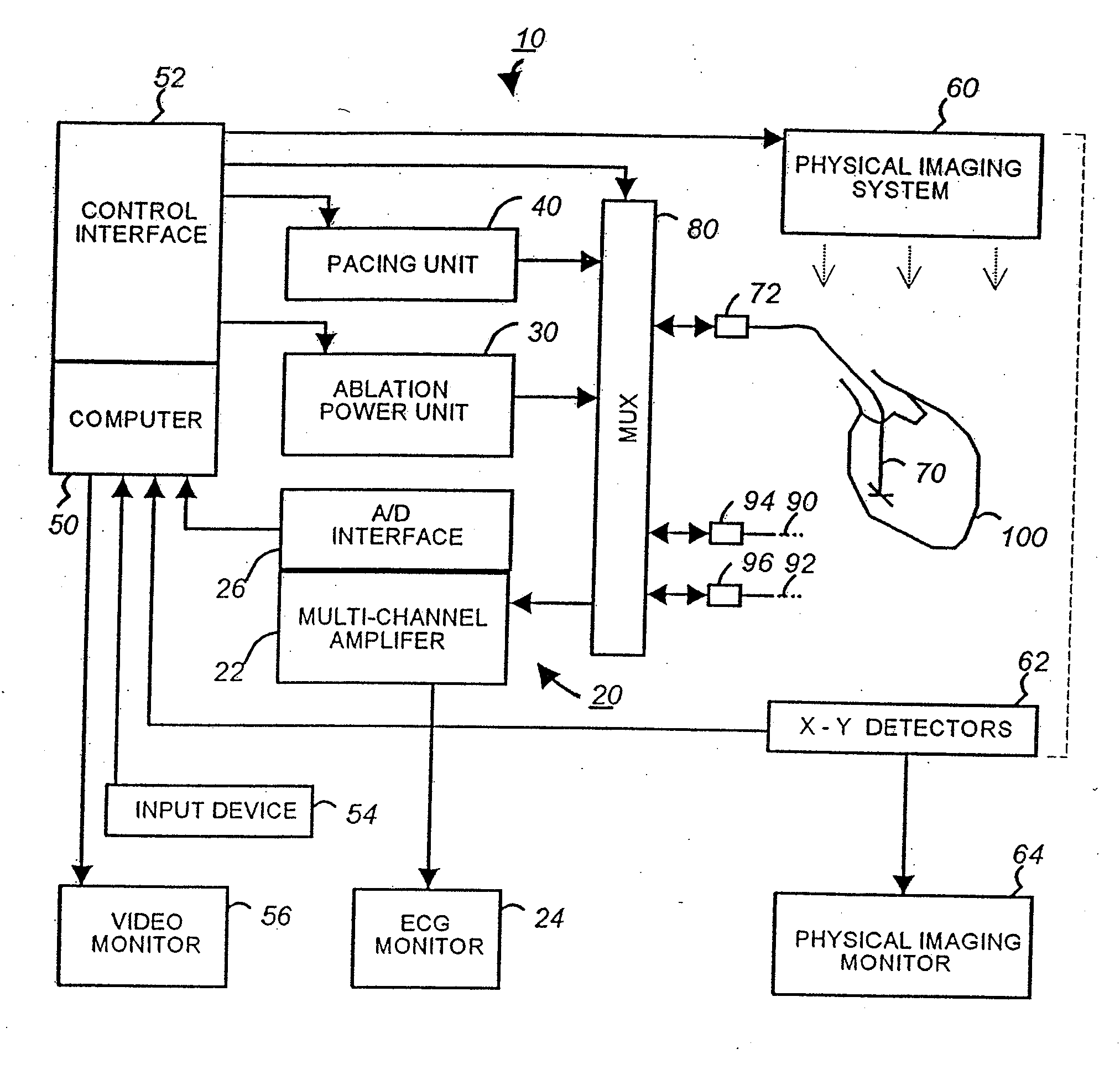
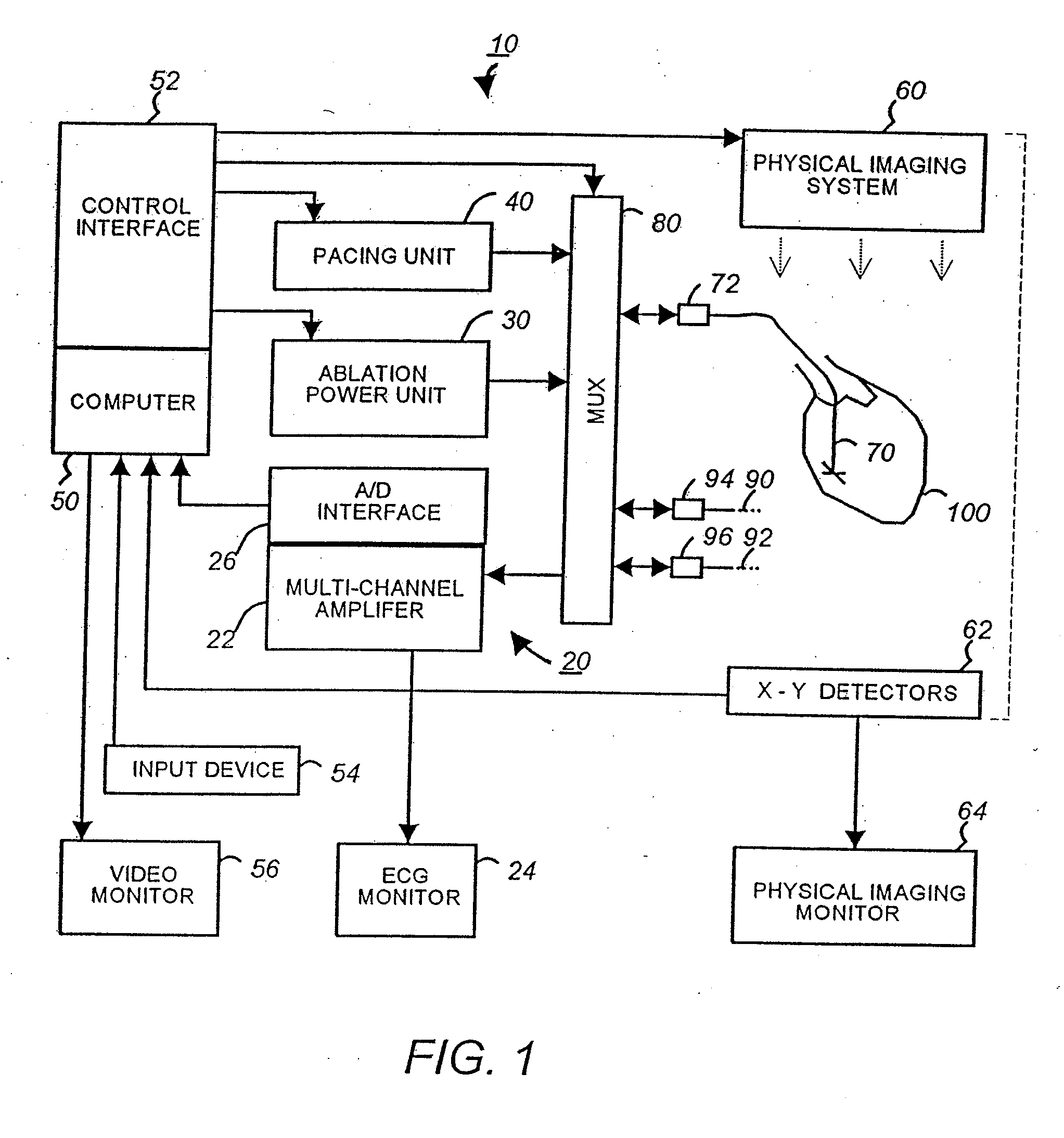
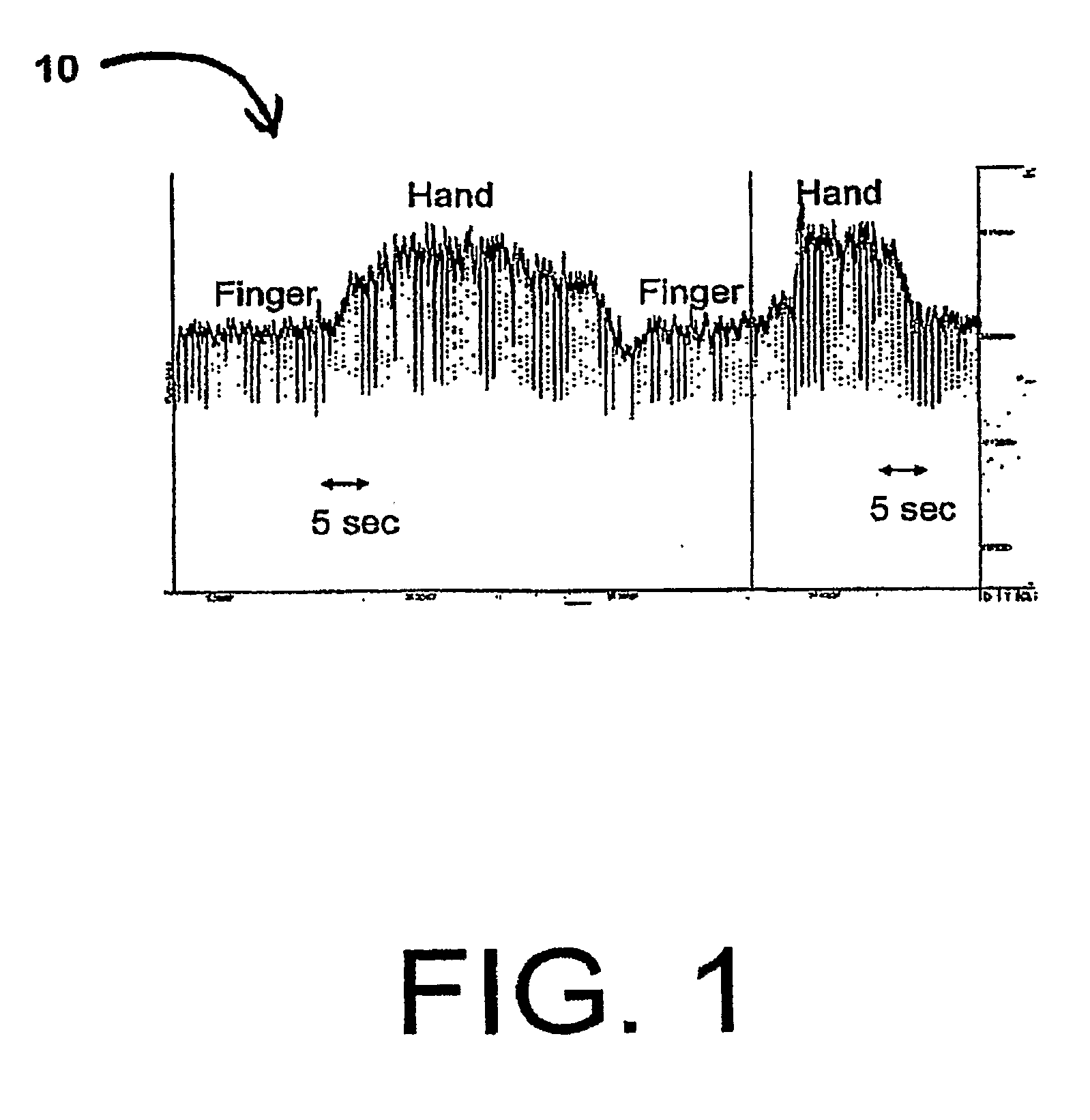
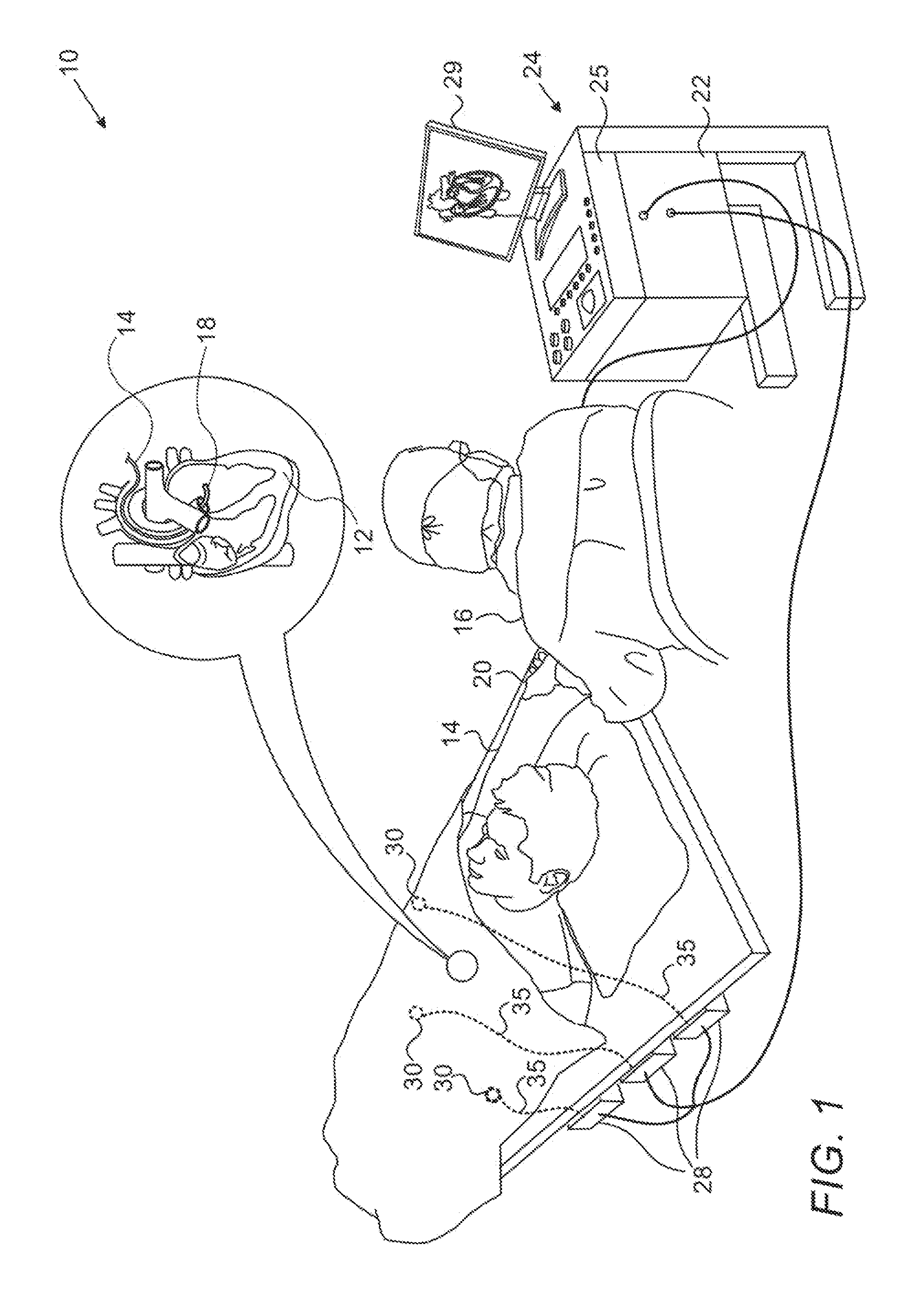
Apparatus and method for cardiac ablation
InactiveUS20050148892A1ElectrocardiographyControlling energy of instrumentVisual perceptionIntracardiac Electrogram
A system and method for cardiac mapping and ablation include a multi-electrode catheter introduced percutaneously into a subject's heart and deployable adjacent to various endocardial sites. The electrodes are connectable to a mapping unit, an ablation power unit a pacing unit, all of which are under computer control. Intracardiac electrogram signals emanated from a tachycardia site of origin are detectable by the electrodes. Their arrival times are processed to generate various visual maps to provide real-time guidance for steering the catheter to the tachycardia site of origin. In another aspect, the system also include a physical imaging system which is capable of providing different imaged physical views of the catheter and the heart. These physical views are incorporated into the various visual maps to provide a more physical representation. Once the electrodes are on top of the tachycardia site of origin, electrical energy is supplied by the ablation power unit to effect ablation.
Owner:DESAI JAWAHAR M
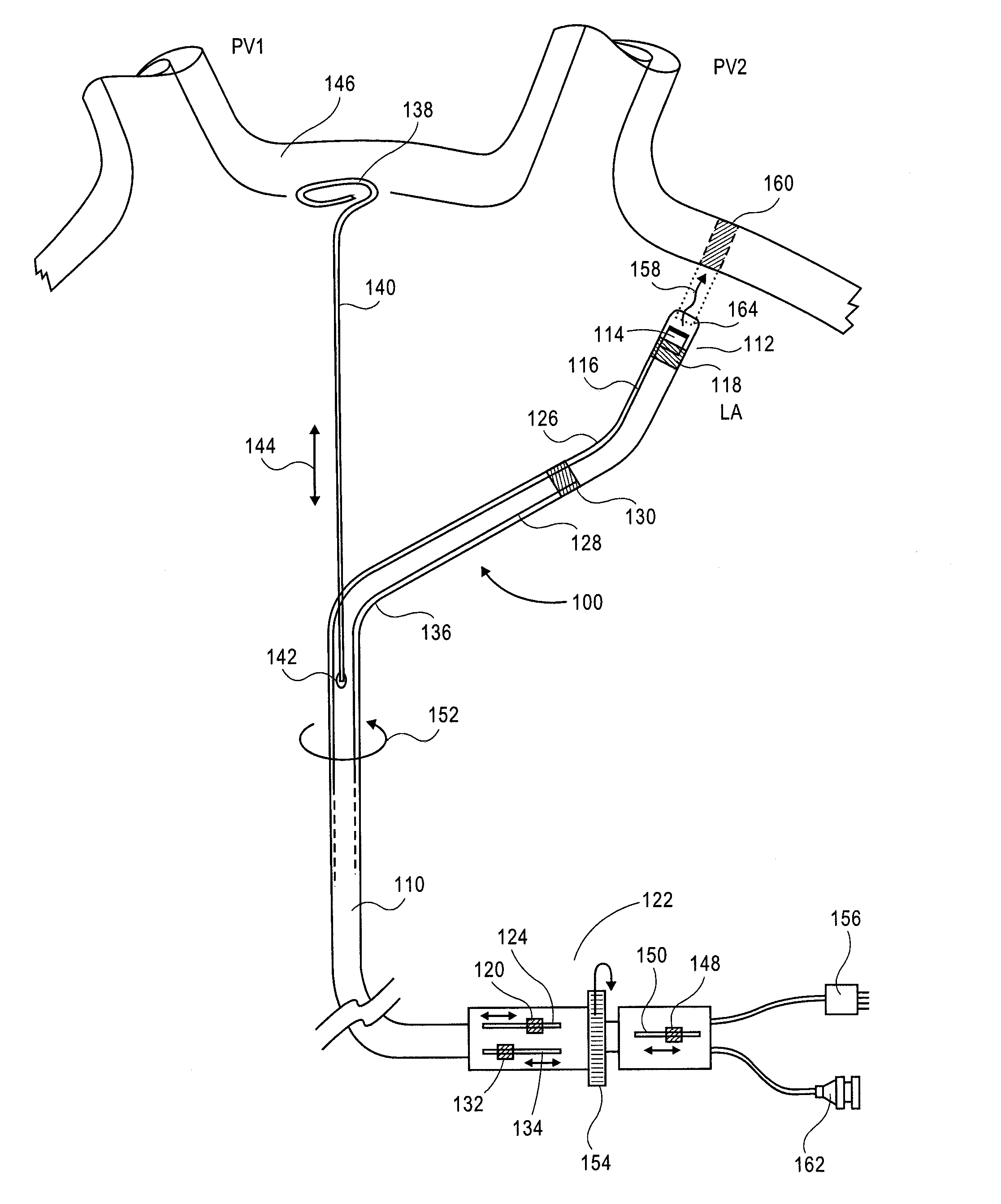
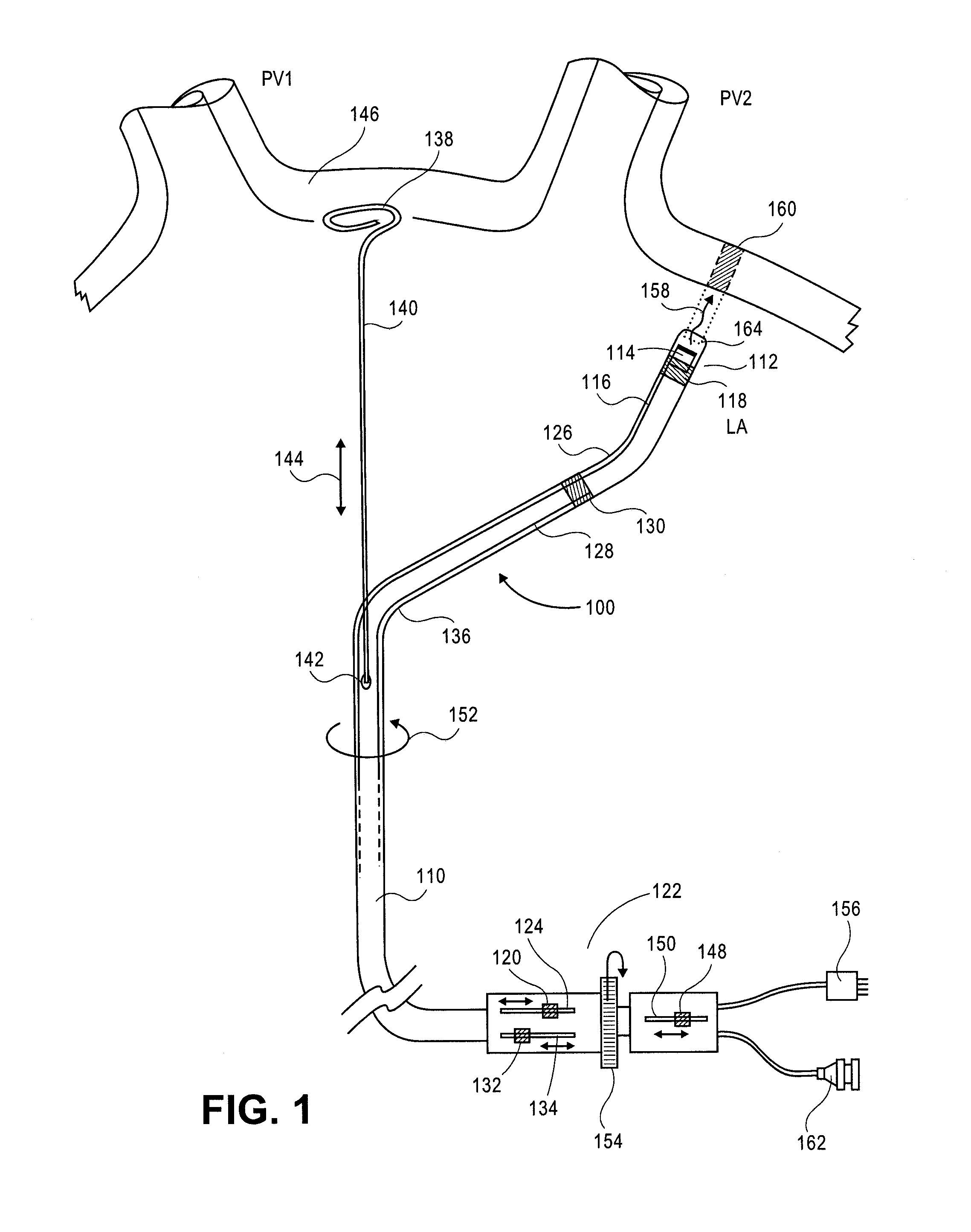
Methods of cardiac ablation employing a deflectable sheath catheter
The present invention provides devices and methods for the treatment of atrial fibrillation. In one embodiment method for treatment of atrial fibrillation is provided that includes positioning a sheath catheter having a deflectable distal end segment in the left atrium of a heart, orienting said sheath catheter such that an ablation instrument can be delivered through the sheath catheter to a position proximal to a first pulmonary vein, activating the ablation instrument to form a circumferential lesion around the first pulmonary vein, repositioning the sheath catheter by deflecting the distal end segment to another orientation, and activating the ablation instrument to form a circumferential lesion around at least one additional pulmonary vein.
Owner:CARDIOFOCUS INC
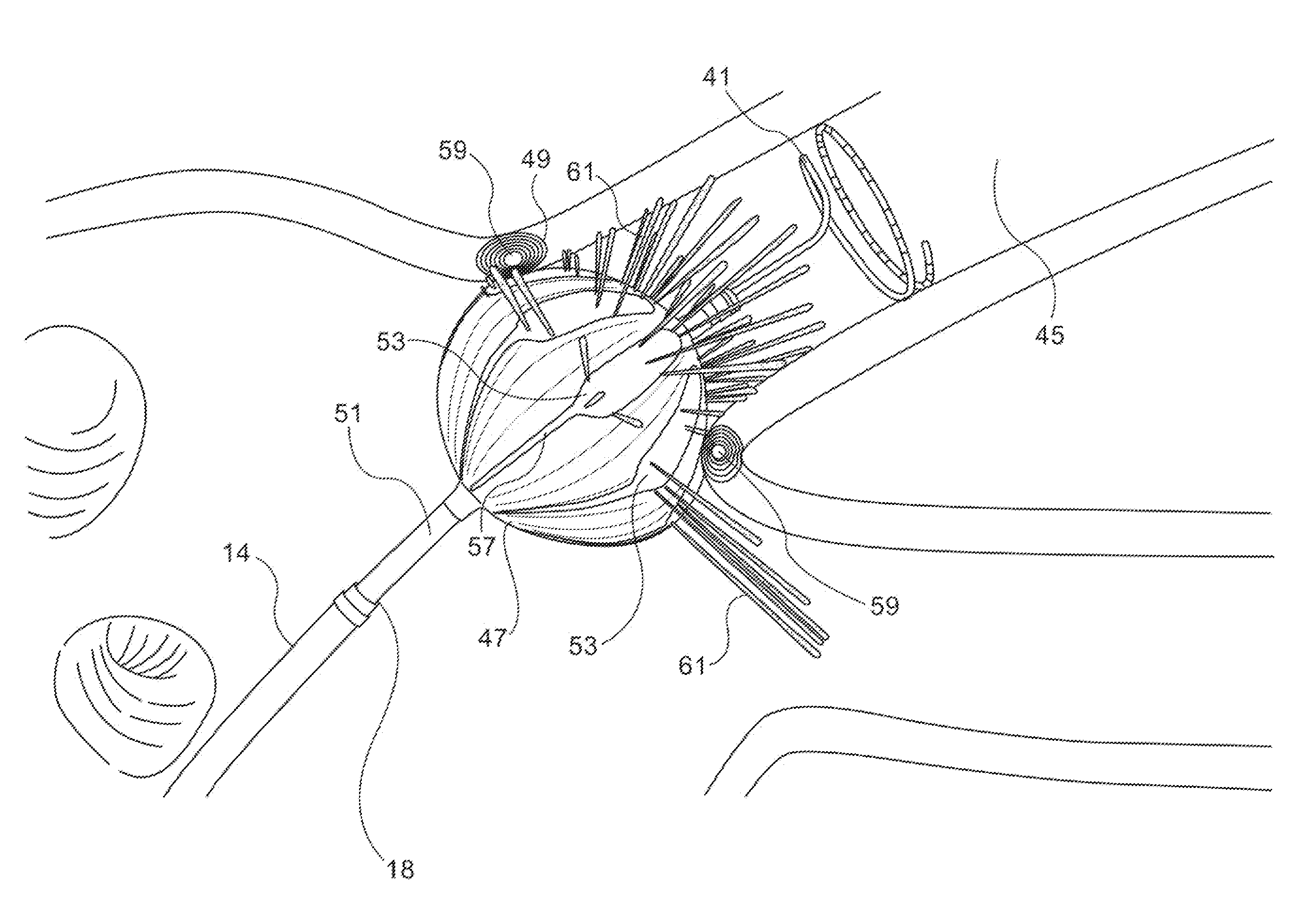
Conduction block verification probe and method of use
ActiveUS20060015165A1Lower impedanceImprove conductivityEpicardial electrodesSurgical needlesVeinCardiac arrhythmia
Devices and methods provide for ablation of cardiac tissue for treating cardiac arrhythmias such as atrial fibrillation. Although the devices and methods are often be used to ablate epicardial tissue in the vicinity of at least one pulmonary vein, various embodiments may be used to ablate other cardiac tissues in other locations on a heart. Devices generally include at least one tissue contacting member for contacting epicardial tissue and securing the ablation device to the epicardial tissue, and at least one ablation member for ablating the tissue. Various embodiments include features, such as suction apertures, which enable the device to attach to the epicardial surface with sufficient strength to allow the tissue to be stabilized via the device. For example, some embodiments may be used to stabilize a beating heart to enable a beating heart ablation procedure. Many of the devices may be introduced into a patient via minimally invasive introducer devices and the like. Although devices and methods of the invention may be used to ablate epicardial tissue to treat atrial fibrillation, they may also be used in veterinary or research contexts, to treat various heart conditions other than atrial fibrillation and / or to ablate cardiac tissue other than the epicardium.
Owner:ATRICURE
Methods of cardiac ablation in the vicinity of the right inferior pulmonary vein
The present invention provides devices and methods for the treatment of atrial fibrillation. In one embodiment a method for ablating tissue about an ostium of a right inferior vein of a heart includes positioning a sheath catheter having a deflectable distal end segment with a bent tip element in the left atrium of a heart, causing the distal end segment to deflect in a compound curve as the catheter is advanced towards an ostium of a right inferior vein, orienting said sheath catheter such that an ablation instrument can be delivered through the sheath catheter to a position proximal to the right inferior vein, and activating the ablation instrument to form at least one lesion about the right inferior vein.
Owner:CARDIOFOCUS INC
Electrosurgical tissue treatment method
InactiveUS20050177210A1Surgical instruments for heatingTherapeutic coolingCardiac AblationBiomedical engineering
A medical probe assembly, system, and methods for the use thereof to treat tissue are described. The system optionally comprises an energy source, two internally-cooled probe assemblies, and one or more cooling devices to provide cooling to at least one of the probe assemblies. The probe assemblies may be configured in a bipolar mode, whereby current flows preferentially between the probe assemblies. The probe assemblies and system described herein are particularly useful to deliver radio frequency energy to a patient's body. RF energy delivery may be used for various applications, including the treatment of pain, tumor ablation and cardiac ablation.
Owner:AVANOS MEDICAL SALES LLC
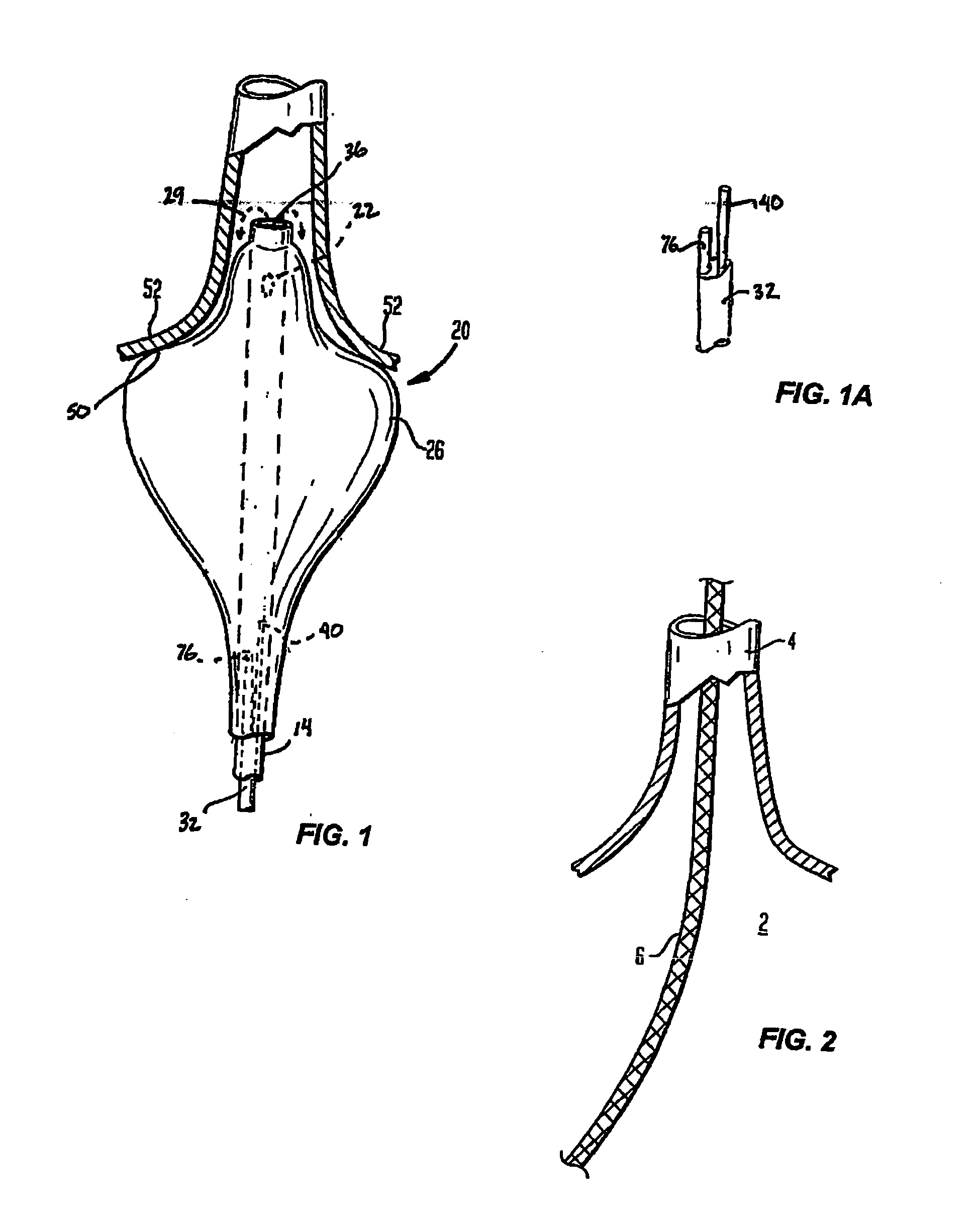
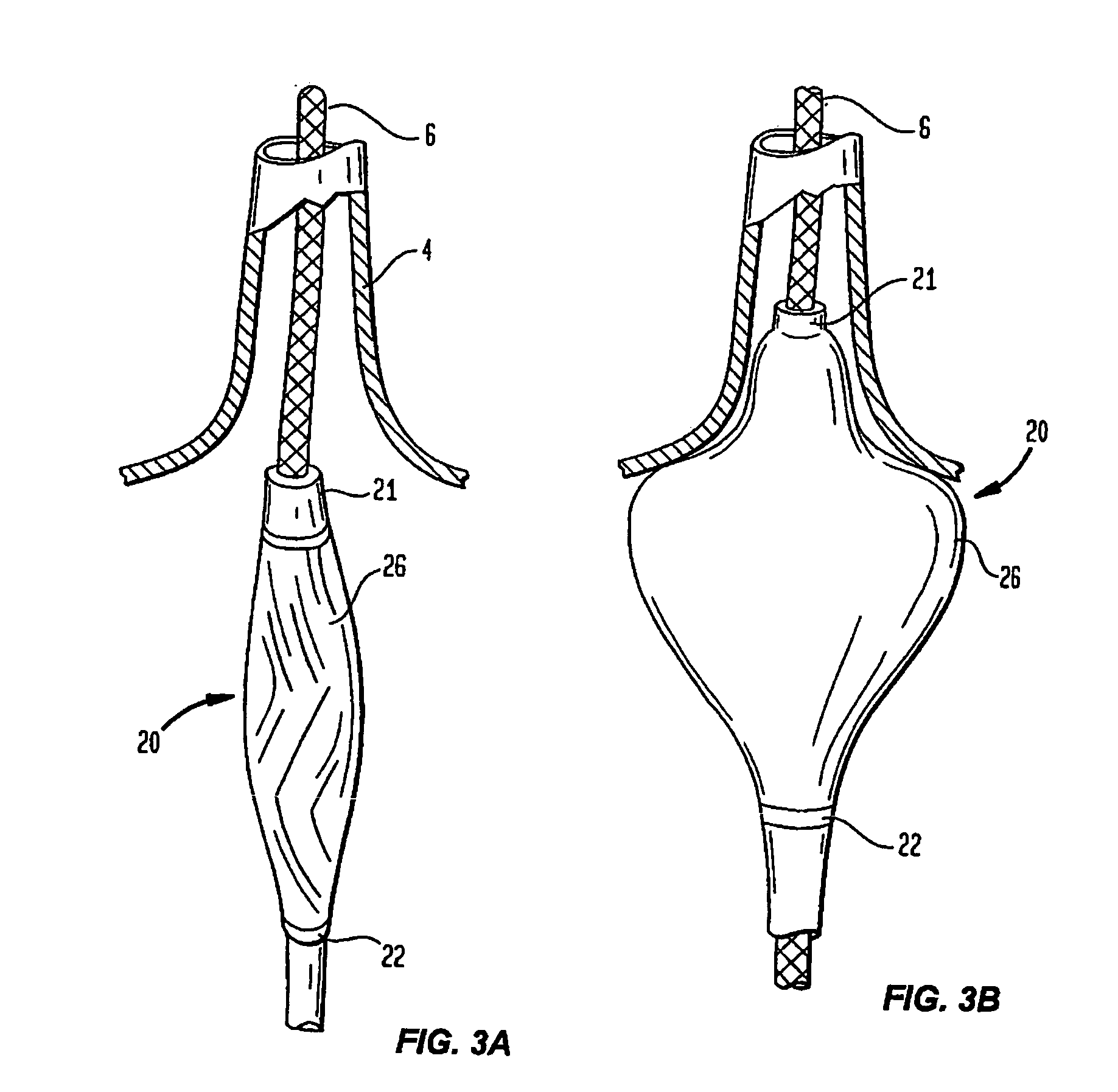
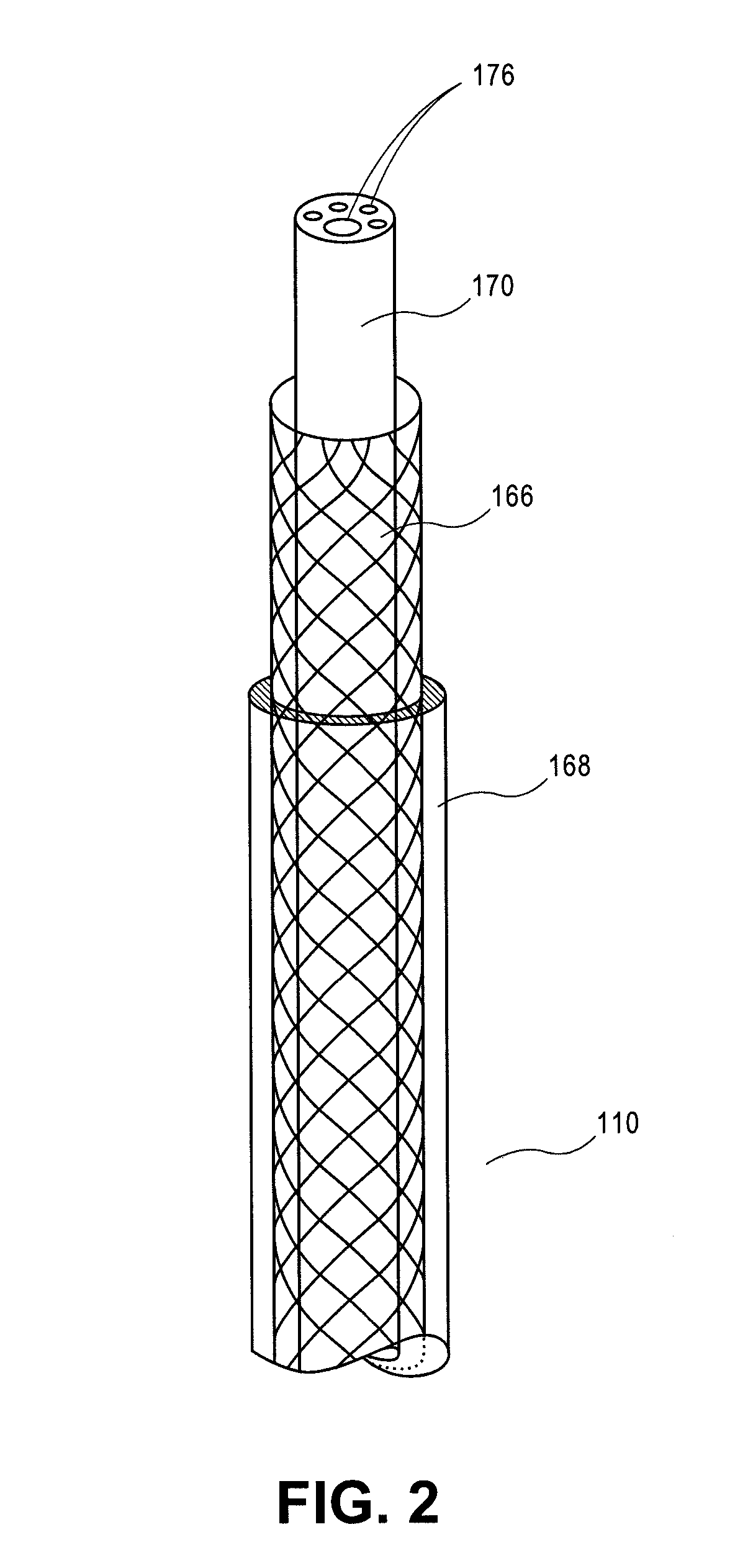
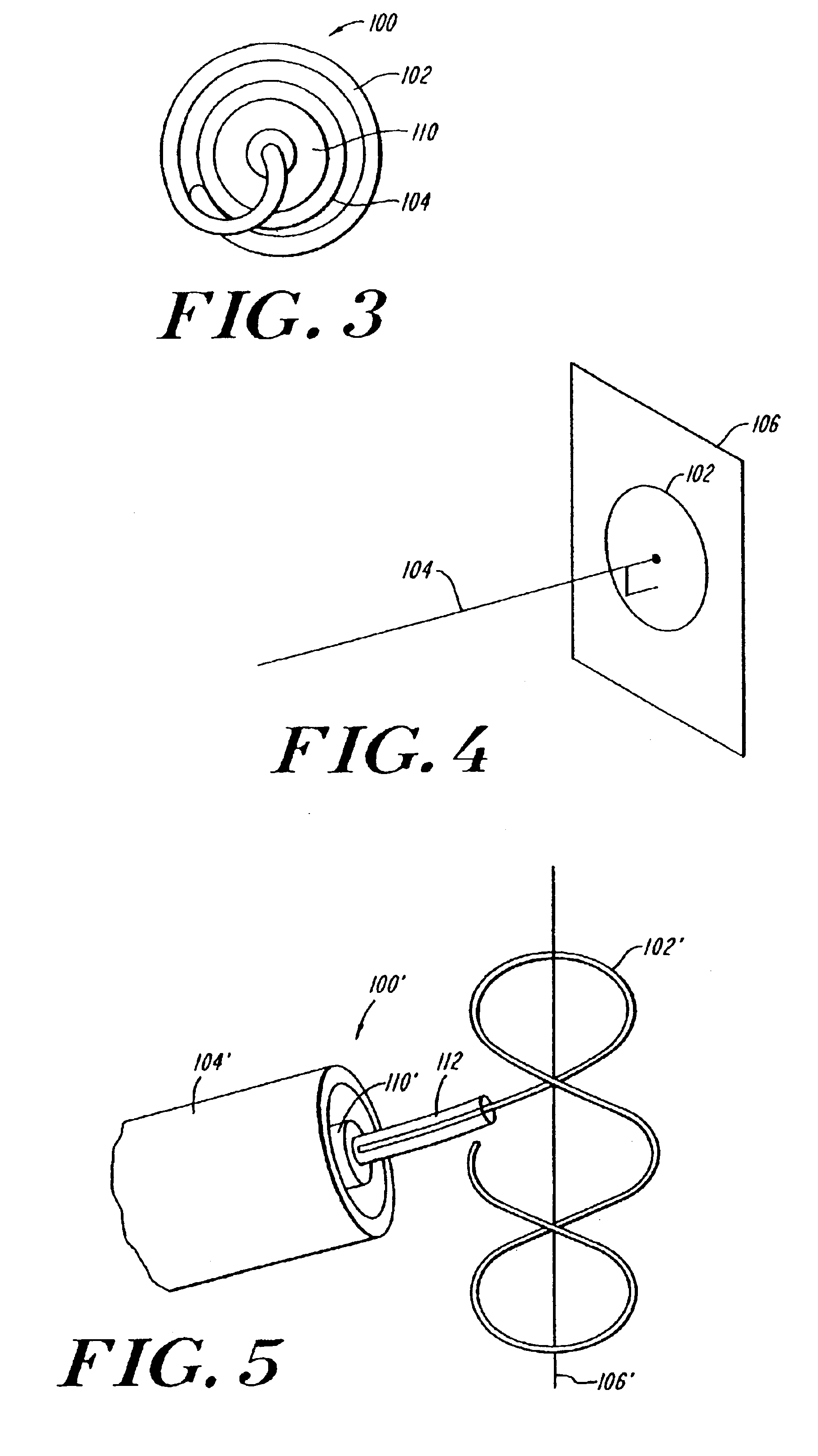
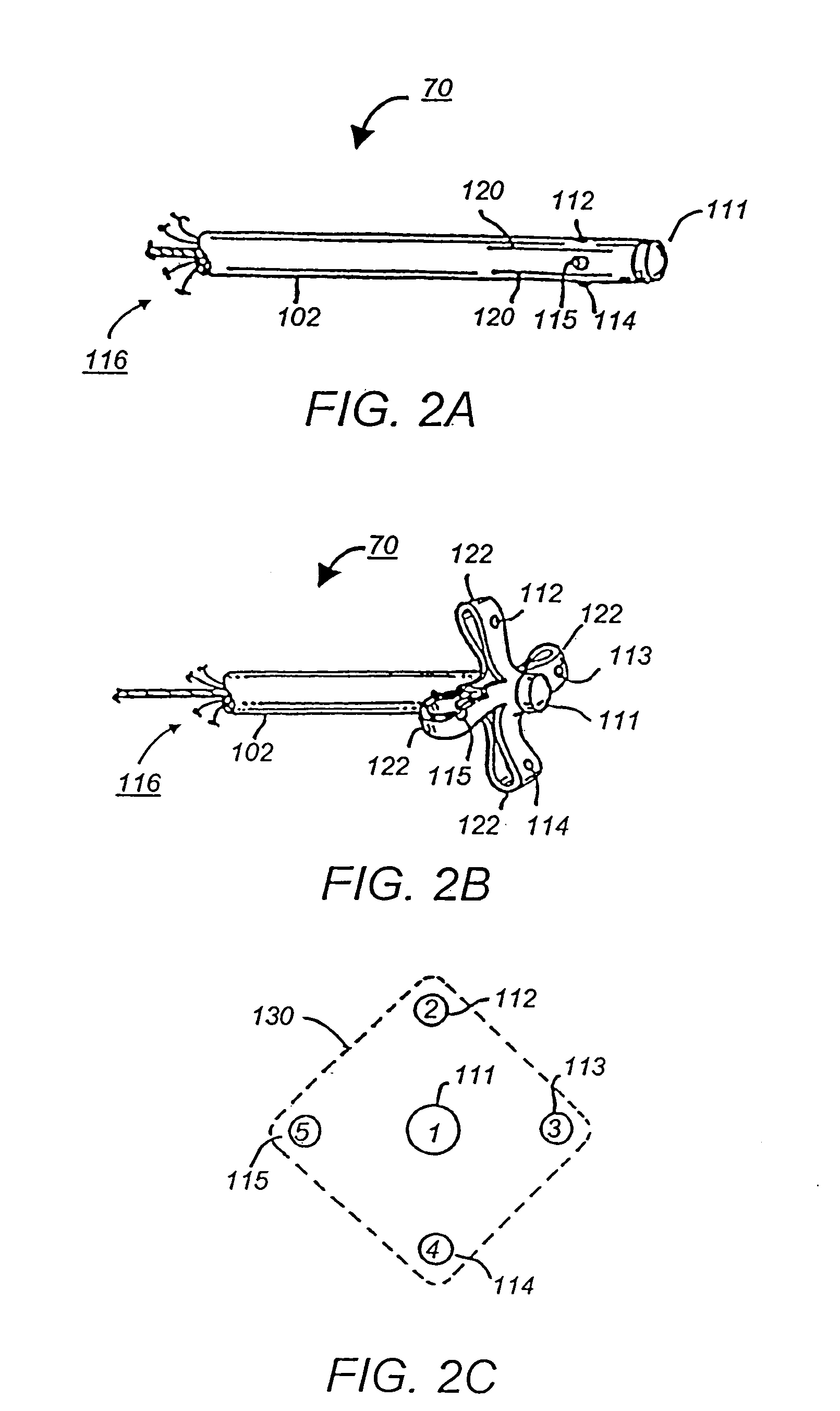
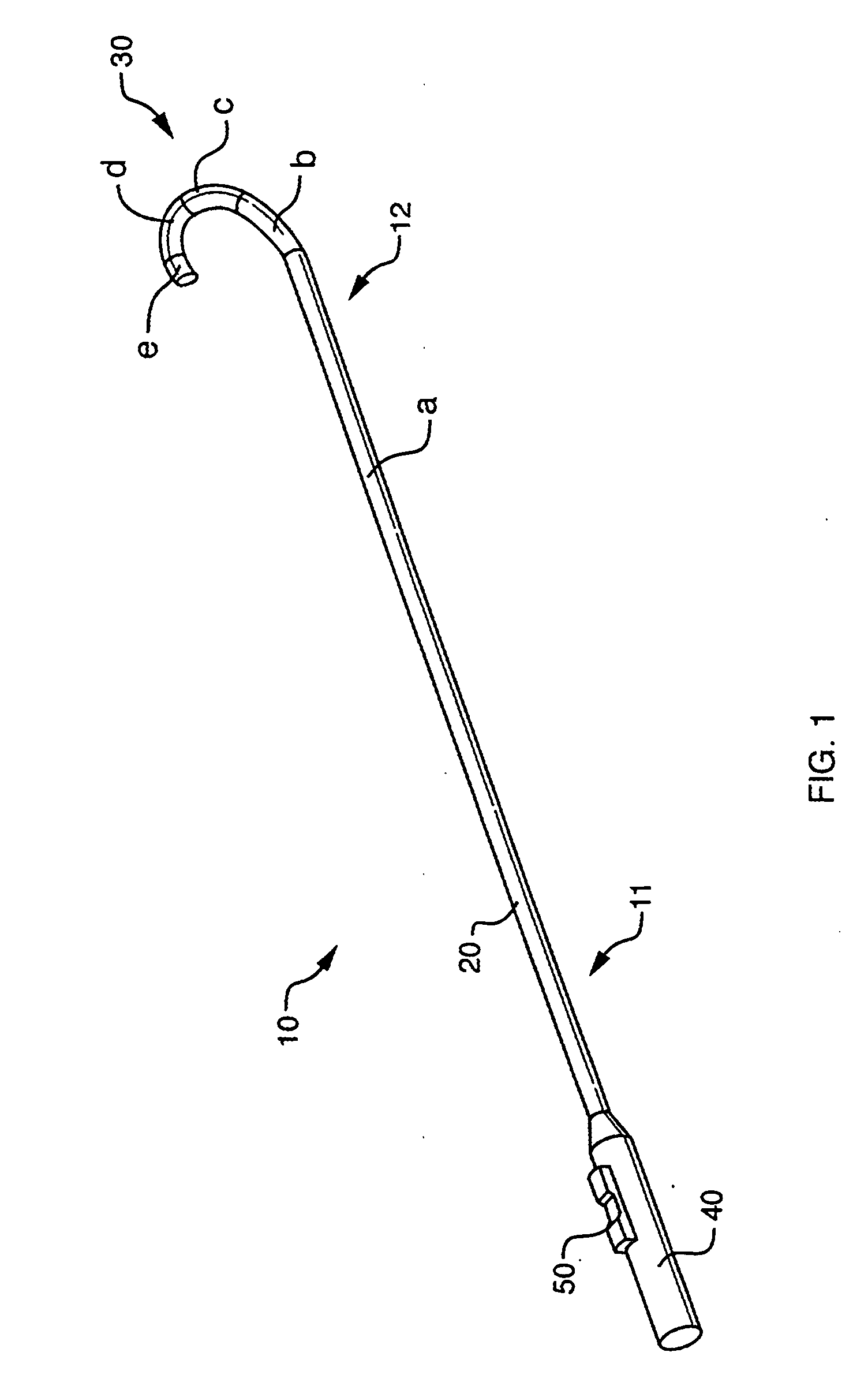
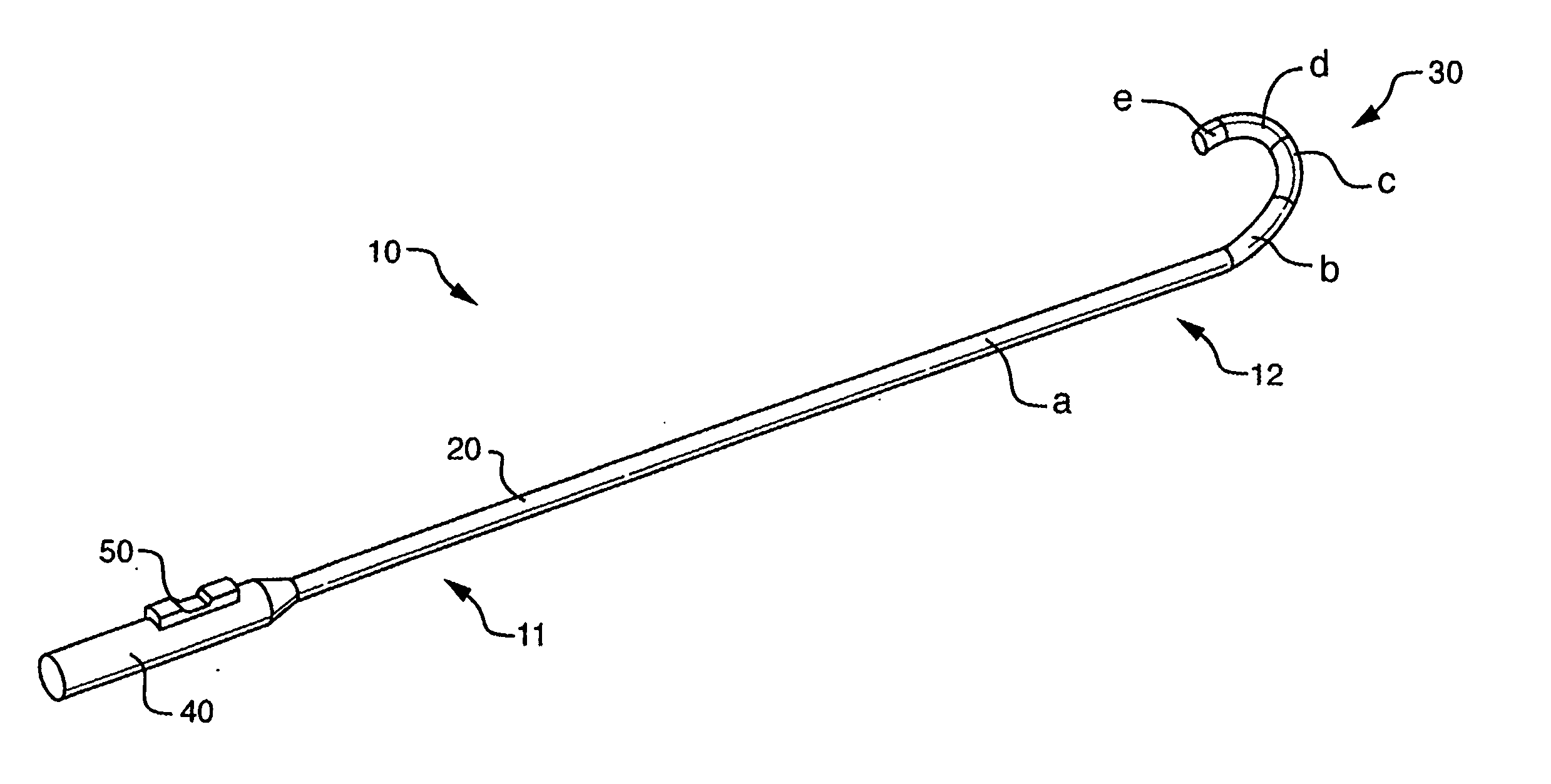
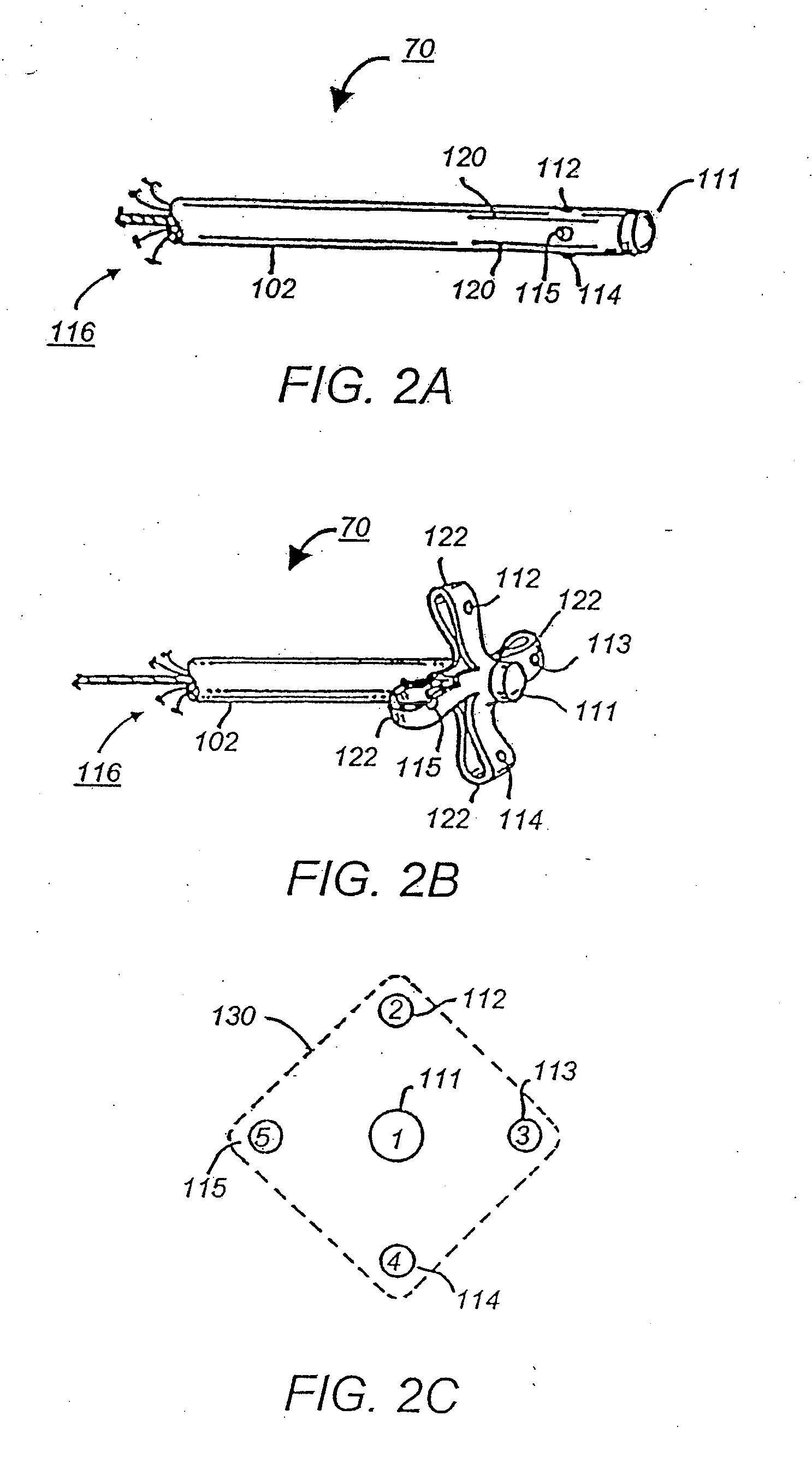
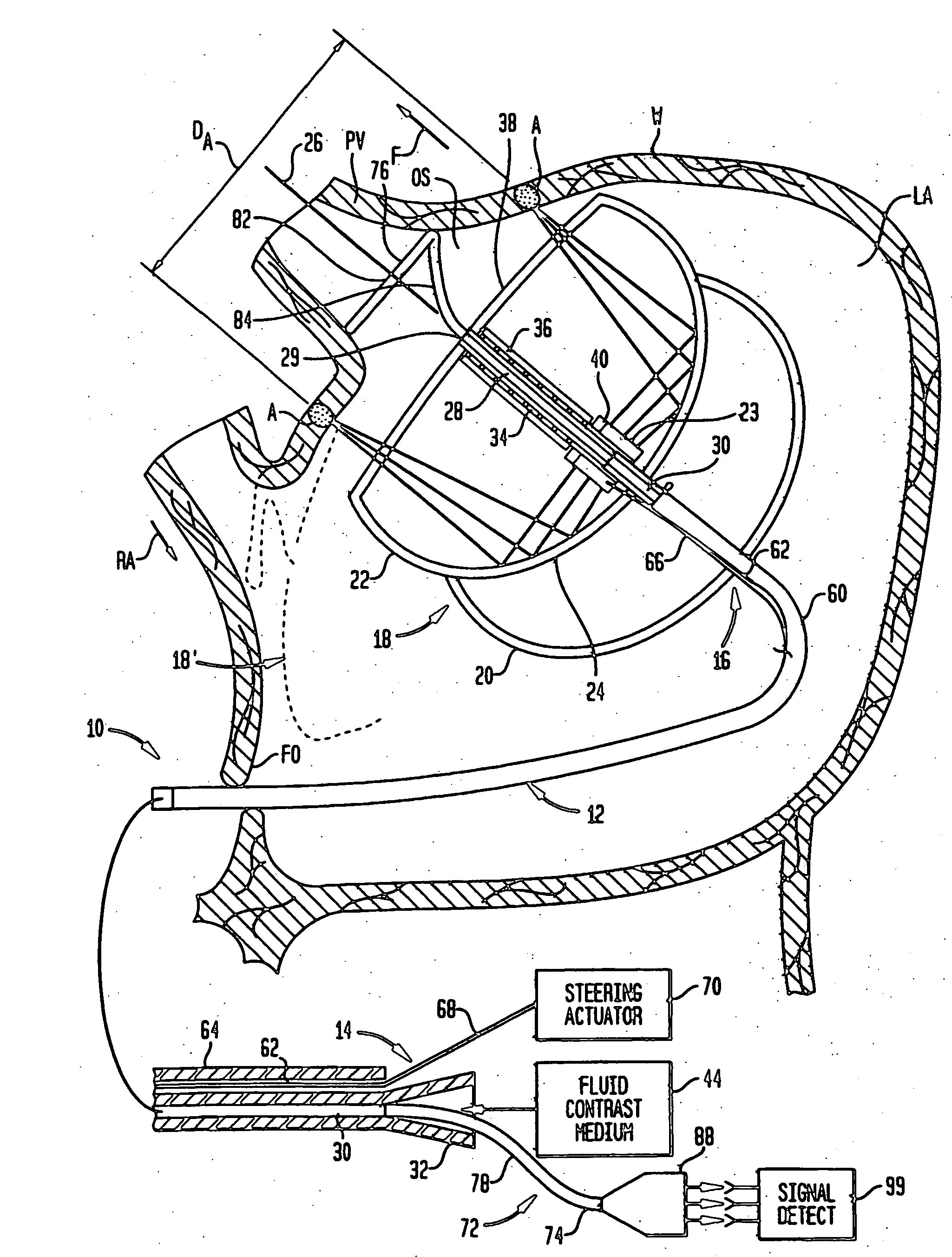
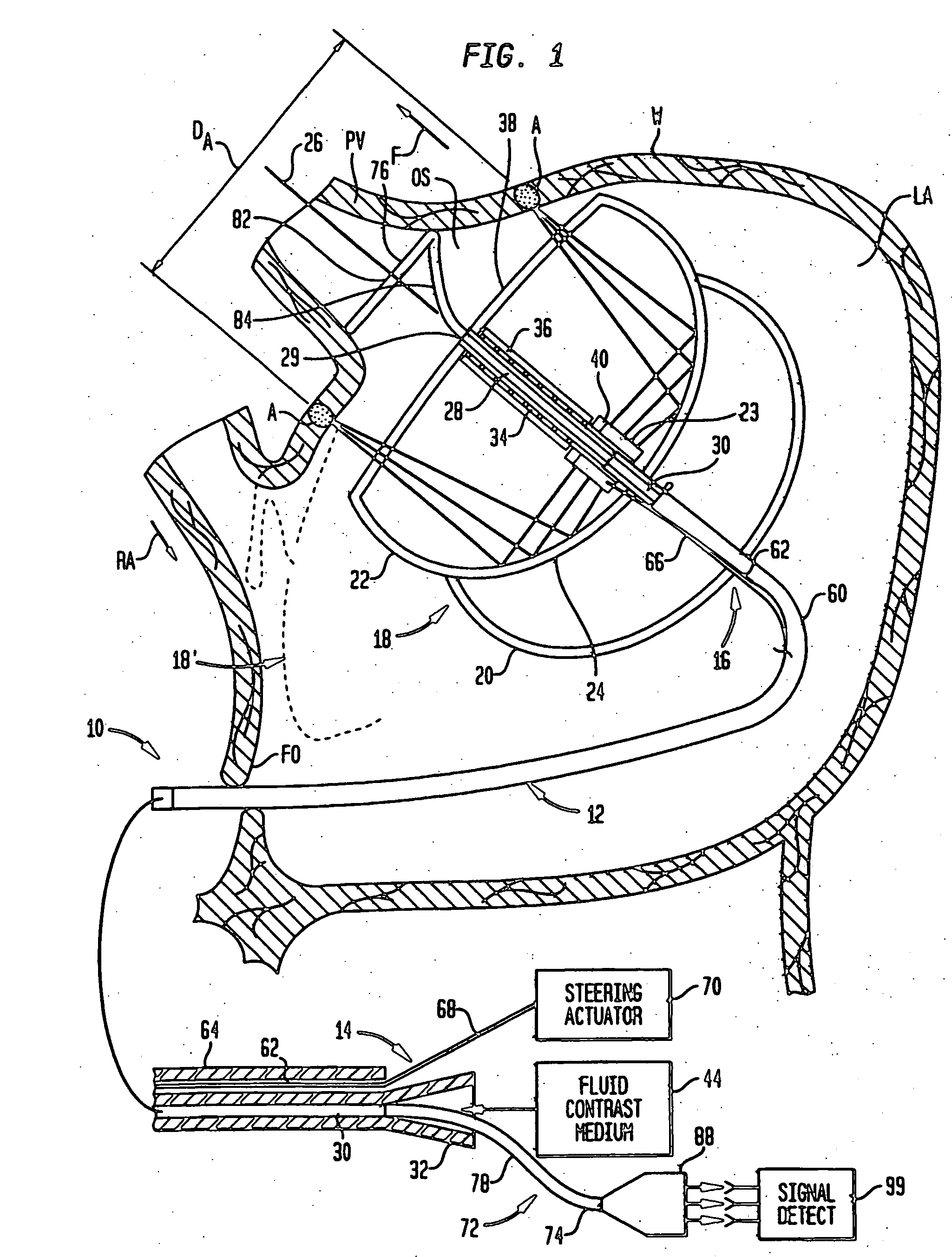
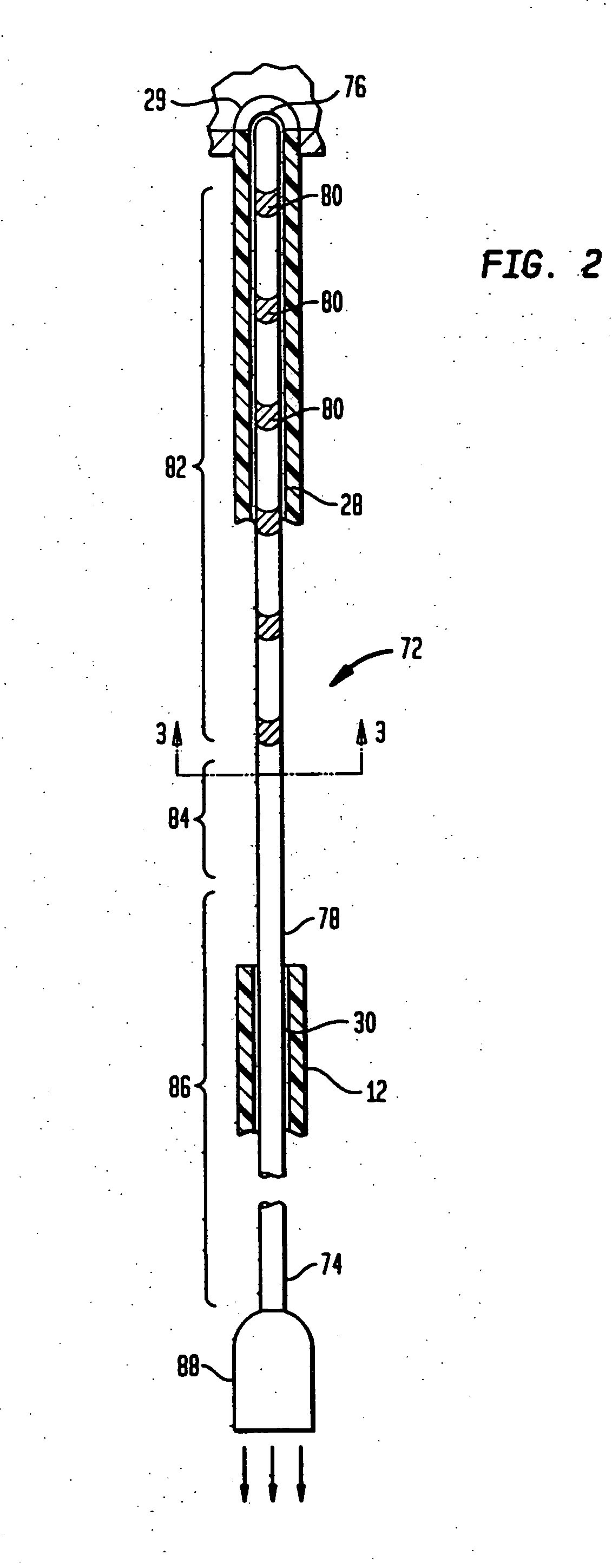
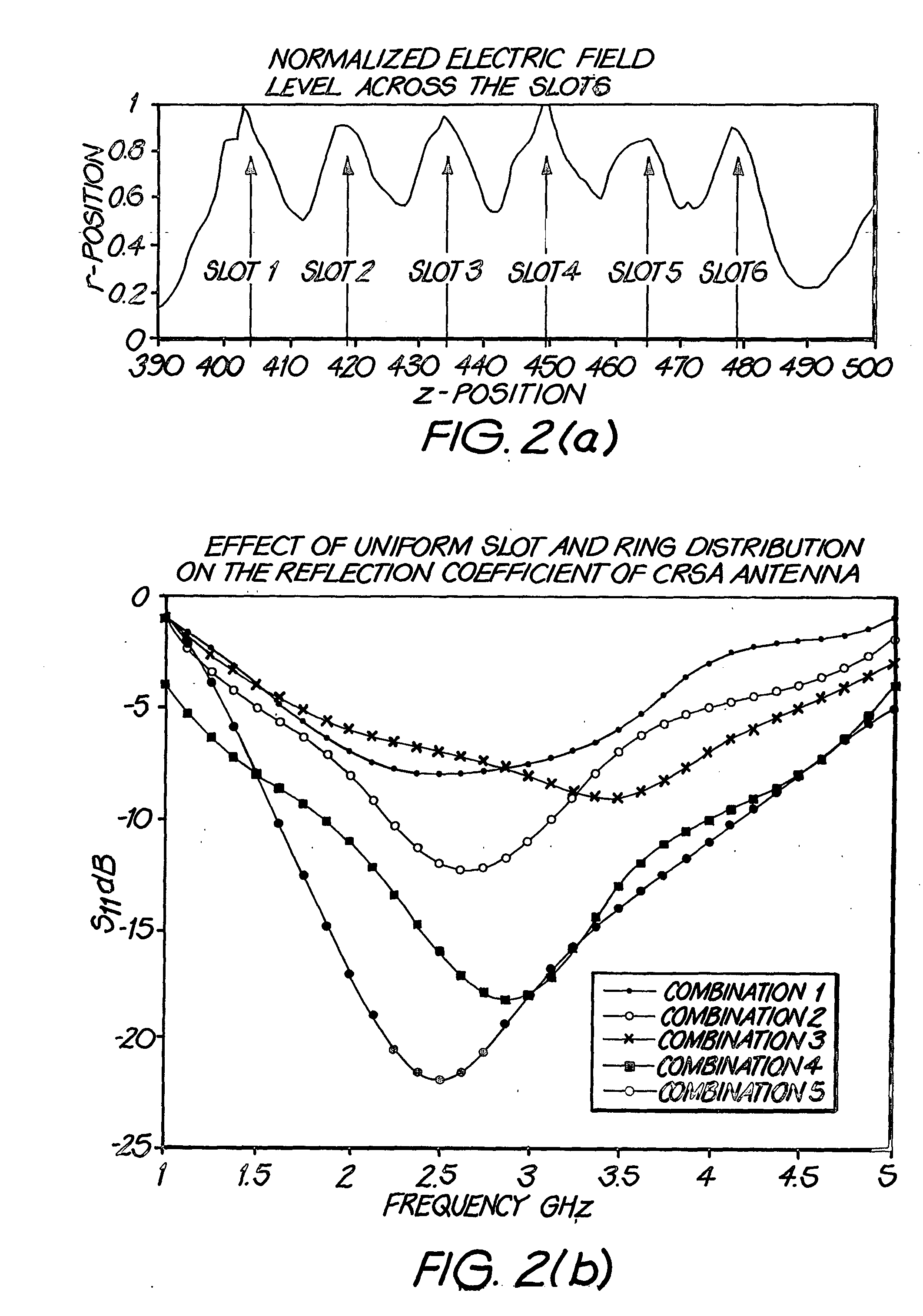
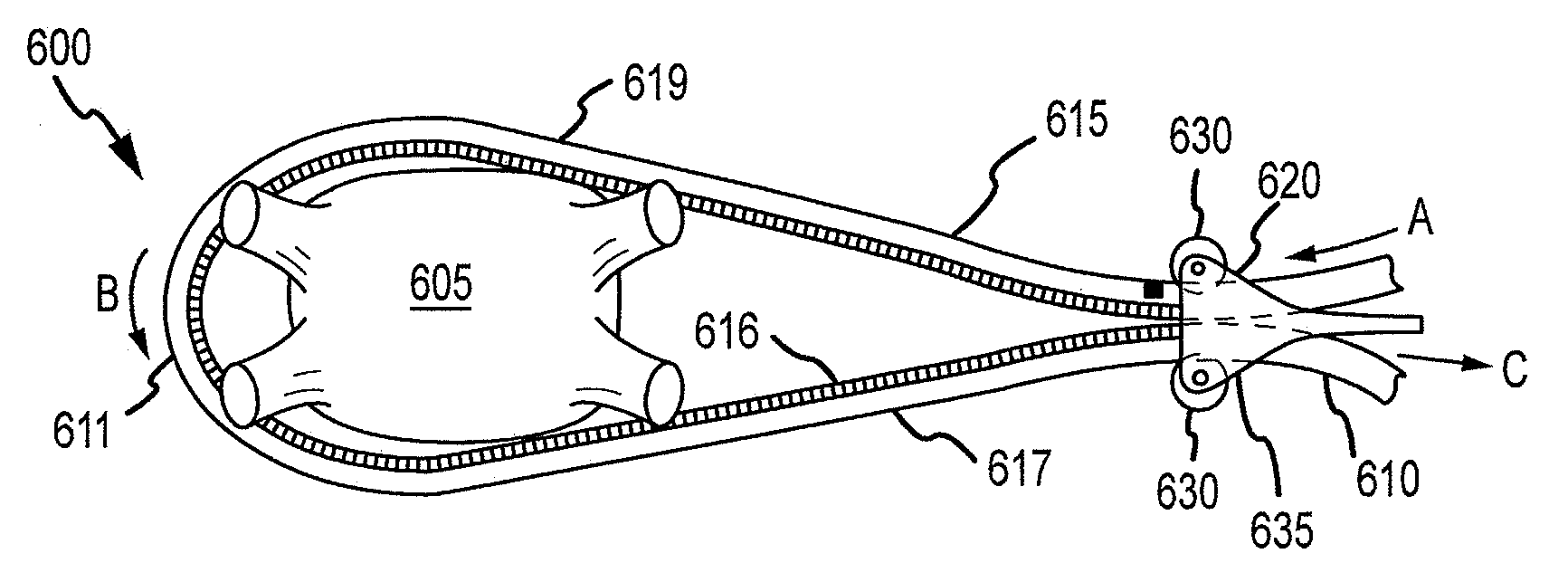
Ablation devices with sensor structures
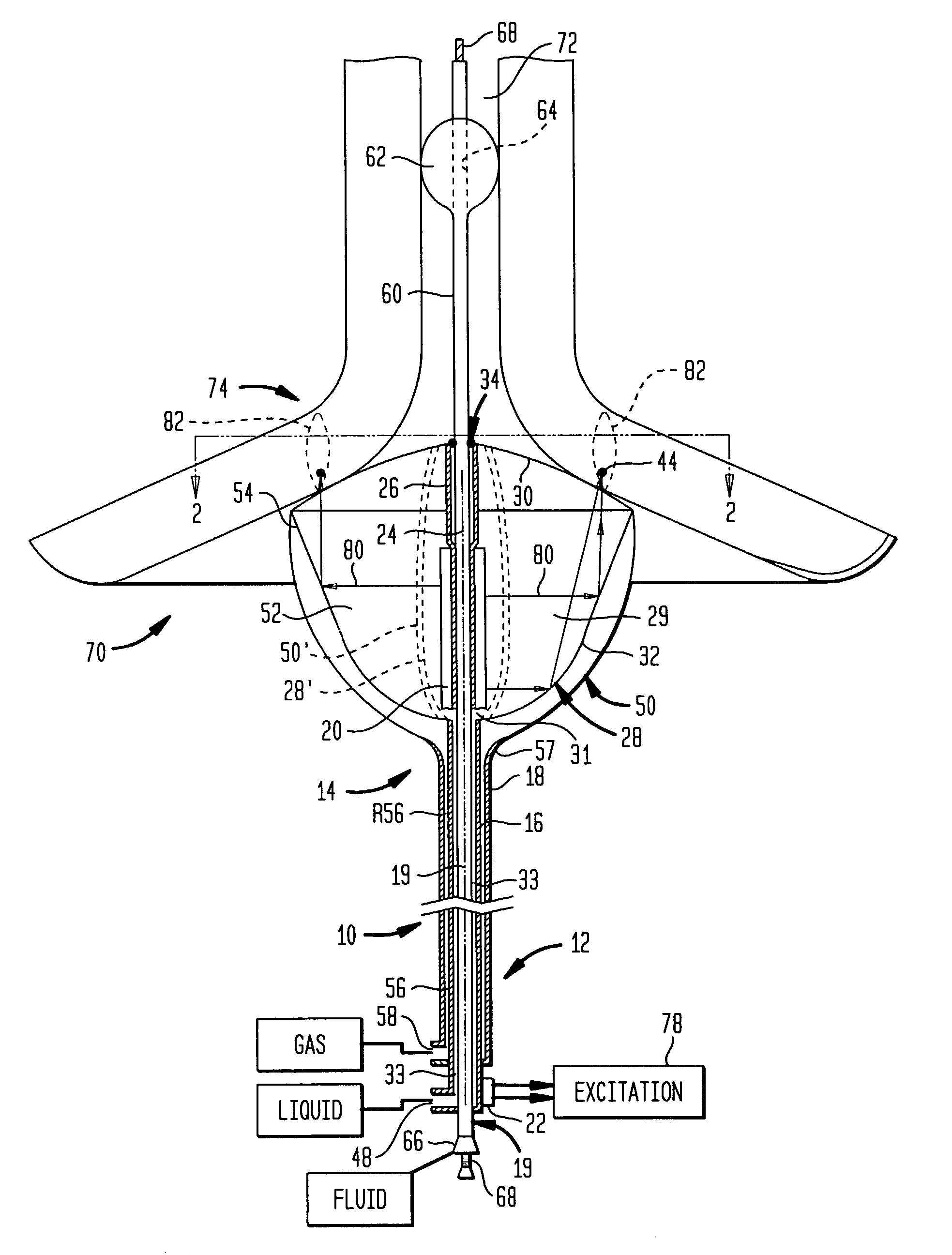
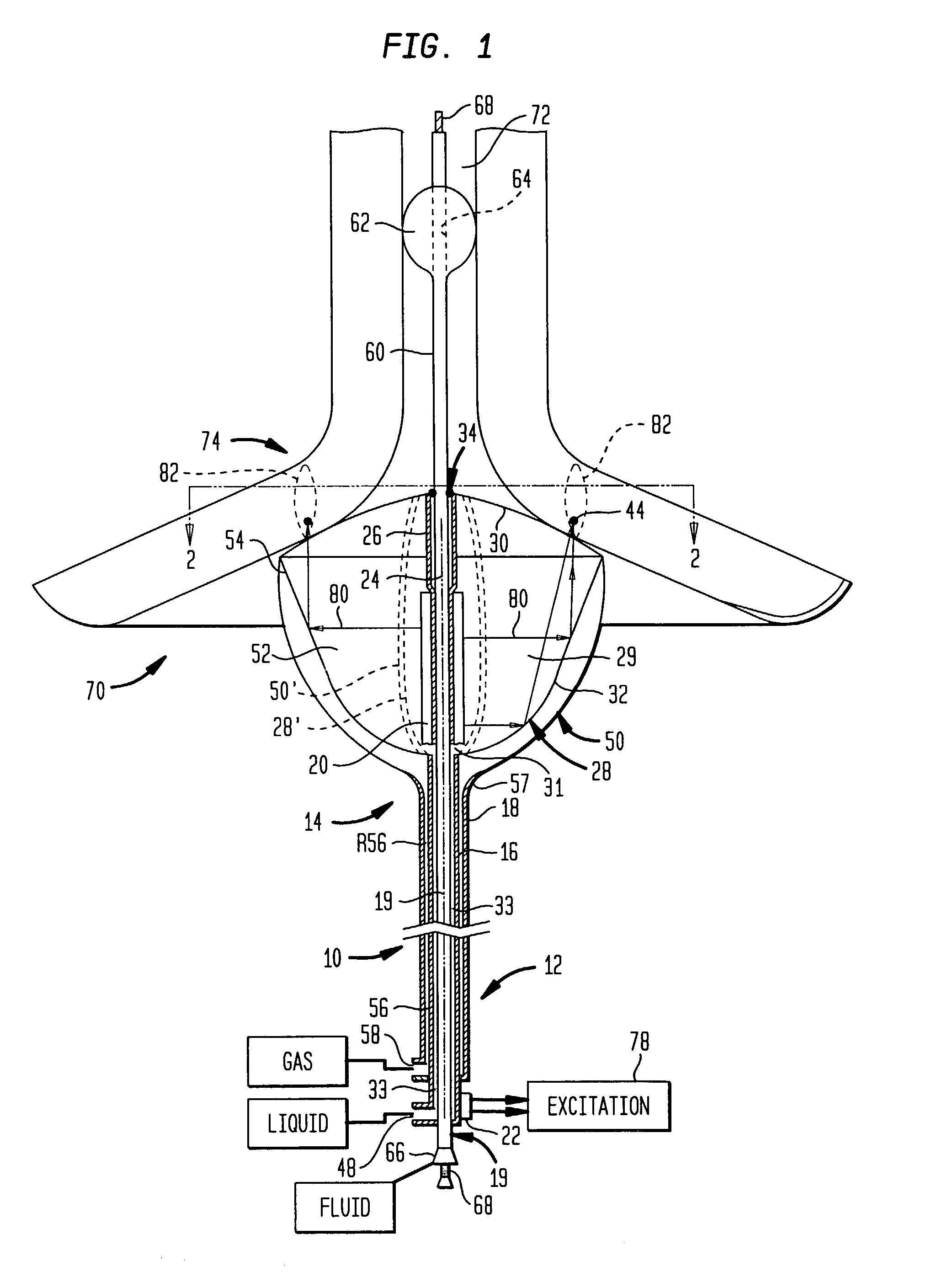
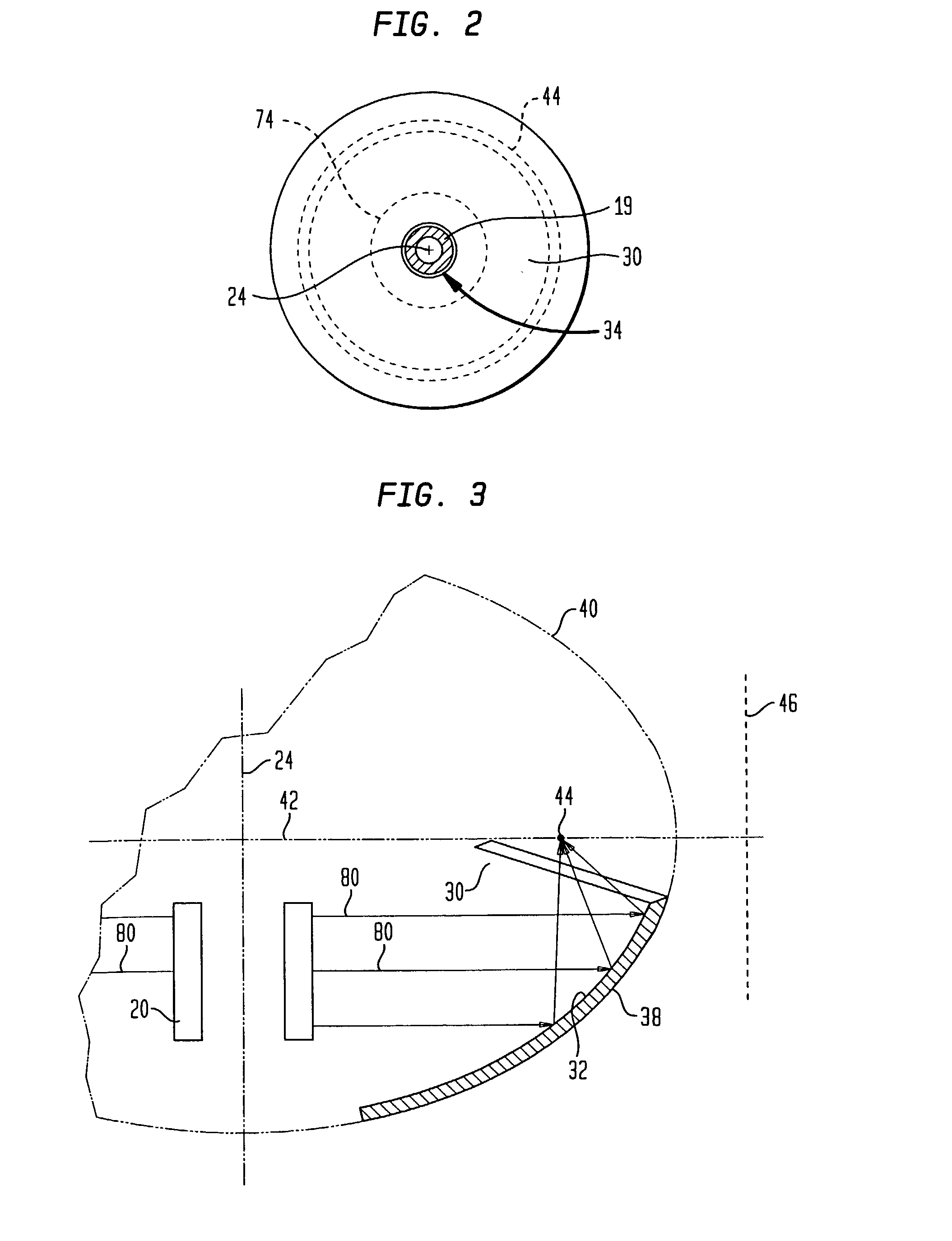
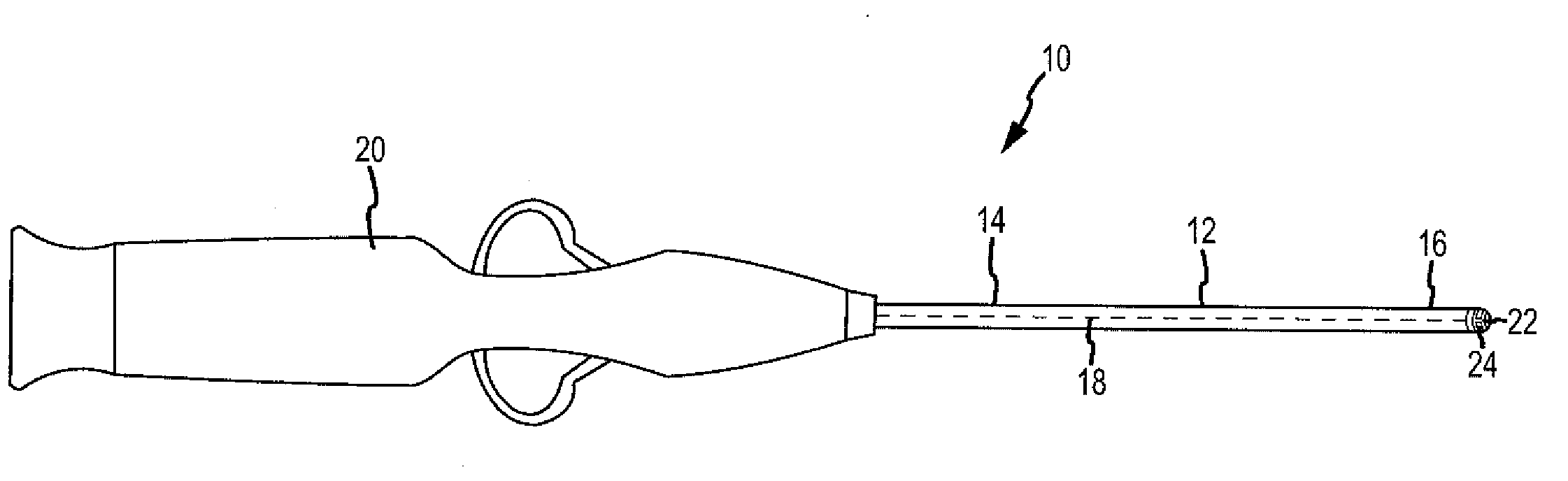
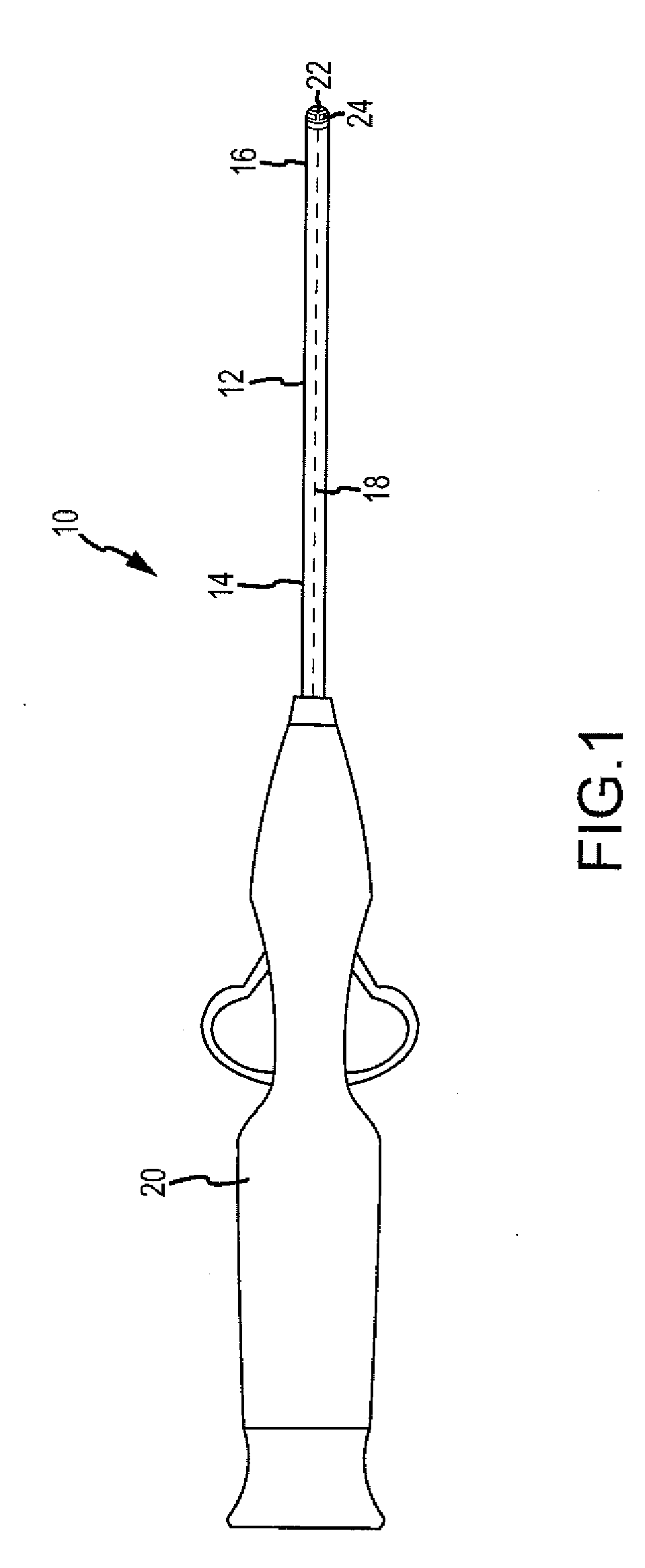
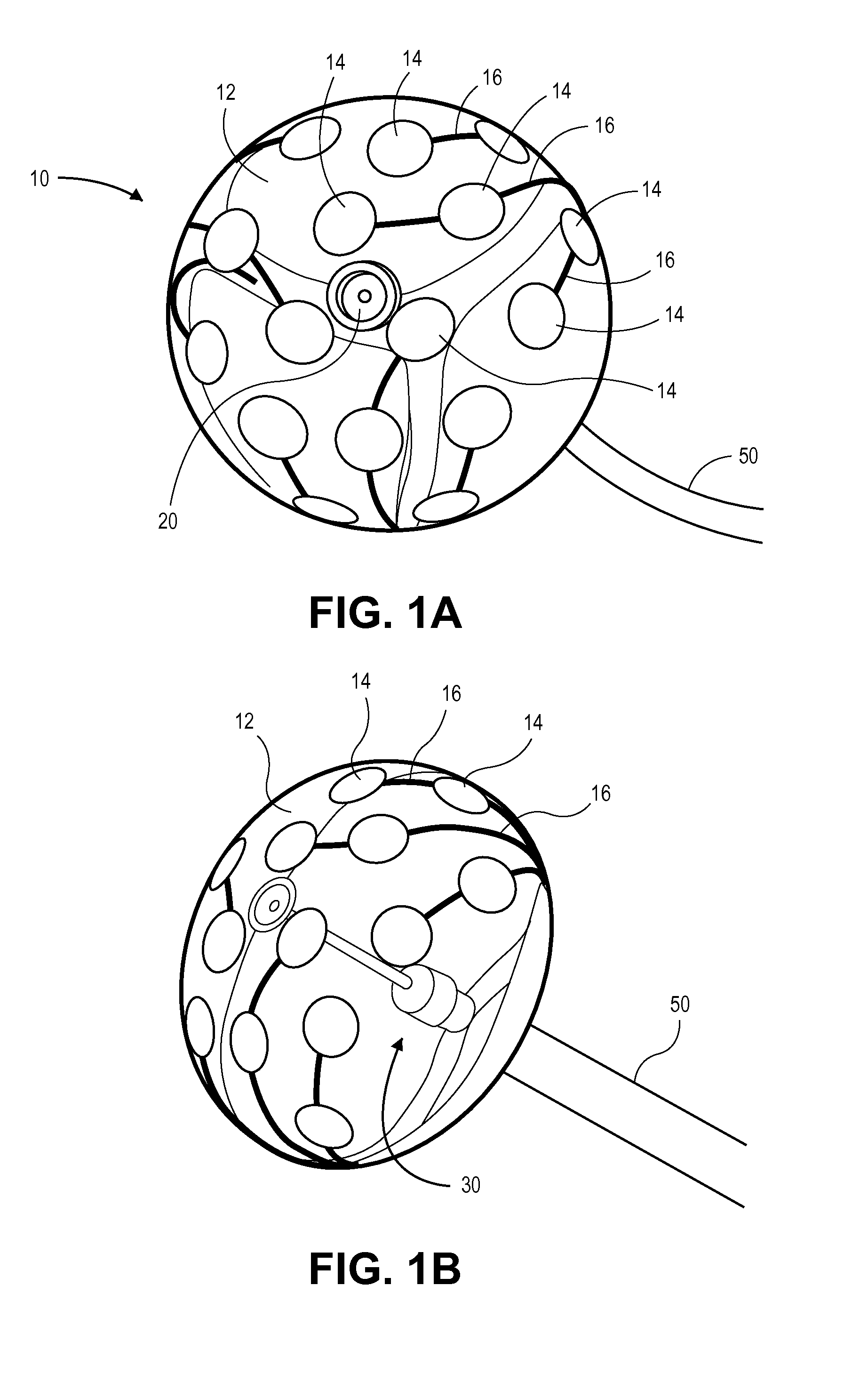
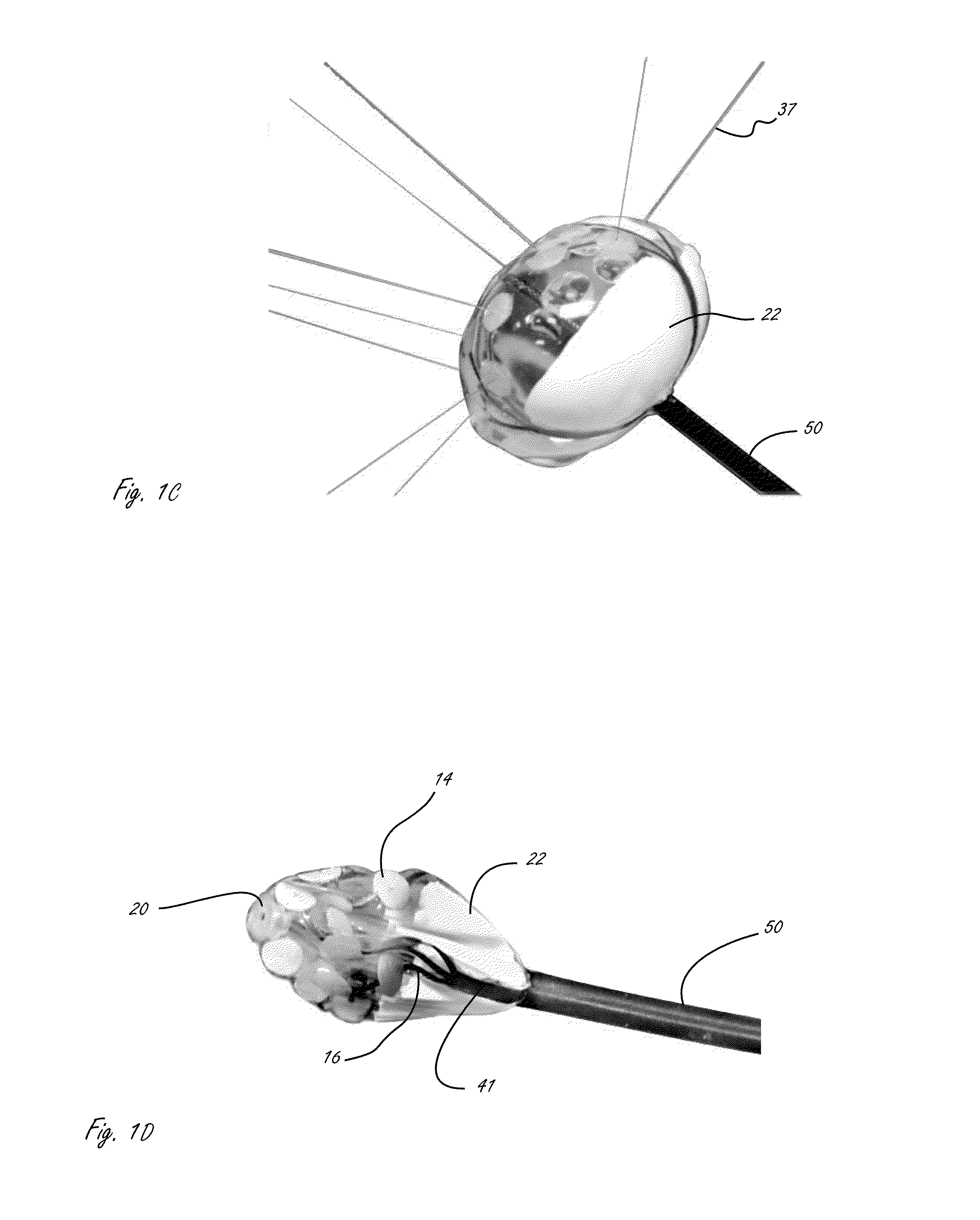
ActiveUS8216216B2Easy to introduceFor automatic alignmentUltrasound therapyDiagnostic recording/measuringCatheterCardiac Ablation
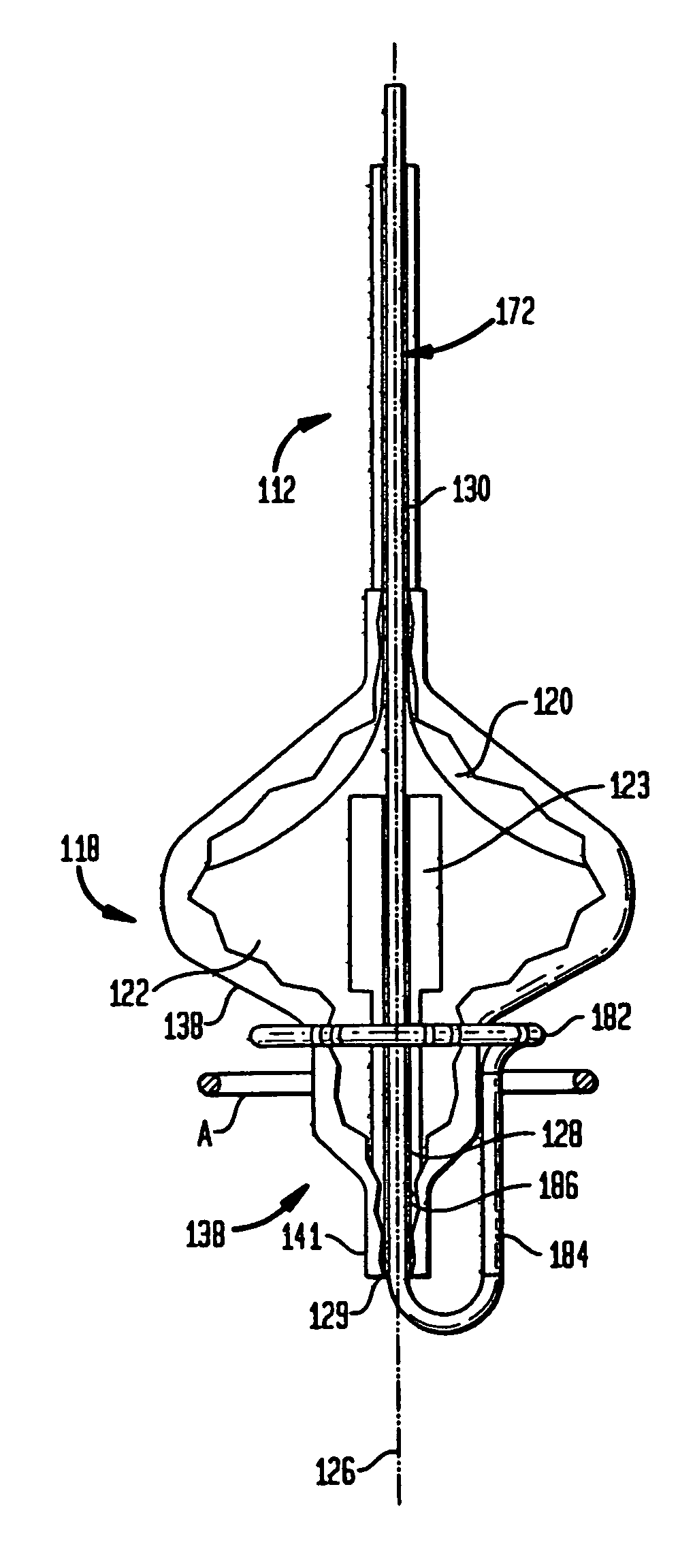
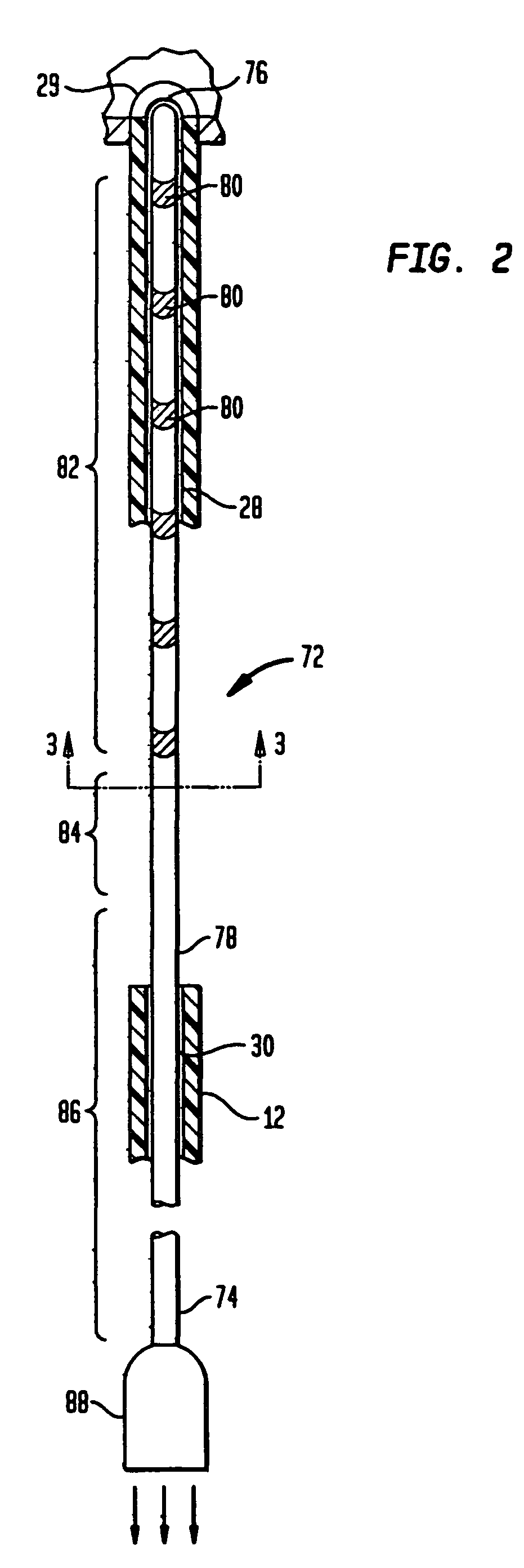
A cardiac ablation device, including a steerable catheter (10) and an expandable ablation element (18) incorporating one or more balloons (20, 22) at the distal end of the catheter, has a continuous passageway (28, 30) extending through it from the proximal end of the catheter to the distal side of the expandable ablation element. A probe (72) carrying electrodes is introduced through this passageway and deploys, under the influence of its own resilience, to a structure incorporating a loop (82) which is automatically aligned with the axis of the expandable ablation device, so that minimal manipulation is required to place the sensor probe.
Owner:BOSTON SCI SCIMED INC
Apparatus And Method For Cardiac Ablation
InactiveUS20070161915A1ElectrocardiographyControlling energy of instrumentVisual perceptionIntracardiac Electrogram
A system and method for cardiac mapping and ablation include a multi-electrode catheter introduced percutaneously into a subject's heart and deployable adjacent to various endocardial sites. The electrodes are connectable to a mapping unit, an ablation power unit a pacing unit, all of which are under computer control. Intracardiac electrogram signals emanated from a tachycardia site of origin are detectable by the electrodes. Their arrival times are processed to generate various visual maps to provide real-time guidance for steering the catheter to the tachycardia site of origin. In another aspect, the system also include a physical imaging system which is capable of providing different imaged physical views of the catheter and the heart. These physical views are incorporated into the various visual maps to provide a more physical representation. Once the electrodes are on top of the tachycardia site of origin, electrical energy is supplied by the ablation power unit to effect ablation.
Owner:CATHEFFECTS
Cardiac ablation catheters and methods of use thereof
Cardiac ablation catheters and methods of use. In some embodiments the catheter includes at least one camera inside an expandable membrane for visualizing an ablation procedure.
Owner:BOSTON SCI SCIMED INC
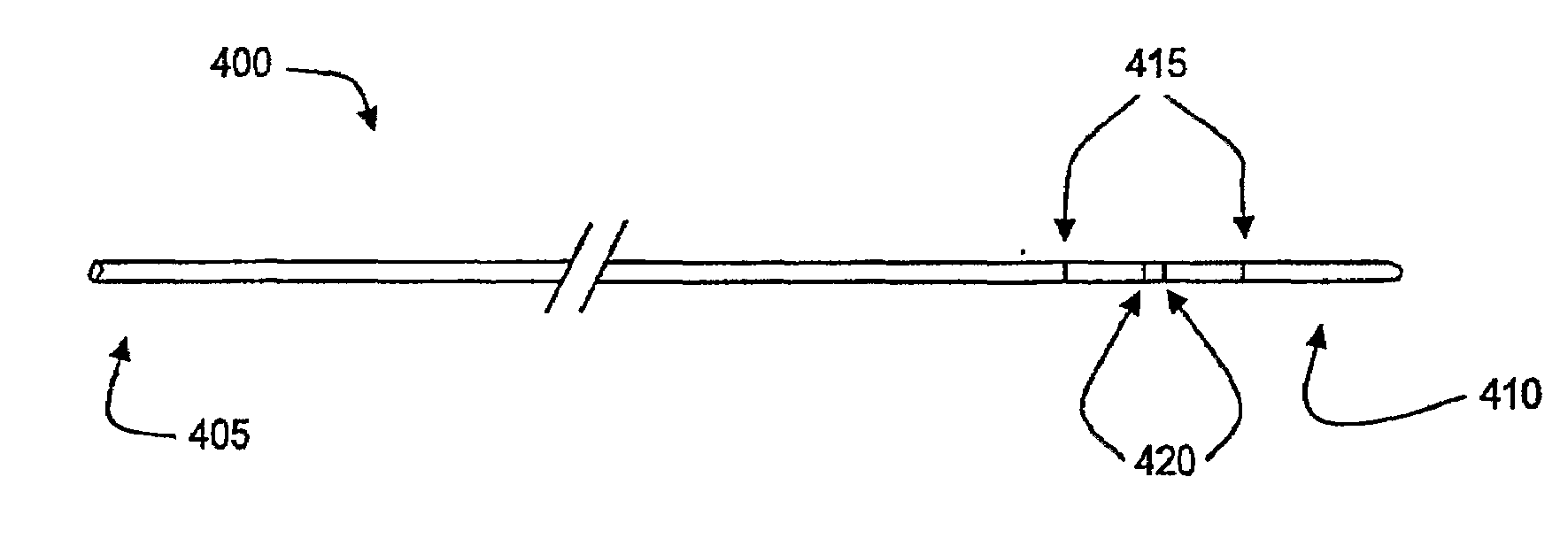
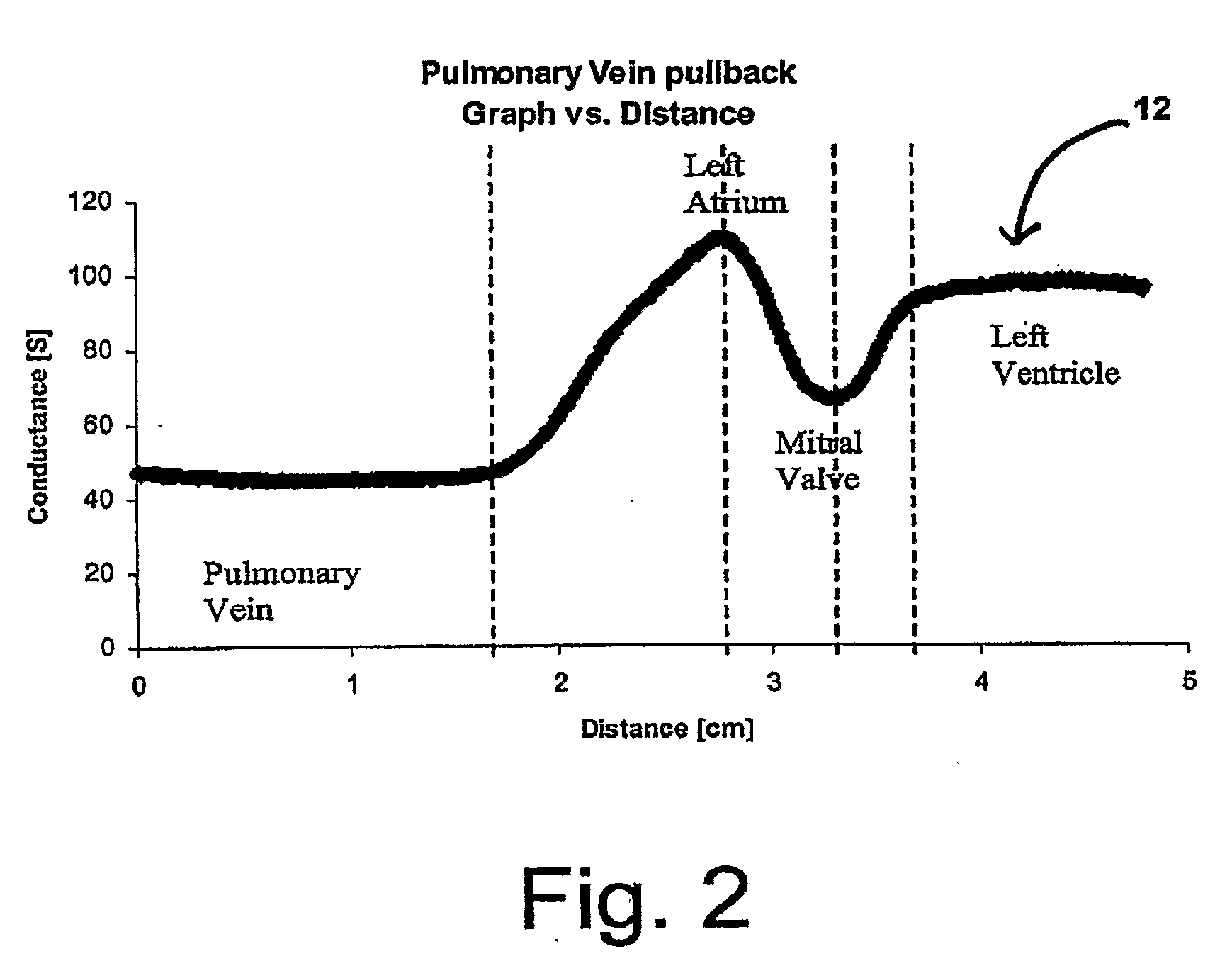
Localization of body lumen junctions
ActiveUS20090182287A1Improve spatial resolutionLower requirementElectrocardiographyCatheterBiomedical engineeringCardiac Ablation
Devices, systems, and methods for the localization of body lumen junctions and other intraluminal structure are disclosed. Various embodiments permit clinicians to identify the locations of intraluminal structures and medical devices during non-surgical medical techniques, such as cardiac ablation, by determining the intralumen conductance and / or cross-sectional area at a plurality of locations within the body lumen.
Owner:3DT HLDG
Ablation Devices with Sensor Structures
ActiveUS20080249518A1Easy to introduceFor automatic alignmentUltrasound therapyChiropractic devicesCardiac AblationBiomedical engineering
A cardiac ablation device, including a steerable catheter (10) and an expandable ablation element (18) incorporating one or more balloons (20, 22) at the distal end of the catheter, has a continuous passageway (28, 30) extending through it from the proximal end of the catheter to the distal side of the expandable ablation element. A probe (72) carrying electrodes is introduced through this passageway and deploys, under the influence of its own resilience, to a structure incorporating a loop (82) which is automatically aligned with the axis of the expandable ablation device, so that minimal manipulation is required to place the sensor probe.
Owner:BOSTON SCI SCIMED INC
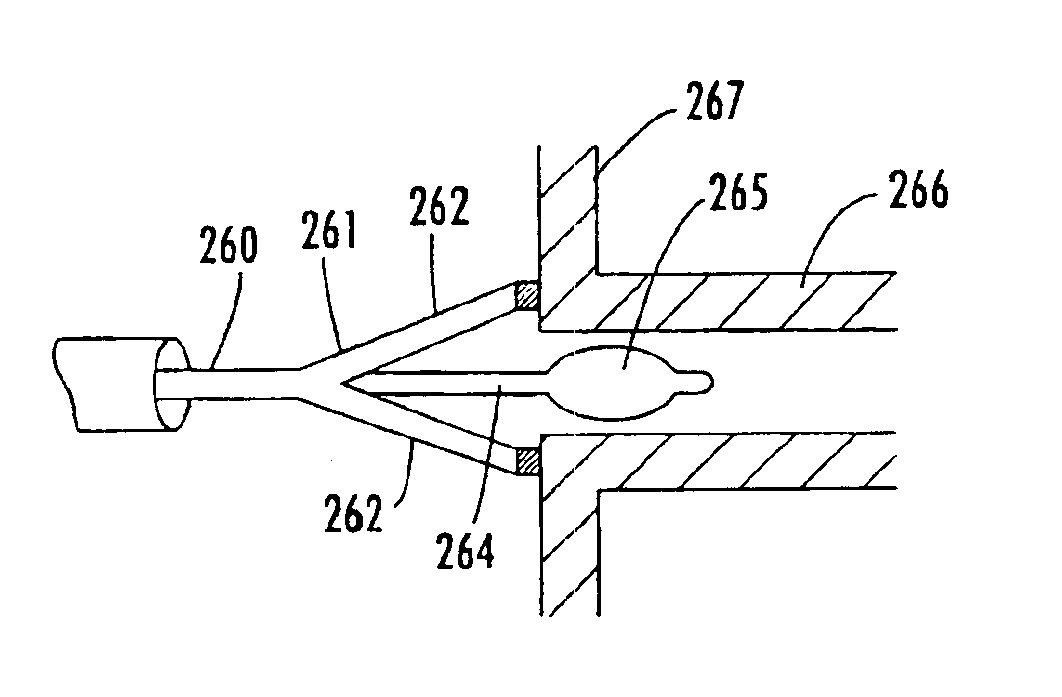
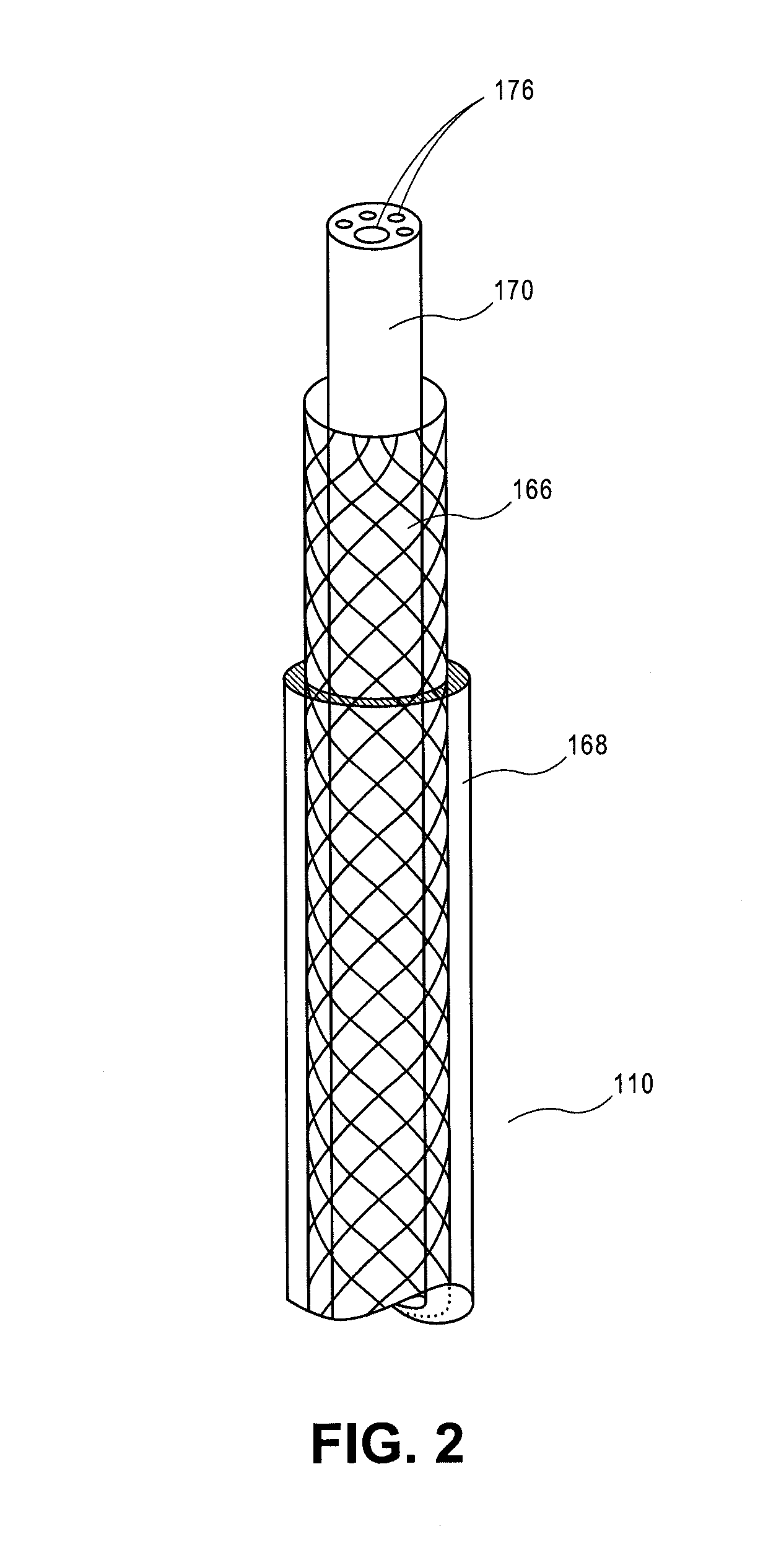
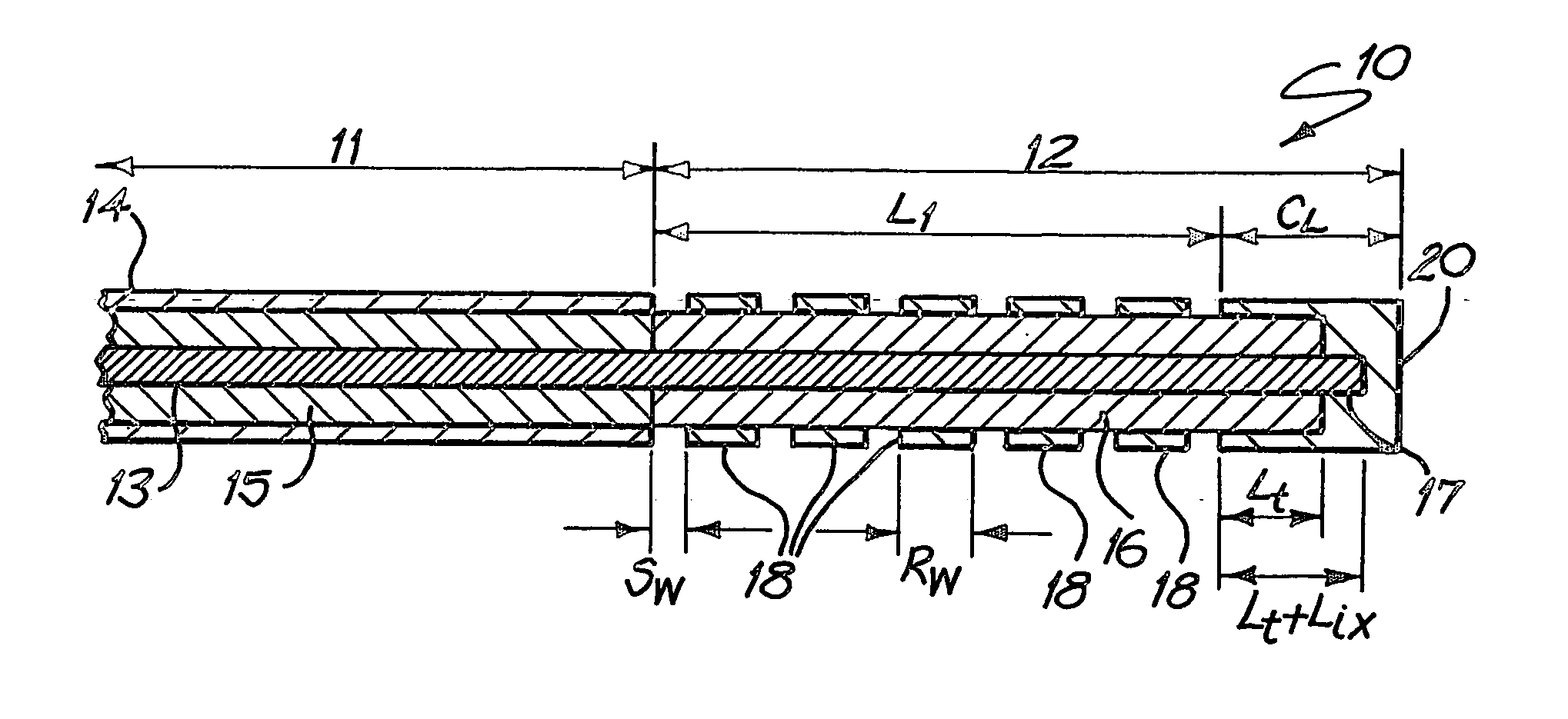
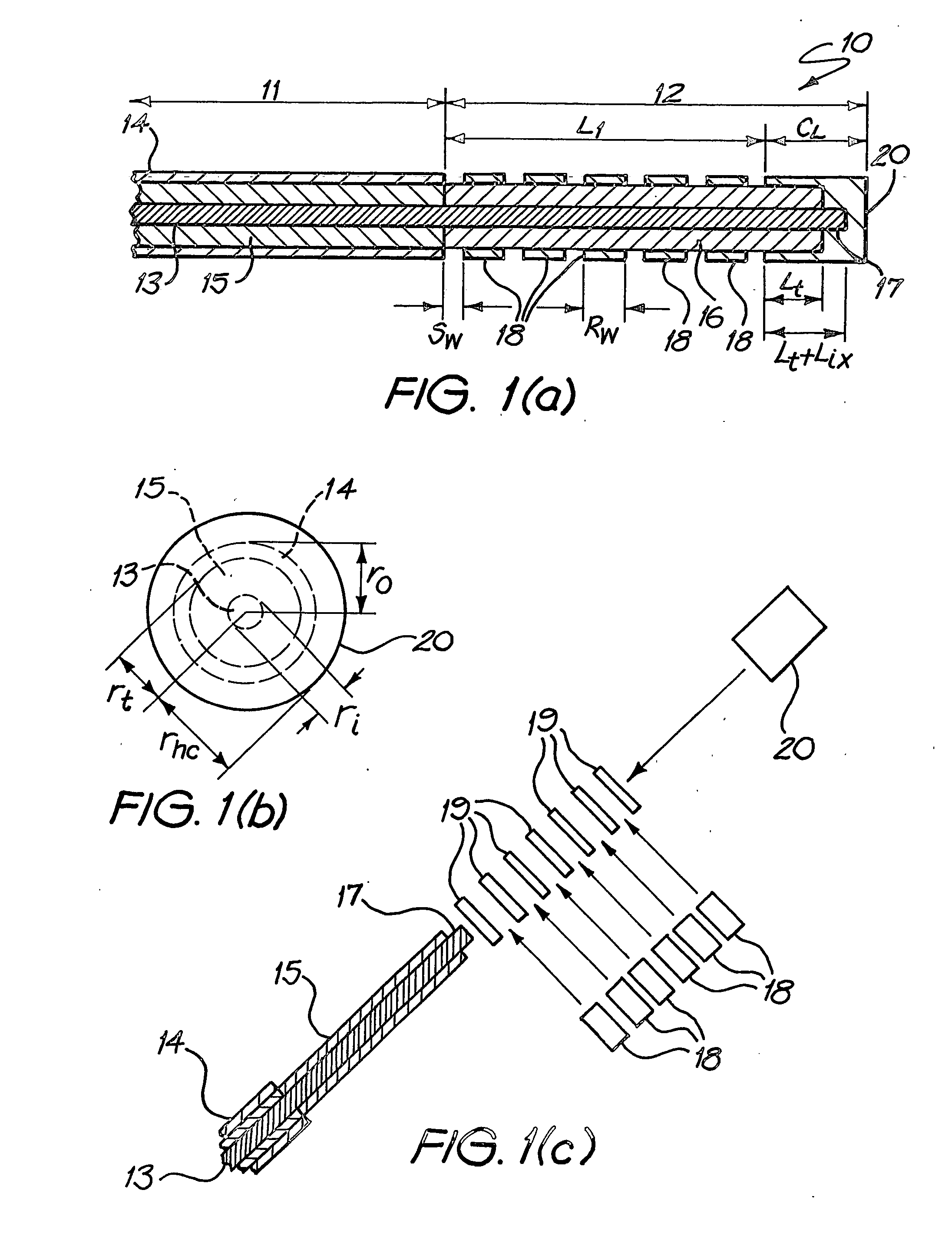
Microwave antenna for medical ablation
InactiveUS20060289528A1Increase powerMinimize reflectionCatheterMicrowave therapyElectrical conductorMicrowave
A microwave antenna suitable for cardiac ablation, in particular for catheter ablation, and a method for making such an antenna. The antenna comprises a transmission line having an inner conductor, an outer conductor, and a dielectric insulator to provide insulation between the inner and outer conductors. An energy emitting antenna element is located at the distal end of the transmission line. The antenna element has an inner conductor which is electrically coupled to the inner conductor of the transmission line, and, around the inner conductor, a sheath of dielectric insulator continuous with the insulator of the transmission line. At its distal end, a hollow metallic cap is electrically connected to the inner conductor, surrounding a length of the insulator.
Owner:UNIV OF TECH SYDNEY +1
Methods for ablation with radiant energy
InactiveUS20060253113A1Rapid and efficient creationRapid and effective photoablationStentsUltrasound therapyCoaxial catheterTarget tissue
Ablation methods and instruments are disclosed for creating lesions in tissue, especially cardiac tissue for treatment of arrhythmias and the like. Percutaneous ablation instruments in the form of coaxial catheter bodies are disclosed having at least one central lumen therein and having one or more balloon structures at the distal end region of the instrument. The instruments include an energy emitting element which is independently positionable within the lumen of the instrument and adapted to project radiant energy through a transmissive region of a projection balloon to a target tissue site. The instrument can optionally include at least one expandable anchor balloon disposed about, or incorporated into an inner catheter body designed to be slid over a guidewire. This anchor balloon can serve to position the device within a lumen, such as a pulmonary vein. A projection balloon structure is also disclosed that can be slid over the first (anchor balloon) catheter body and inflated within the heart, to define a staging from which to project radiant energy. An ablative fluid can also be employed outside of the instrument (e.g., between the balloon and the target region) to ensure efficient transmission of the radiant energy when the instrument is deployed. In another aspect of the invention, generally applicable to a wide range of cardiac ablation instruments, mechanisms are disclosed for determining whether the instrument has been properly seated within the heart, e.g., whether the device is in contact with a pulmonary vein and / or the atrial surface, in order to form a lesion by heating, cooling or projecting energy. This contact-sensing feature can be implemented by an illumination source situated within the instrument and an optical detector that monitors the level of reflected light. Measurements of the reflected light (or wavelengths of the reflected light) can thus be used to determine whether contact has been achieved and whether such contact is continuous over a desired ablation path.
Owner:CARDIOFOCUS INC
Catheter assembly with front-loaded tip and multi-contact connector
ActiveUS20090306655A1Minimizes and eliminates traumaLess traumaElectrocardiographyCatheterCardiac AblationElectrical connector
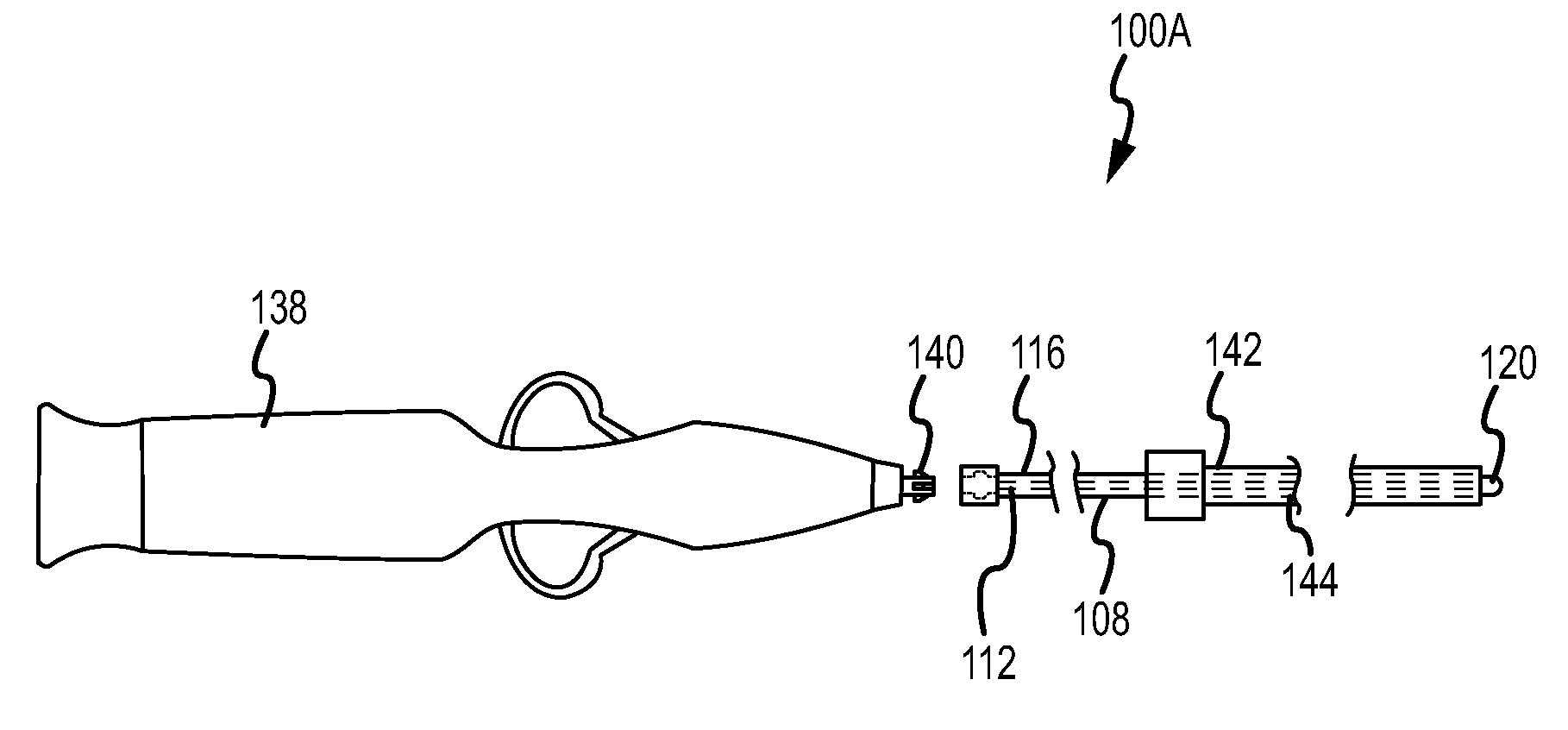
The invention is directed to a catheter suitable for medical procedures such as cardiac ablation. The catheter includes a front-loaded catheter tip with an electrically active element. The catheter can include an elongate catheter shaft assembly having an inner shaft member with a distal end and a proximal end, and an outer shaft member with a distal end, a proximal end, and a lumen between the distal end and the proximal end. The inner shaft member can be inserted into the lumen of the outer shaft member along a longitudinal direction. The inner shaft member can include, at the distal end, a catheter tip member having a lateral dimension that is larger than a lateral dimension of the lumen of the outer shaft member. The catheter tip member includes at least one electrically active element, and the proximal end of the inner shaft member has at least one electrode disposed on the external surface of the shaft member, such that when inserted into a handle, the electrode electrically contacts an electrical connector element.
Owner:ST JUDE MEDICAL ATRIAL FIBRILLATION DIV
Balloon for ablation around pulmonary veins
PendingUS20160175041A1Simple procedureDiagnostic recording/measuringSensorsVeinPulmonary vein ablation
Cardiac ablation is carried out by introducing a catheter into the left atrium, extending a lasso guide through the lumen of the catheter to engage the wall of a pulmonary vein, and deploying a balloon over the lasso guide. The balloon has an electrode assembly disposed its exterior. The electrode assembly includes a plurality of ablation electrodes circumferentially arranged about the longitudinal axis of the catheter. The inflated balloon is positioned against the pulmonary vein ostium, so that the ablation electrodes are in galvanic contact with the pulmonary vein, and electrical energy is conducted through the ablation electrodes to produce a circumferential lesion that circumscribes the pulmonary vein.
Owner:BIOSENSE WEBSTER (ISRAEL) LTD
Catheter with cryogenic and electrical heating ablation
InactiveUS20060004351A1Reduce tip temperatureReduce movement sequenceCatheterDiagnostic recording/measuringTissue remodelingCelsius Degree
A catheter includes a cryoablation tip with an electrically-driven ablation assembly for heating tissue. The cryoablation tip may be implemented with a cooling chamber through which a controllably injected coolant circulates to lower the tip temperature, and having an RF electrode at its distal end. The RF electrode may be operated to warm cryogenically-cooled tissue, or the coolant may be controlled to conductively cool the tissue in coordination with an RF treatment regimen, allowing greater versatility of operation and enhancing the lesion size, speed or placement of multi-lesion treatment or single lesion re-treatment cycles. In one embodiment a microwave energy source operates at a frequency to extend beyond the thermal conduction depth, or to penetrate the cryogenic ice ball and be absorbed in tissue beyond an ice boundary, thus extending the depth and / or width of a single treatment locus. In another embodiment, the cooling and the application of RF energy are both controlled to position the ablation region away from the surface contacted by the electrode, for example to leave surface tissue unharmed while ablating at depth or to provide an ablation band of greater uniformity with increasing depth. The driver or RF energy source may supply microwave energy at a frequency effective to penetrate the ice ball which develops on a cryocatheter, and different frequencies may be selected for preferential absorption in a layer of defined thickness at depth in the nearby tissue. The catheter may operate between 70 and minus 70 degrees Celsius for different tissue applications, such as angioplasty, cardiac ablation and tissue remodeling, and may preset the temperature of the tip or adjacent tissue, and otherwise overlay or delay the two different profiles to tailor the shape or position where ablation occurs or to speed up a treatment cycle.
Owner:MEDTRONIC CRYOCATH LP
Cardiac ablation systems and methods
ActiveUS20090048591A1Rapid and effective ablative lesionEasy to adjust the lengthSurgical instruments for heatingCardiac AblationBiomedical engineering
Cardiac ablation systems and methods of their use and manufacture involve an ablation mechanism, a stabilizer mechanism, and a cinching mechanism that urges the ablation mechanism toward a patient tissue. Embodiments encompass methods for administering epicardial and endocardial lesions, including box lesions and connecting lesions, to patient tissue.
Owner:ATRICURE +1
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com