System and method for repairing tendons and ligaments
a technology for tendons and ligaments, applied in the field of surgical repair of torn tendons and ligaments, can solve the problems of 20-60% of rotator cuff repairs fail, and excess material or insufficient strength, etc., to achieve minimal detrimental tissue response during absorption, relieve the load of a tendon, and absorb over long periods of time
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
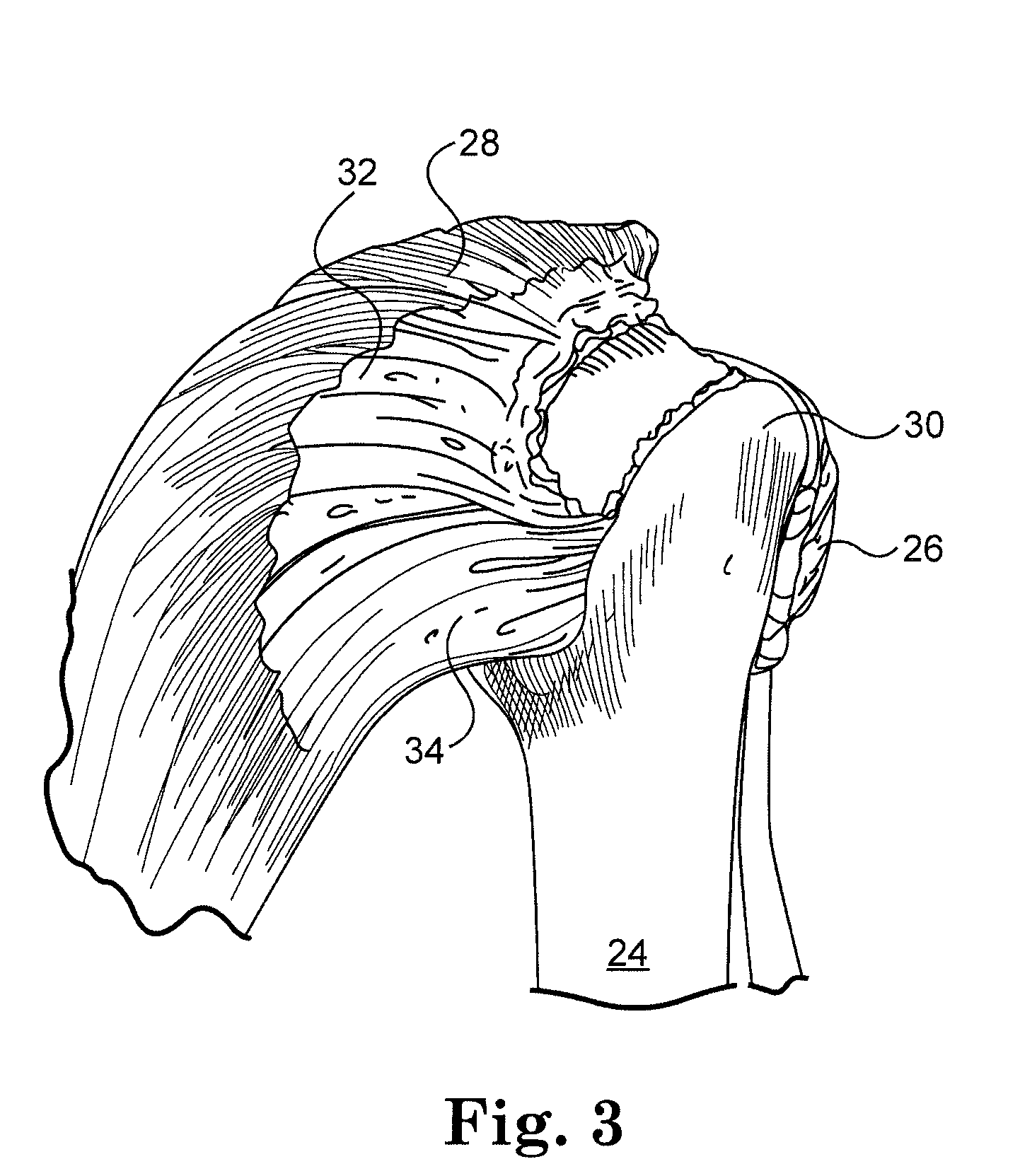
[0077]The present method and apparatus can be used to repair and reconstruct torn ligaments and tendons in a variety of locations of the body. The rotator cuff muscles were selected for the exemplary embodiments because of the complexity of the human shoulder. It will be appreciated that the following method and apparatus has many other possible applications.
[0078]FIG. 6 shows a bioabsorbable implant 70 made from a patch material 72 in accordance with an embodiment of the present invention. Implant 70 includes first and second edges 74, 76, and first and second side edges 78, 80. In a rotator cuff application, the implant 70 includes lateral edge 74, medial edge 76, anterior edge 78, and posterior 80 edges. The lateral edge (i.e., first edge) 74 and medial edge (i.e., second edge) 76 are preferably reinforced to facilitate attachment. The anterior 78 and posterior edges 80 (i.e., the side edges) are also optionally reinforced.
[0079]In some embodiments the anterior and posterior edge...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com