System of preoperative planning and provision of patient-specific surgical aids
a preoperative planning and patient-specific technology, applied in the field of preoperative planning system, can solve the problems of difficult to palpate boney landmarks, may be difficult to implant,/b> may not enable desired shoulder function, and surgeons cannot always readily determine whether even a remodeled glenoid vault can be used
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
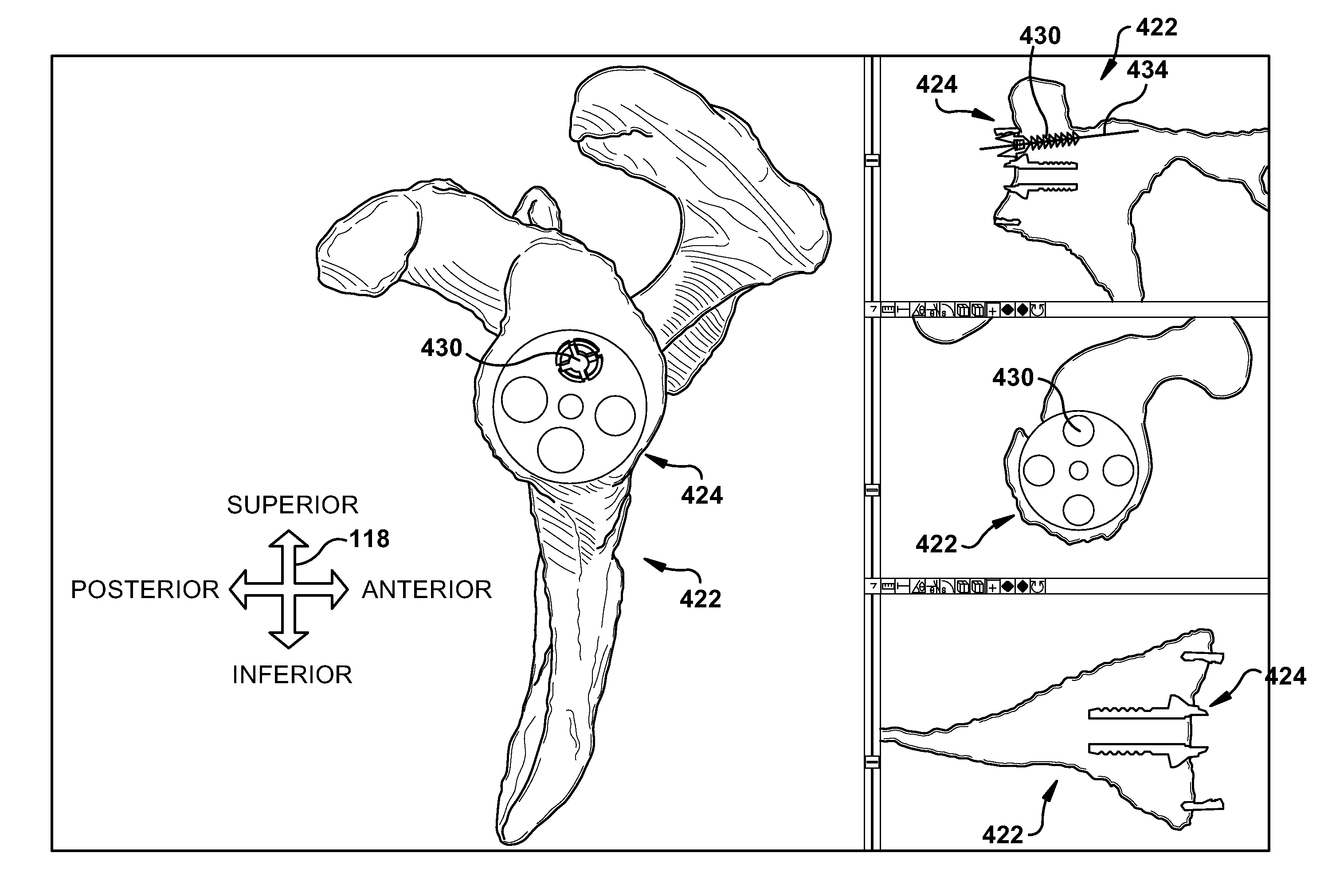
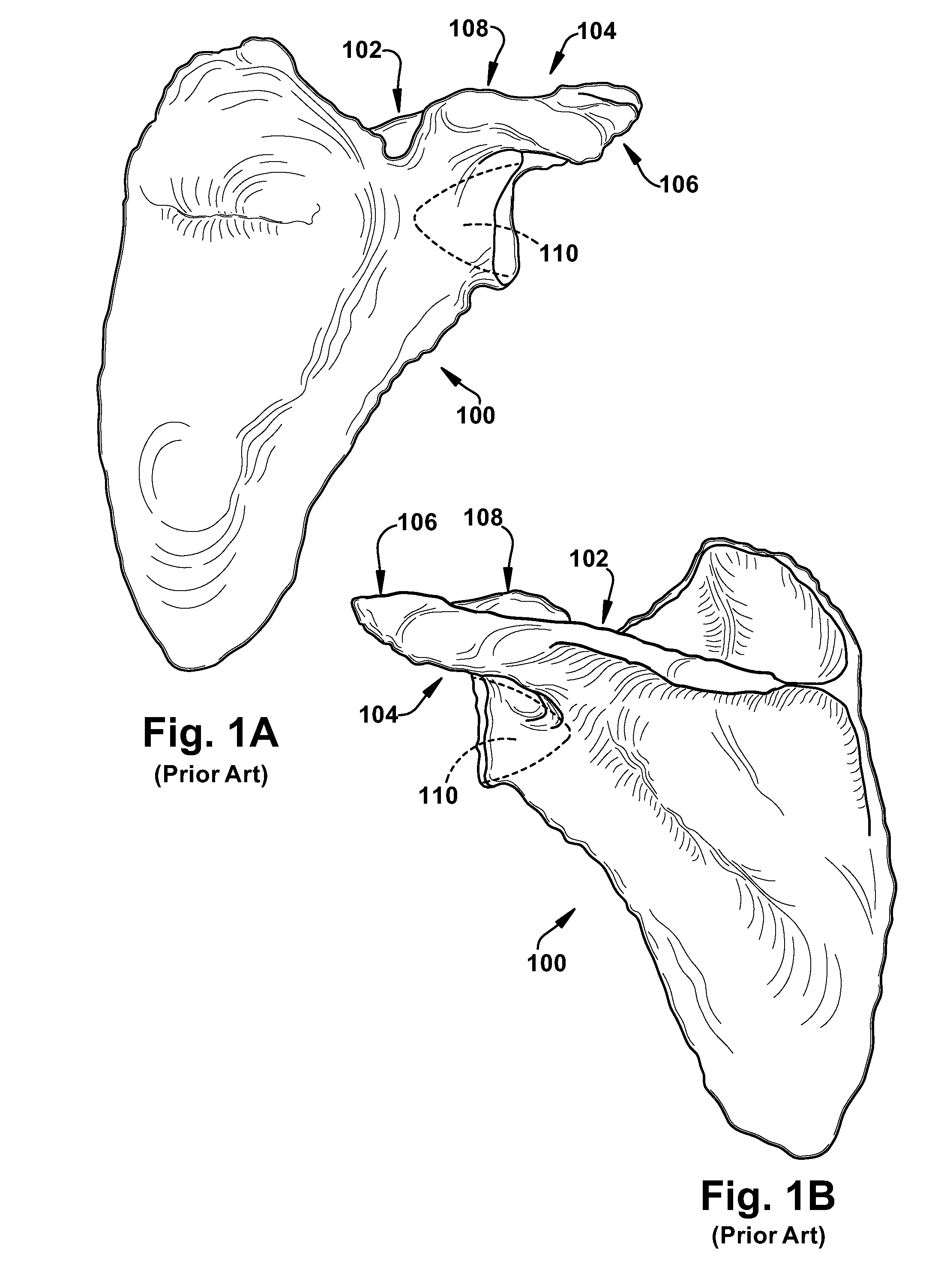
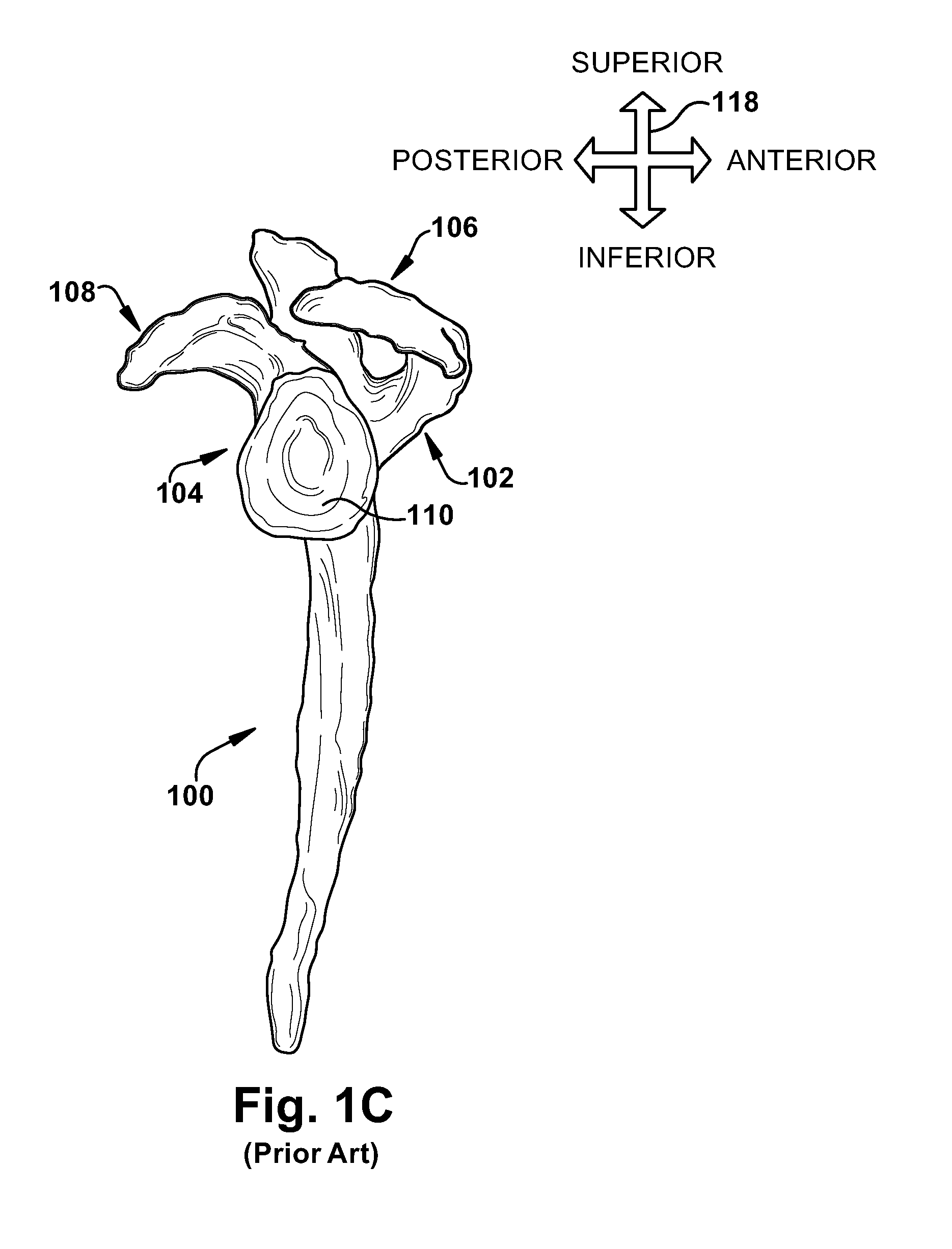
[0044]The patient tissue is shown and described herein at least as a scapula 100 and the prosthetic implant component is shown and described herein at least as a glenoid component 216, but the patient tissue and corresponding prosthetic implant component could be any desired types such as, but not limited to, hip joints, shoulder joints, knee joints, ankle joints, phalangeal joints, metatarsal joints, spinal structures, long bones (e.g., fracture sites), or any other suitable patient tissue use environment for the present invention. For example, the prosthetic implant component could be an internal fixation device (e.g., a bone plate), a structure of a replacement / prosthetic joint, or any other suitable artificial device to replace or augment a missing or impaired part of the body.
[0045]The term “lateral” is used herein to refer to a direction indicated by directional arrow 118 in FIG. 1C; the lateral direction in FIG. 1C lies substantially within the plane of the drawing and includ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com