Minimally-invasive retroperitoneal lateral approach for spinal surgery
a retroperitoneal lateral and minimally invasive technology, applied in the field of minimally invasive retroperitoneal lateral approach for spinal surgery, can solve the problems of pain and sometimes debilitating nerve impingement syndrome, unfettered anterior spinal exposure for precise midline placement of prosthetic discs, and significant surgical disruption of the anterior annular element around the dis
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
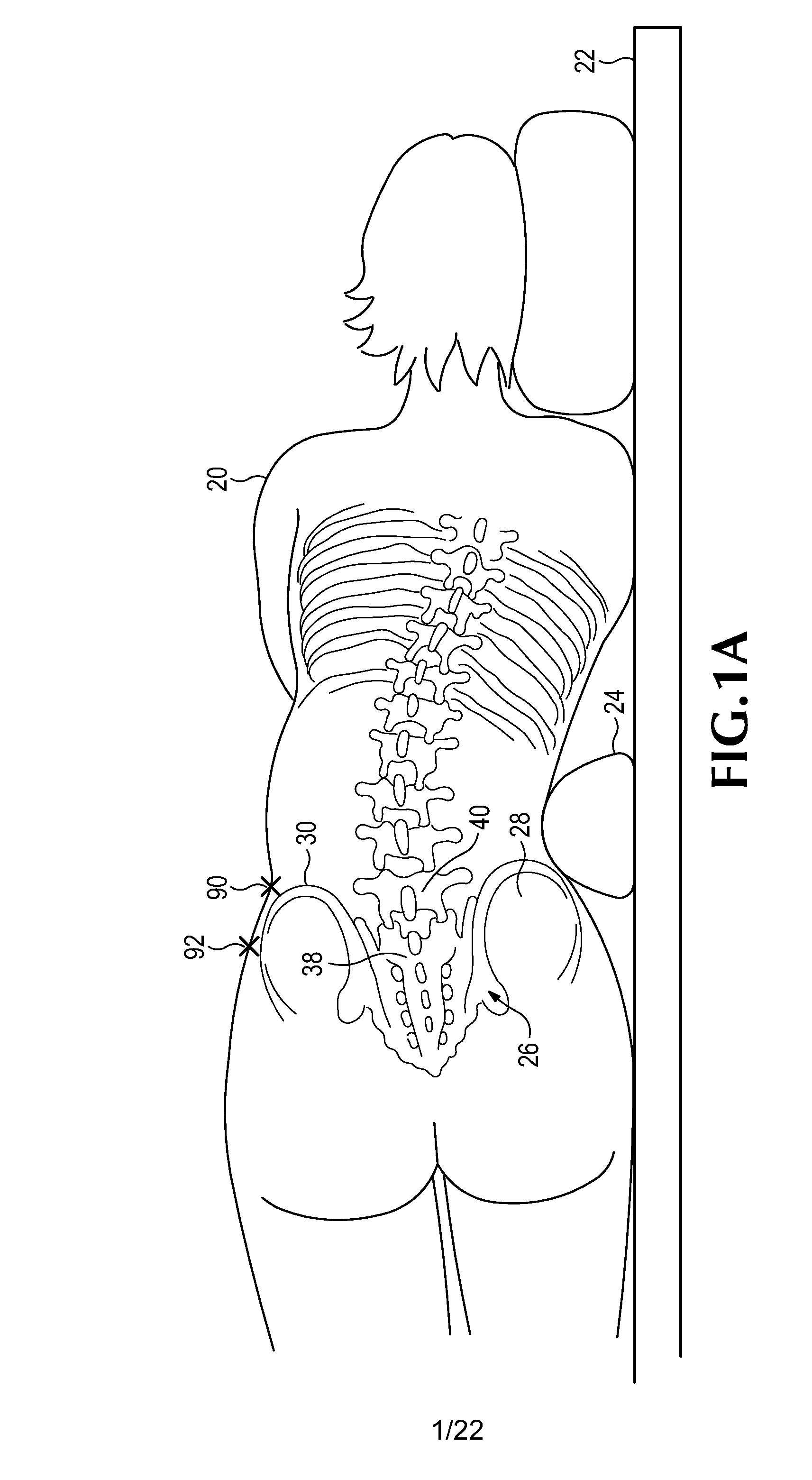
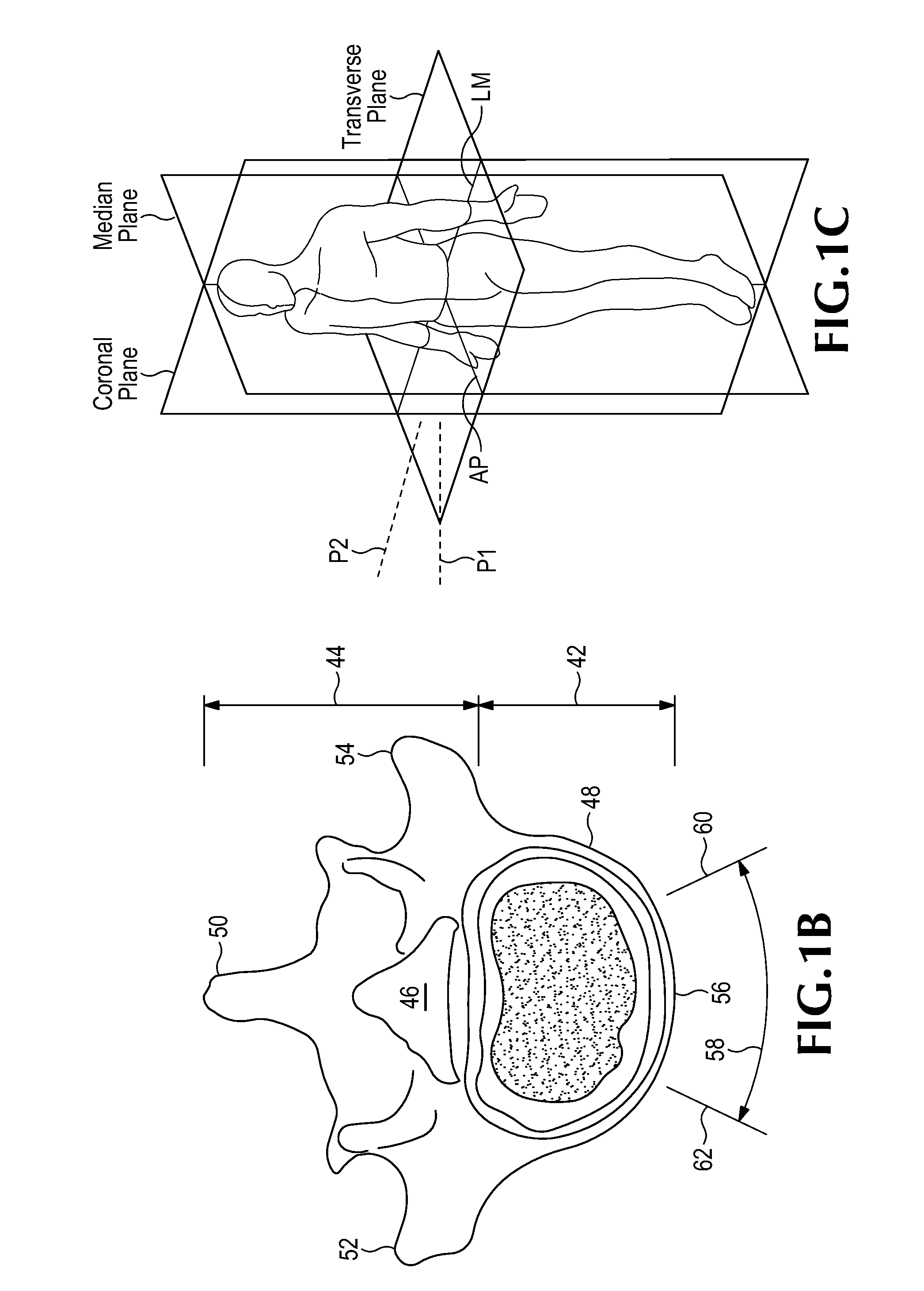
[0063]Embodiments of the invention are disclosed herein for accessing an intervertebral space, such as the L5-S1 space, and implanting a prosthetic disc implant within that space. The disclosed devices, methods and systems are suitable for use in a minimally invasive procedure for repairing degenerated or otherwise injured intervertebral discs.
General Overview of the Surgical Procedure
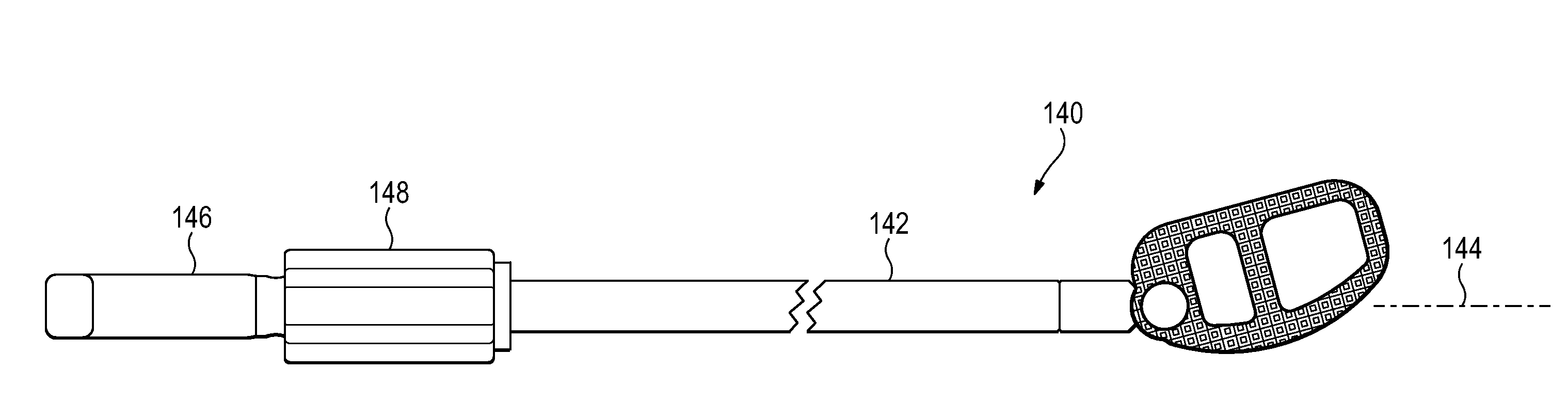
[0064]The method generally includes initially accessing the intervertebral space using a retroperitoneal lateral approach. Then, with a finger-directed dilator or other suitable instrument, the distal retroperitoneum is swept anteriorly to expose an eventual channel to a direct approach to L5-S1. In most people, the direct approach to L5-S1 is anterior to the anterior superior iliac spine, or between the anterior superior iliac spine and the anterior inferior iliac spine. An incision is then made to open this channel, and blunt dilators are directed in an oblique direction directly to the mid-anterior ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com