Apparatus, systems and methods for determining tissue oxygenation
a tissue oxygenation and apparatus technology, applied in the field of apparatus, systems and medical devices, can solve the problems of inability to pain, need for reoperation, extreme sickness or death, and inability to reliably predict when a failure will occur
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
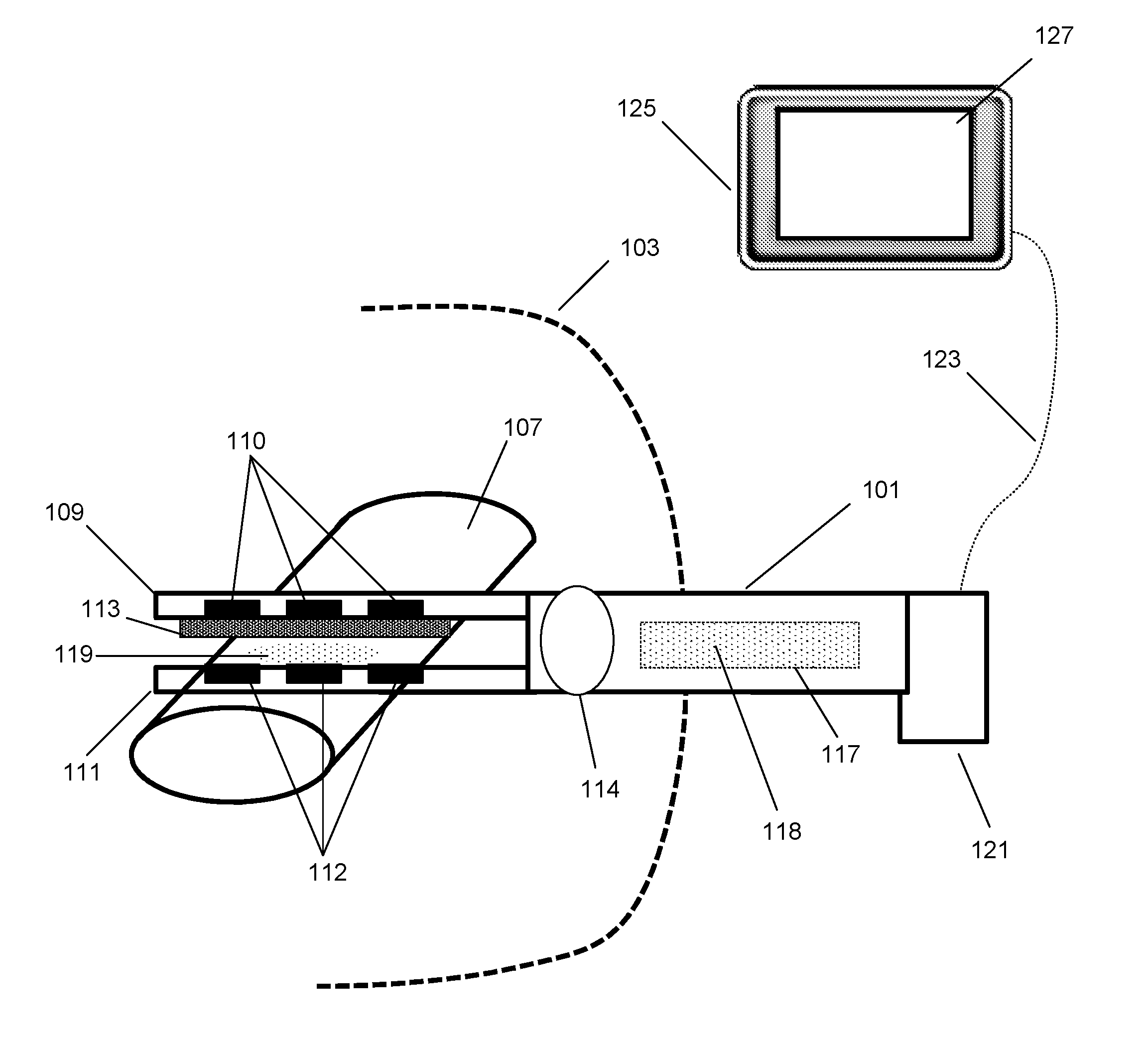
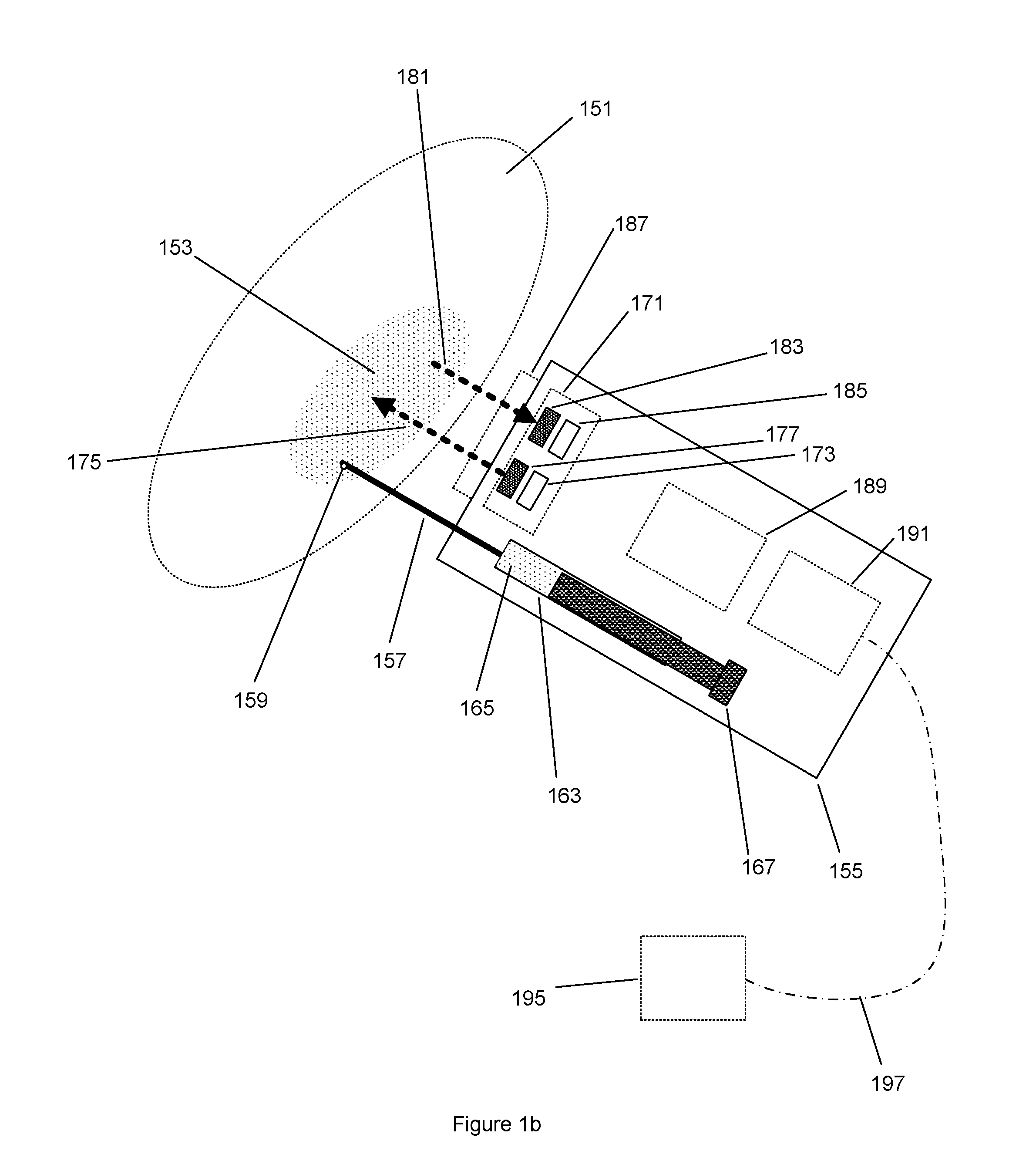
[0036]Each surgical procedure has the potential for failure. A common procedure in gastrointestinal surgery is a bowel resection—removing the affected portion of the bowel and then mechanically joining the ends of the remaining segments to re-establish bowel continuity. The mechanical connection of the free ends of bowel forms what is termed a surgical anastomosis. A surgical anastomosis is formed by either traditional techniques using suture material, or by contemporary techniques which may include utilizing surgical staplers or other surgical fastening device. A surgical stapler mechanically joins the bowel by firing a pattern of staples from a cartridge or housing through the two free ends of bowel against an anvil that ultimately forms a securing crimp on the opposing side. There are many embodiments of surgical staplers. Some staplers form linear staple patterns, while others form circular patterns. Some staplers incorporate functionality for cutting tissue. Many staplers have ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com