Trapezium implant for thumb and method
a technology applied in the field of thumb and implant, can solve the problems of prior art prosthesis slipping out of place, insufficient ligament reconstruction, compounding the pathological process, etc., and achieve the effect of increasing strength and longevity
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
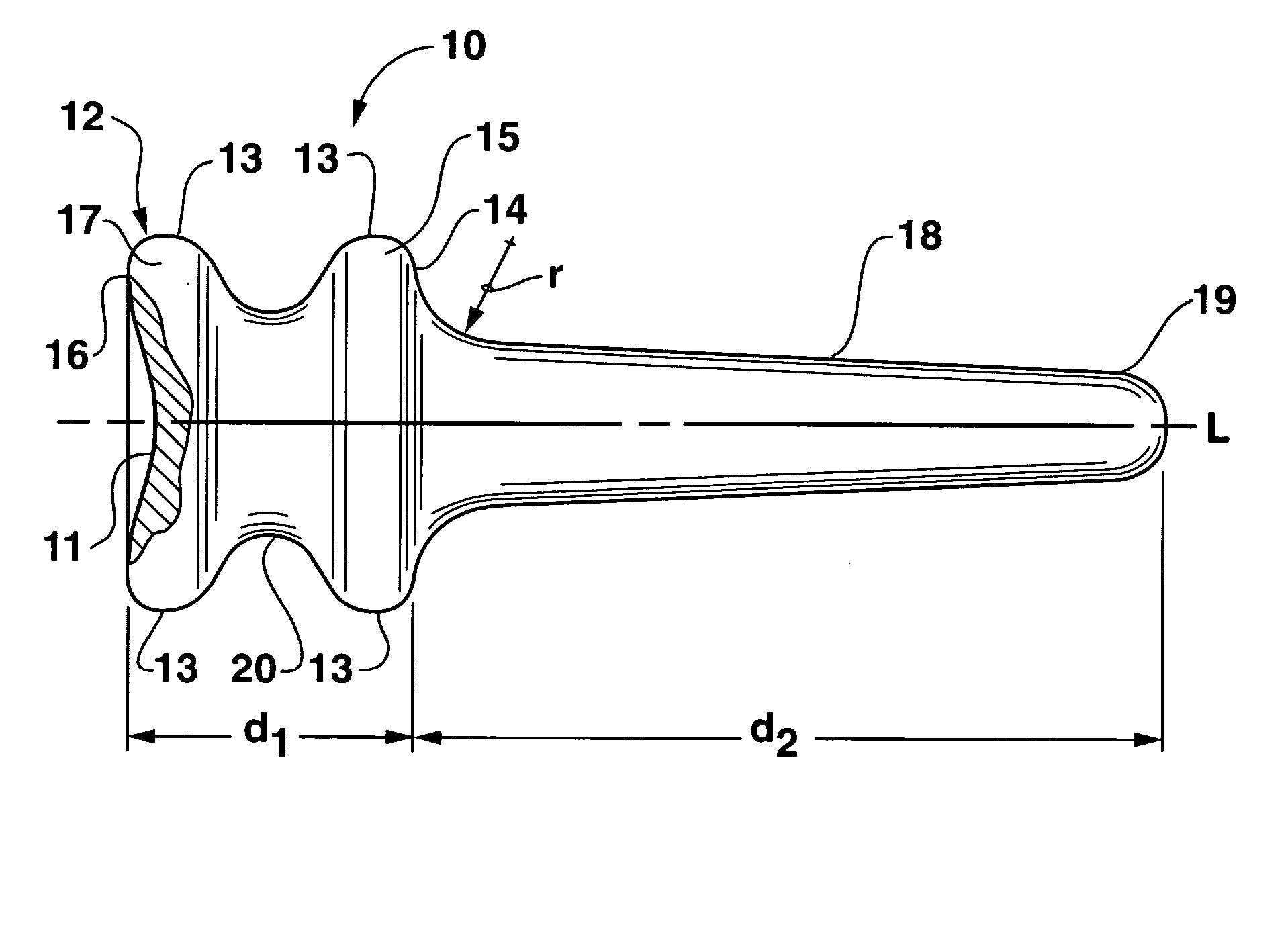
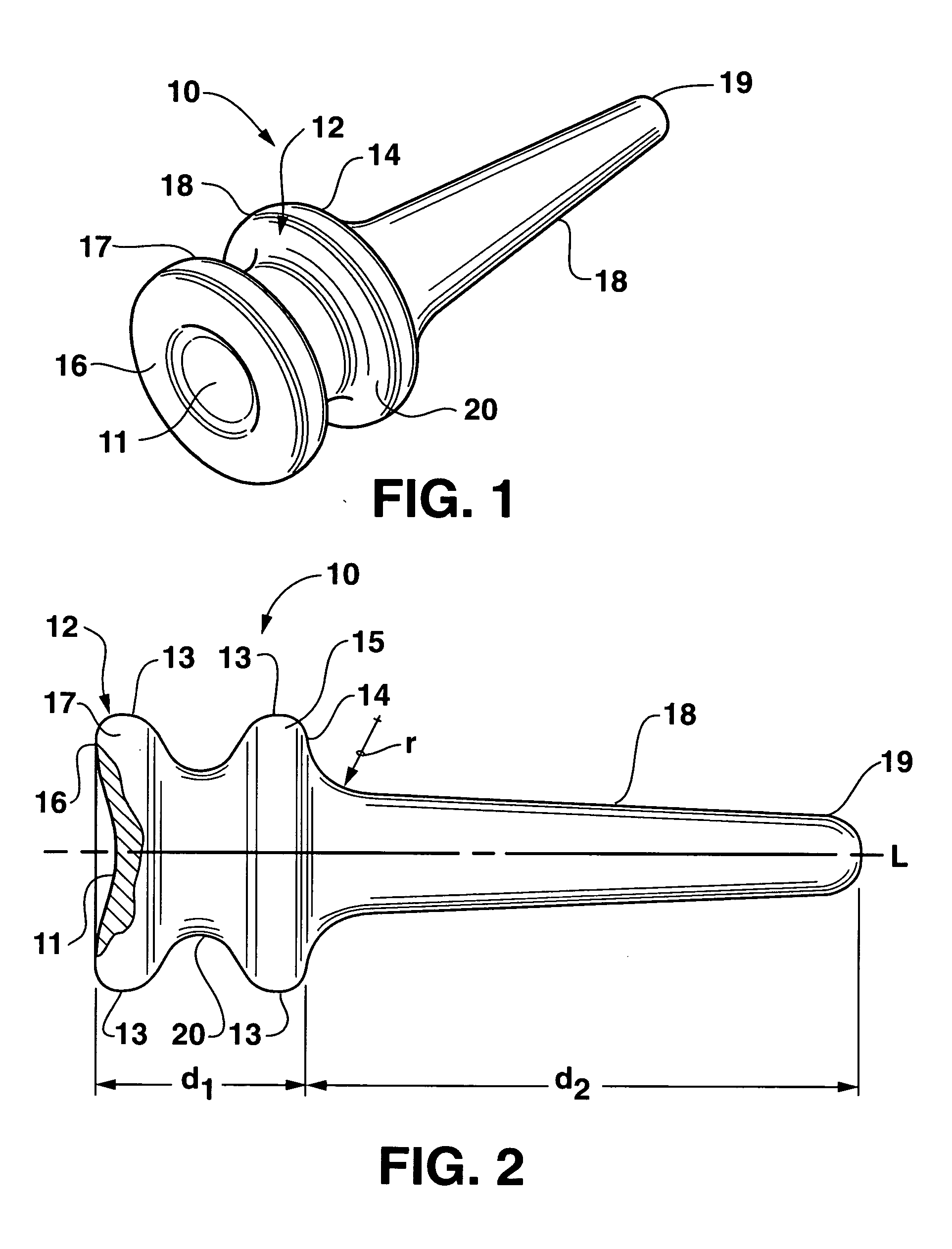
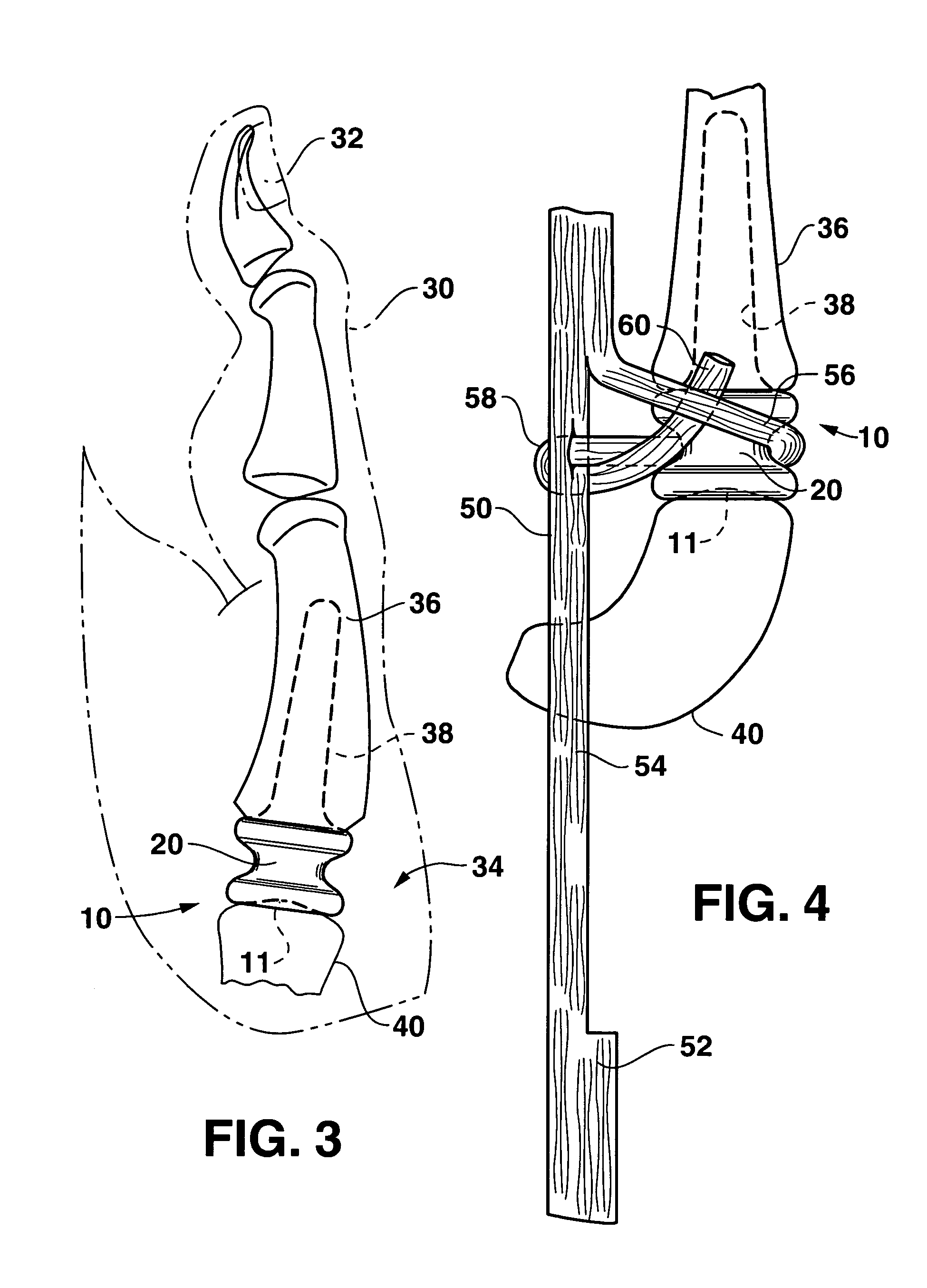
[0019] With reference to the figures, an exemplary embodiment of a trapezium prosthesis / implant for the thumb that meets and achieves all the above-mentioned objects of the invention will now be described.
[0020] Referring to FIGS. 1 and 2, the exemplary embodiment of the trapezium implant according to the invention is generally designated by the numeral 10 and comprises an integral elastomeric member, preferably a silastic material such as silicone rubber, and which is inherently flexible and physiologically inert. The implant 10 includes a body portion 12 having tapered conical portions 15 and 17 separated by a tapered neck 20. Tapered portions 15 and 17 have end faces 14 and 16, respectively. Integrally formed and projecting from the end face 14 is an elongated, longitudinally extended tapered portion18 which extends along the longitudinal axis L of implant 10. Tapered portion 18 will have a length d2 that is typically equal to 3 (three) times the length d1 of body portion 12 so ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com