Patents
Literature
1035results about "Ankle joints" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
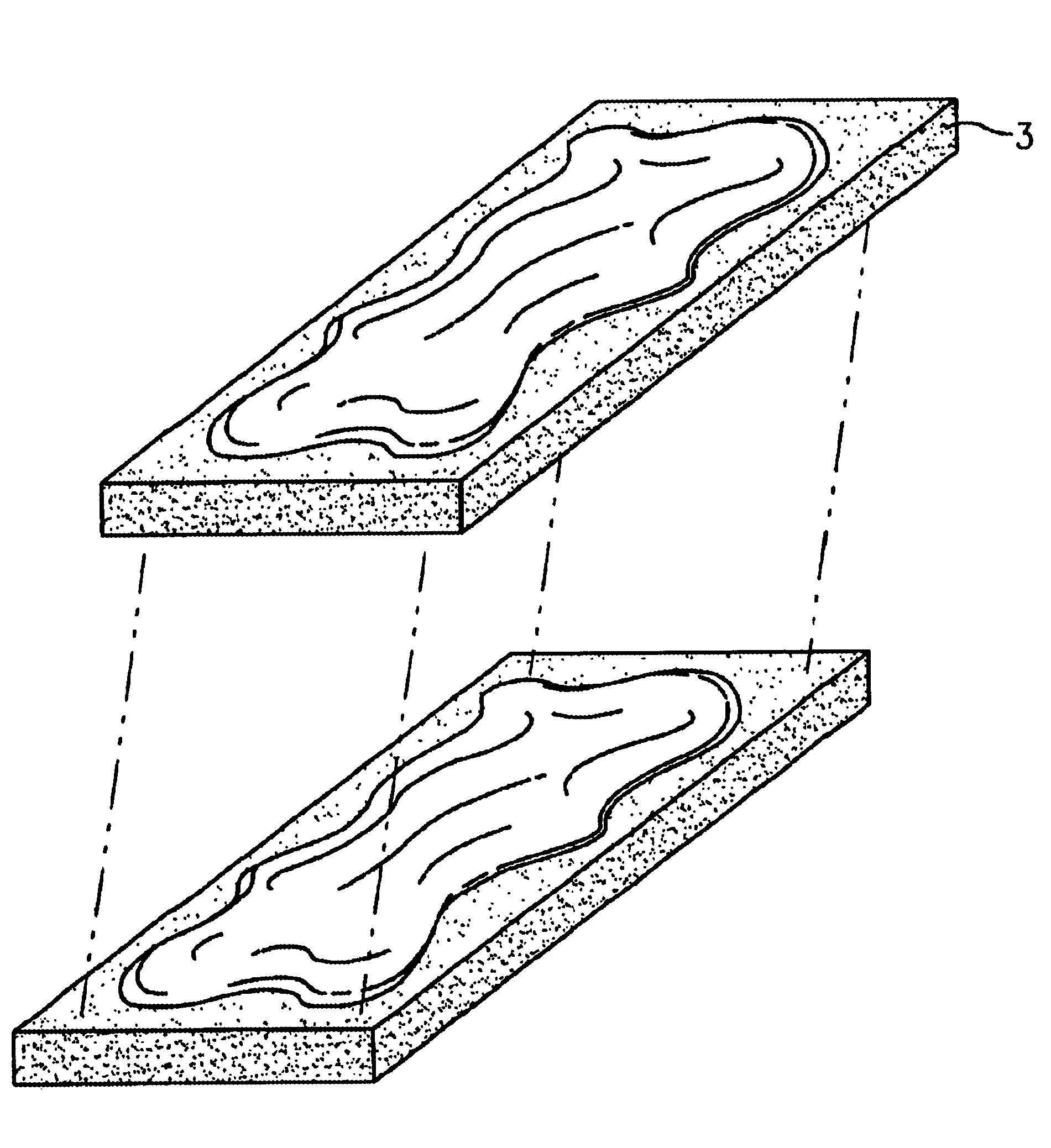
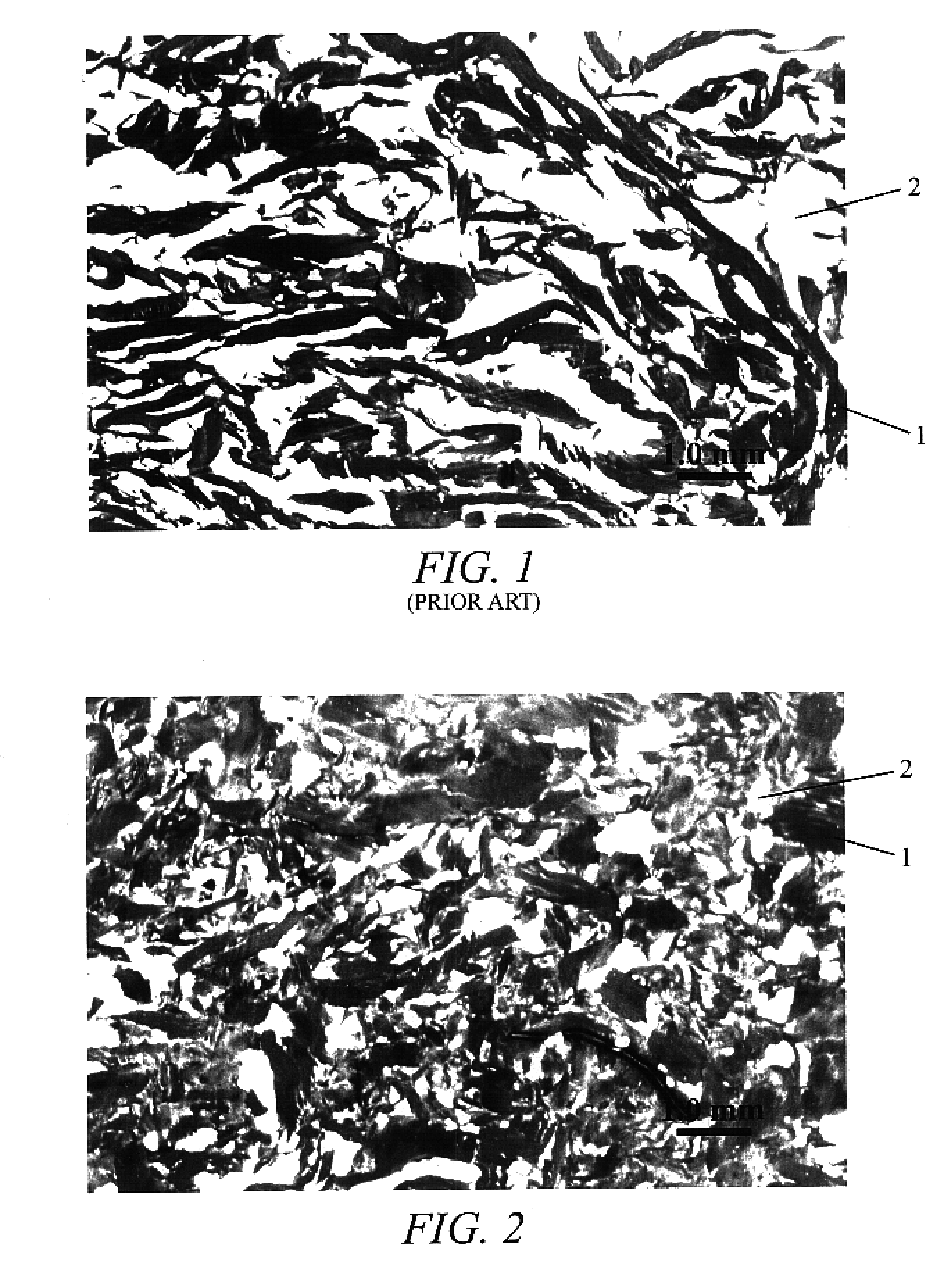
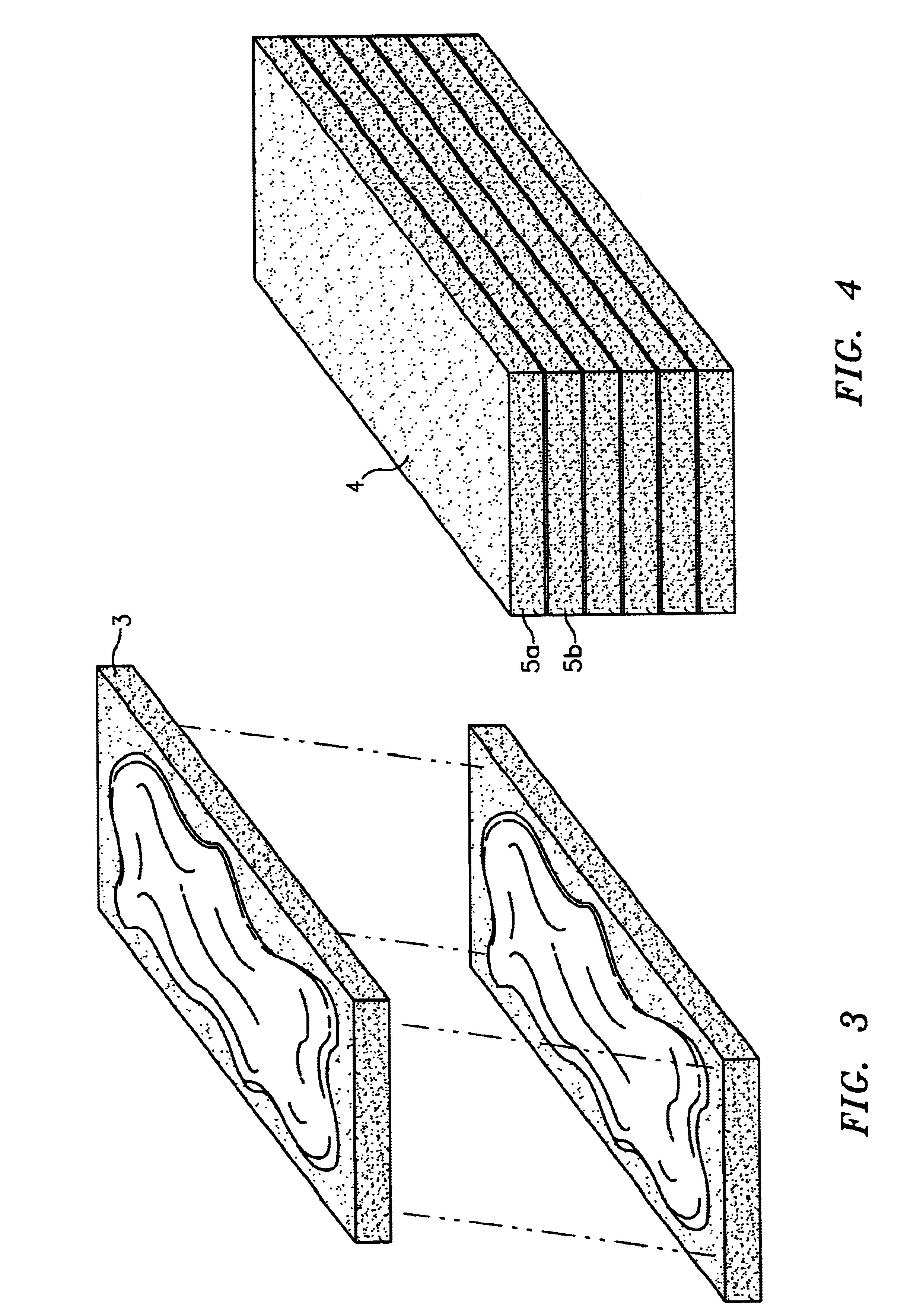
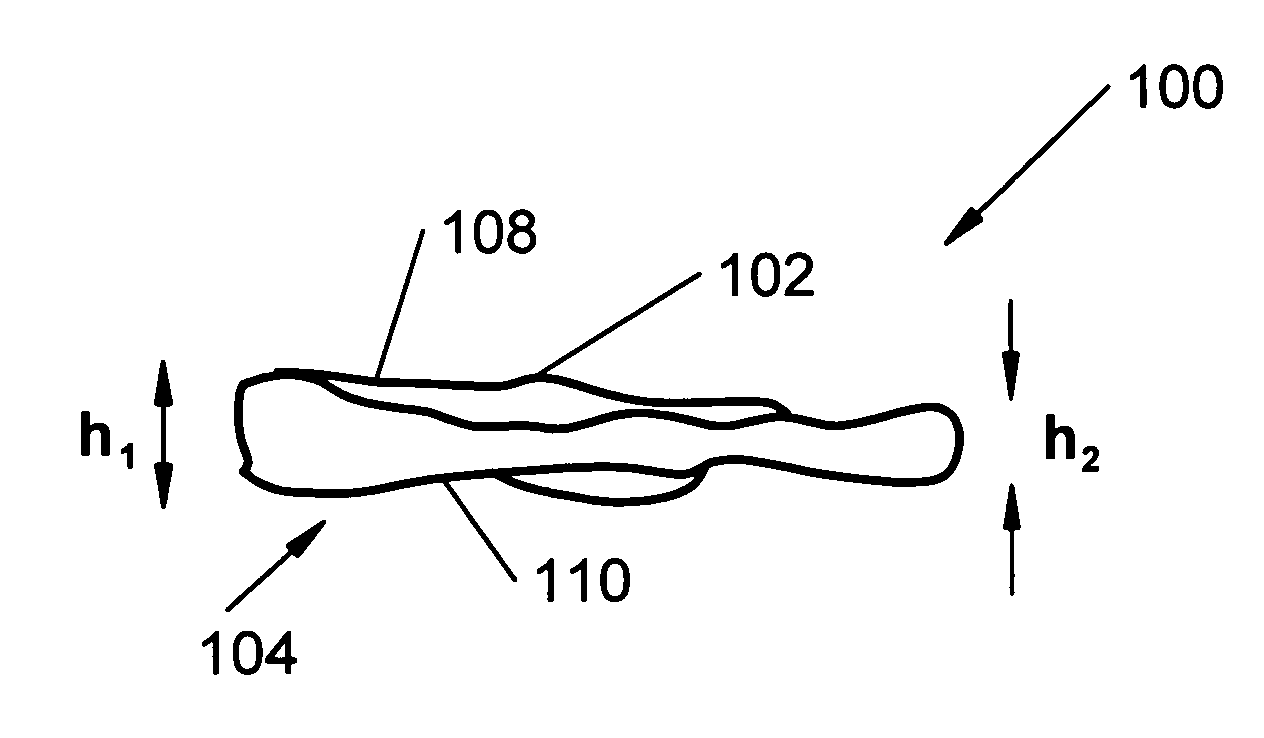
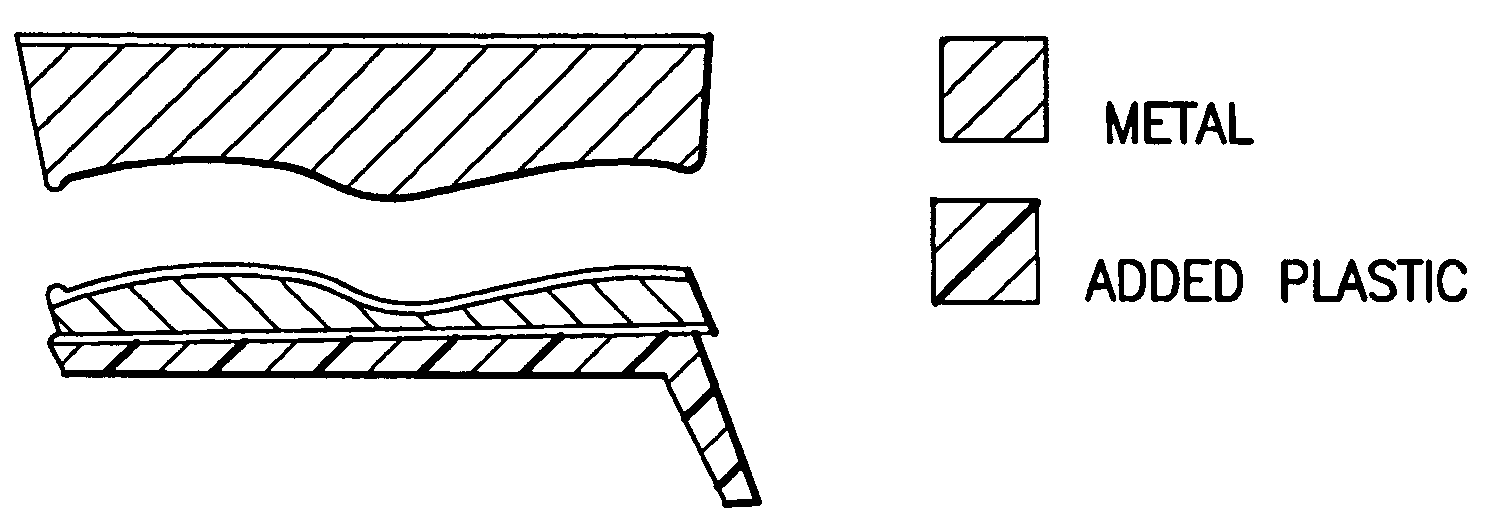
Osteogenic implants derived from bone
An osteogenic osteoimplant in the form of a flexible sheet comprising a coherent mass of bone-derived particles, the osteoimplant having a void volume not greater than about 32% and a method of making an osteogenic osteoimplant having not greater than about 32% void volume, the method comprising: providing a coherent mass of bone-derived particles; and, mechanically shaping the coherent mass of bone-derived particles to form an osteogenic osteoimplant in the form of a flexible sheet.
Owner:WARSAW ORTHOPEDIC INC
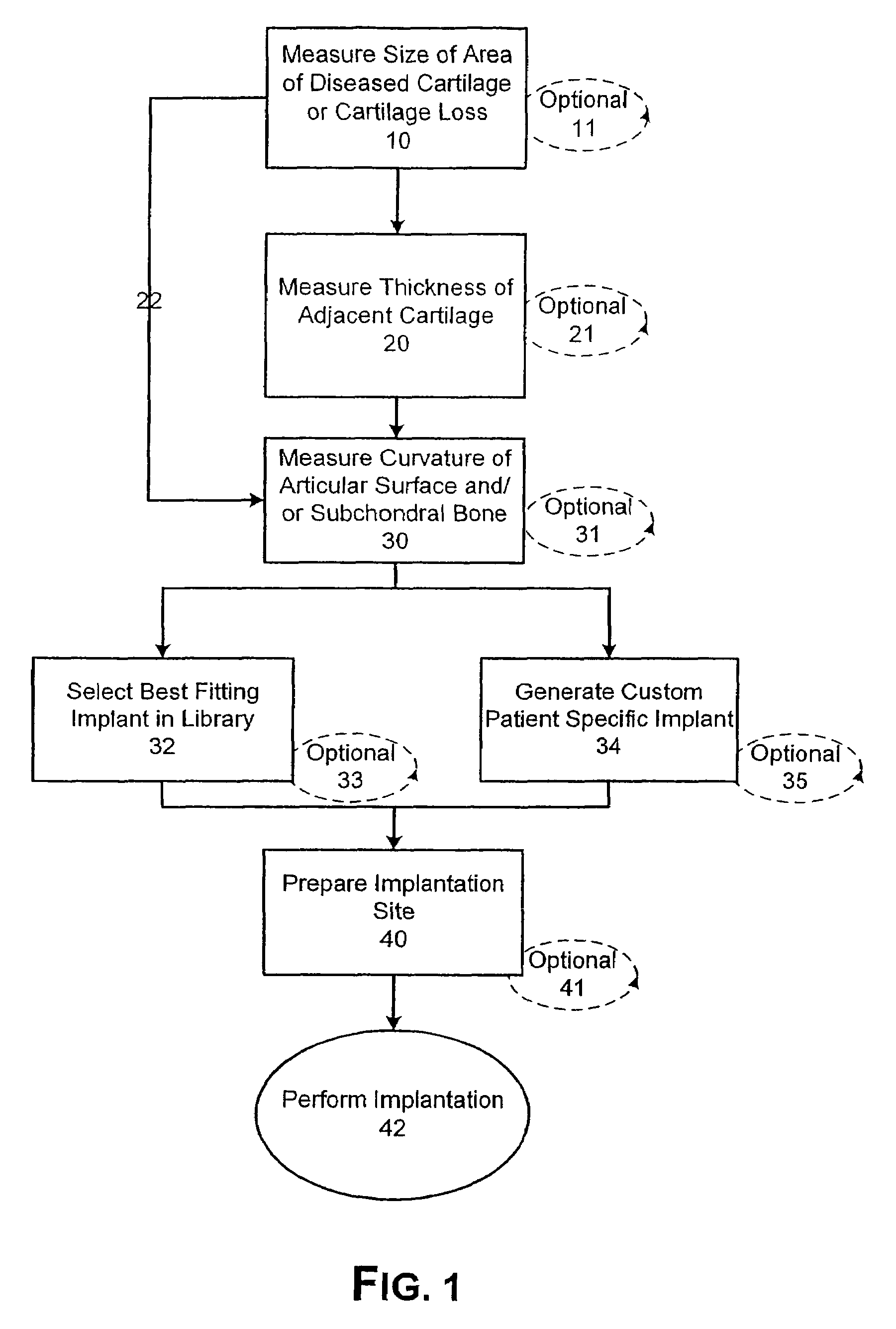
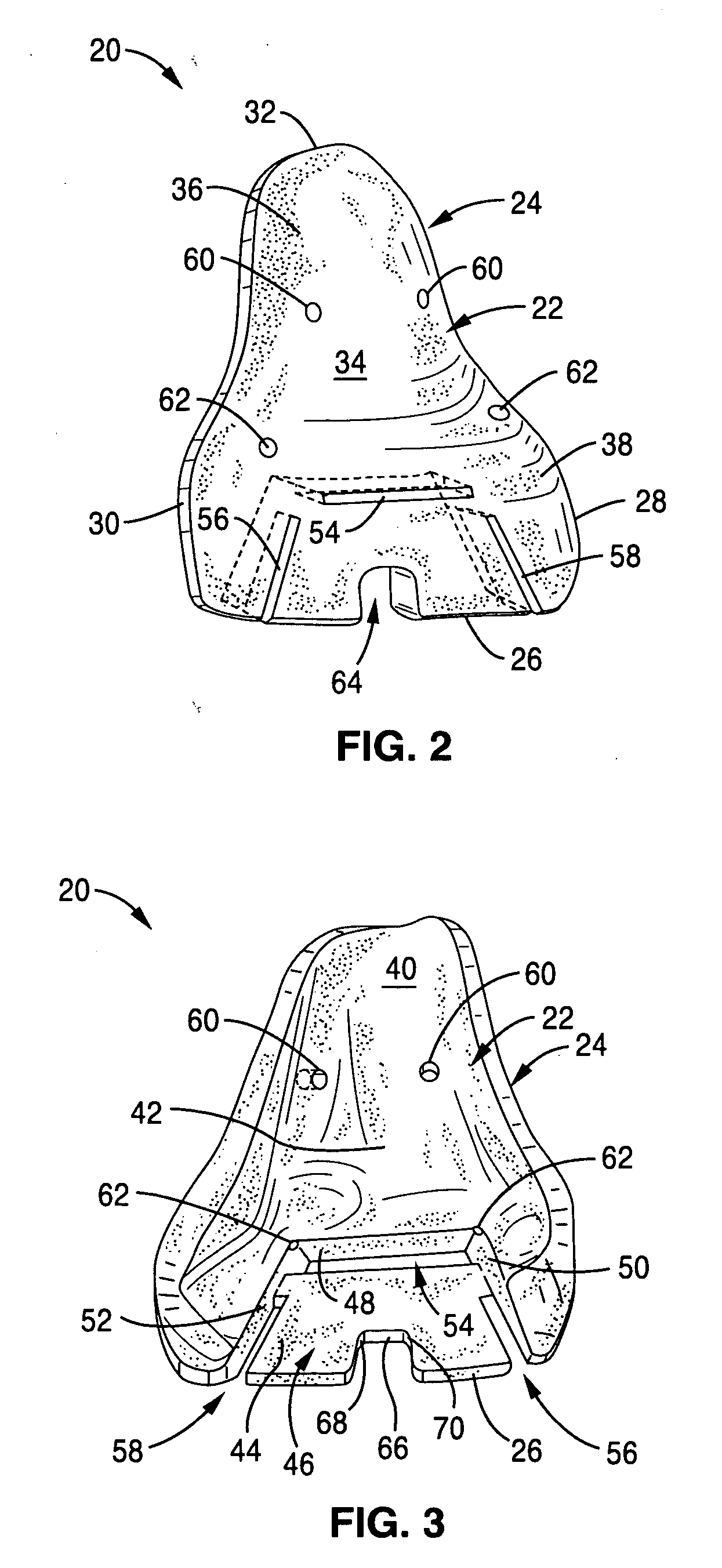
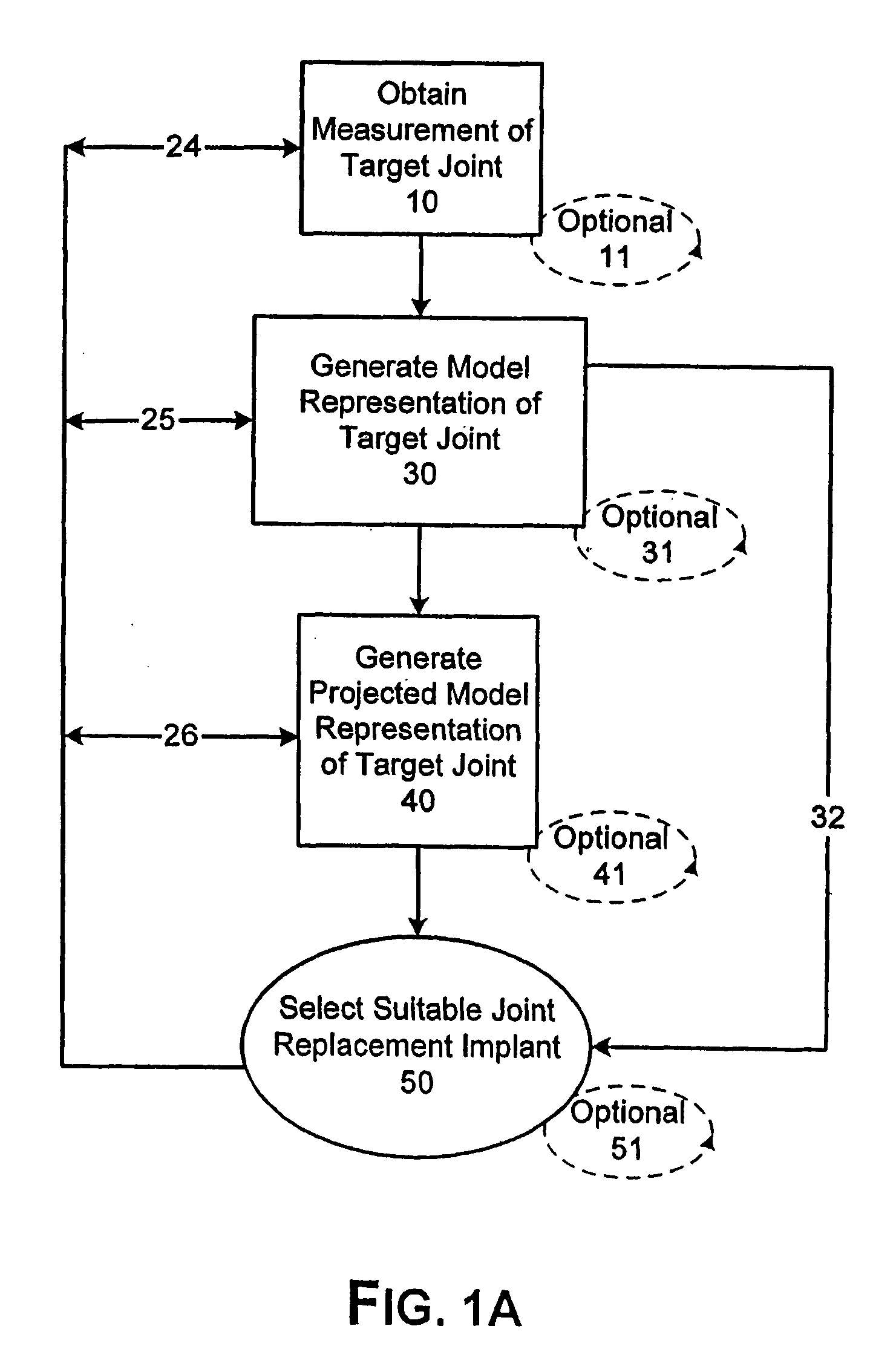
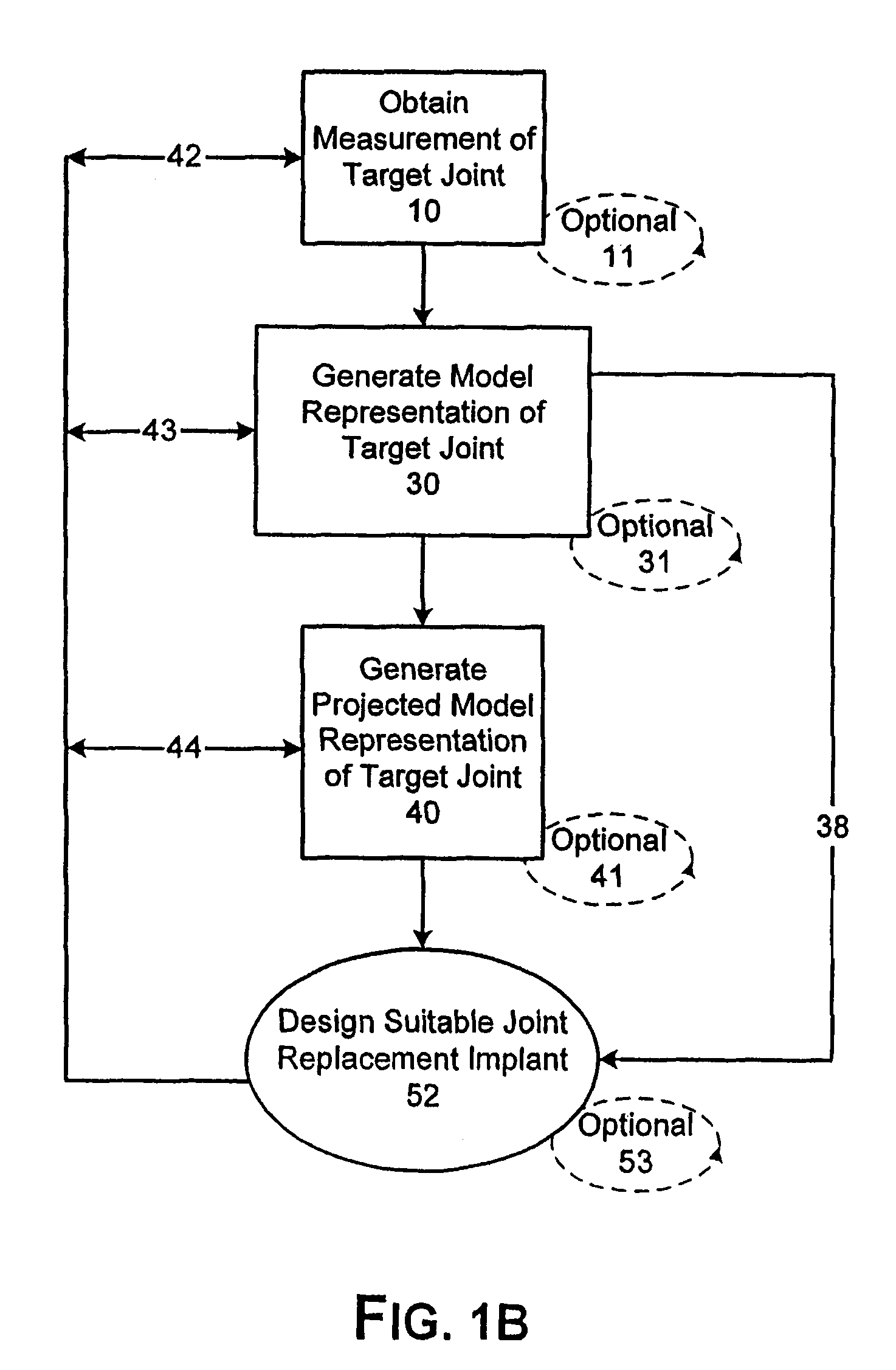
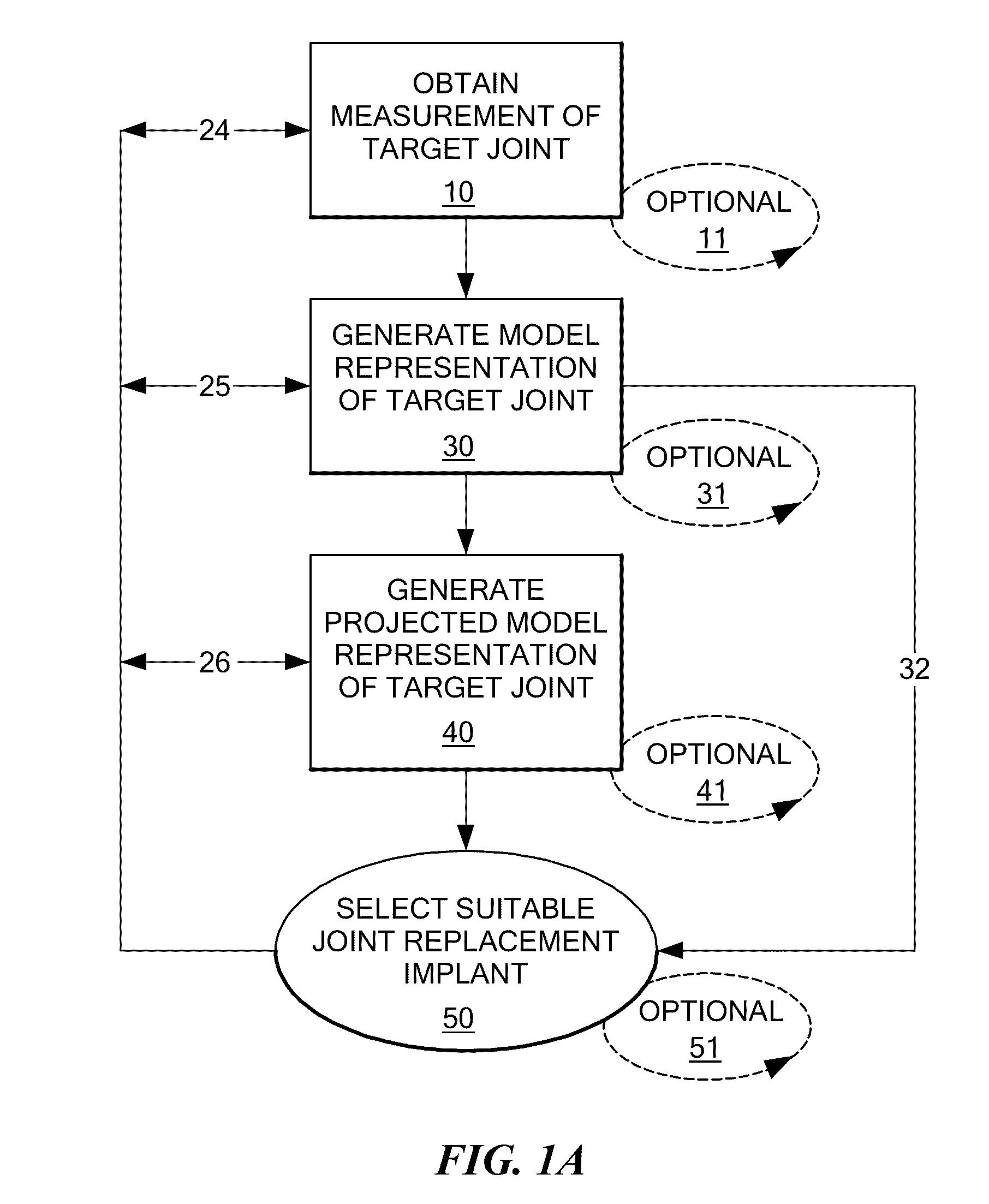
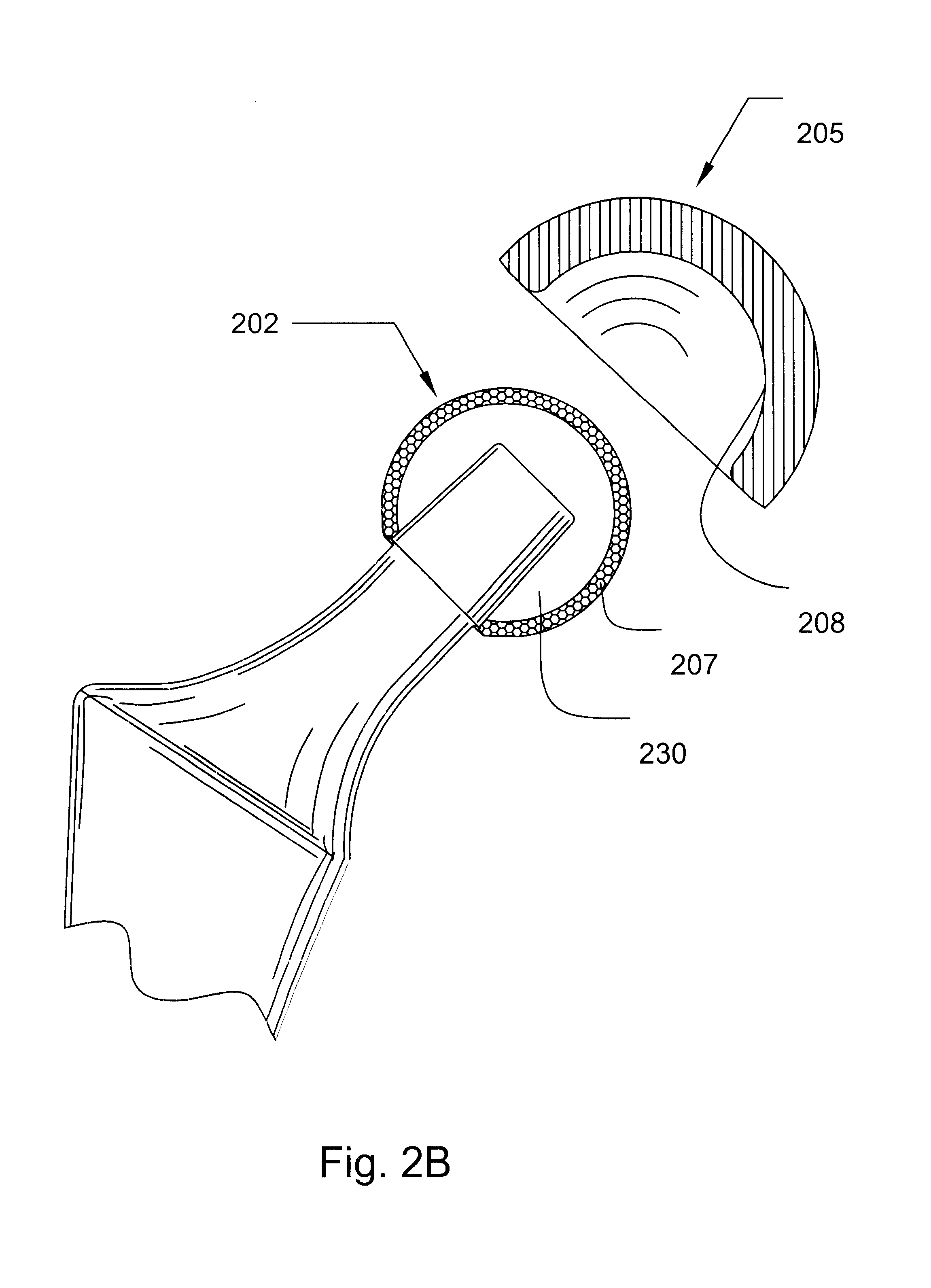
Patient selectable joint arthroplasty devices and surgical tools facilitating increased accuracy, speed and simplicity in performing total and partial joint arthroplasty
Disclosed herein are methods, compositions and tools for repairing articular surfaces repair materials and for repairing an articular surface. The articular surface repairs are customizable or highly selectable by patient and geared toward providing optimal fit and function. The surgical tools are designed to be customizable or highly selectable by patient to increase the speed, accuracy and simplicity of performing total or partial arthroplasty.
Owner:CONFORMIS
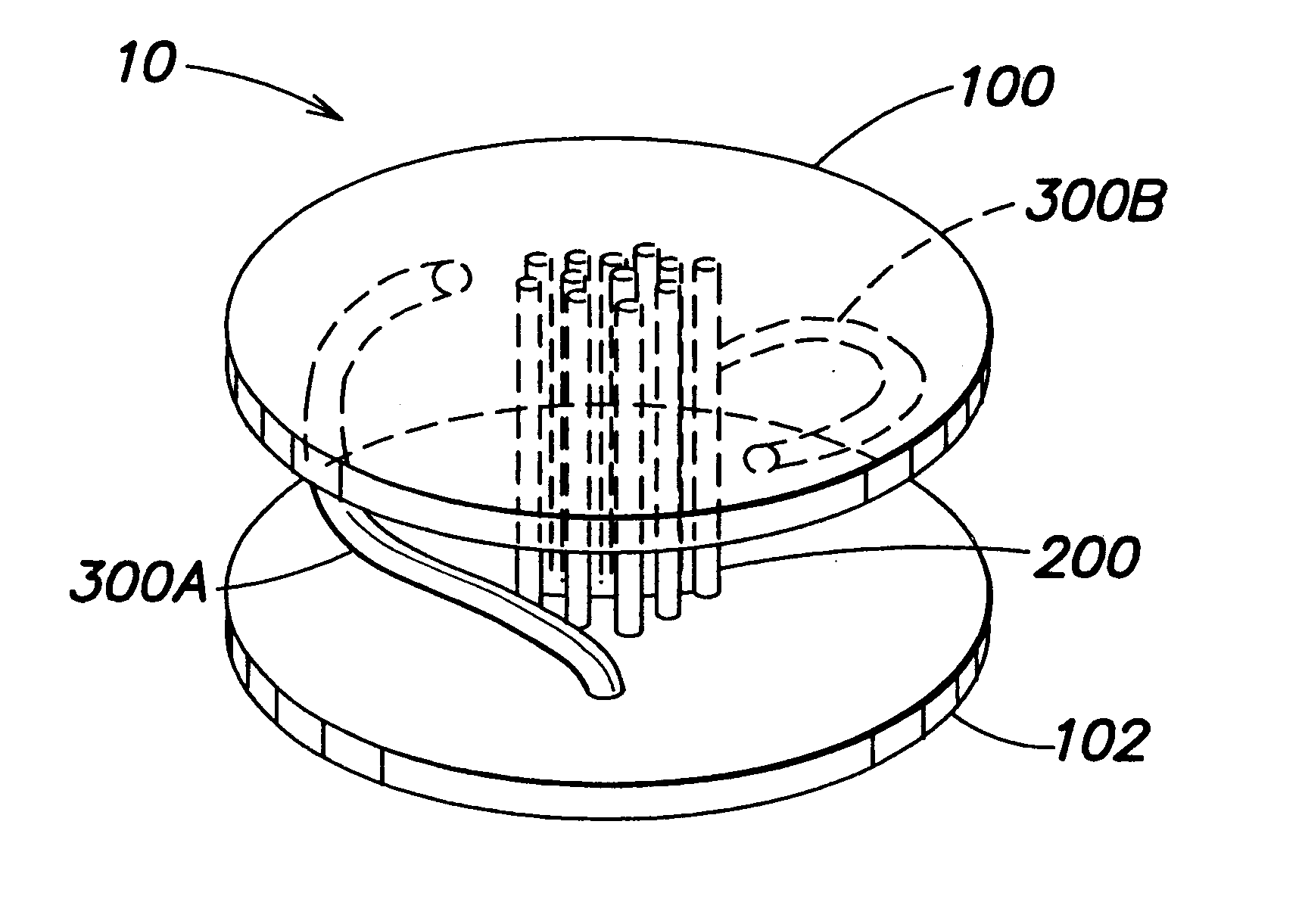
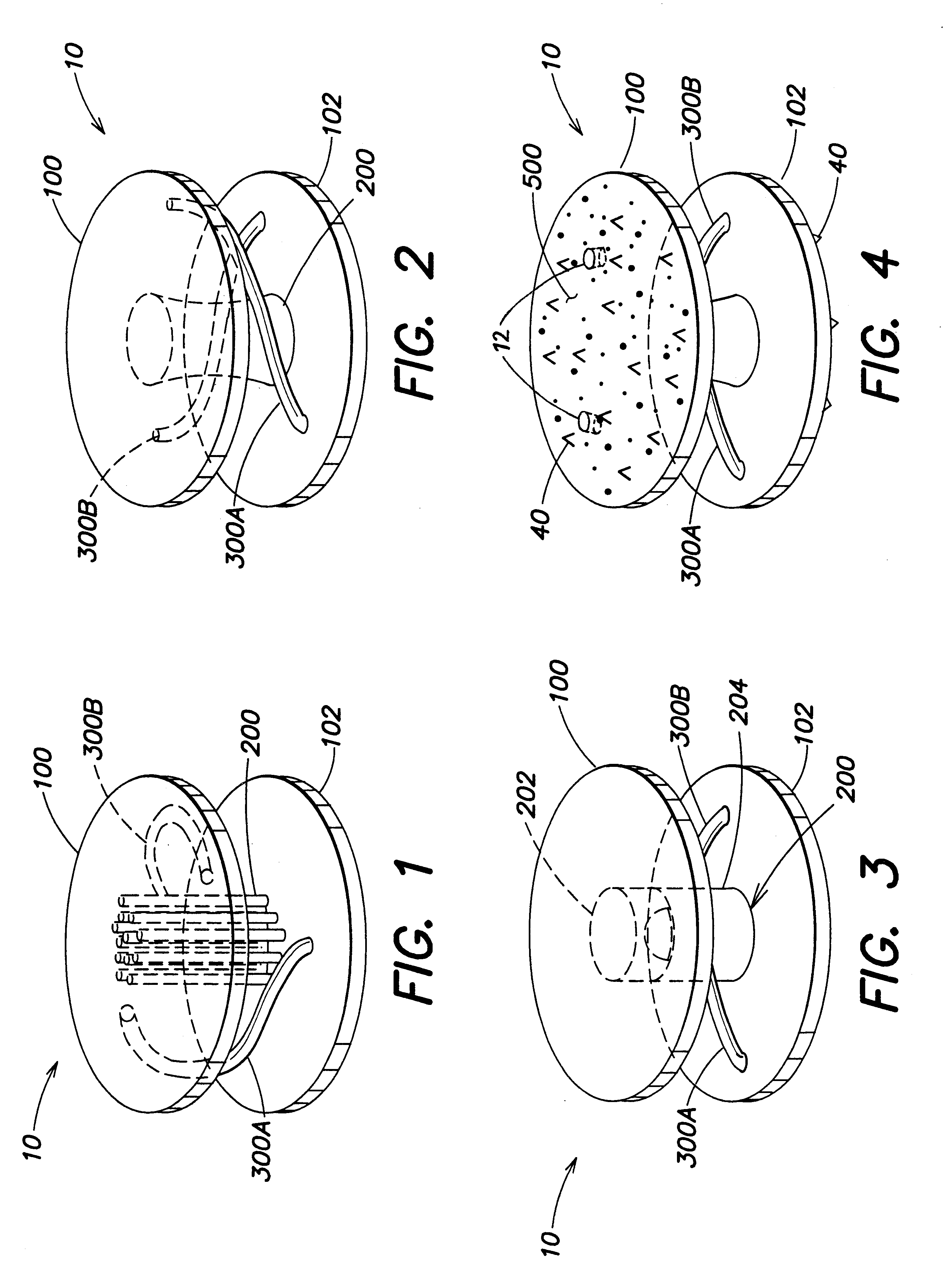
Orthopedic implant
Disclosed is an orthopedic implant suitable for arthroplasty procedures. The orthopedic implant includes a first plate, a second plate, an axial support between the first plate and the second plate and one or more torsional supports connecting the first plate and the second plate. The axial support may be, for example, one or more flexible struts, such as cables, or a ball and socket joint. The torsional supports connect the first and second plates and may be, for example, curved around the axial support. The torsional supports may be integrally formed with the first and second plates as a single unitary device, by, for example, a Laser Engineered Net Shape (LENS) process.
Owner:DEPUY ACROMED INC
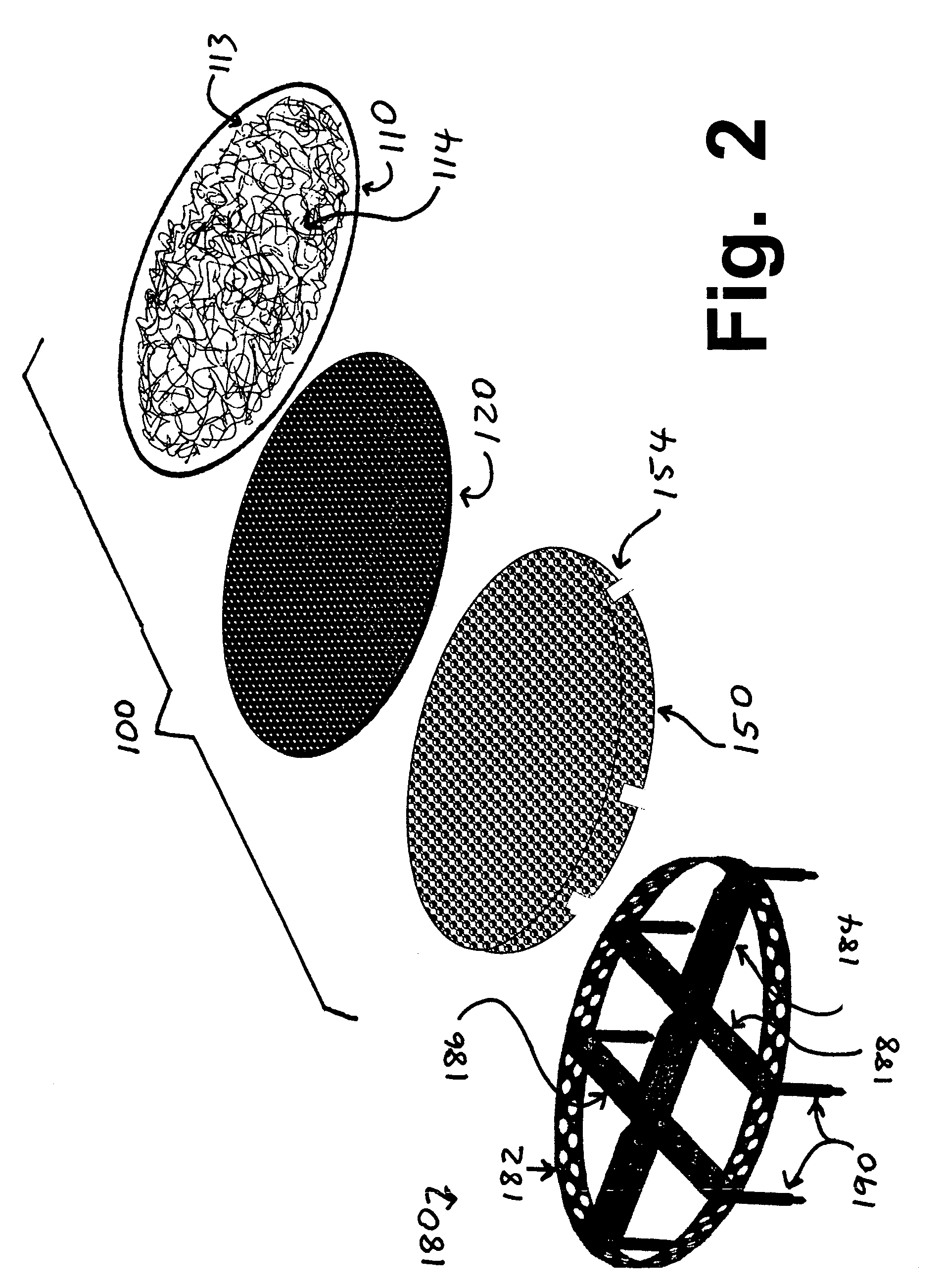
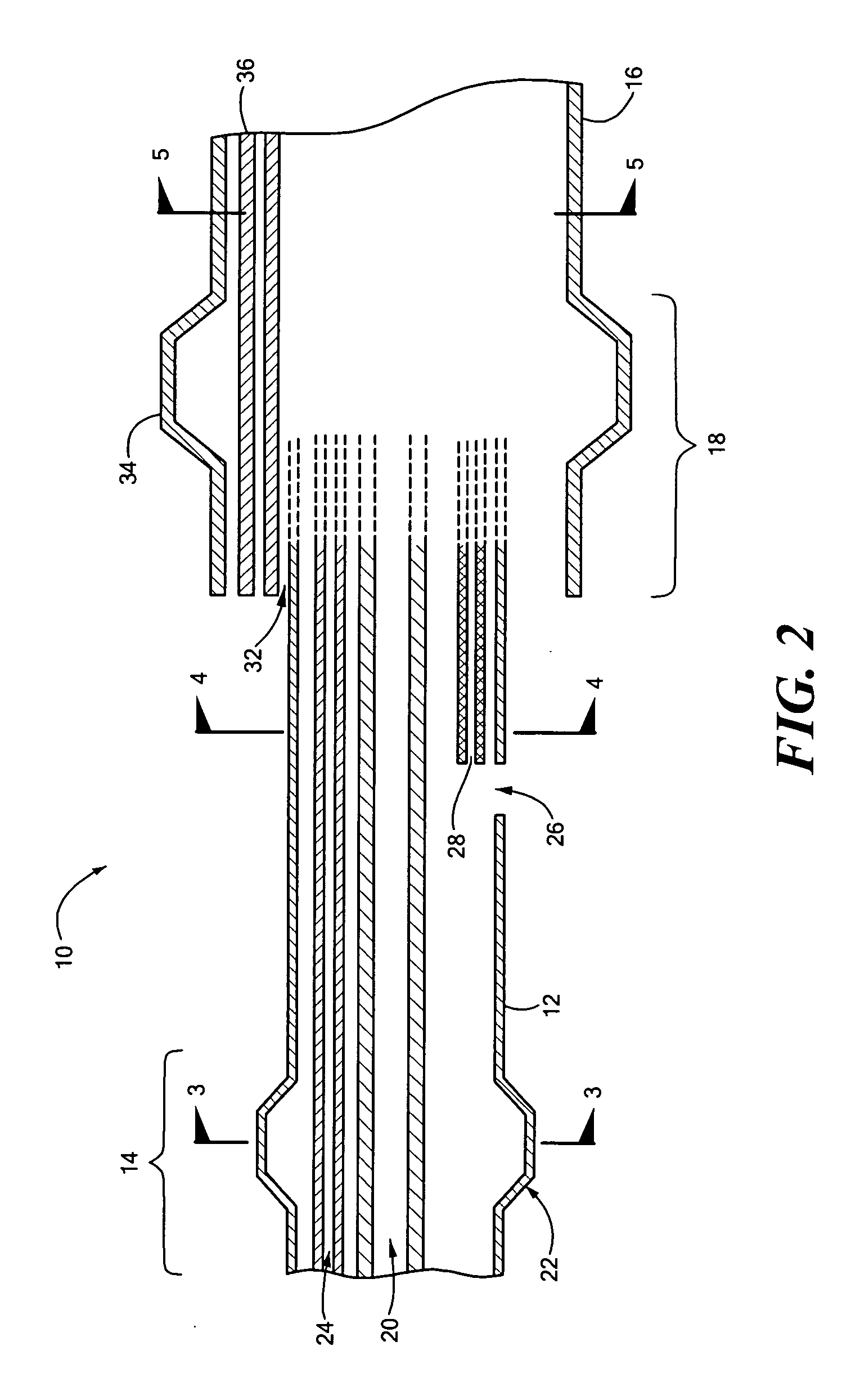
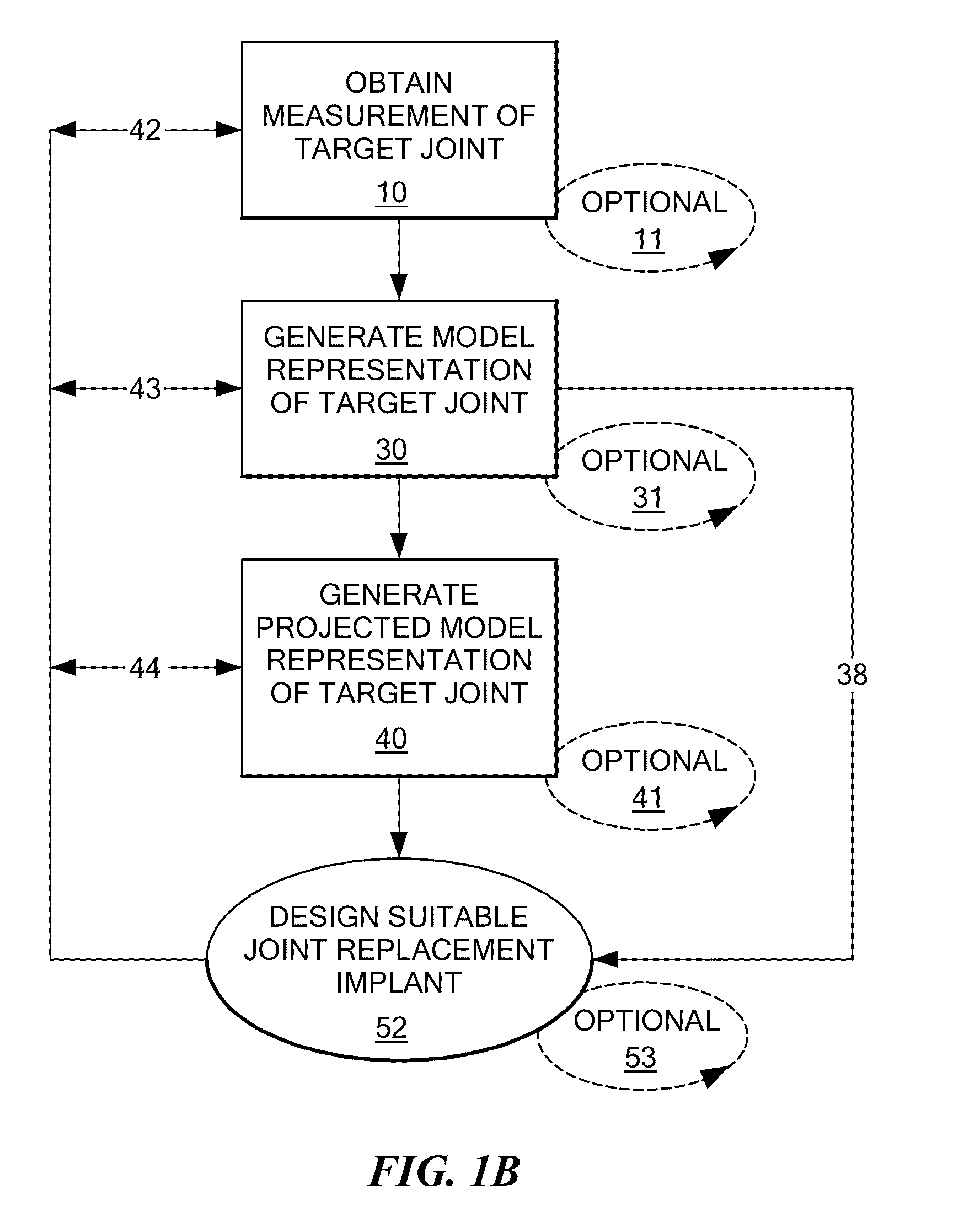
Implants for replacing cartilage, with negatively-charged hydrogel surfaces and flexible matrix reinforcement
ActiveUS9314339B2Strong and durableStrong and secure anchoringFinger jointsWrist jointsFiberChemical agent
A permanent non-resorbable implant allows surgical replacement of cartilage in articulating joints, using a hydrogel material (such as a synthetic polyacrylonitrile polymer) reinforced by a flexible fibrous matrix. Articulating hydrogel surface(s) are chemically treated to provide a negative electrical charge that emulates the negative charge of natural cartilage, and also can be treated with halogenating, cross-linking, or other chemical agents for greater strength. For meniscal-type implants, the reinforcing matrix can extend out from the peripheral rim of the hydrogel, to allow secure anchoring to soft tissue such as a joint capsule. For bone-anchored implants, a porous anchoring layer enables tissue ingrowth, and a non-planer perforated layer can provide a supportive interface between the hard anchoring material and the softer hydrogel material.
Owner:FORMAE
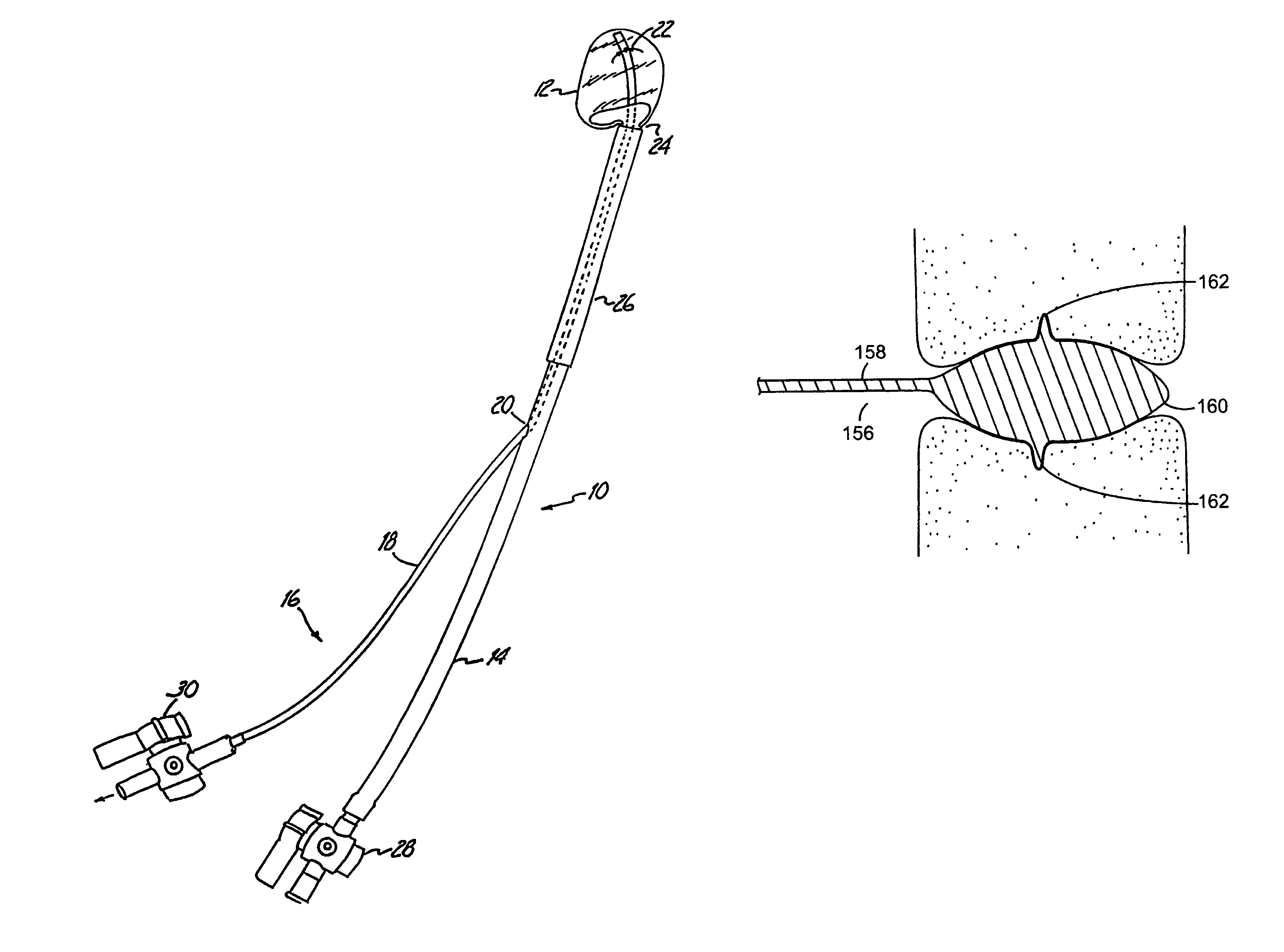
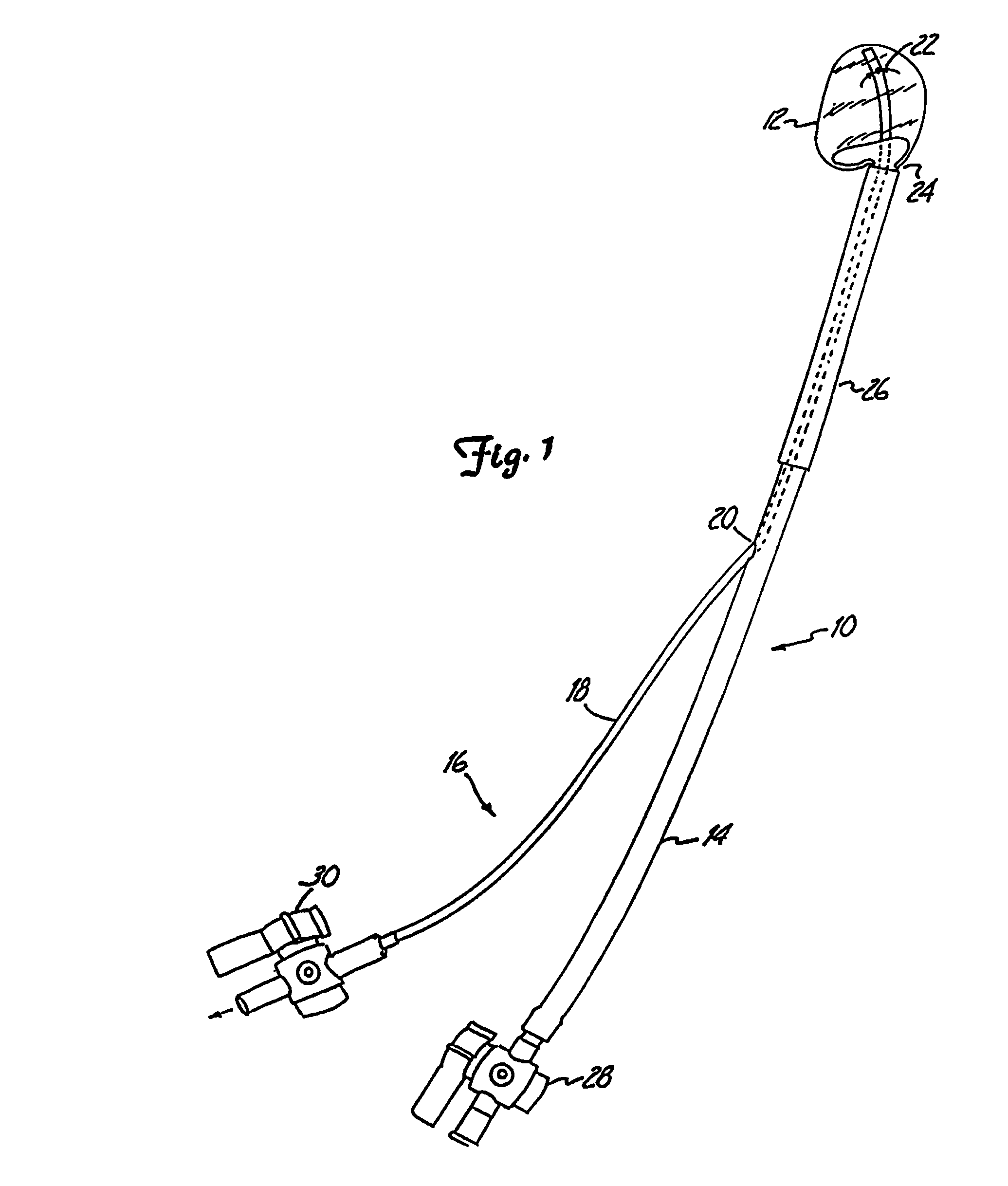
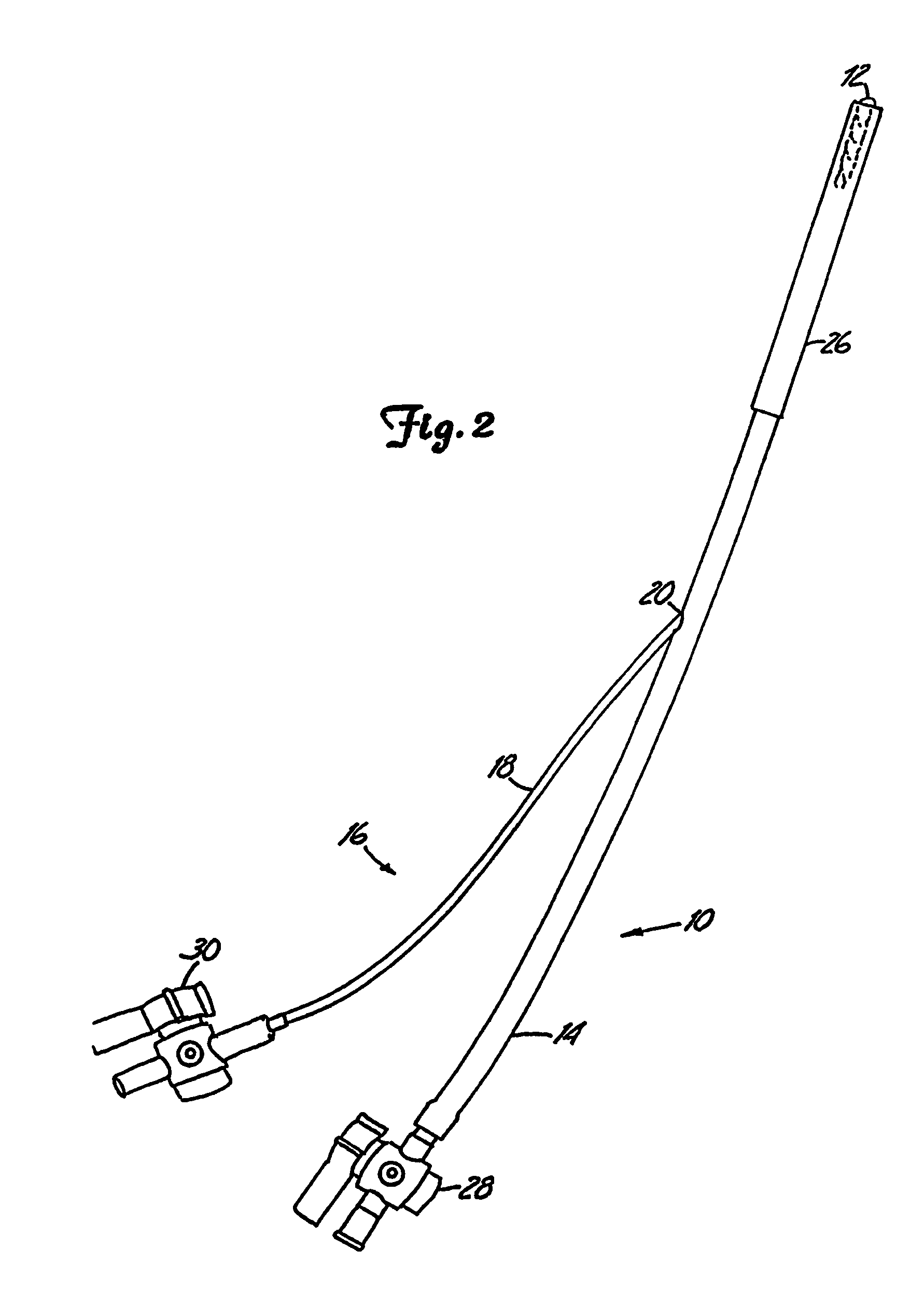
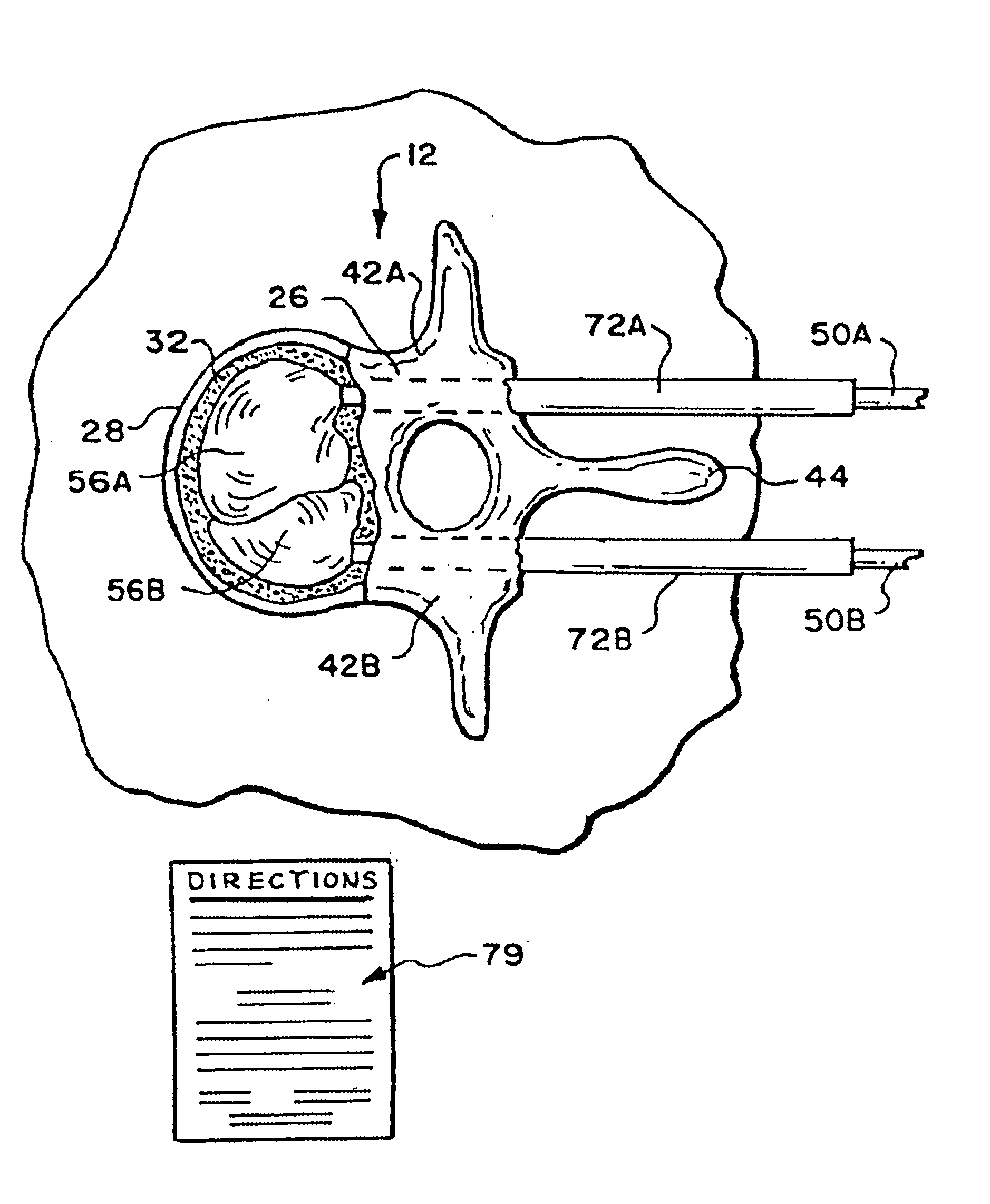
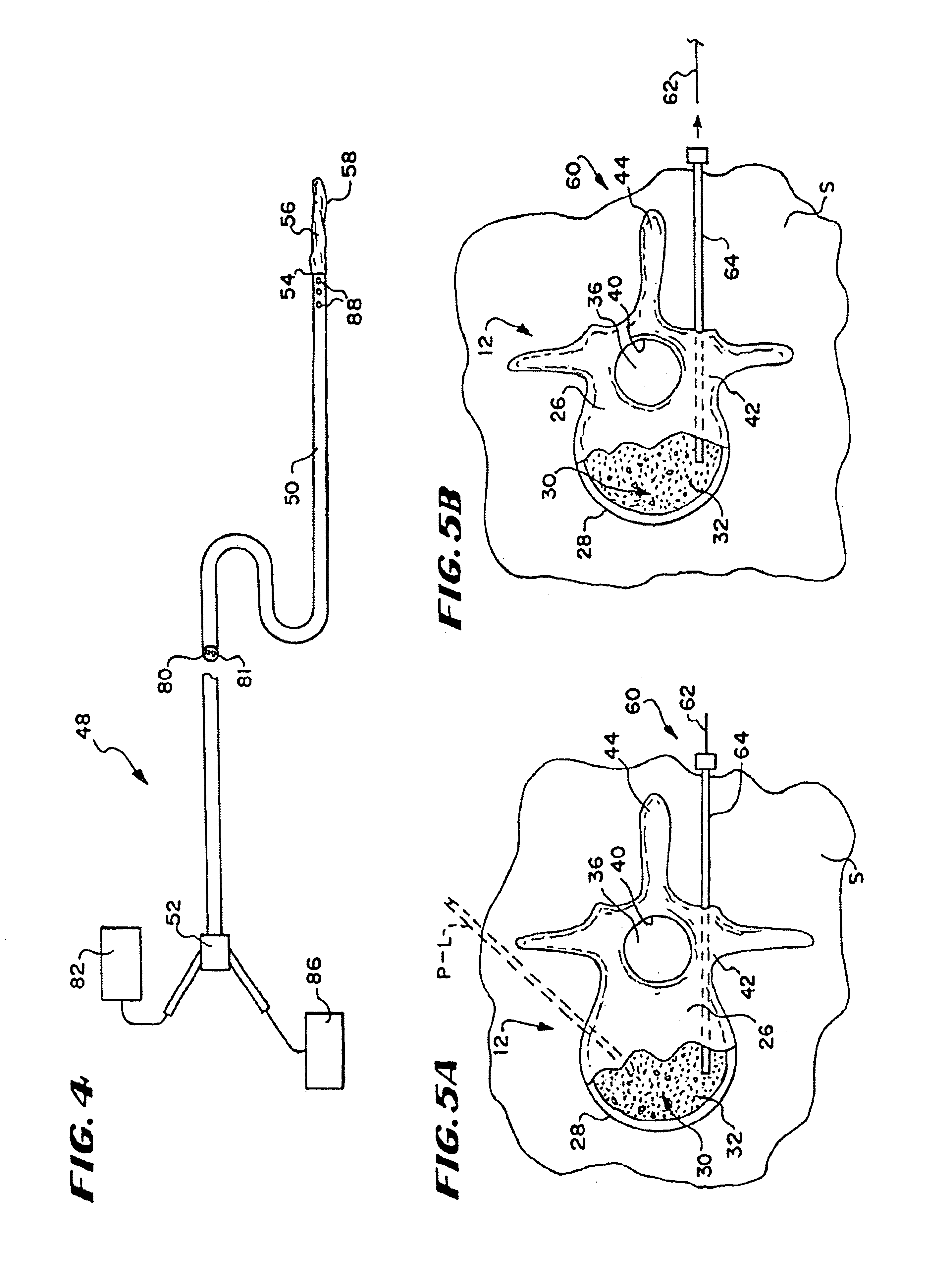
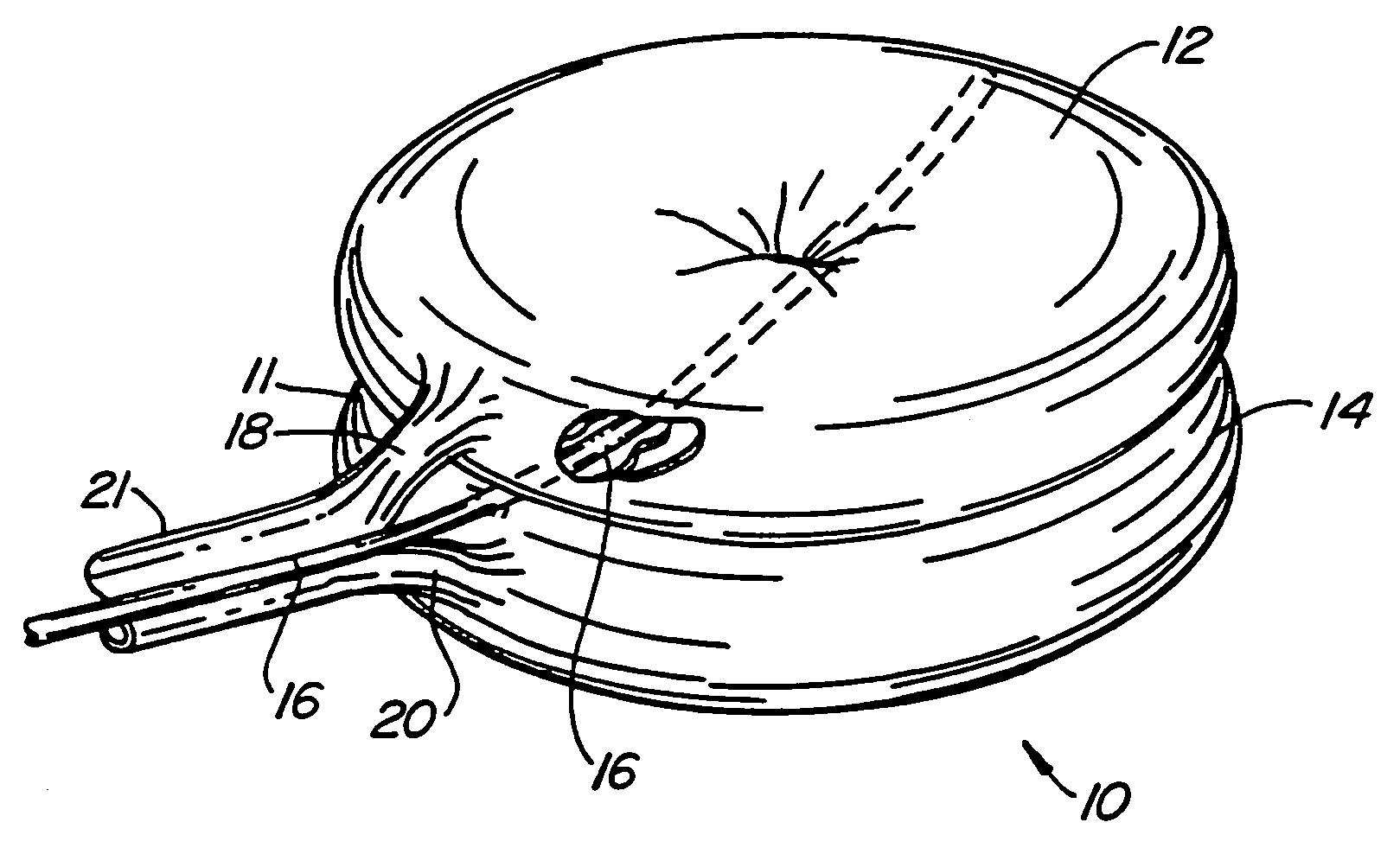
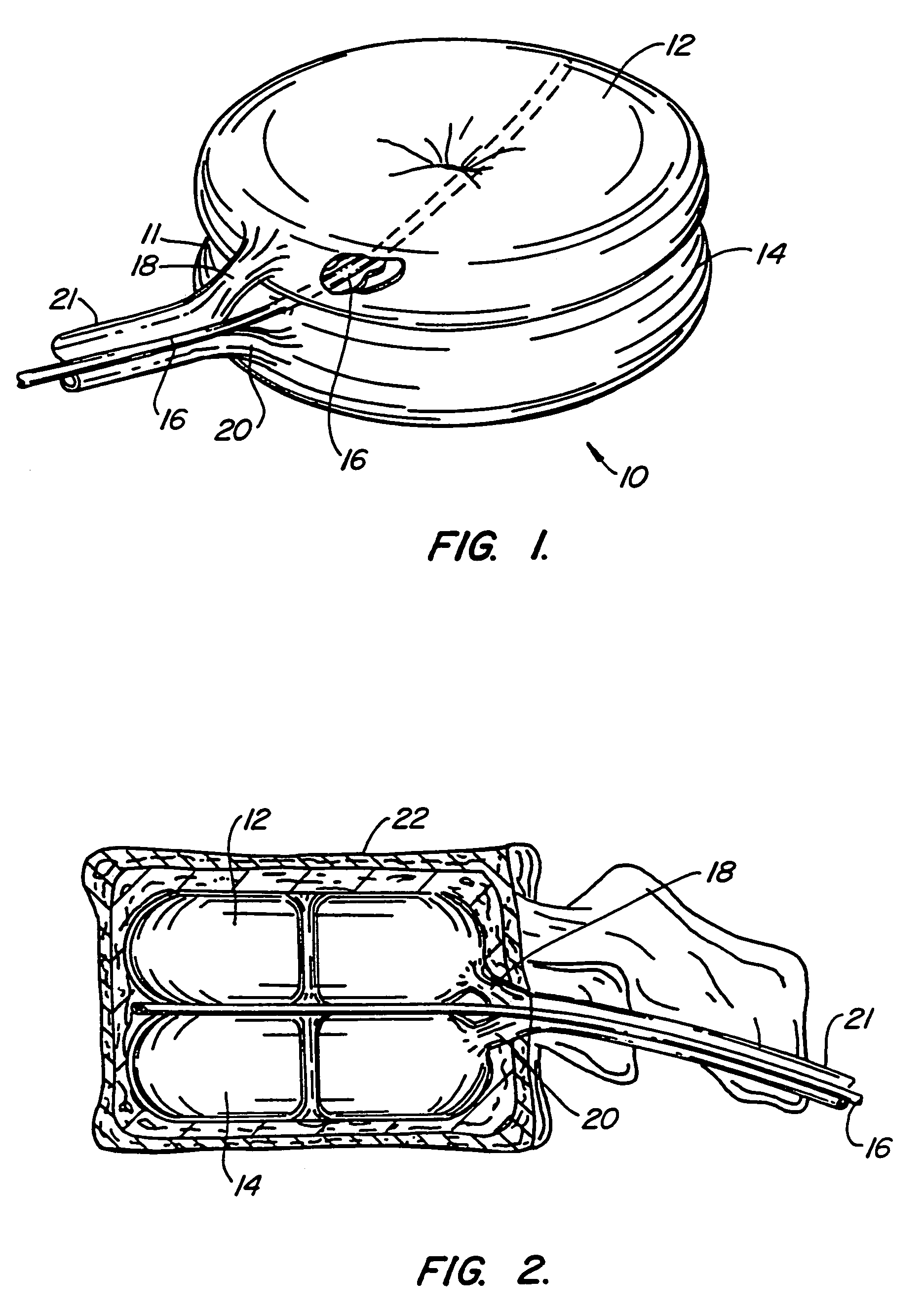
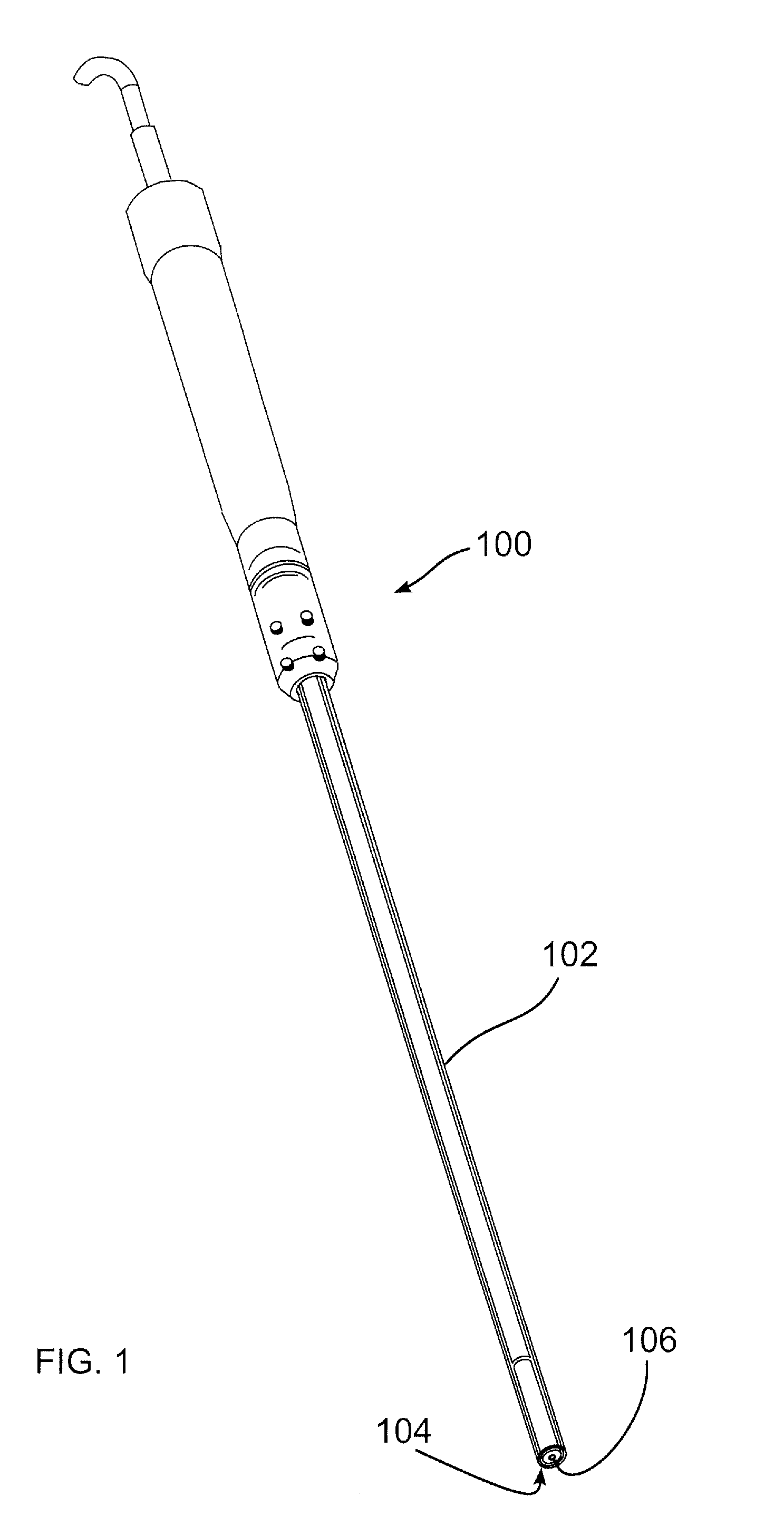
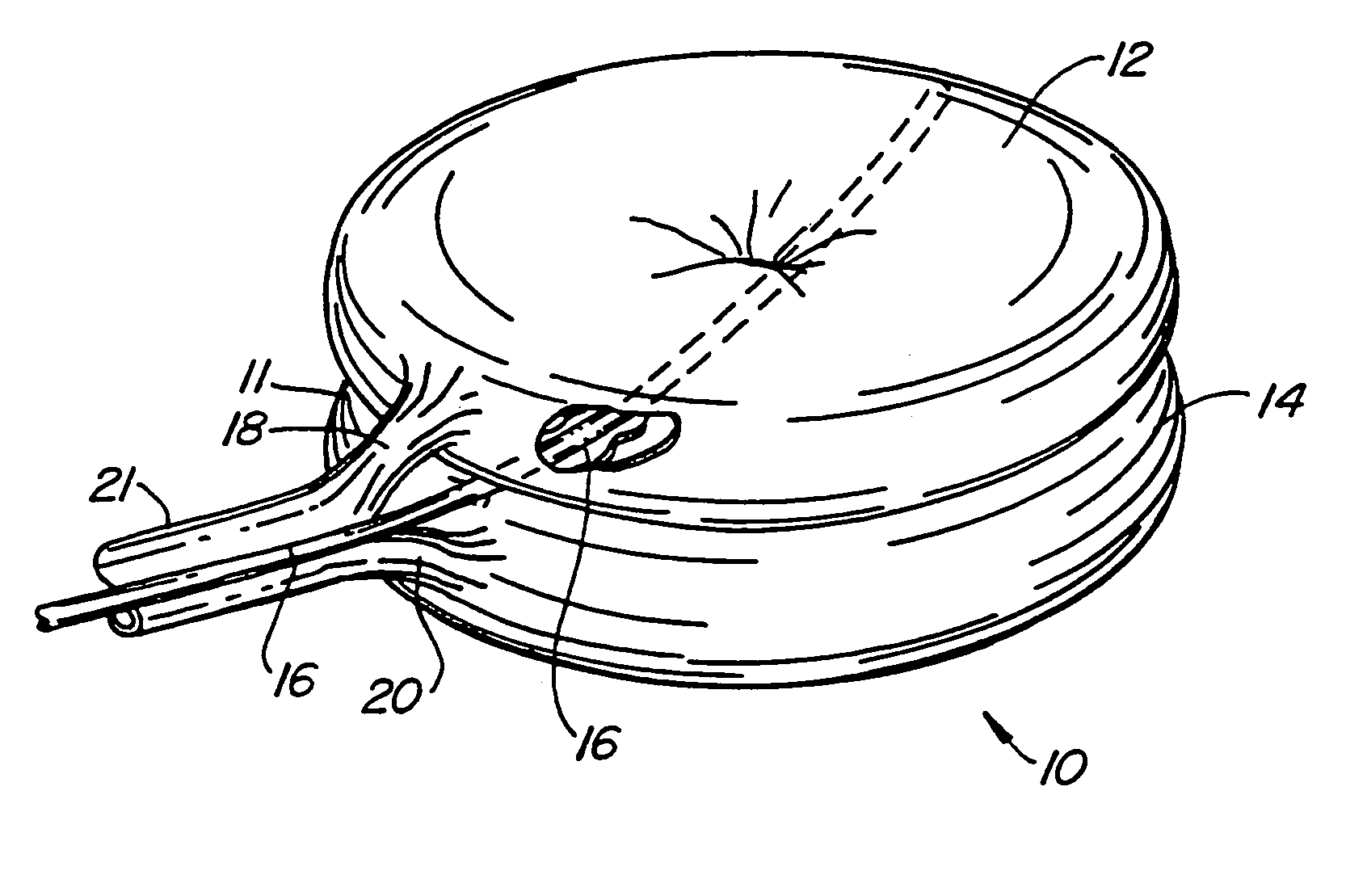
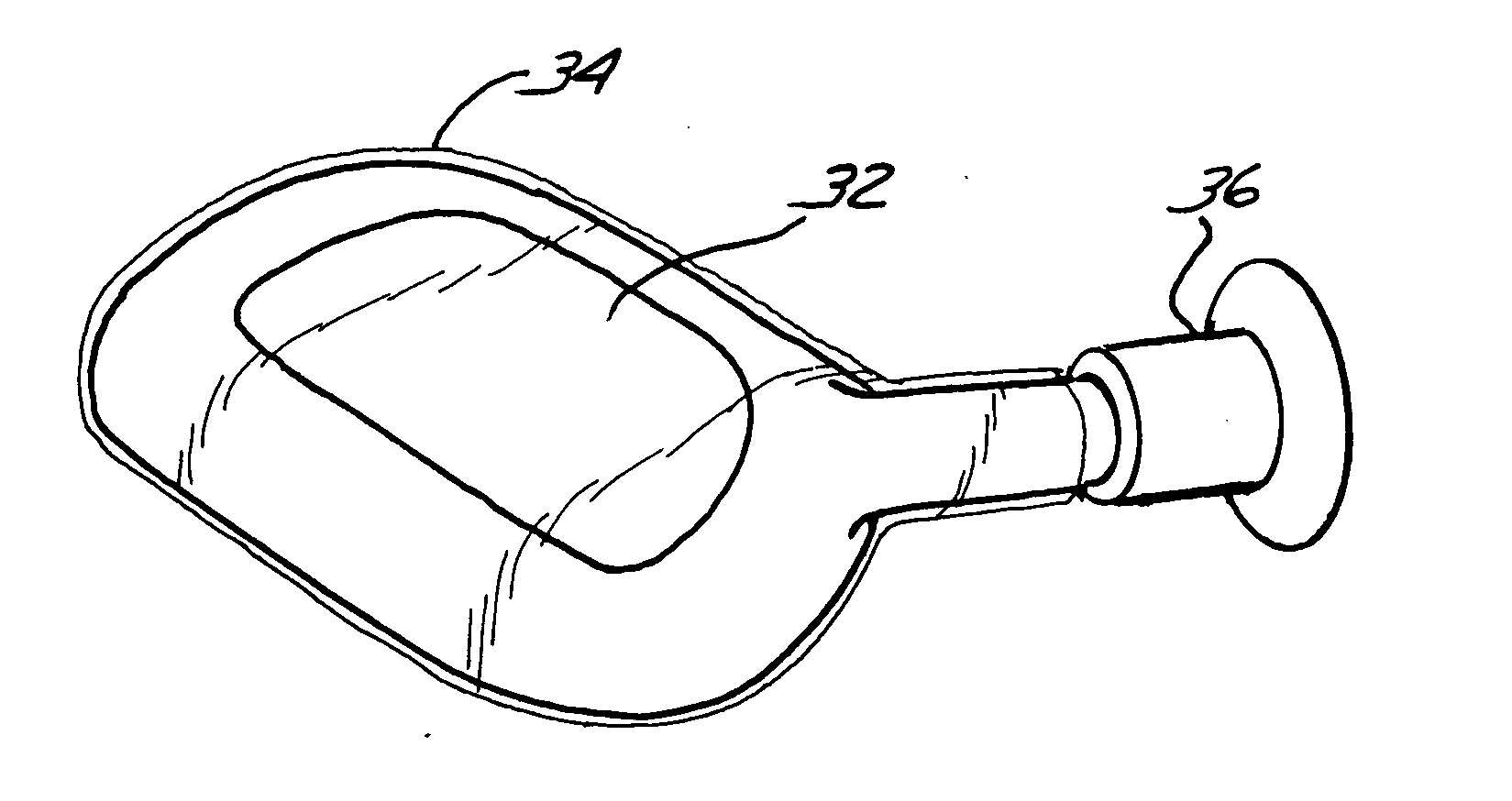
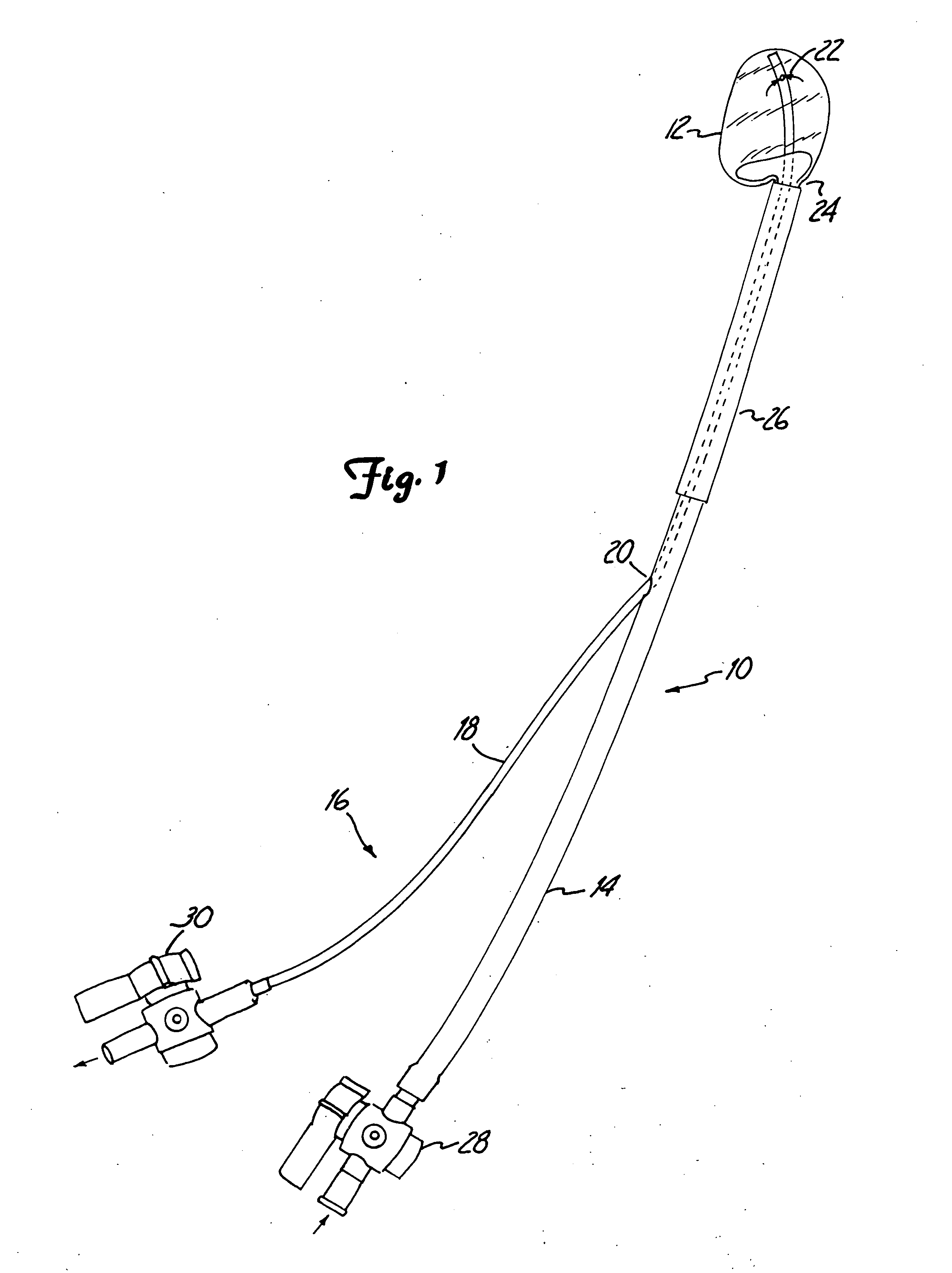
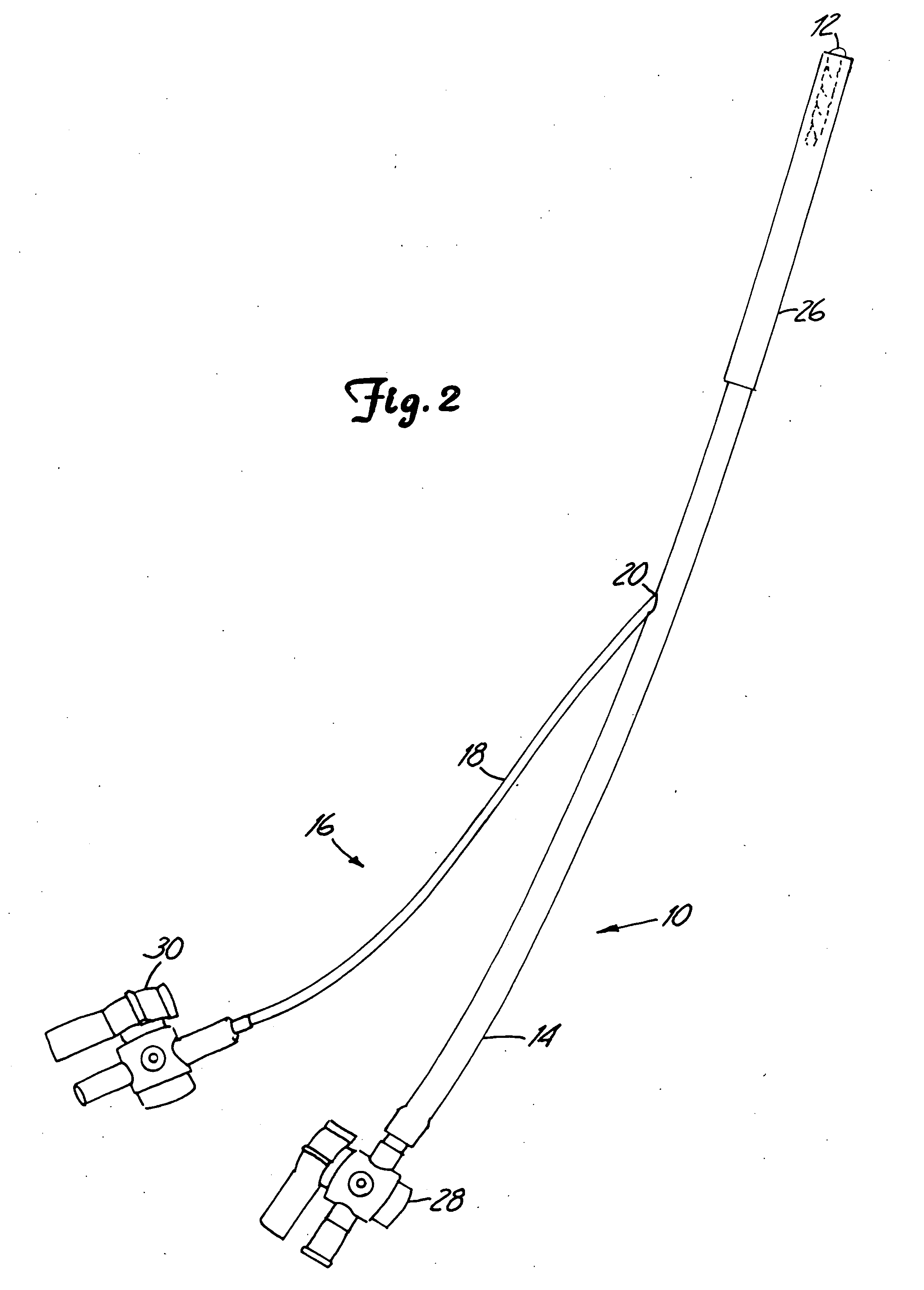
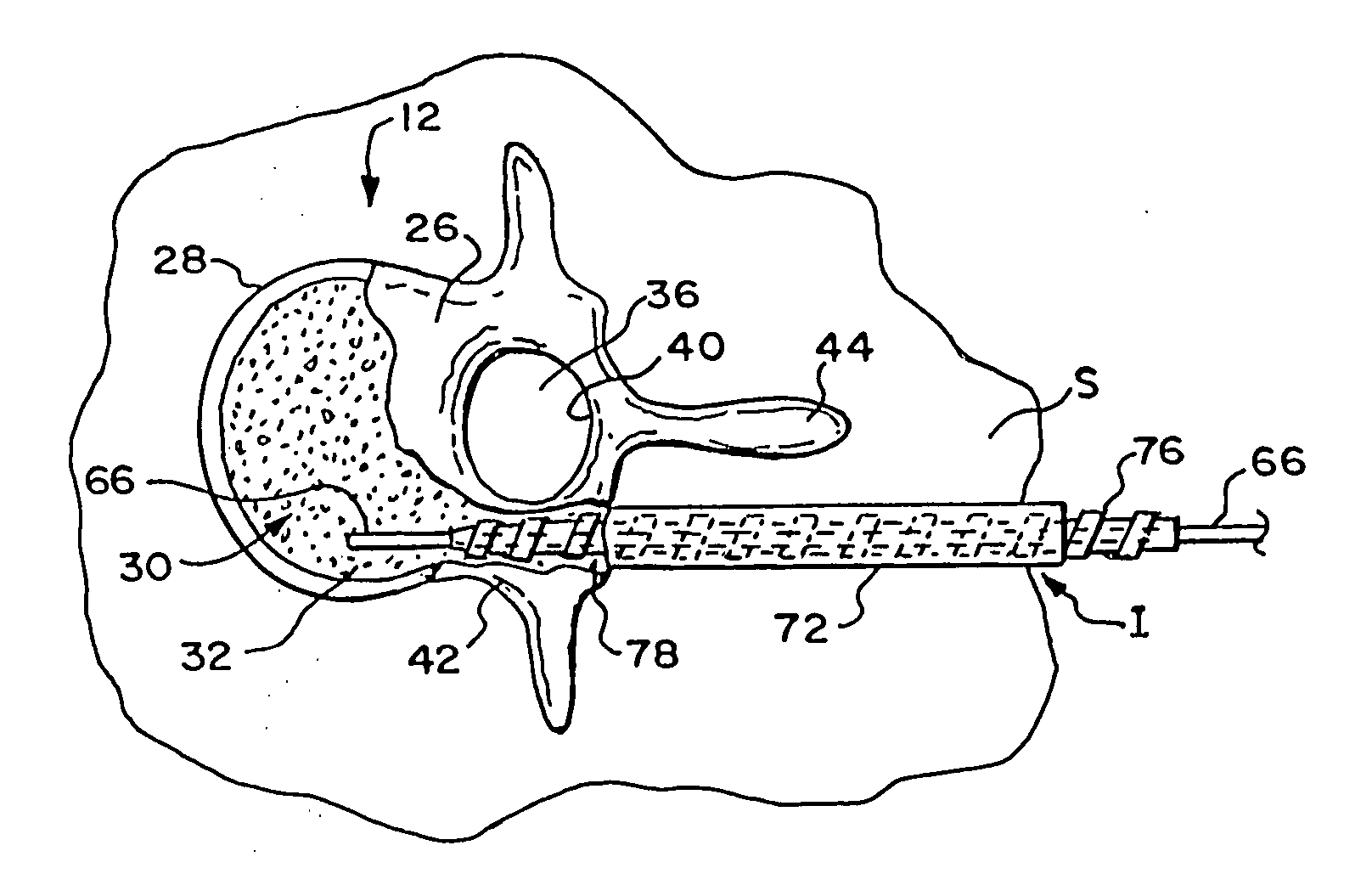
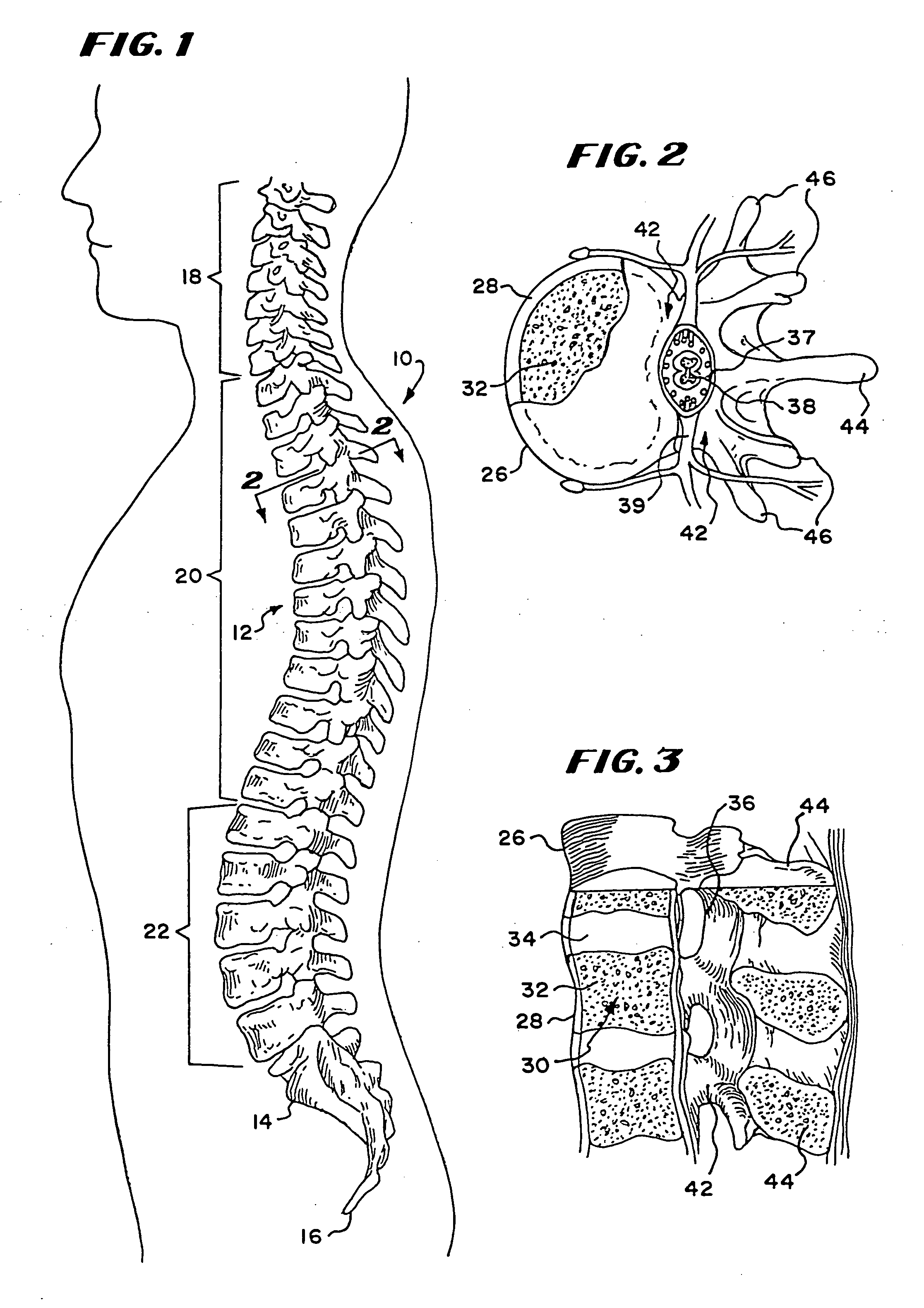
Intervertebral disc prosthesis
InactiveUS7001431B2Improved polymer cureImproved implant characteristicInternal osteosythesisAnkle jointsIntervertebral discPolymer
A system for repairing an intervertebral disc by delivering and curing a biomaterial in situ within the disc. The system includes both a device, having an insertable balloon and related lumen, controls and adapters, as well as an in situ curable biomaterial (and related biomaterial delivery means). The system can allow the doctor to determine a suitable endpoint for biomaterial delivery, by controlling distraction and / or biomaterial delivery pressure, and in turn, to deliver a desired quantity of biomaterial to the balloon in order to achieve improved polymer cure and implant characteristics. Also provided is a related method for repairing an intervertebral disc by using such a system to deliver and cure the biomaterial in situ. The system can be used to implant a prosthetic total disc, or a prosthetic disc nucleus in a manner that leaves the surrounding disc tissue substantially intact.
Owner:DISC DYNAMICS
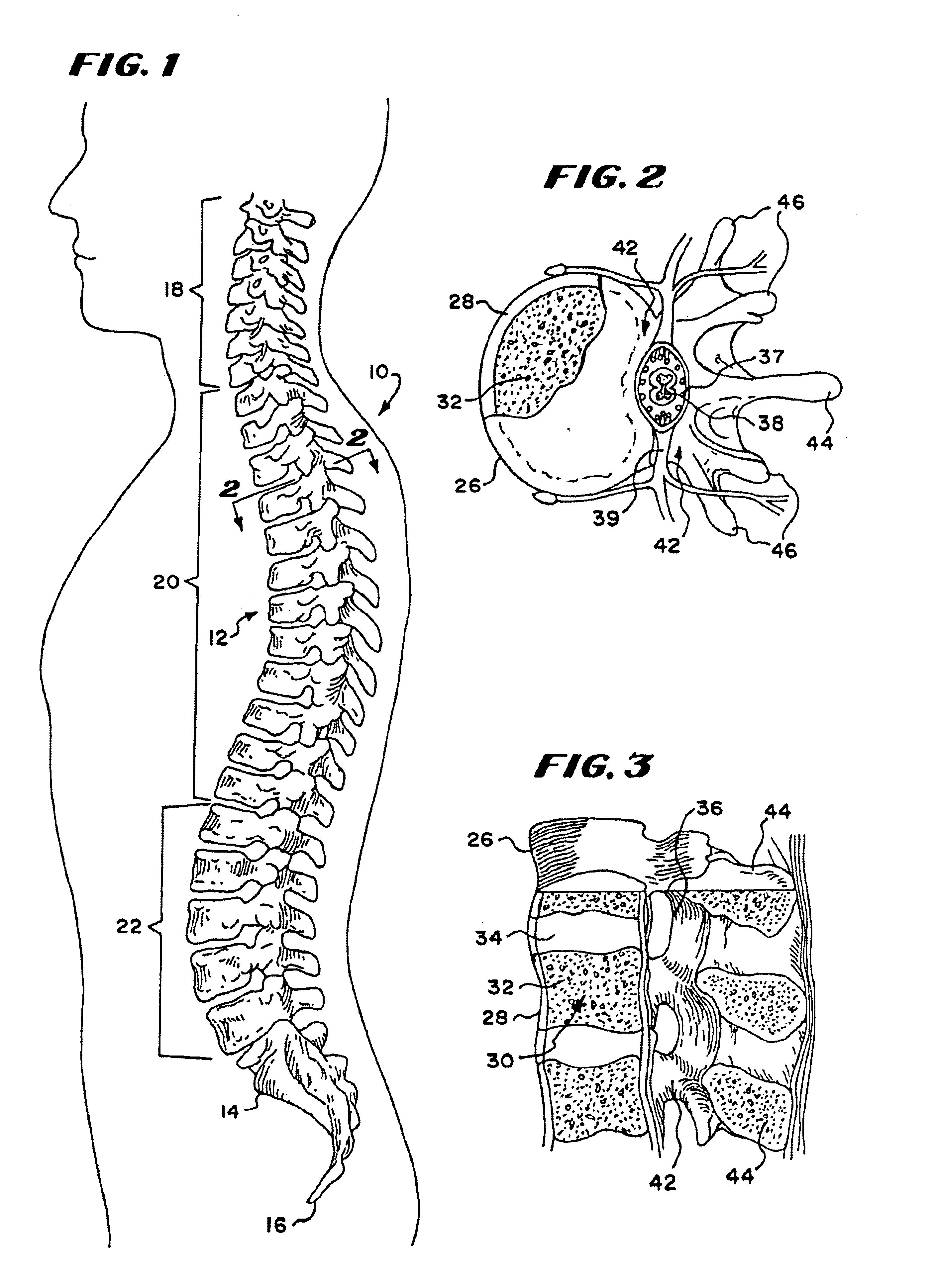
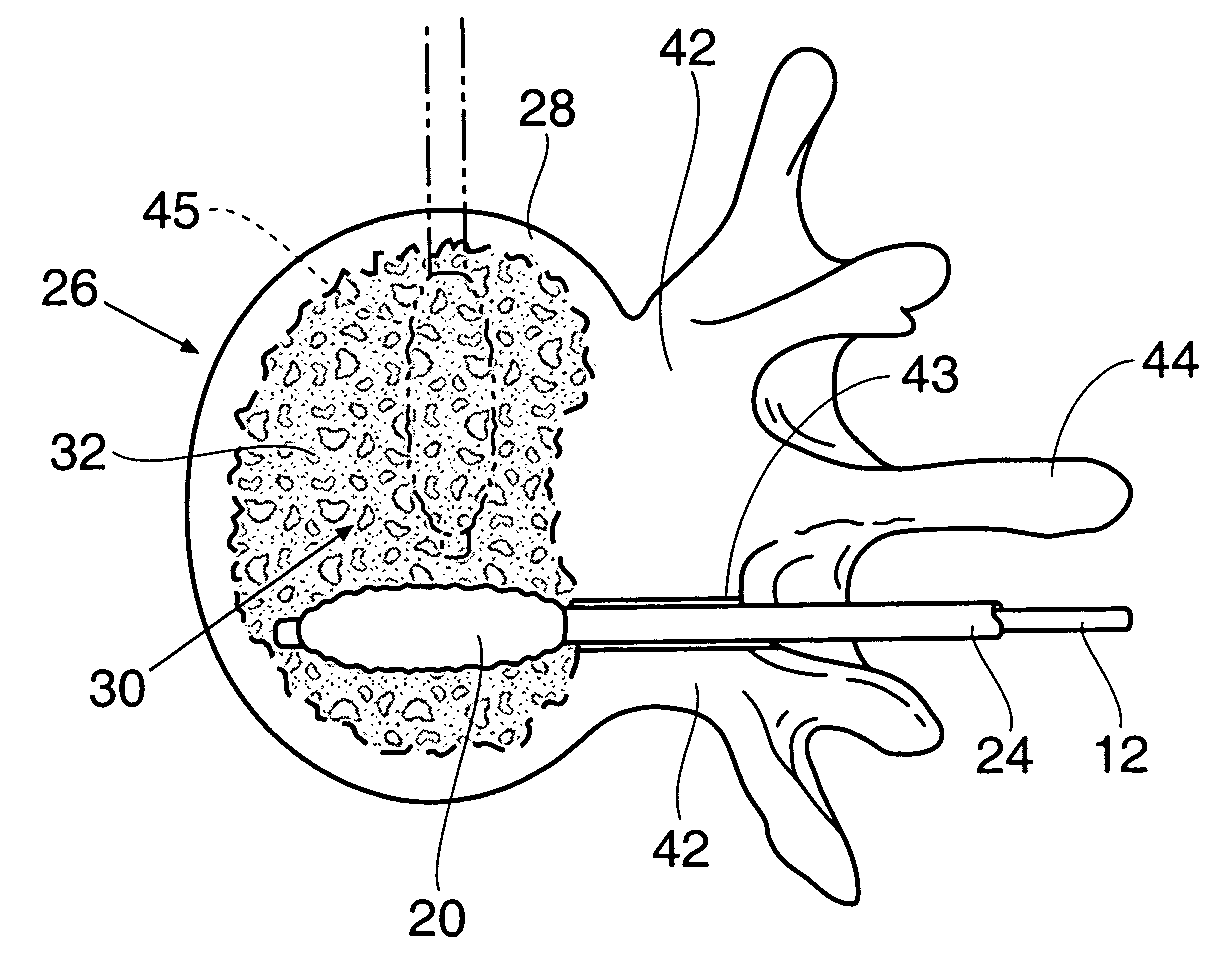
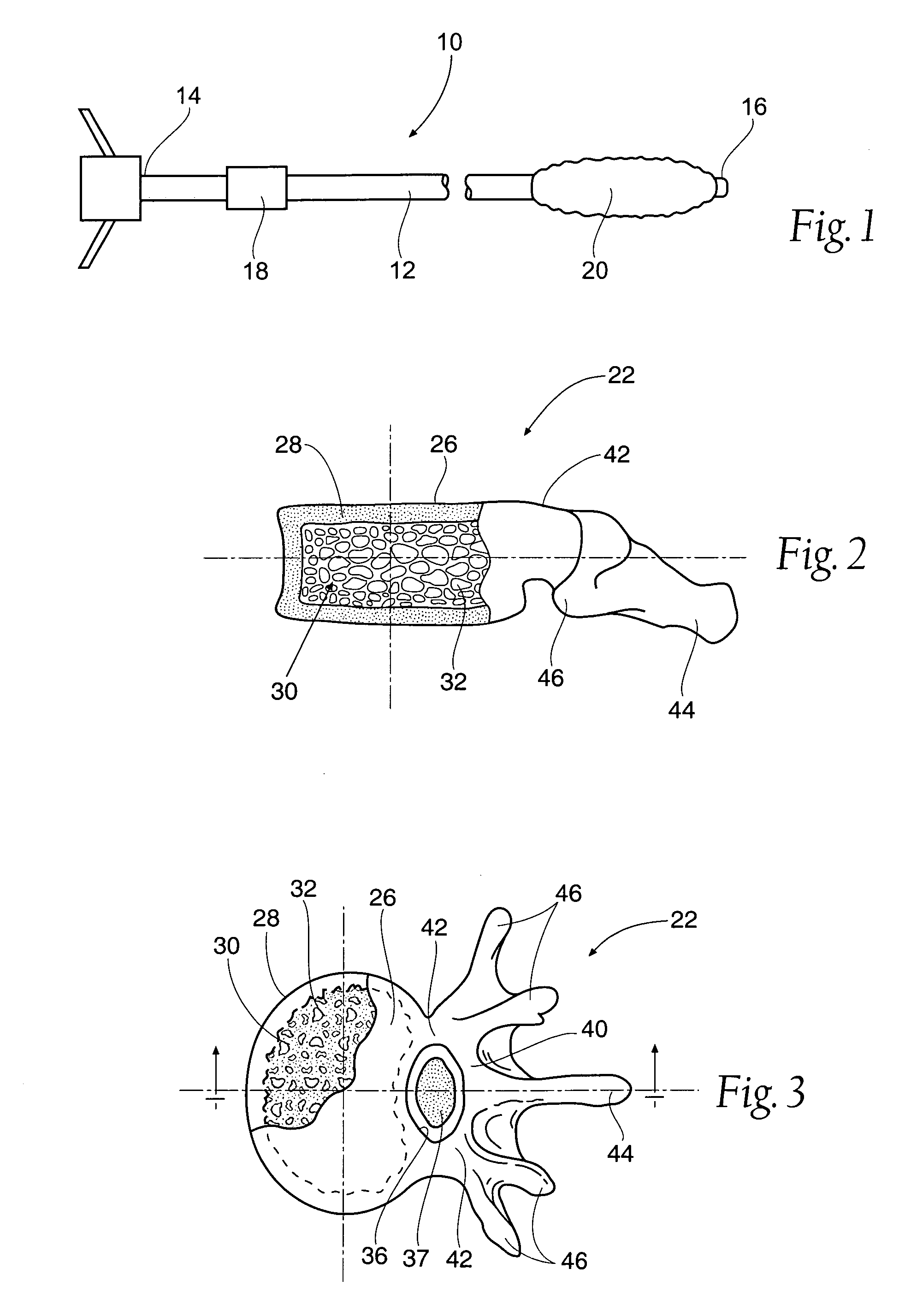
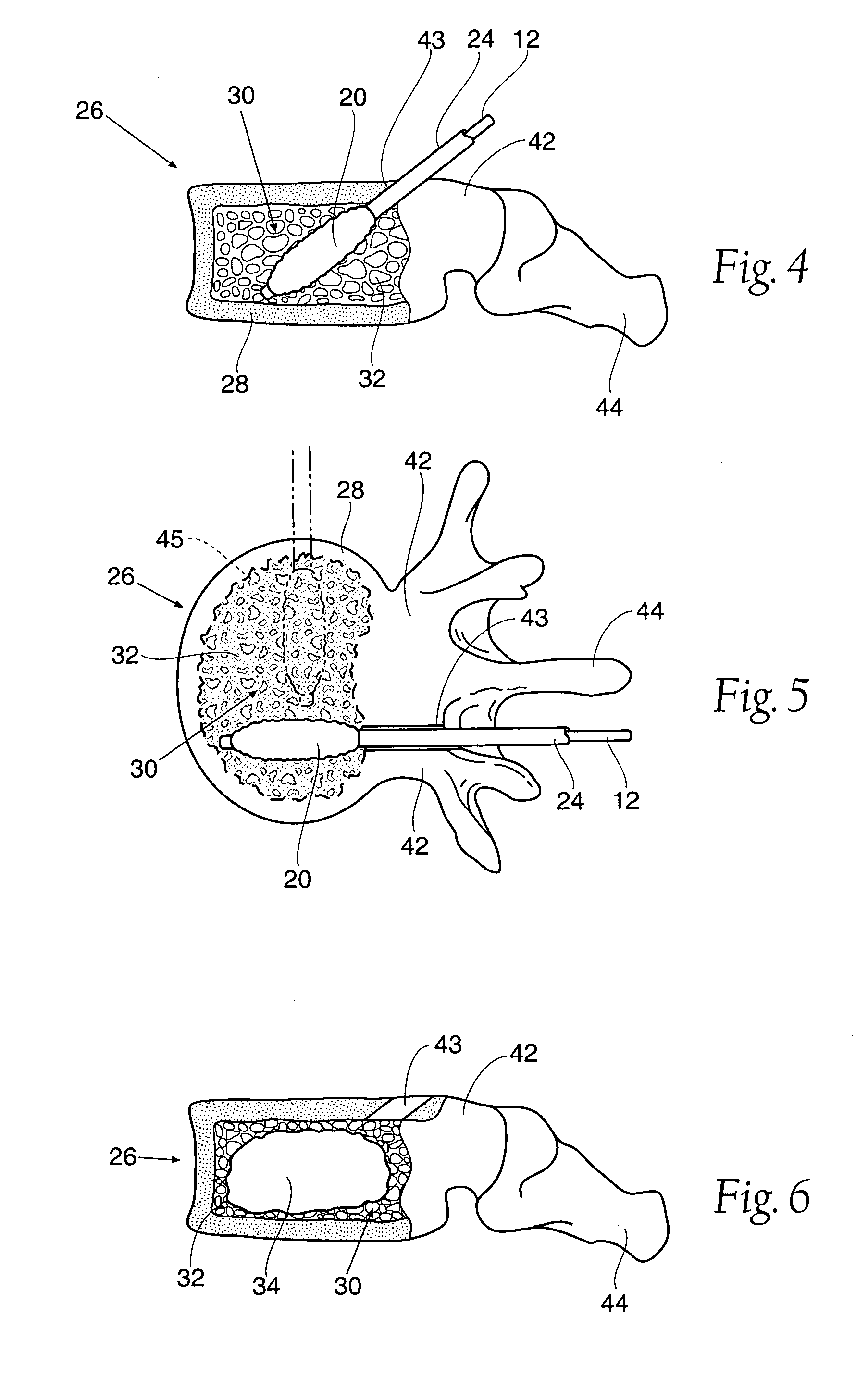
Inflatable device for use in surgical protocol relating to fixation of bone
InactiveUS6981981B2Improve clinical outcomesWorsen conditionSurgical furnitureInternal osteosythesisFilling materialsCancellous bone
Systems for treating a bone, e.g. a vertebral body, having an interior volume occupied, at least in part, by cancellous bone provide a first tool, a second tool, and a third tool. The first tool establishes a percutaneous access path to bone. The second tool is sized and configured to be introduced through the percutaneous access path to form a void that occupies less than the interior volume. The third tool places within the void through the percutaneous access path a volume of filling material. Related methods for treating a bone, e.g. a vertebral body, having an interior volume occupied, at least in part, by cancellous bone provide establishing a percutaneous access path to bone. A tool is introduced through the percutaneous access path and manipulated to form a void that occupies less than the interior volume. A volume of filling material is then placed within the void through the percutaneous access path.
Owner:ORTHOPHOENIX
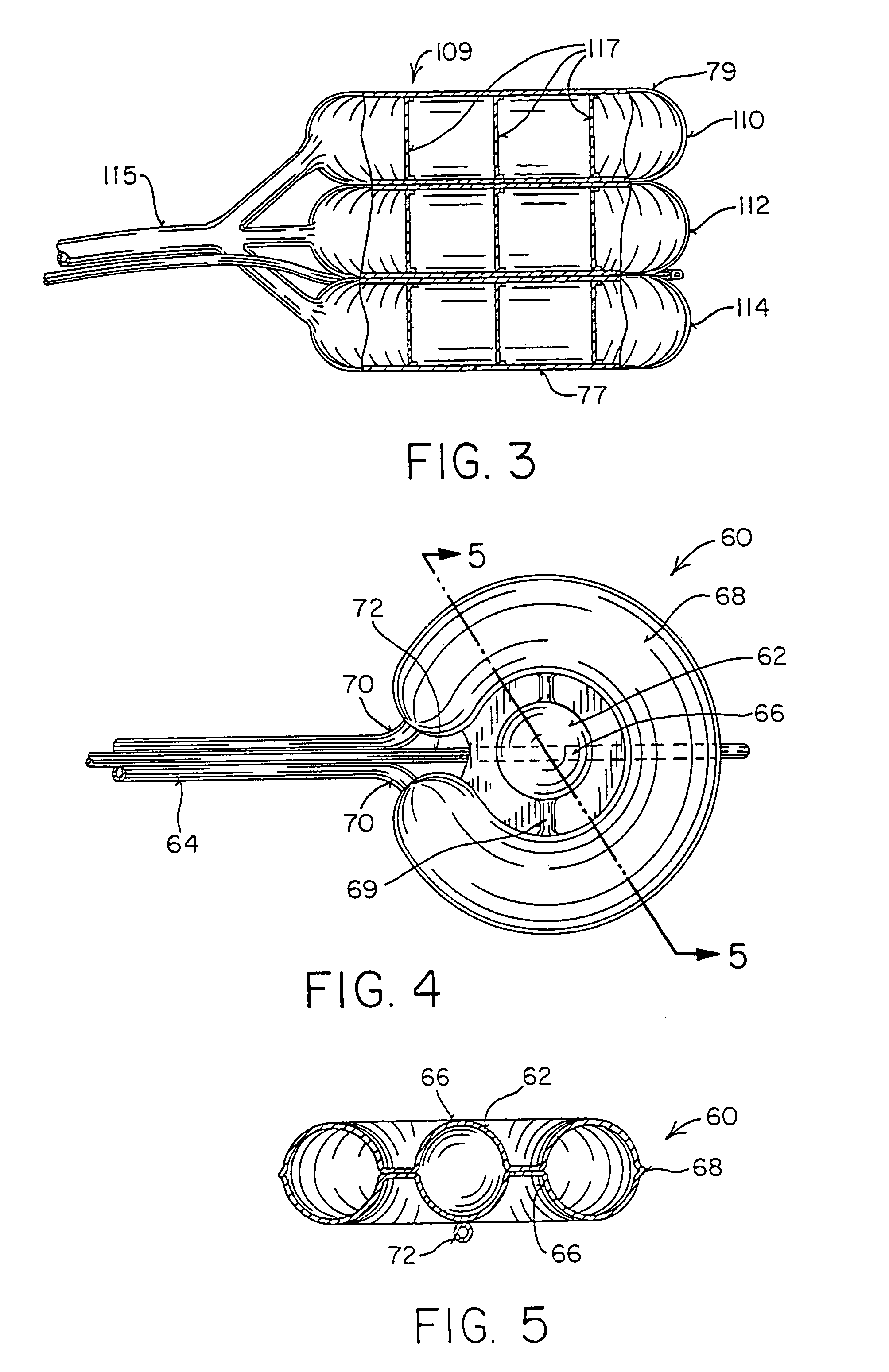
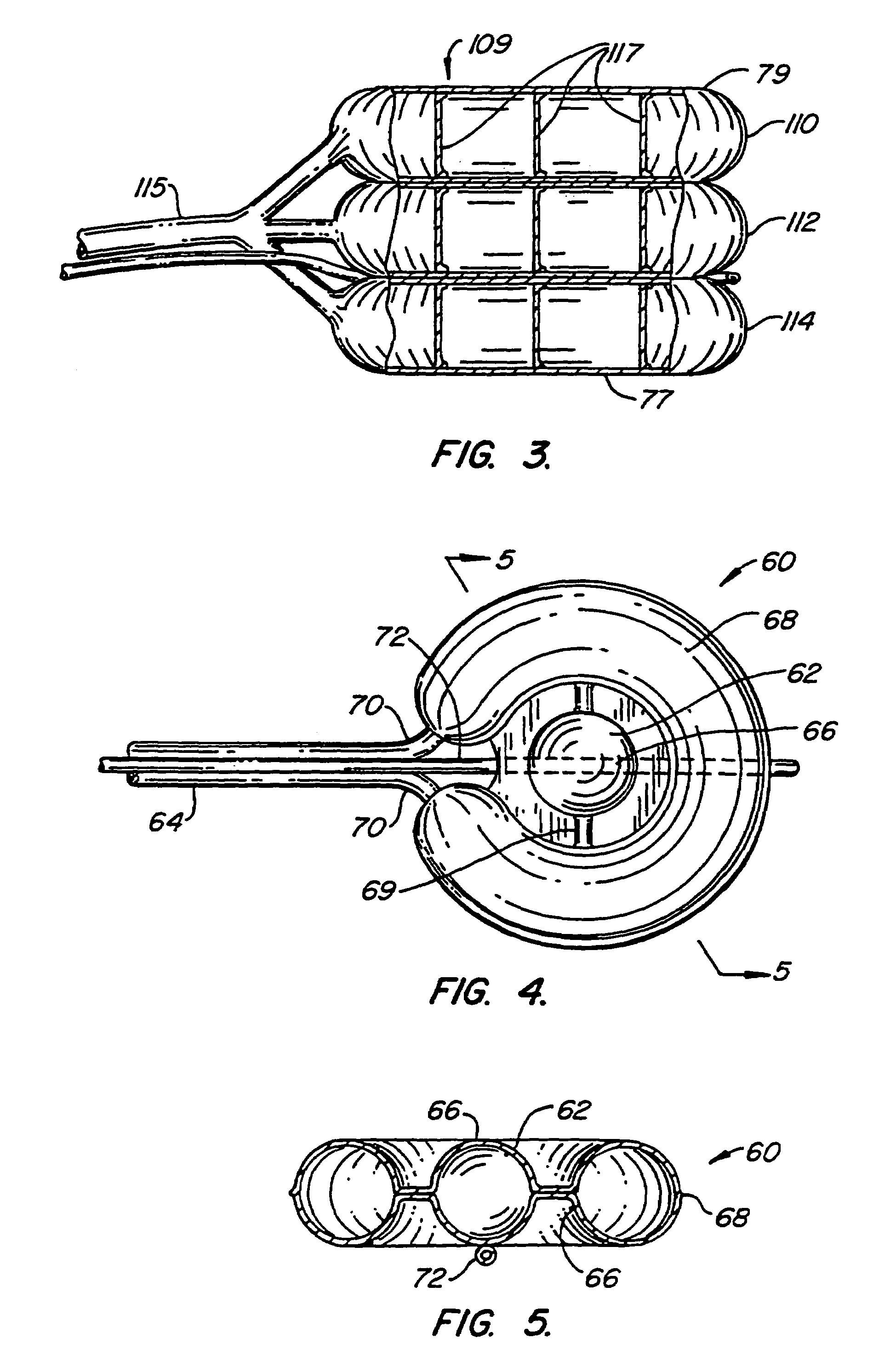
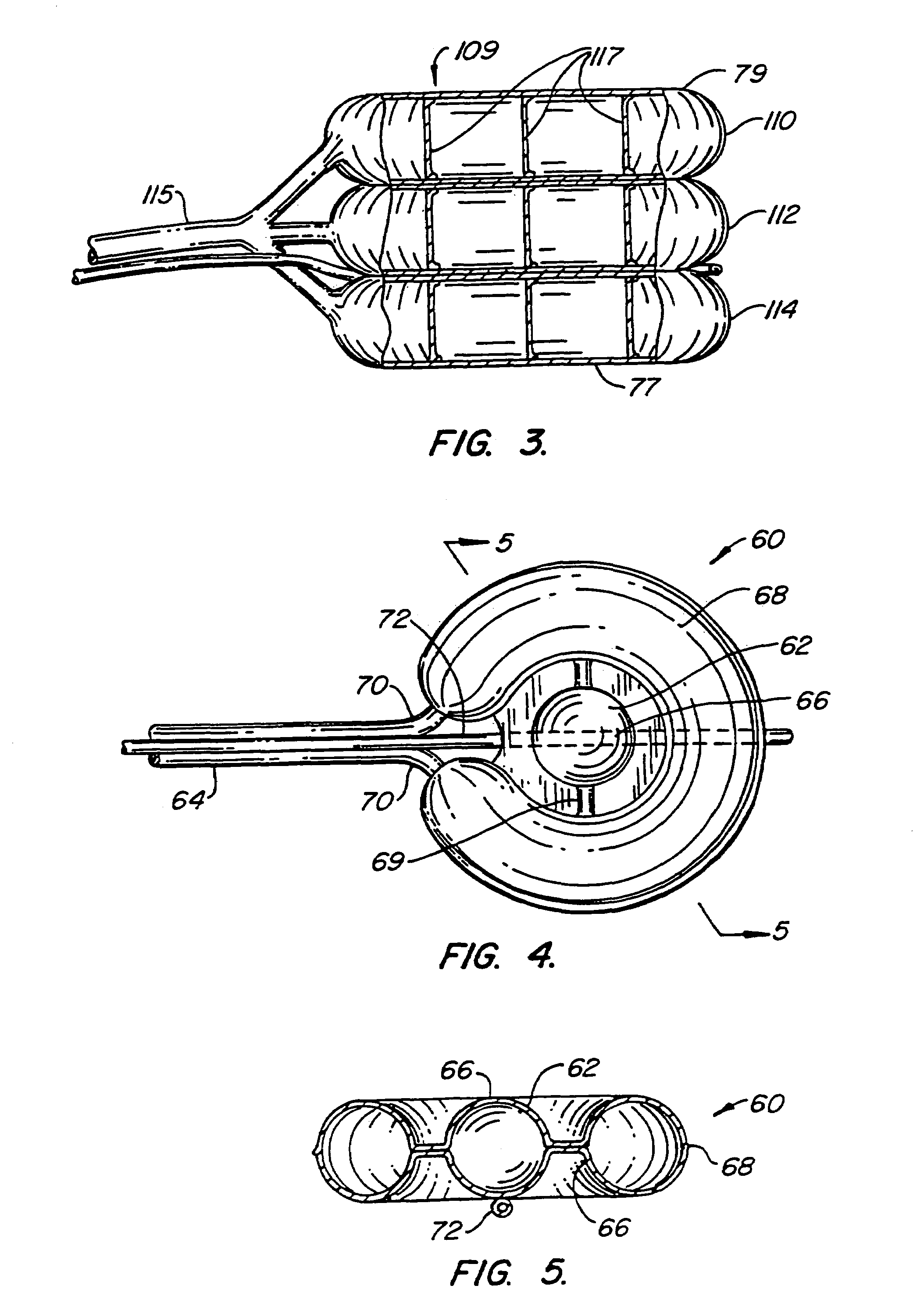
Systems and methods for treating fractured or diseased bone using expandable bodies
Systems and methods treat fractured or diseased bone by deploying more than a single therapeutic tool into the bone. In one arrangement, the systems and methods deploy an expandable body in association with a bone cement nozzle into the bone, such that both occupy the bone interior at the same time. In another arrangement, the systems and methods deploy multiple expandable bodies, which occupy the bone interior volume simultaneously. Expansion of the bodies form cavity or cavities in cancellous bone in the interior bone volume.
Owner:ORTHOPHOENIX
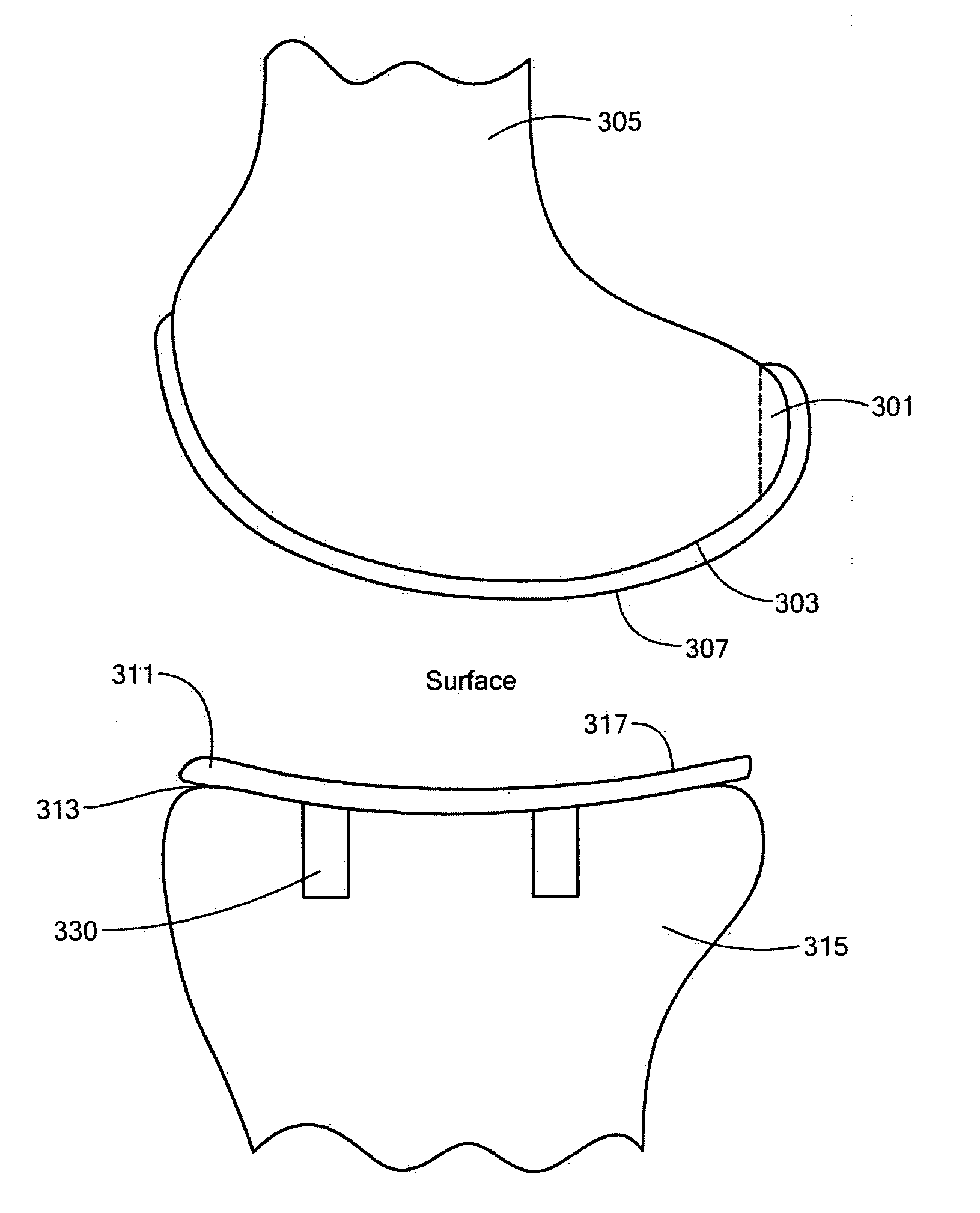
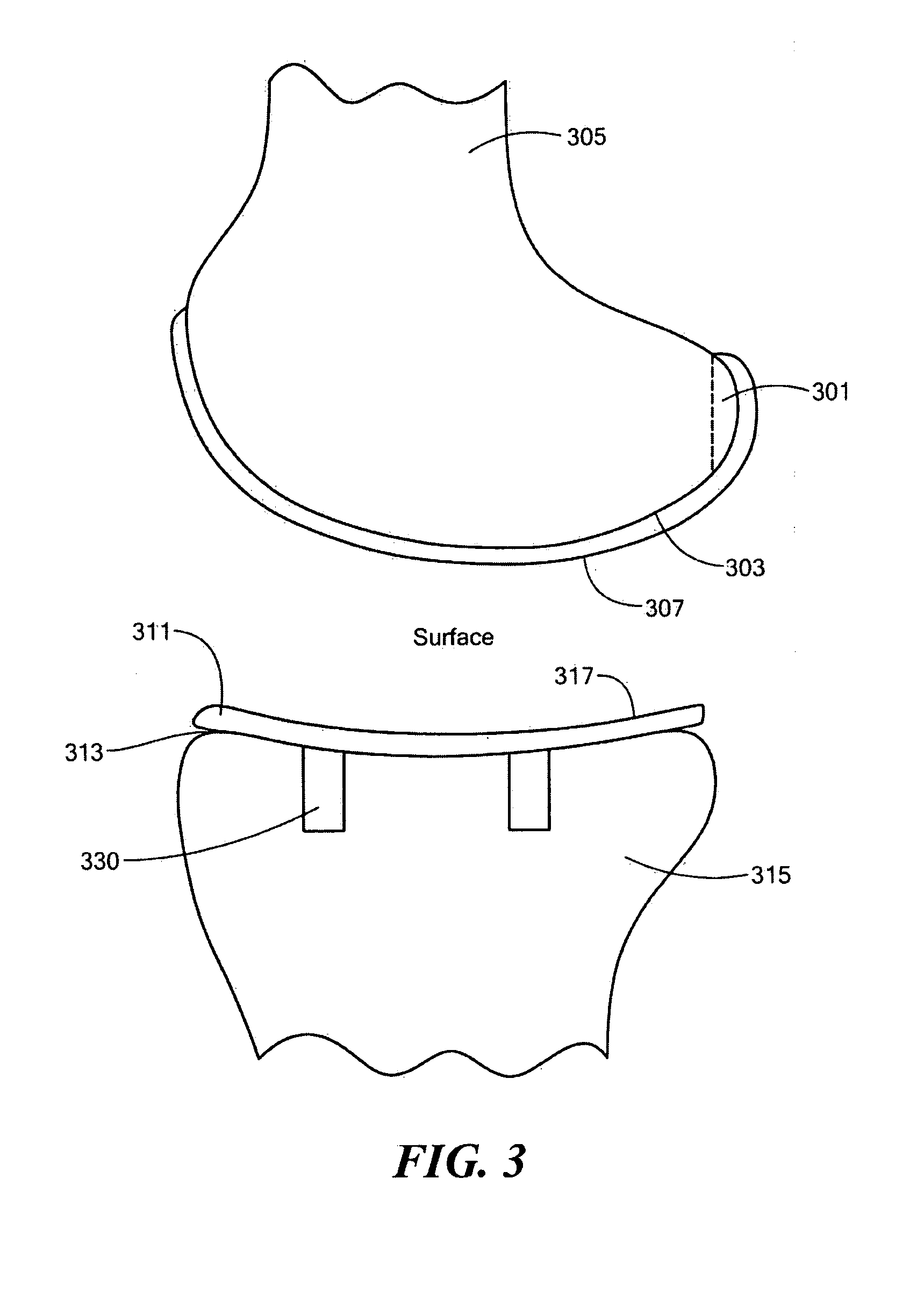
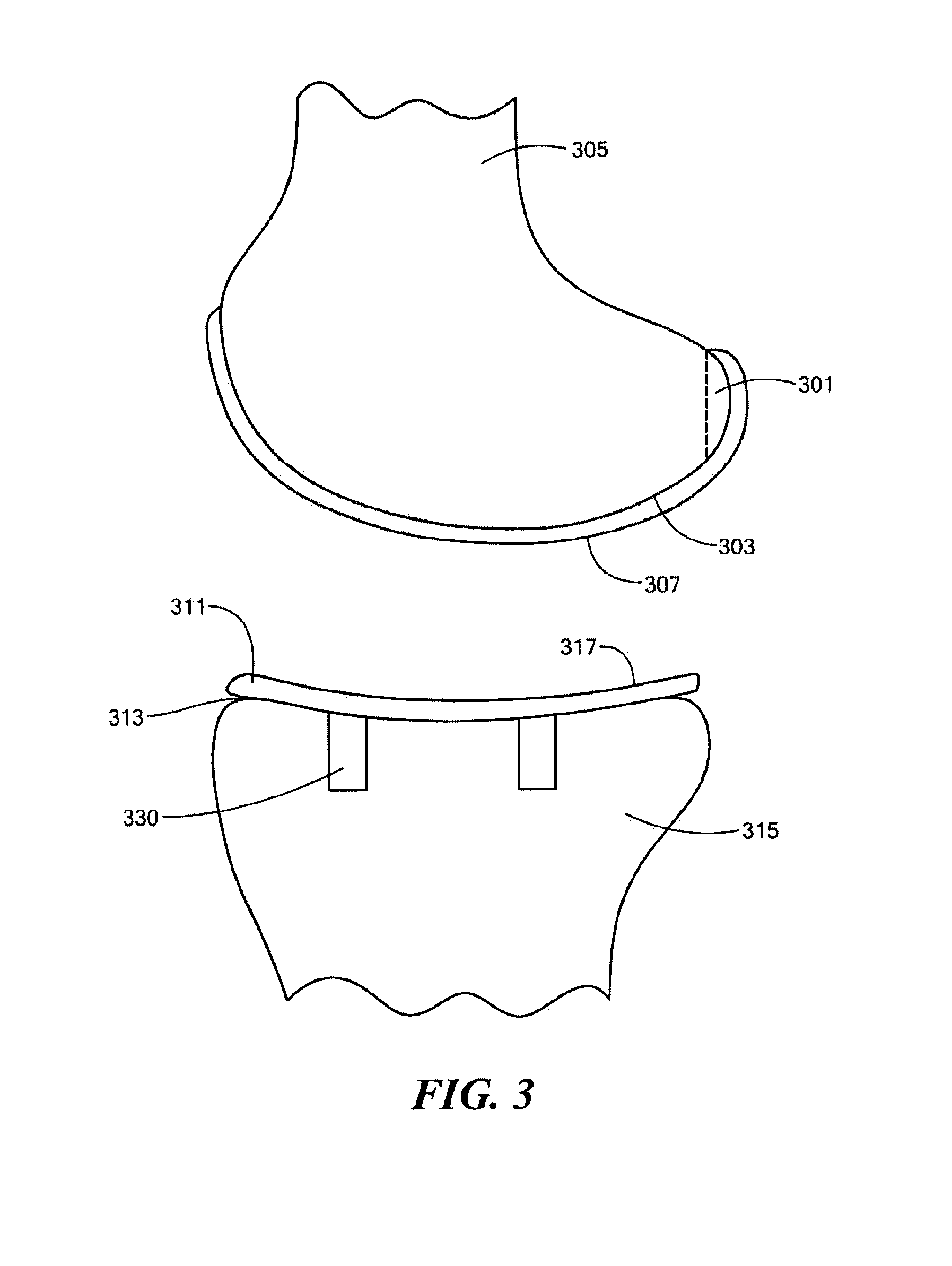
Implant Device and Method for Manufacture
A knee implant includes a femoral component having first and second femoral component surfaces. The first femoral component surface is for securing to a surgically prepared compartment of a distal end of a femur. The second femoral component surface is configured to replicate the femoral condyle. The knee implant further includes a tibial component having first and second tibial component surfaces. The first tibial component surface is for contacting a proximal surface of the tibia that is substantially uncut subchondral bone. At least a portion of the first tibial component surface is a mirror image of the proximal tibial surface. The second tibial component surface articulates with the second femoral component surface.
Owner:CONFORMIS
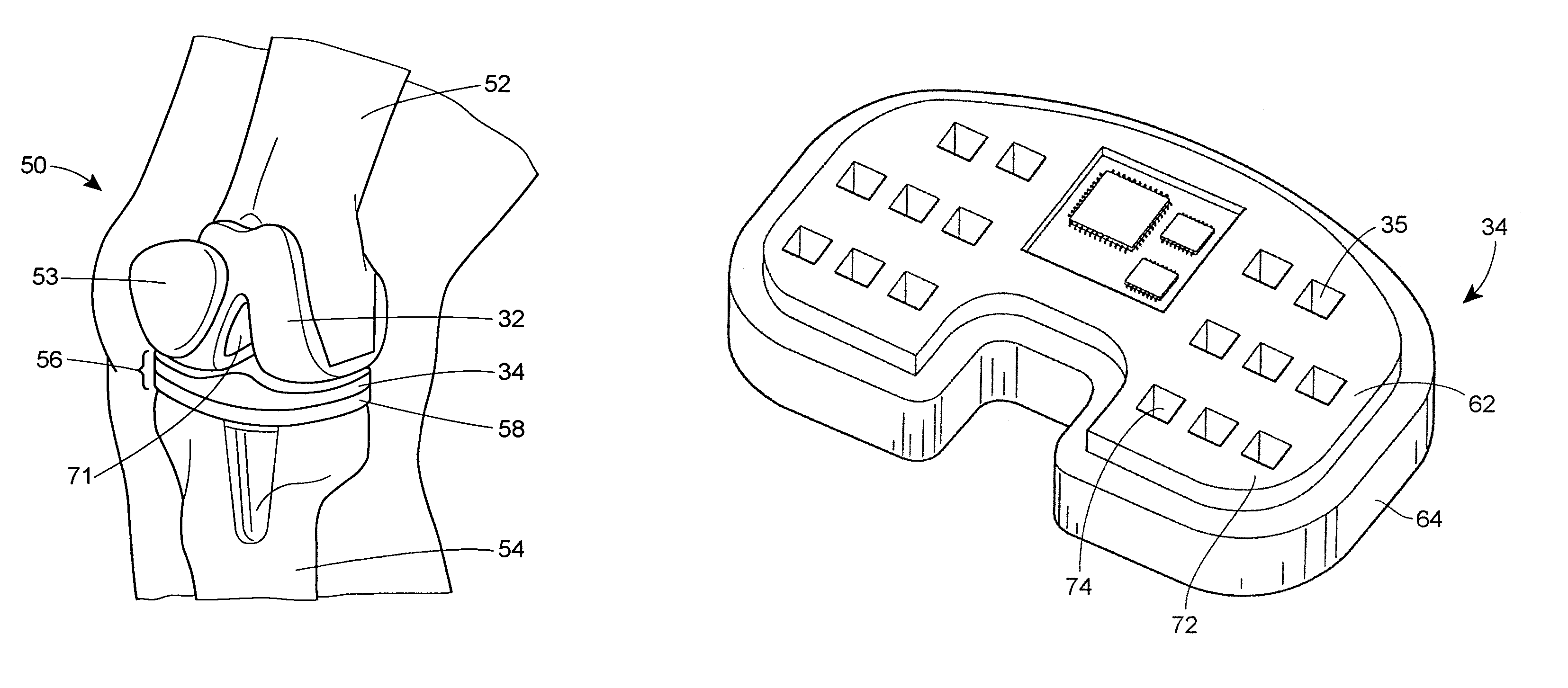
System and method for prosthetic fitting and balancing in joints
InactiveUS7575602B2Physical therapies and activitiesFinger jointsProsthesis fittingArtificial joints
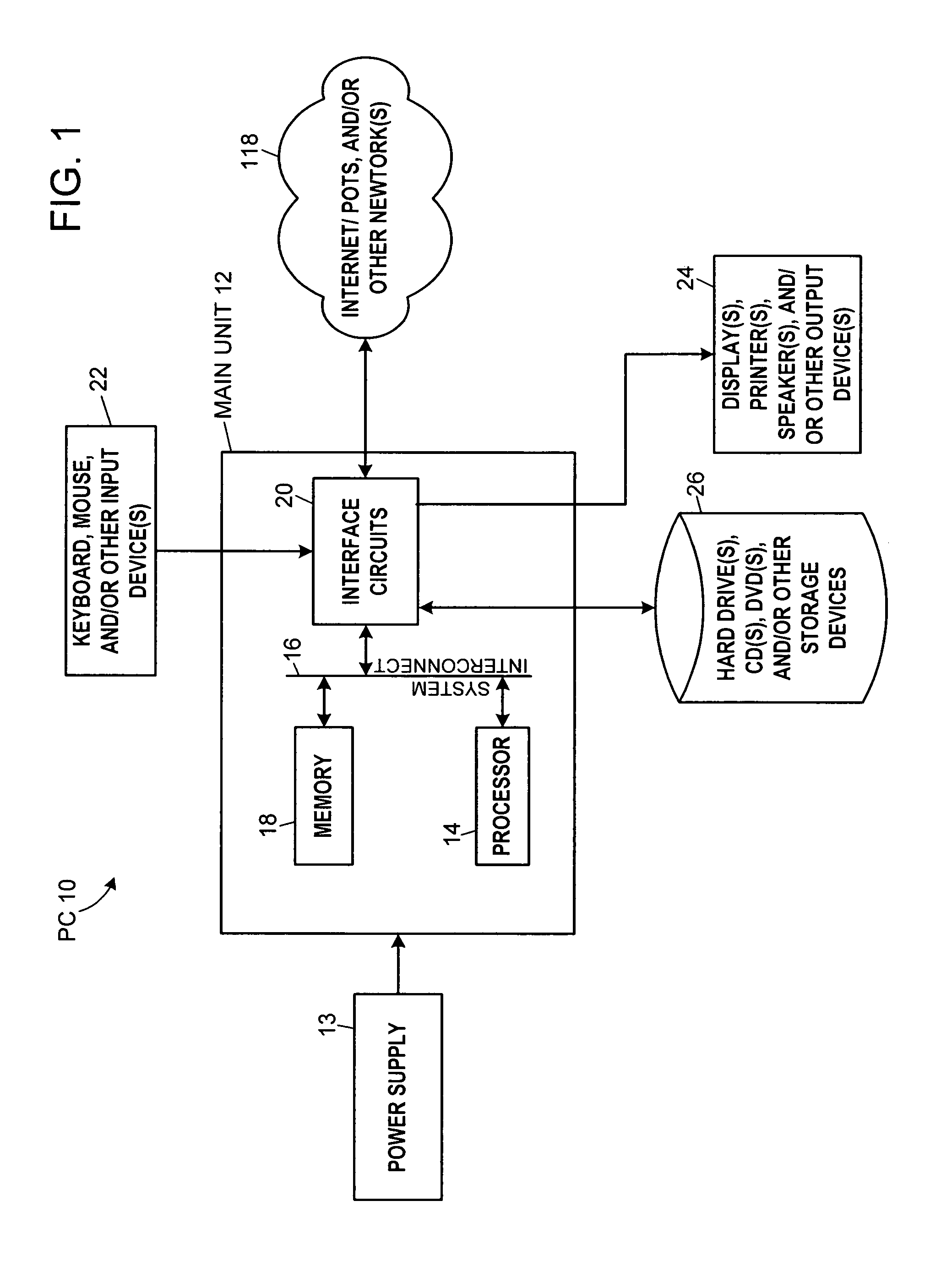
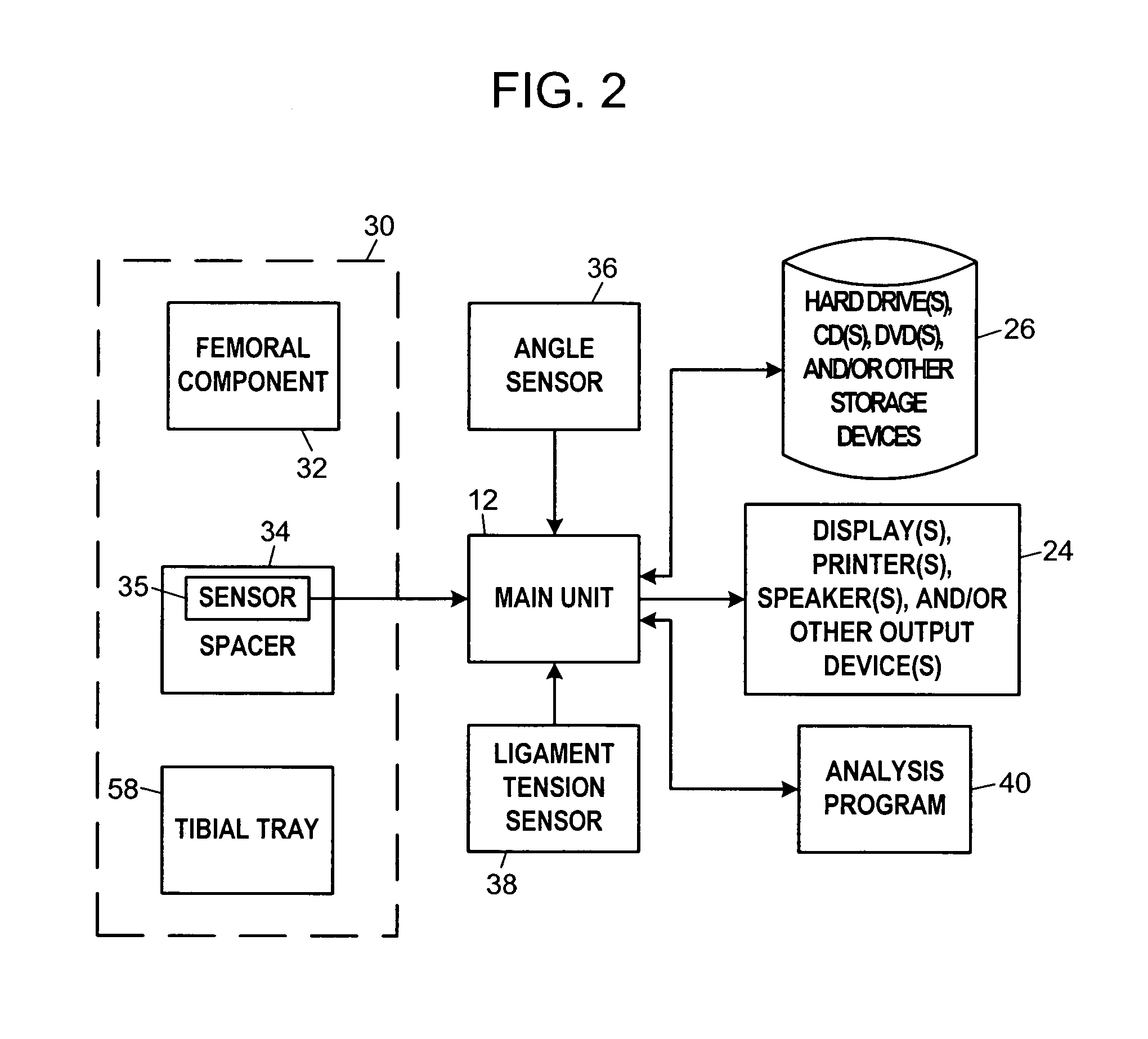
A system and method for prosthesis fitting in joints comprising an artificial condyle and a spacer which cooperates with the condyle to form an artificial joint. The spacer embedded with at least one sensor which is responsive to a force generated between the condyle and the spacer. The artificial joint is adapted to move between a flexed position and an extended position defining a range of motion. The sensor is responsive to the force and generates an output representative of that force. The output is transmitted, either wirelessly or other, to a processor which utilizes an analysis program to display a representation of the forces applied. A practitioner utilizing the displayed analysis may intraoperatively determine the adjustments and balancing required within the artificial joint. The system may also utilize a ligament tension sensor which generates data representative of tension on a ligament of the artificial joint, and a joint angle sensor responsive to the range of motion of the artificial joint. The processor may be adapted to store the outputted sensor data to provide the practitioner with statistically relevant historical data.
Owner:THE BOARD OF TRUSTEES OF THE UNIV OF ILLINOIS
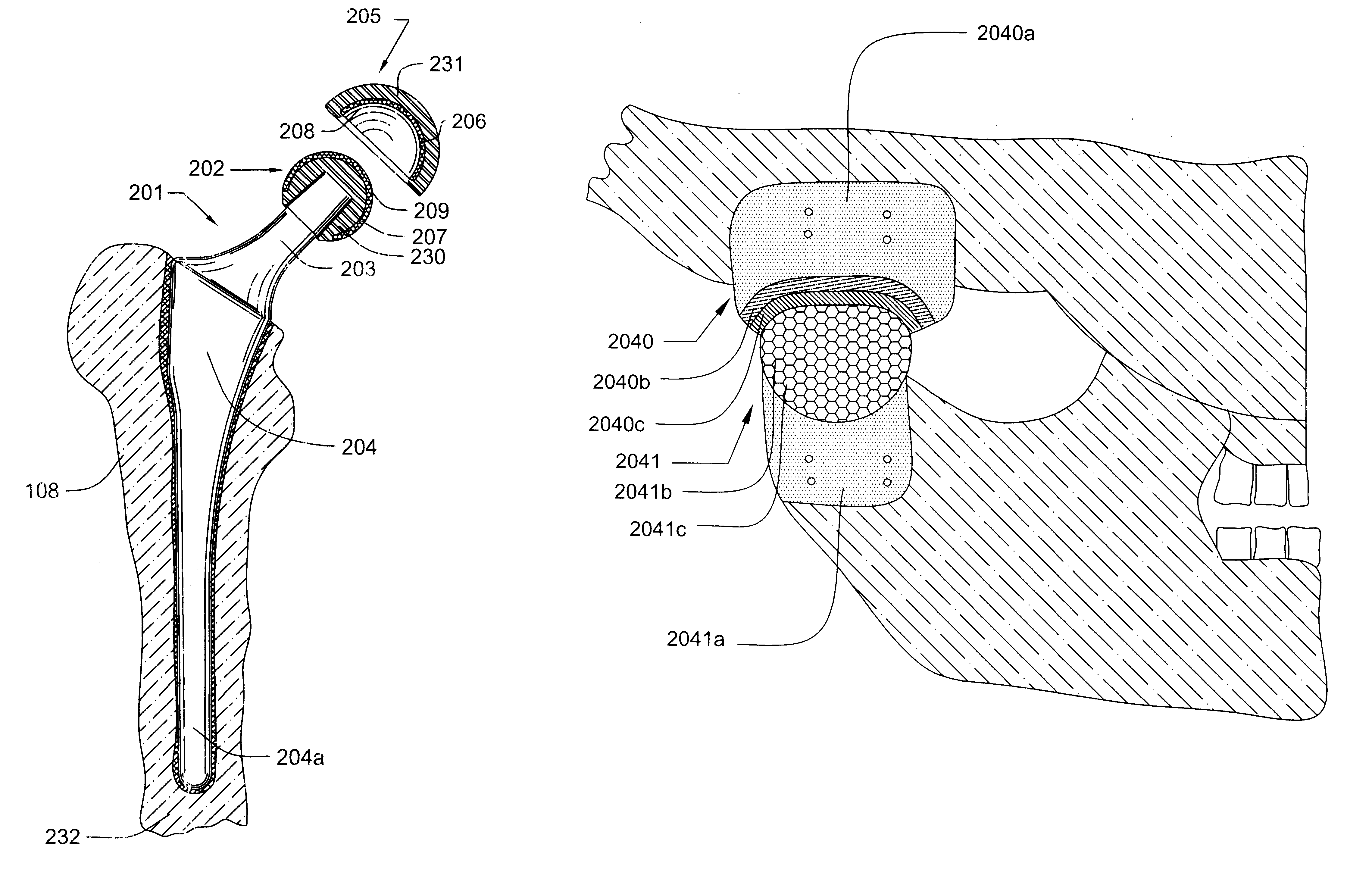
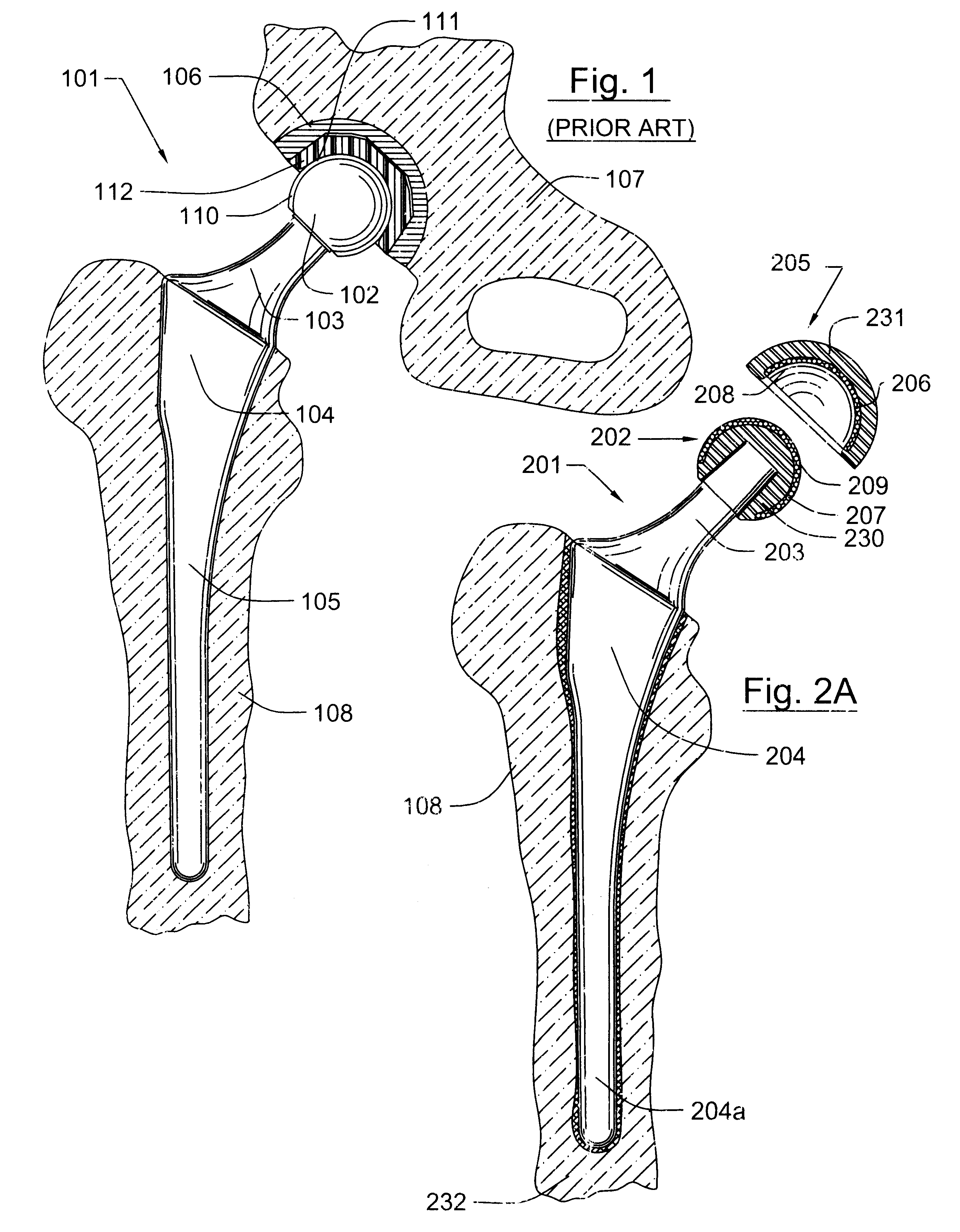
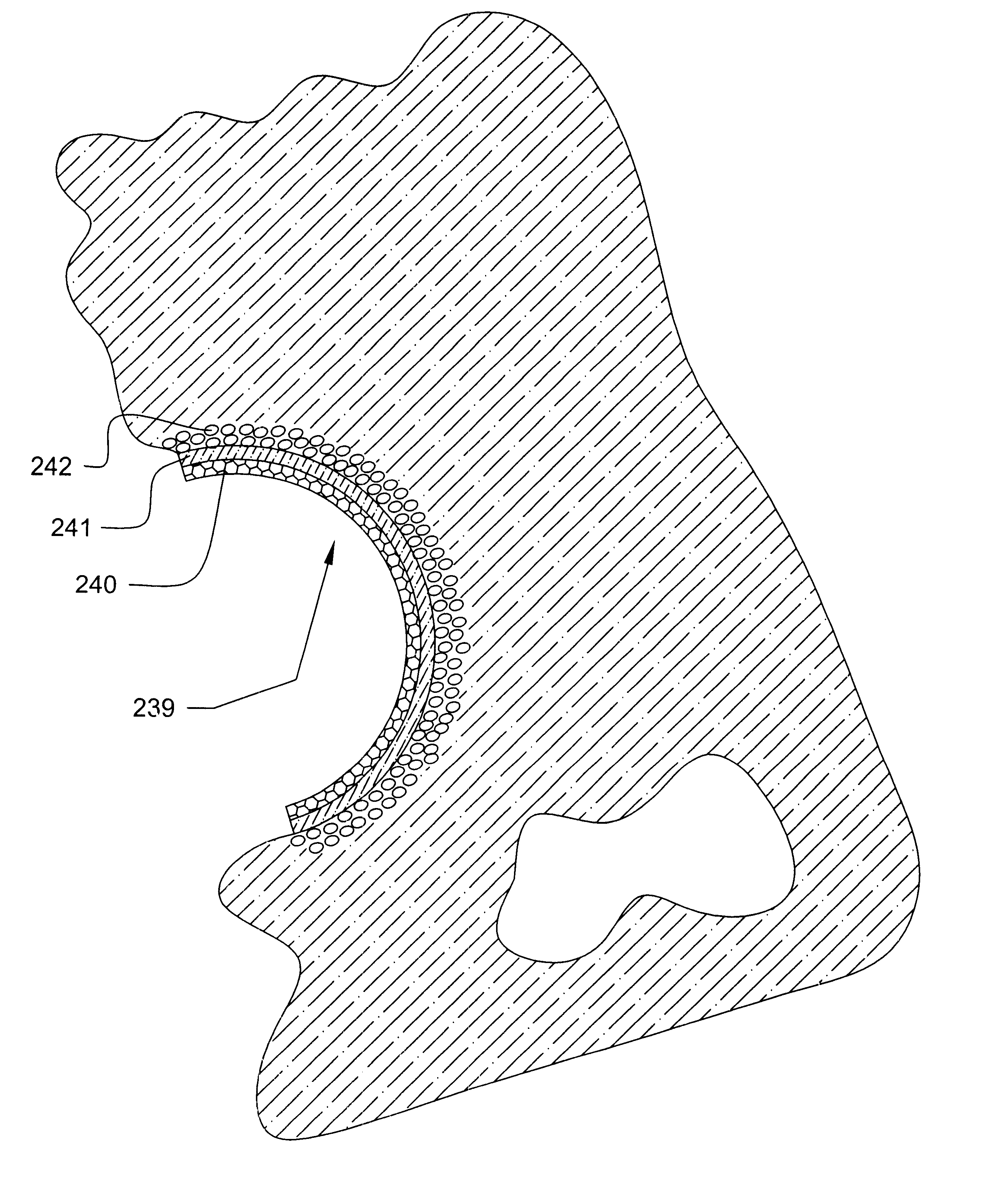
Prosthetic hip joint having sintered polycrystalline diamond compact articulation surfaces
InactiveUS6290726B1Improve wear resistanceReduce coefficient of frictionFinger jointsWrist jointsArticular surfacesProsthesis
Prosthetic joints, components for prosthetic joints, superhard bearing and articulation surfaces, diamond bearing and articulation surfaces, substrate surface topographical features, materials for making joints, bearing and articulation surfaces, and methods for manufacturing and finishing the same, and related information are disclosed, including a prosthetic hip joint having sintered polycrystalline diamond articulation.
Owner:DIAMICRON
Method for treating a vertebral body
Owner:ORTHOPHOENIX
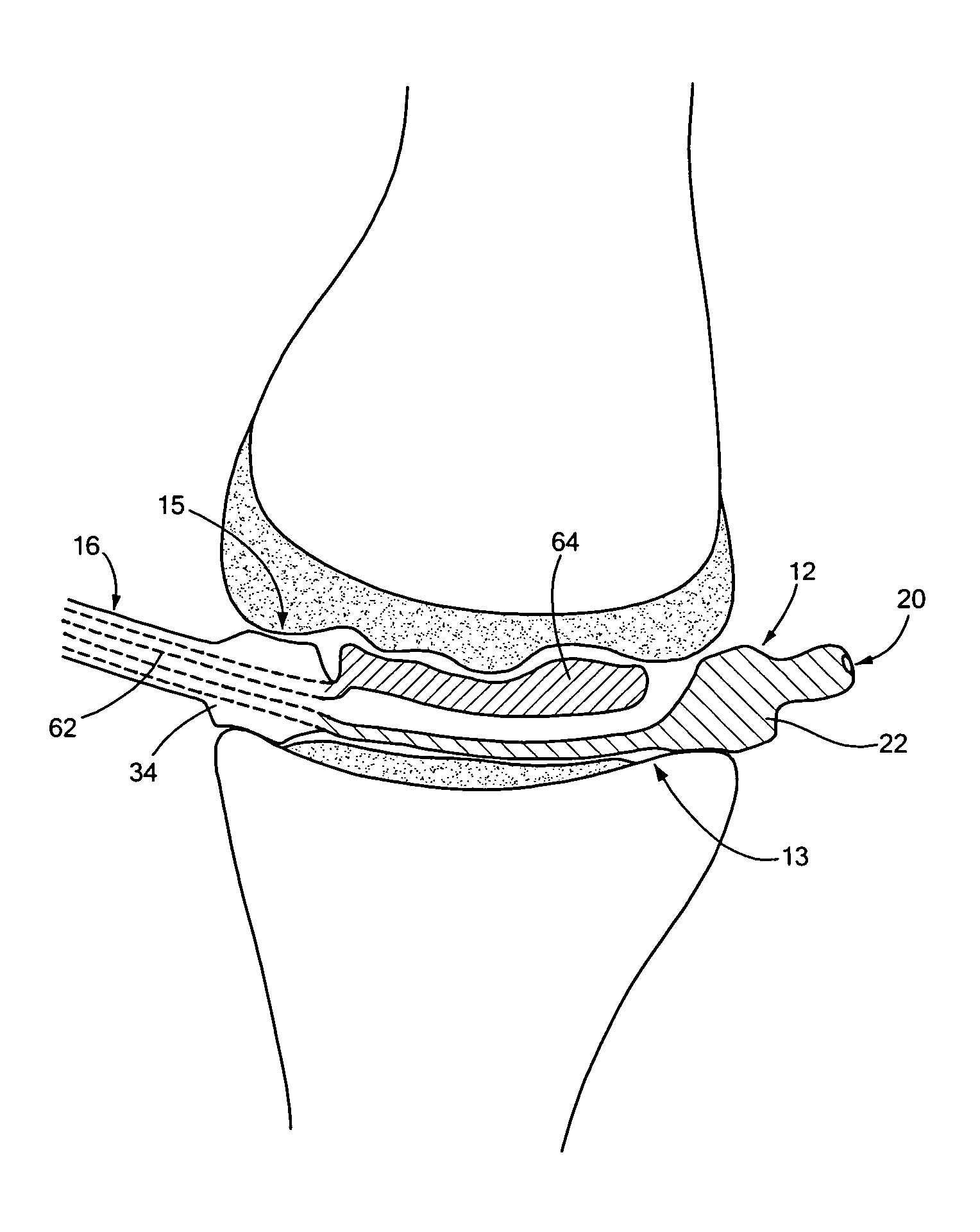
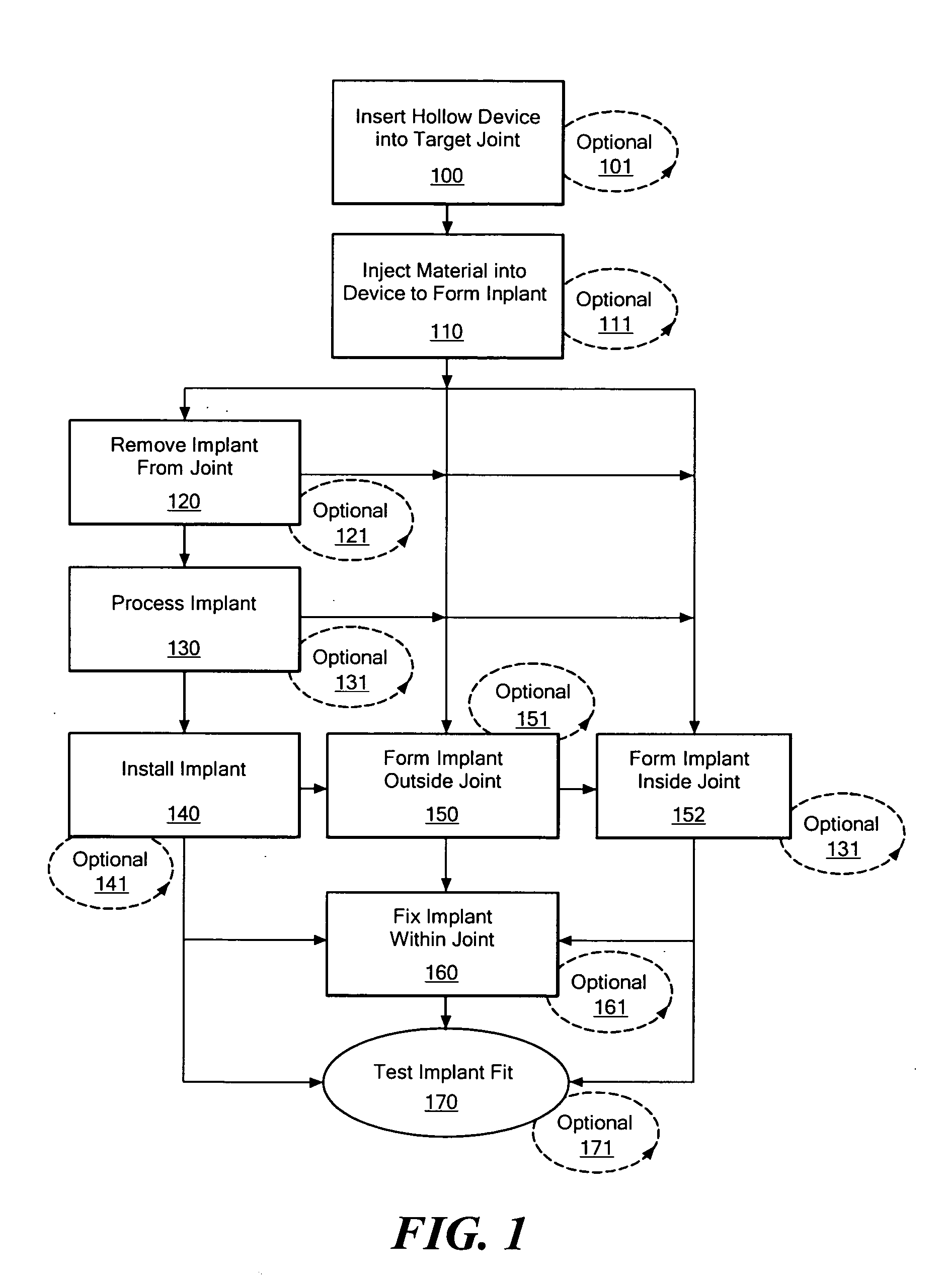
Joint arthroplasty devices formed in situ
InactiveUS20070250169A1Improve accuracyImage analysisWrist jointsArticular surfacesJoint arthroplasty
Disclosed herein are methods and devices for repairing articular surfaces. The articular surface repairs are customizable or highly selectable by patient and geared toward providing optimal fit and function.
Owner:CONFORMIS
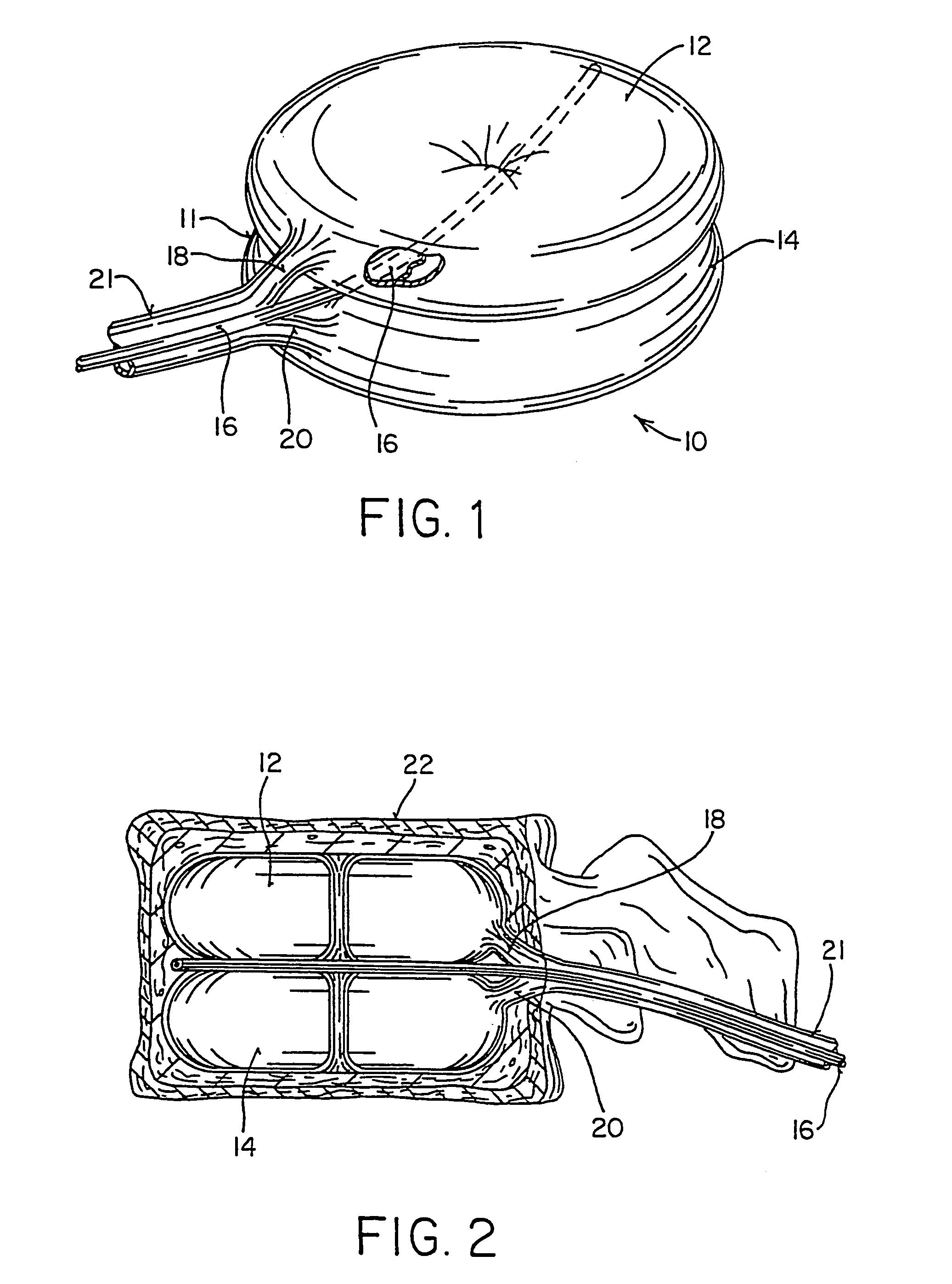
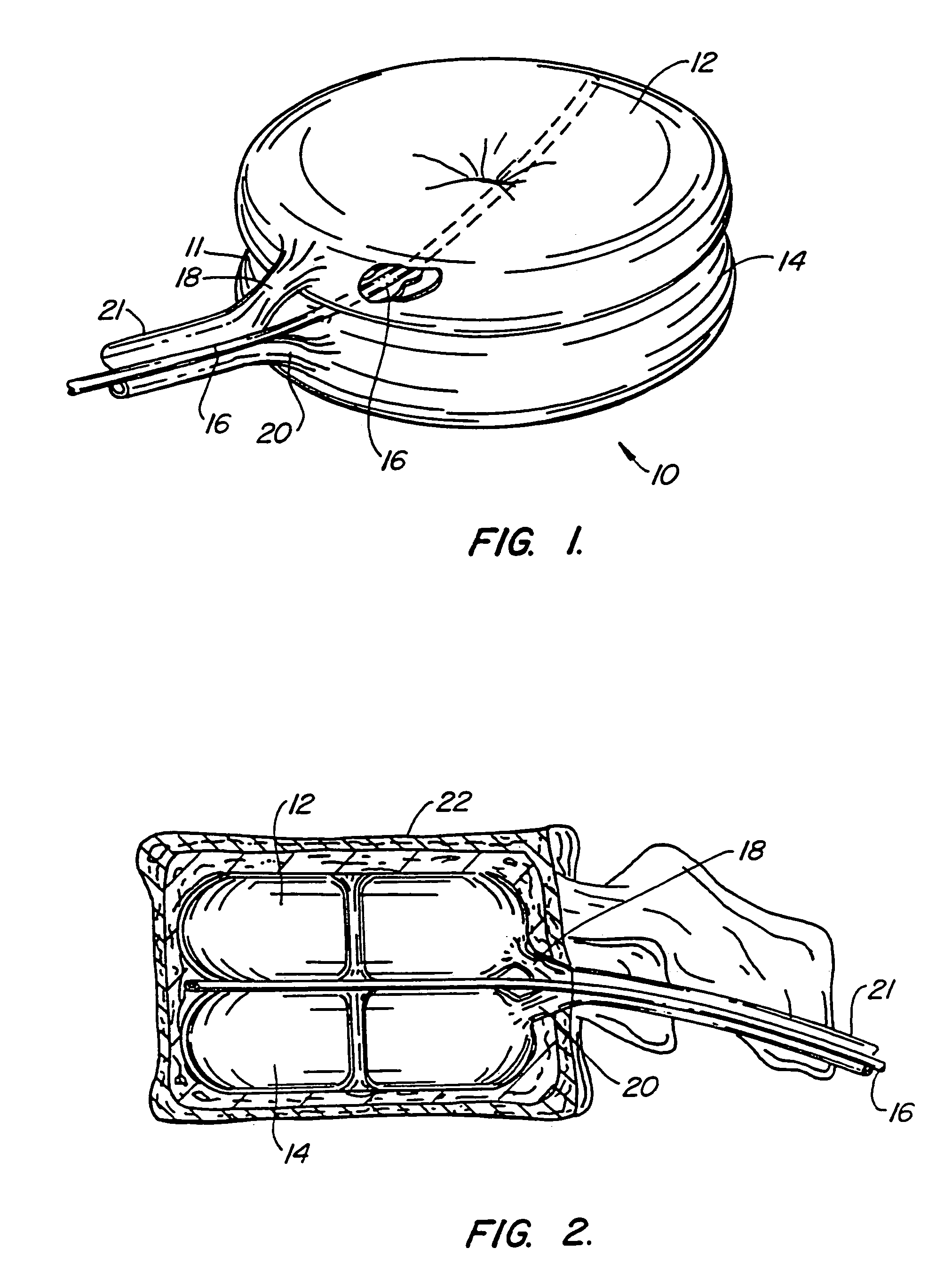
Inflatable device for use in surgical protocol relating to fixation of bone
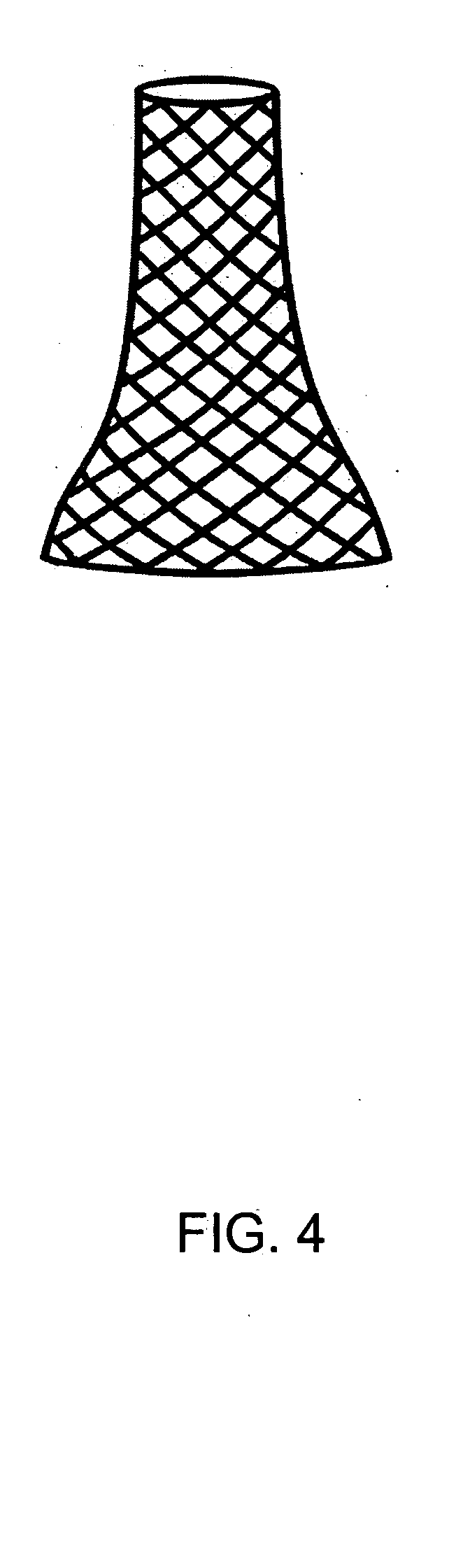
InactiveUS7261720B2Easy to compressEasy to foldSurgical furnitureInternal osteosythesisBone CortexTrabecular bone
A balloon for use in compressing cancellous bone and marrow (also known as medullary bone or trabecular bone). The balloon comprises an inflatable balloon body for insertion into said bone. The body has a shape and size to compress at least a portion of the cancellous bone to form a cavity in the cancellous bone and / or to restore the original position of the outer cortical bone, if fractured or collapsed. The balloon desirably incorporates restraints which inhibit the balloon from applying excessive pressure to various regions of the cortical bone. The wall or walls of the balloon are such that proper inflation of the balloon body is achieved to provide for optimum compression of the bone marrow. The balloon can be inserted quickly into a bone. The balloon can be made to have a suction catheter. The balloon can be used to form and / or enlarge a cavity or passage in a bone, especially in, but not limited to, vertebral bodies. Various additional embodiments facilitate directionally biasing the inflation of the balloon.
Owner:ORTHOPHOENIX
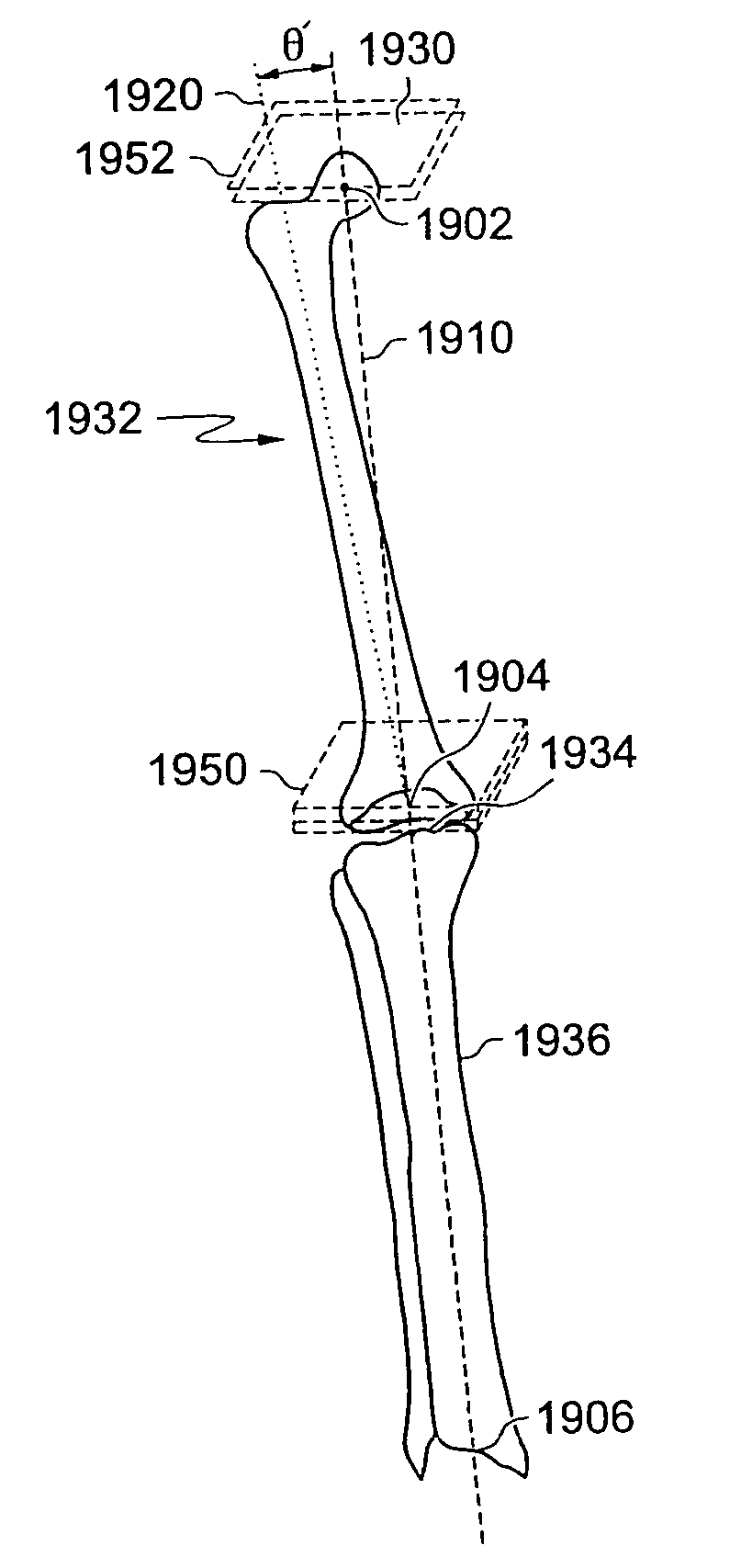
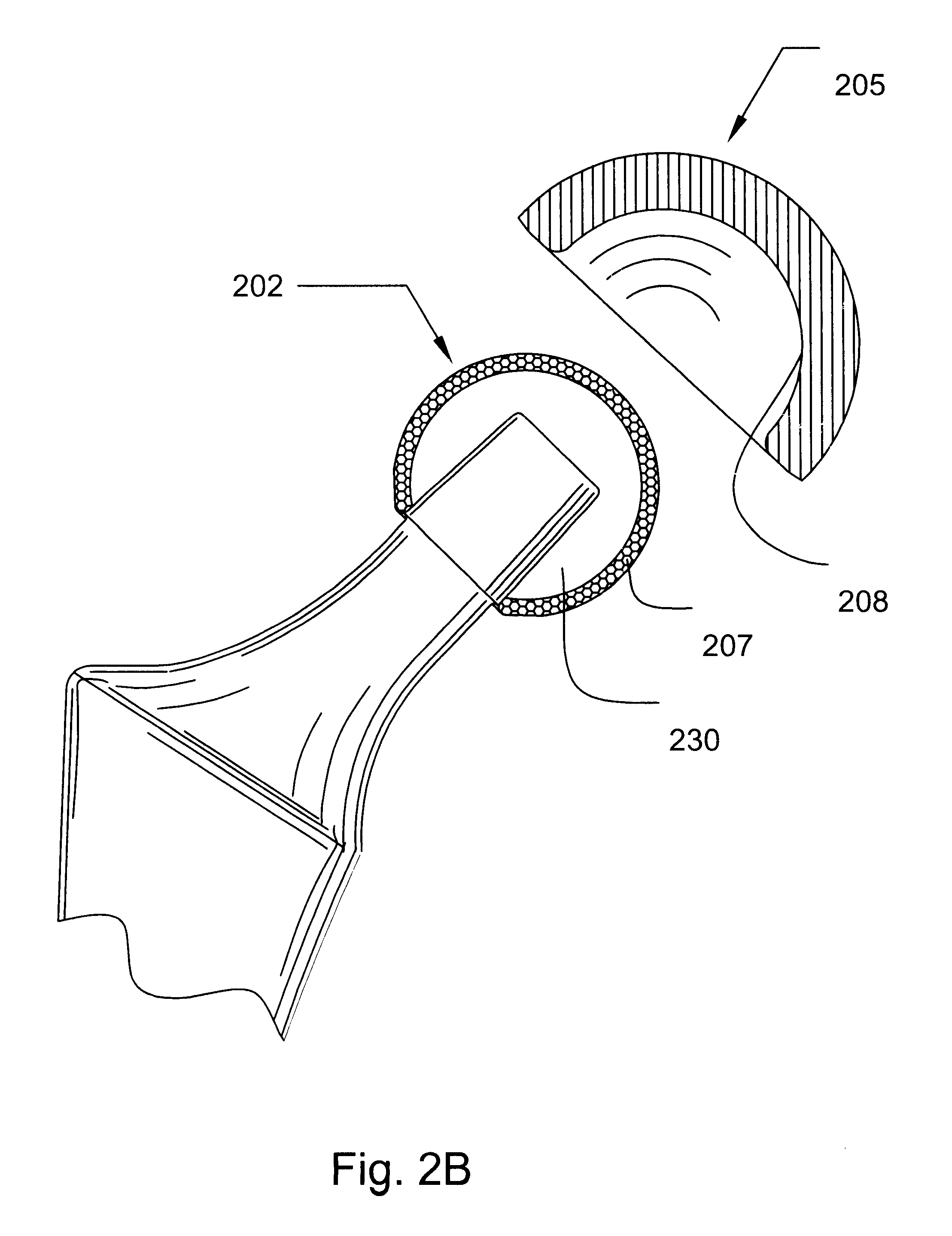
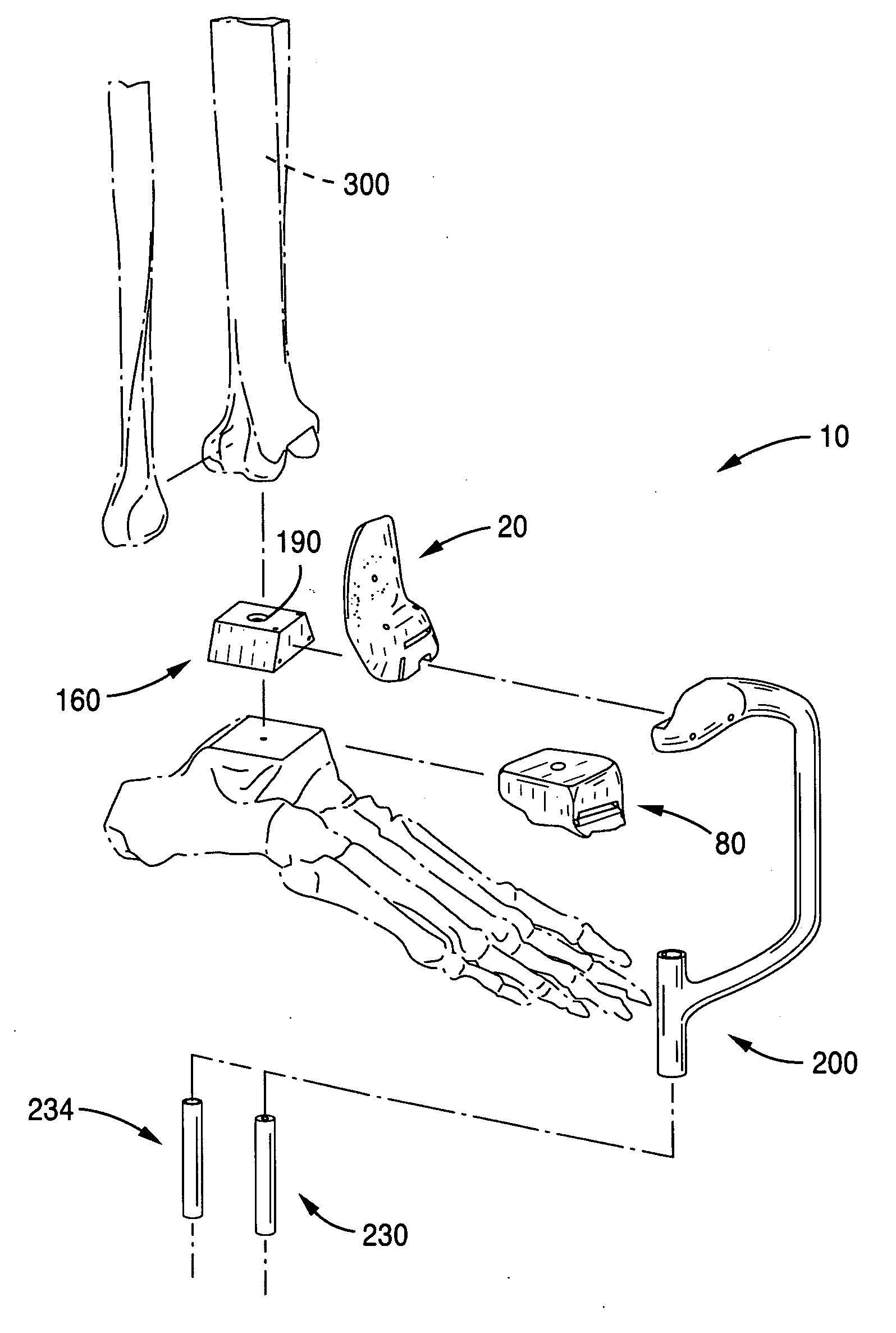
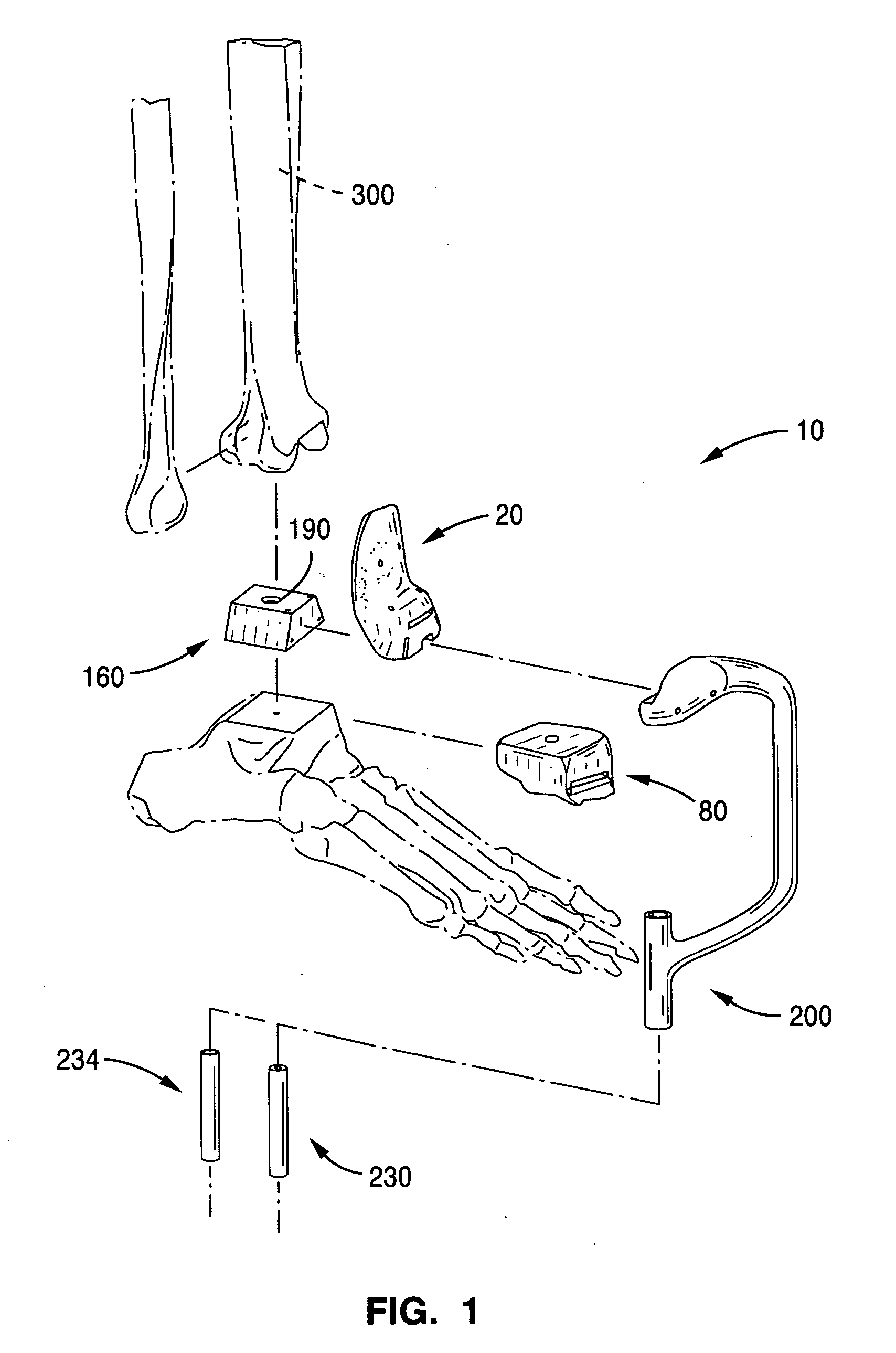
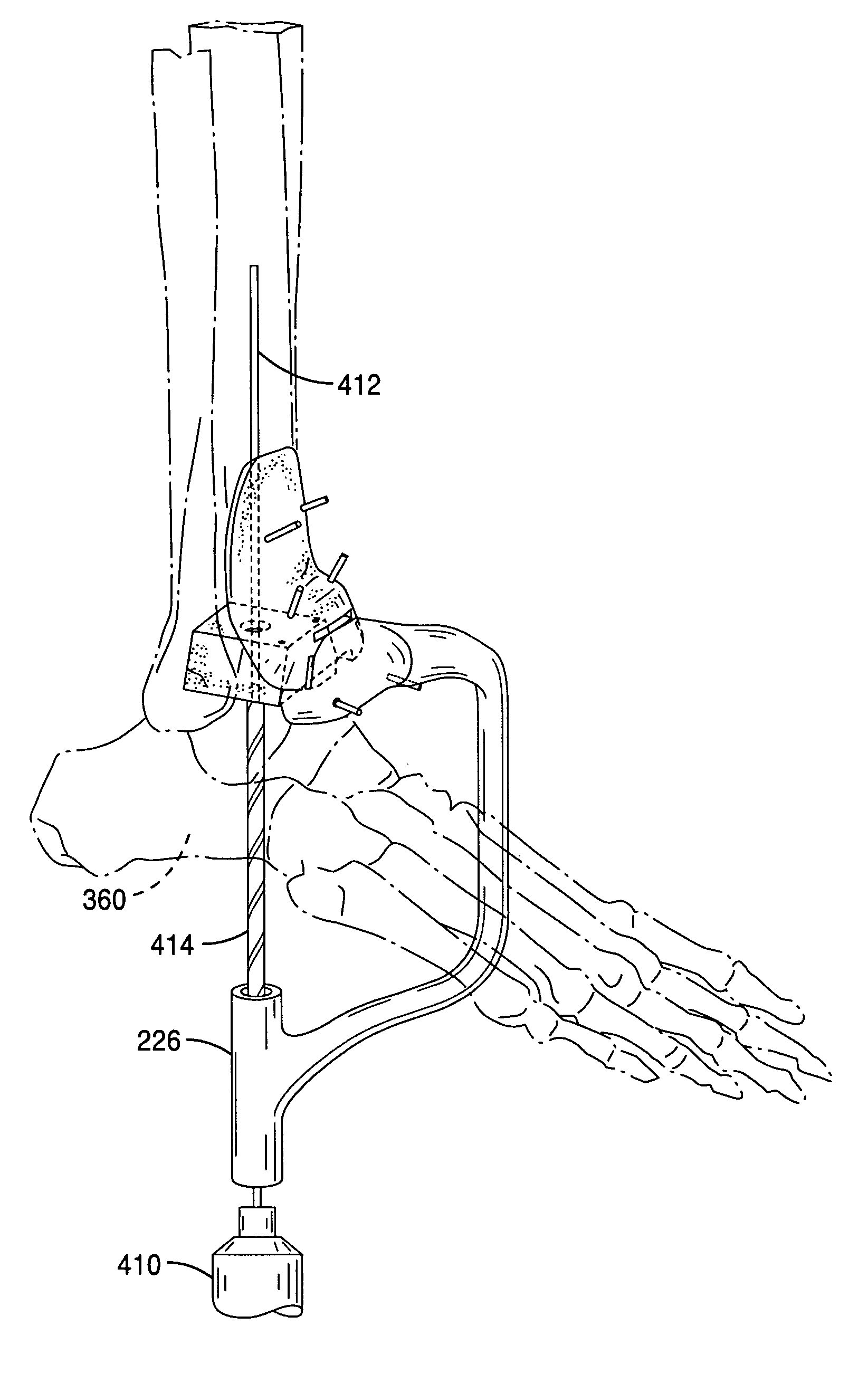
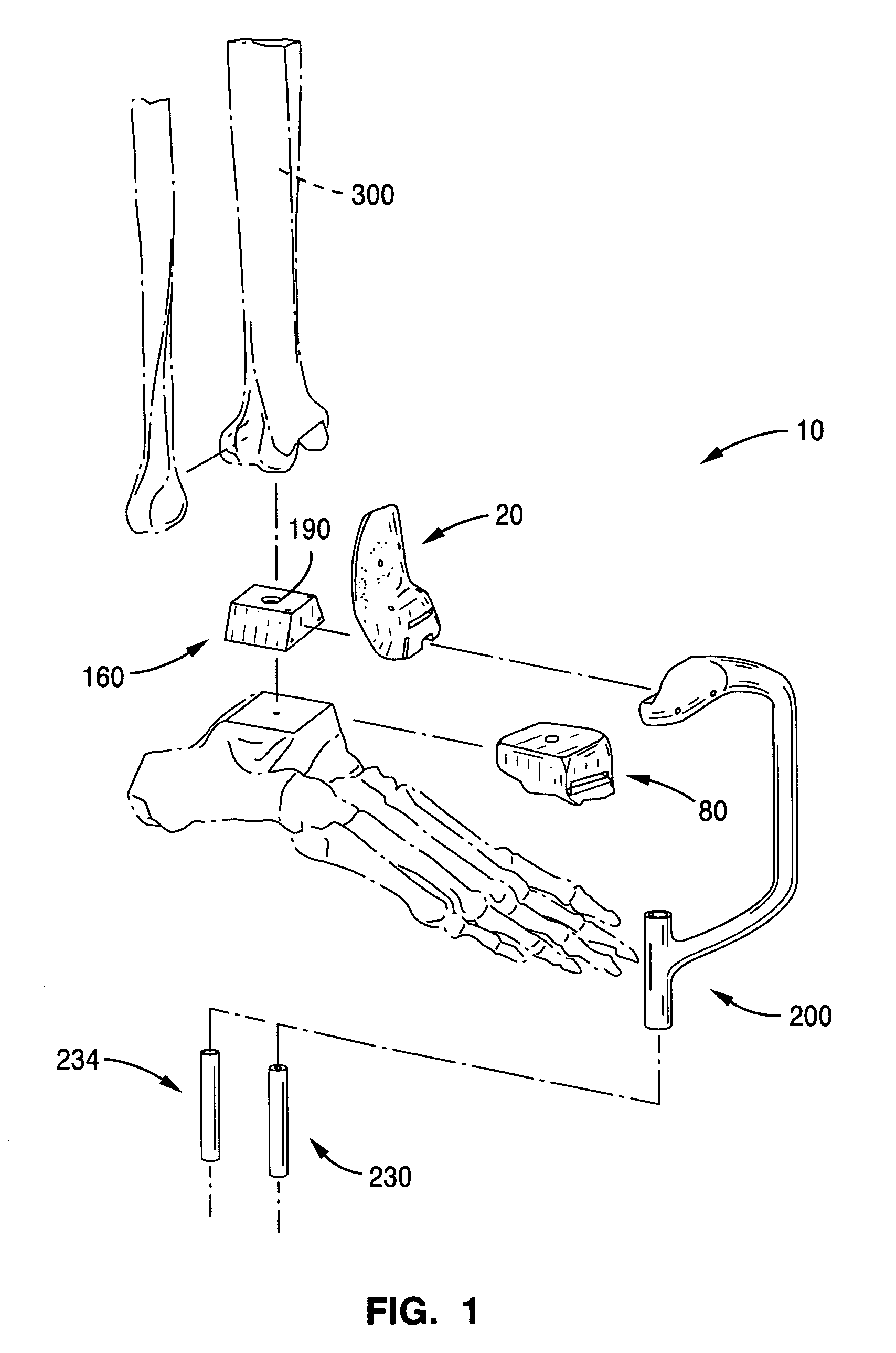
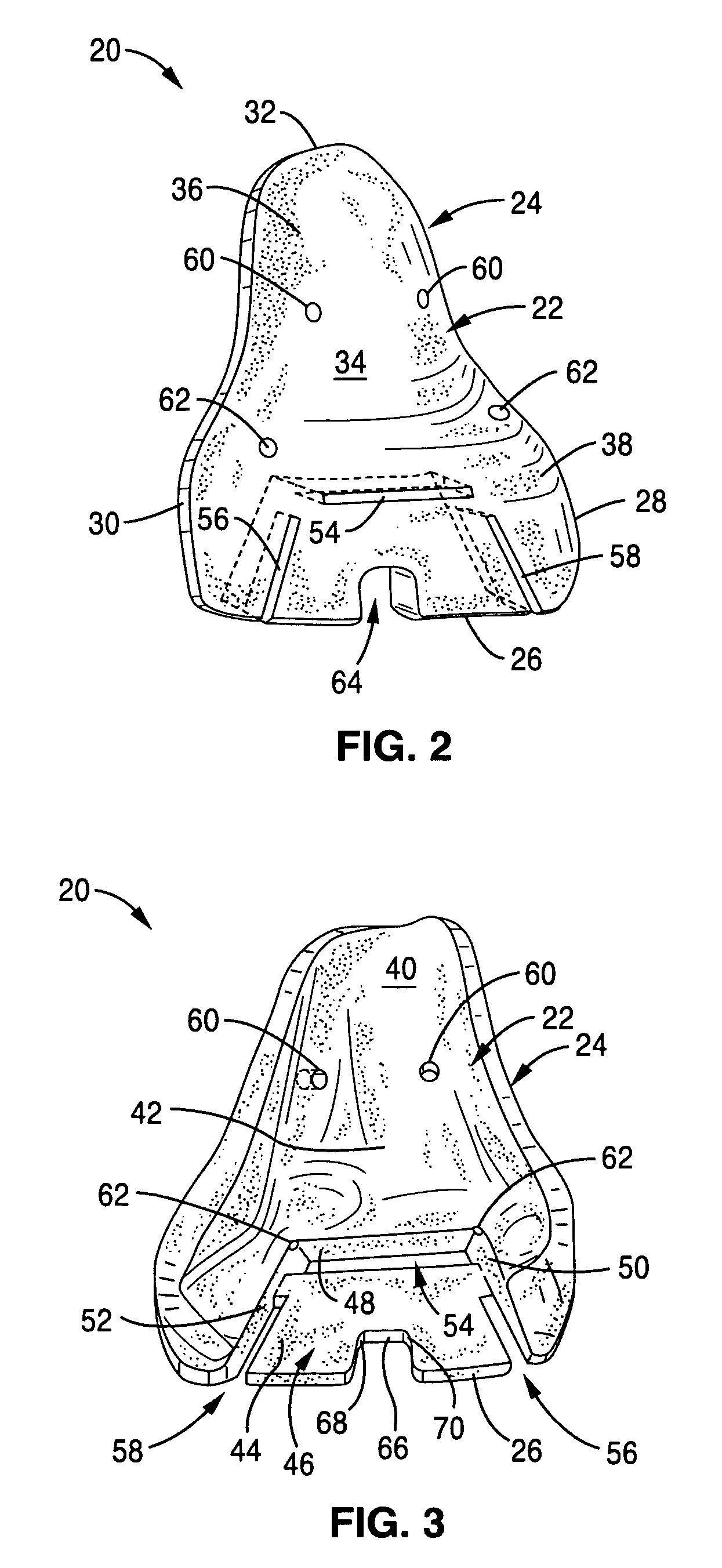
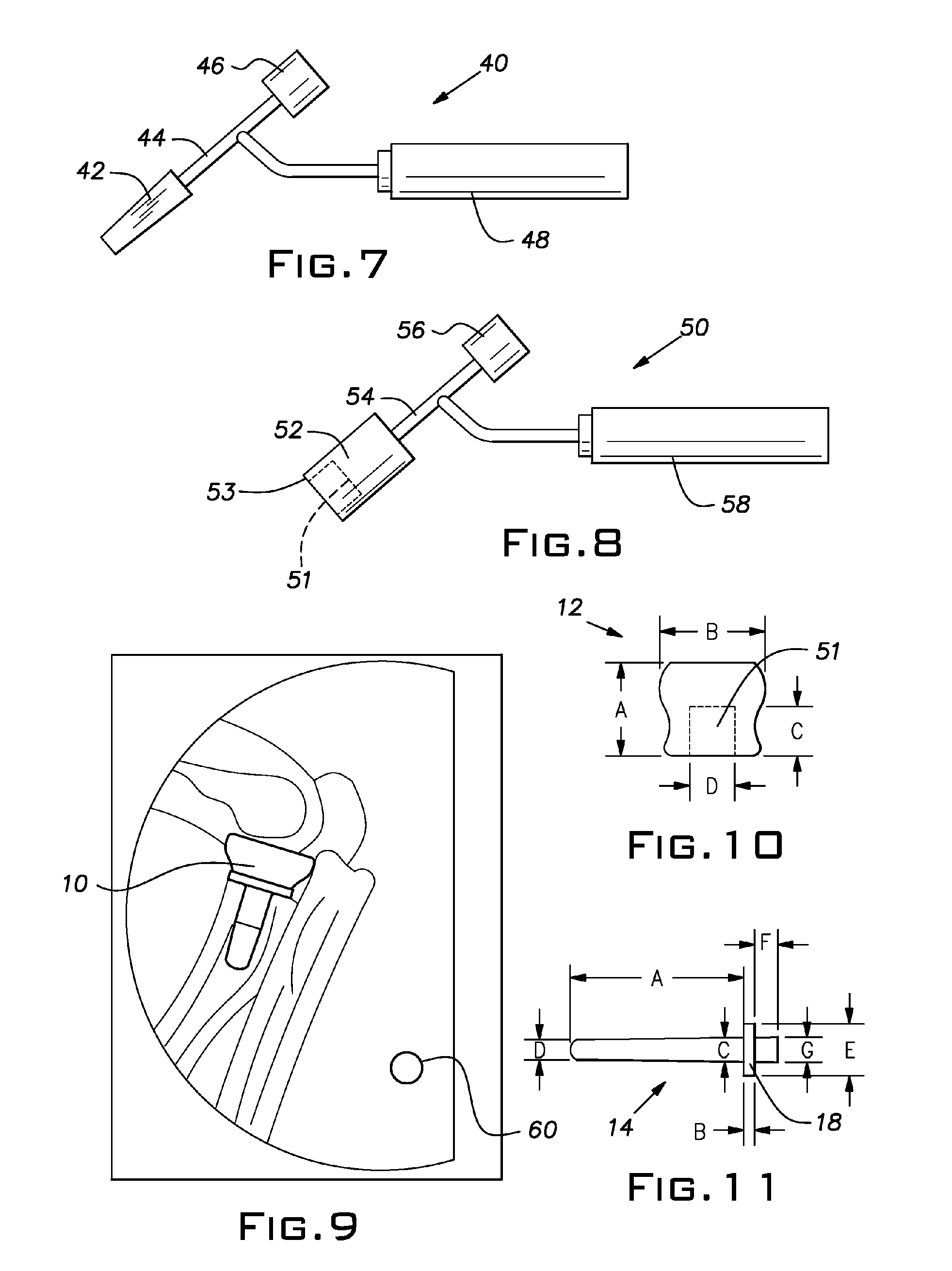
Custom radiographically designed cutting guides and instruments for use in total ankle replacement surgery
ActiveUS20100262150A1High precisionSimplify operating proceduresWrist jointsAnkle jointsTibiaSacroiliac joint
A system comprised of custom radiographically designed tibial and talar cutting guides, a tibial reaming guide and bit, and instrumentalities for use in total ankle replacement surgery and a computer-based system and method for making the custom radiographically designed tibial and talar cutting guides.
Owner:LIAN GEORGE JOHN
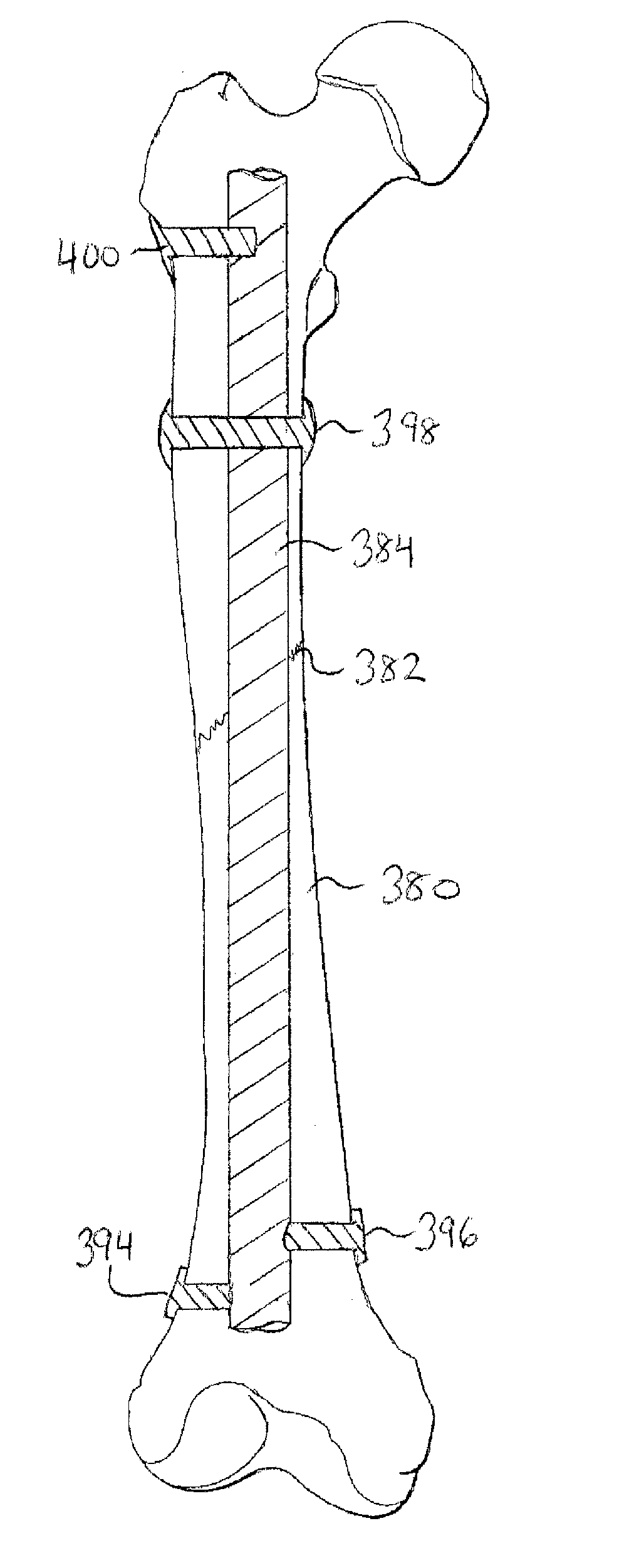
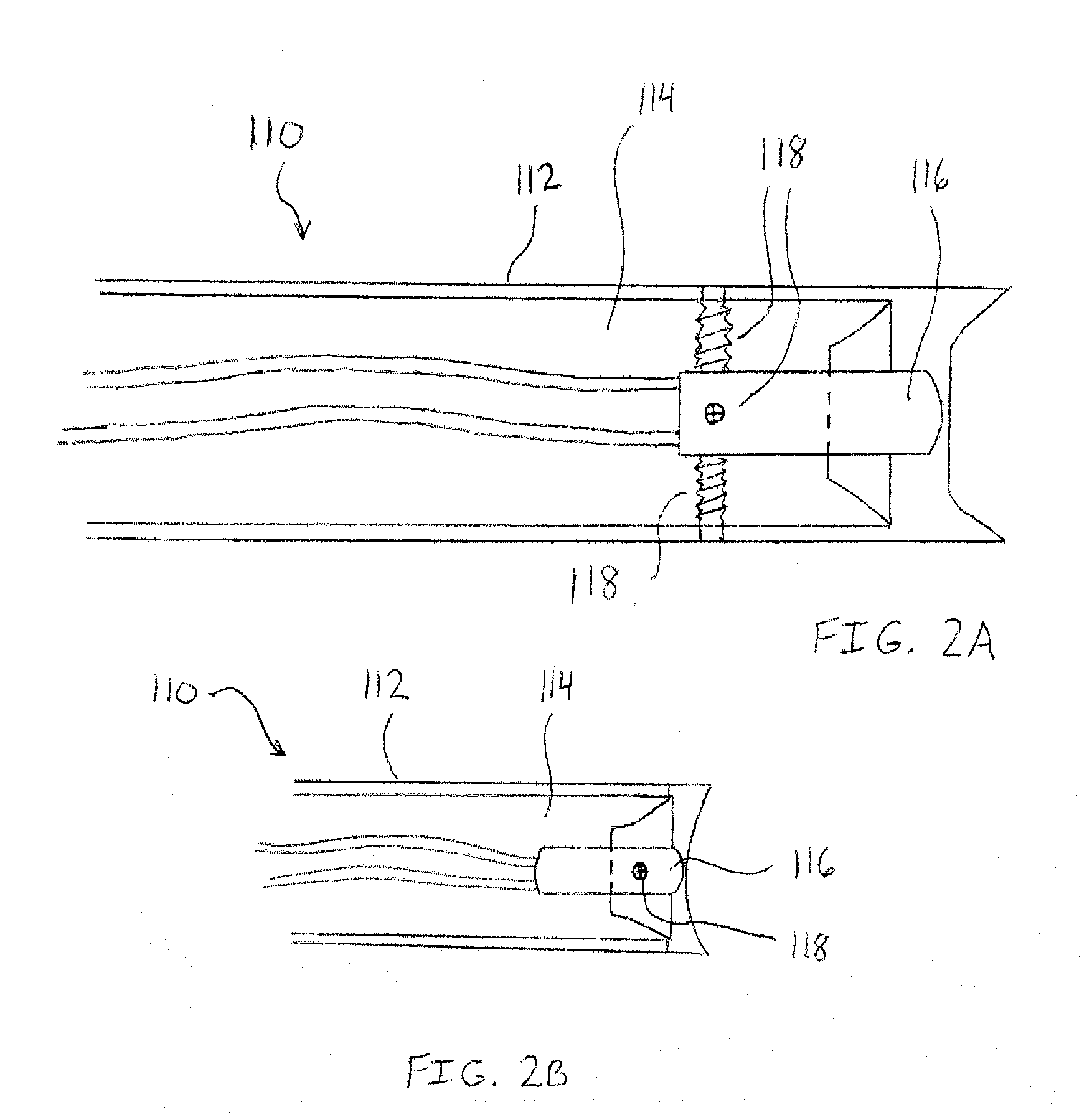
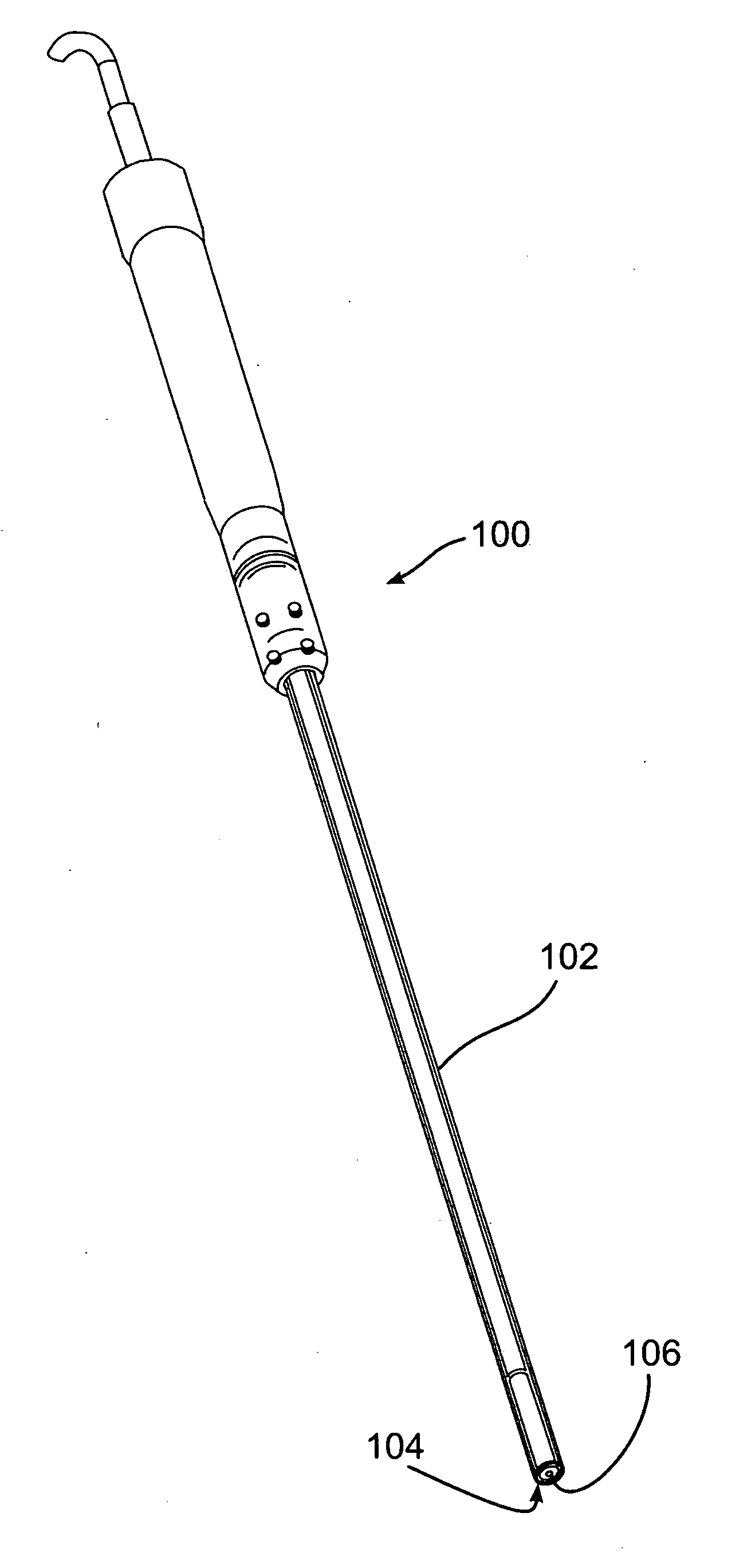
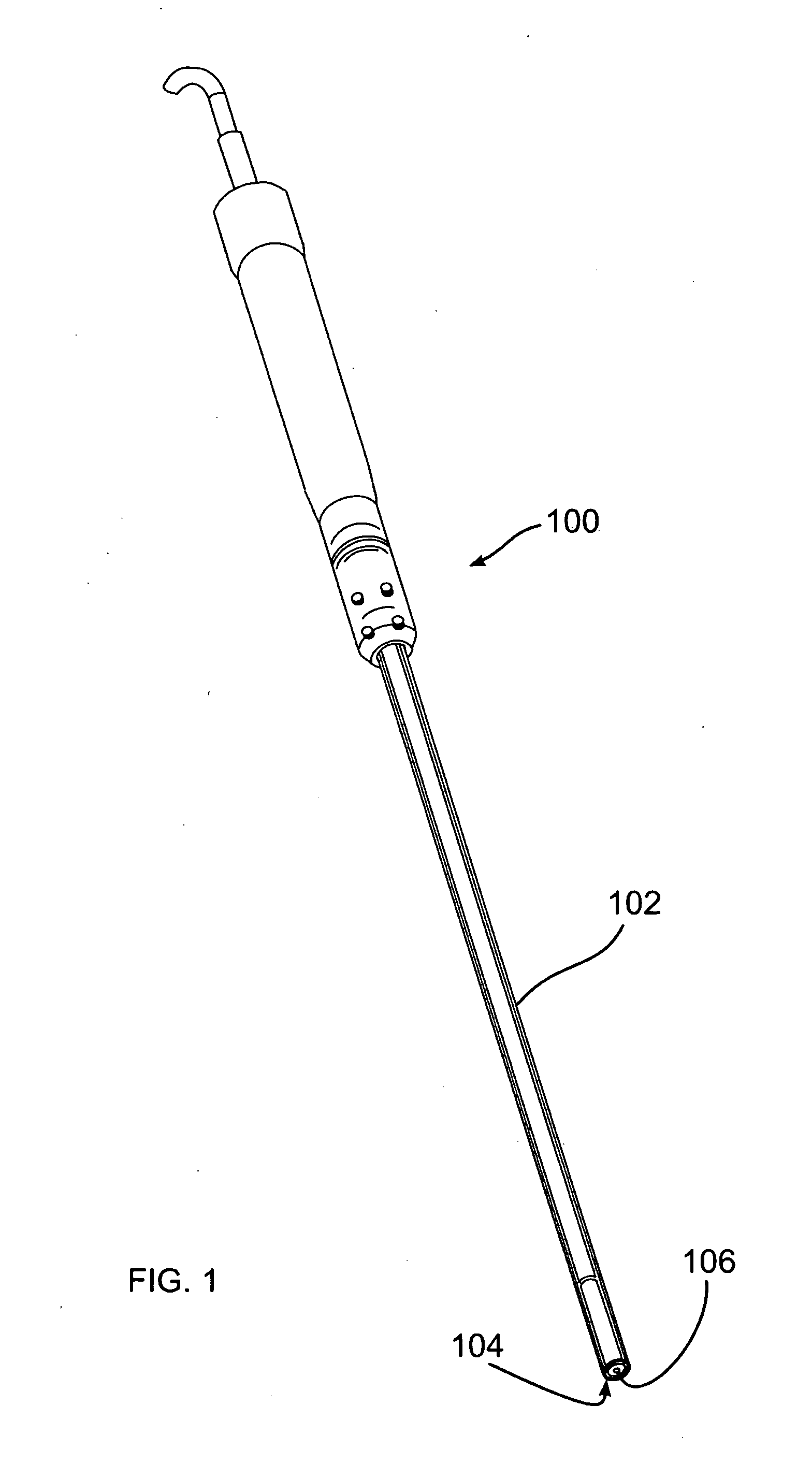
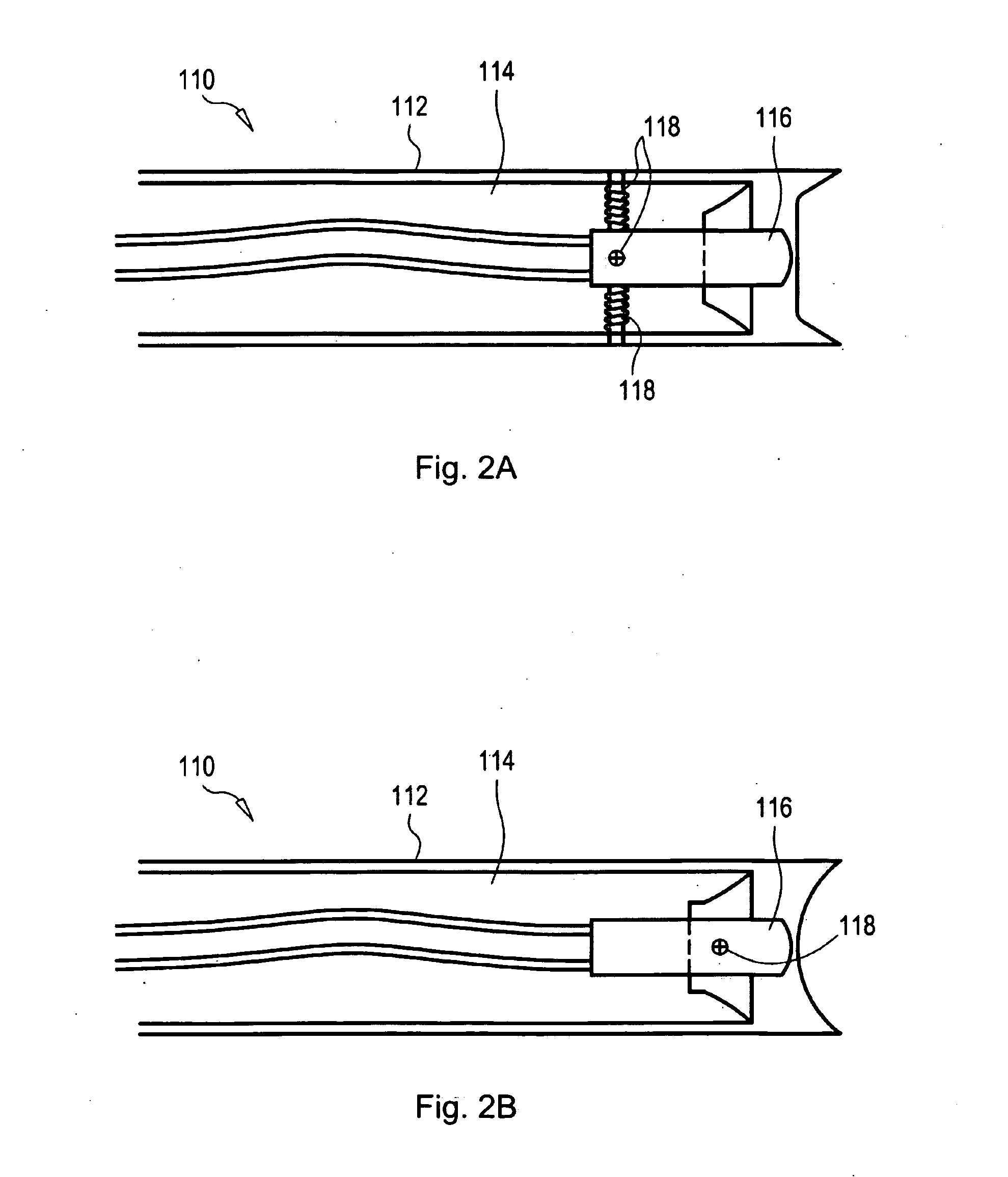
Methods and devices for intracorporeal bonding of implants with thermal energy
The present invention provides a method for stabilizing a fractured bone. The method includes positioning an elongate rod in the medullary canal of the fractured bone and forming a passageway through the cortex of the bone. The passageway extends from the exterior surface of the bone to the medullary canal of the bone. The method also includes creating a bonding region on the elongate rod. The bonding region is generally aligned with the passageway of the cortex. Furthermore, the method includes positioning a fastener in the passageway of the cortex and on the bonding region of the elongate rod and thermally bonding the fastener to the bonding region of the elongate rod while the fastener is positioned in the passageway of the cortex.
Owner:P TECH
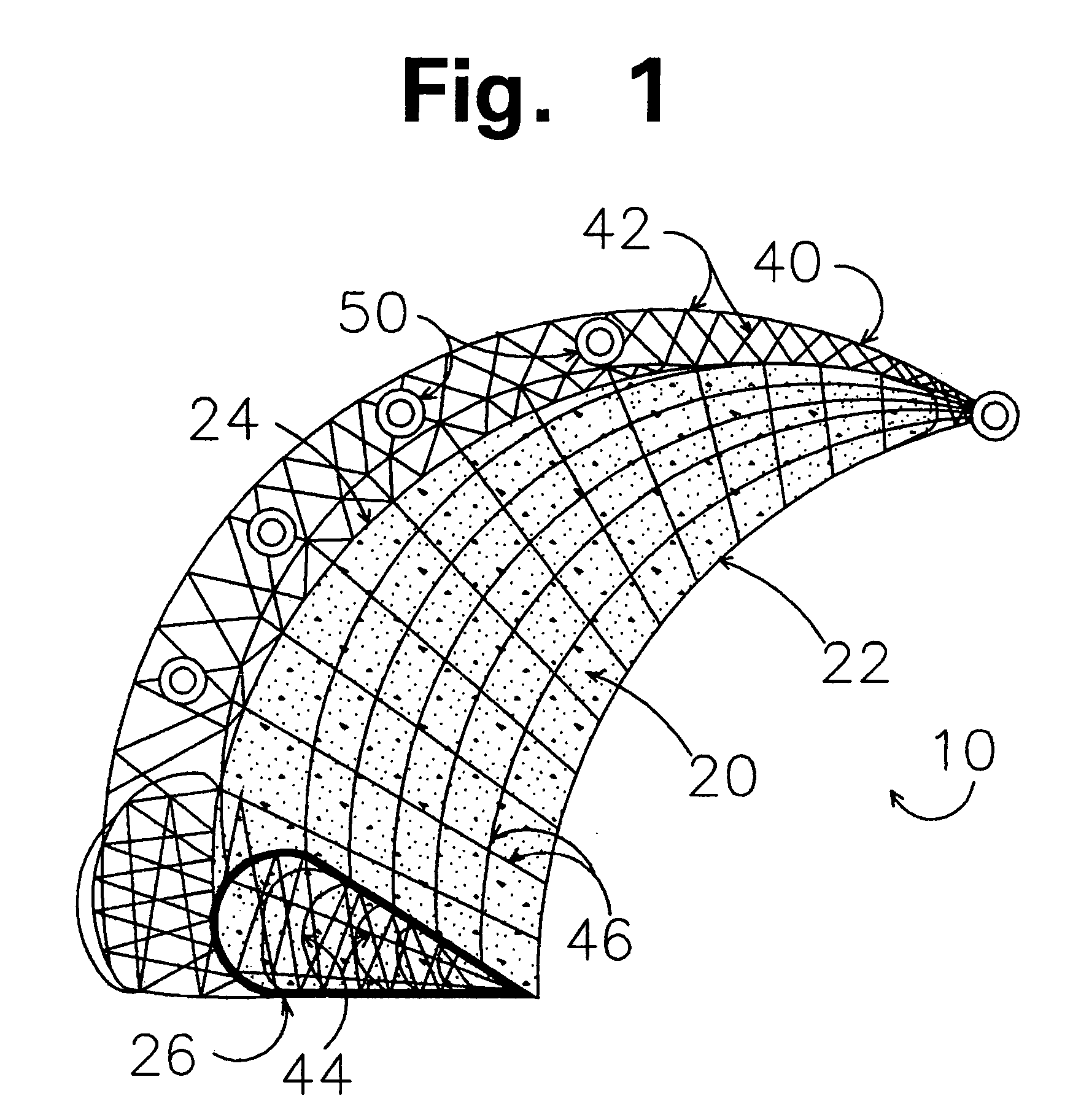
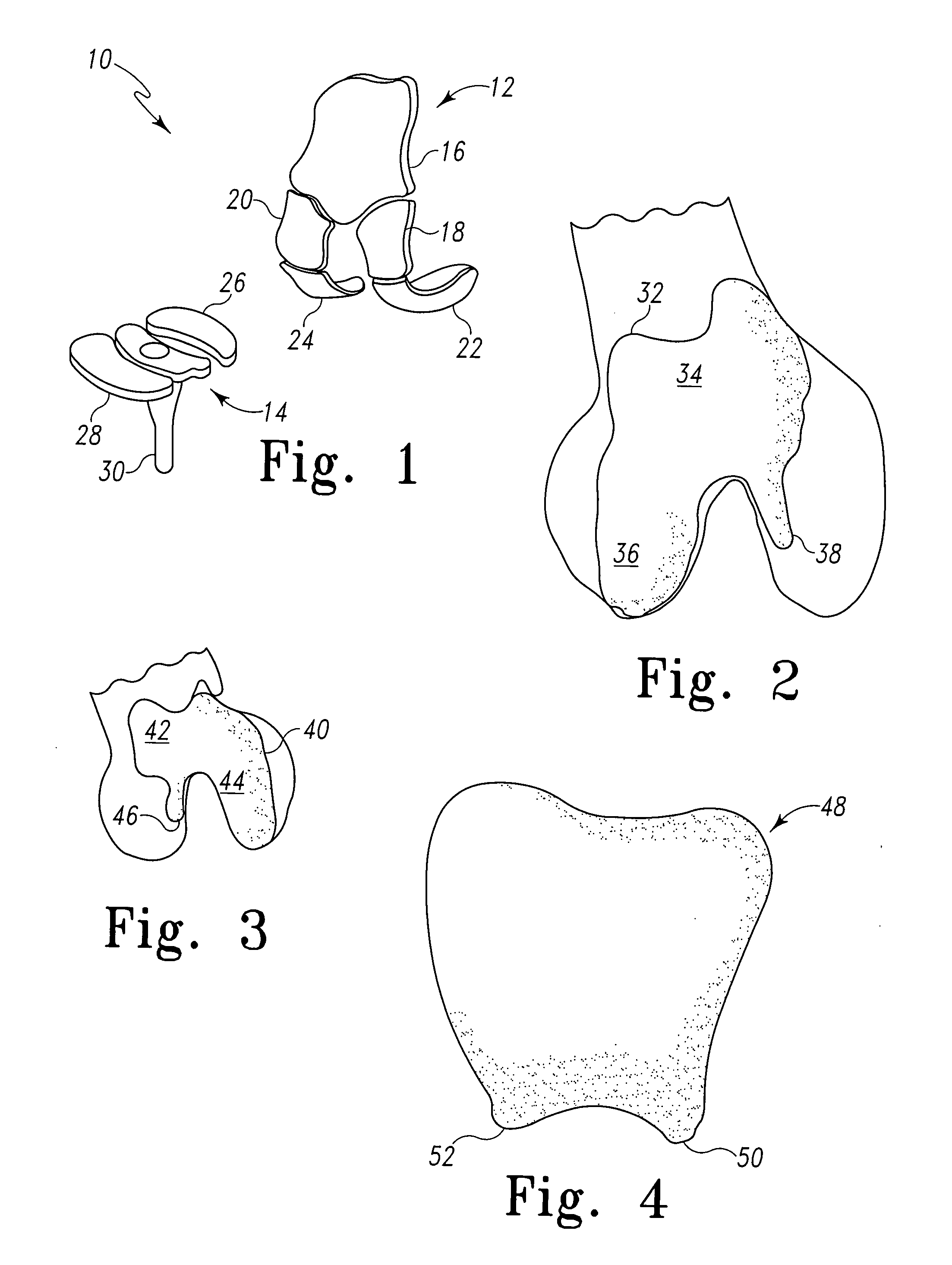
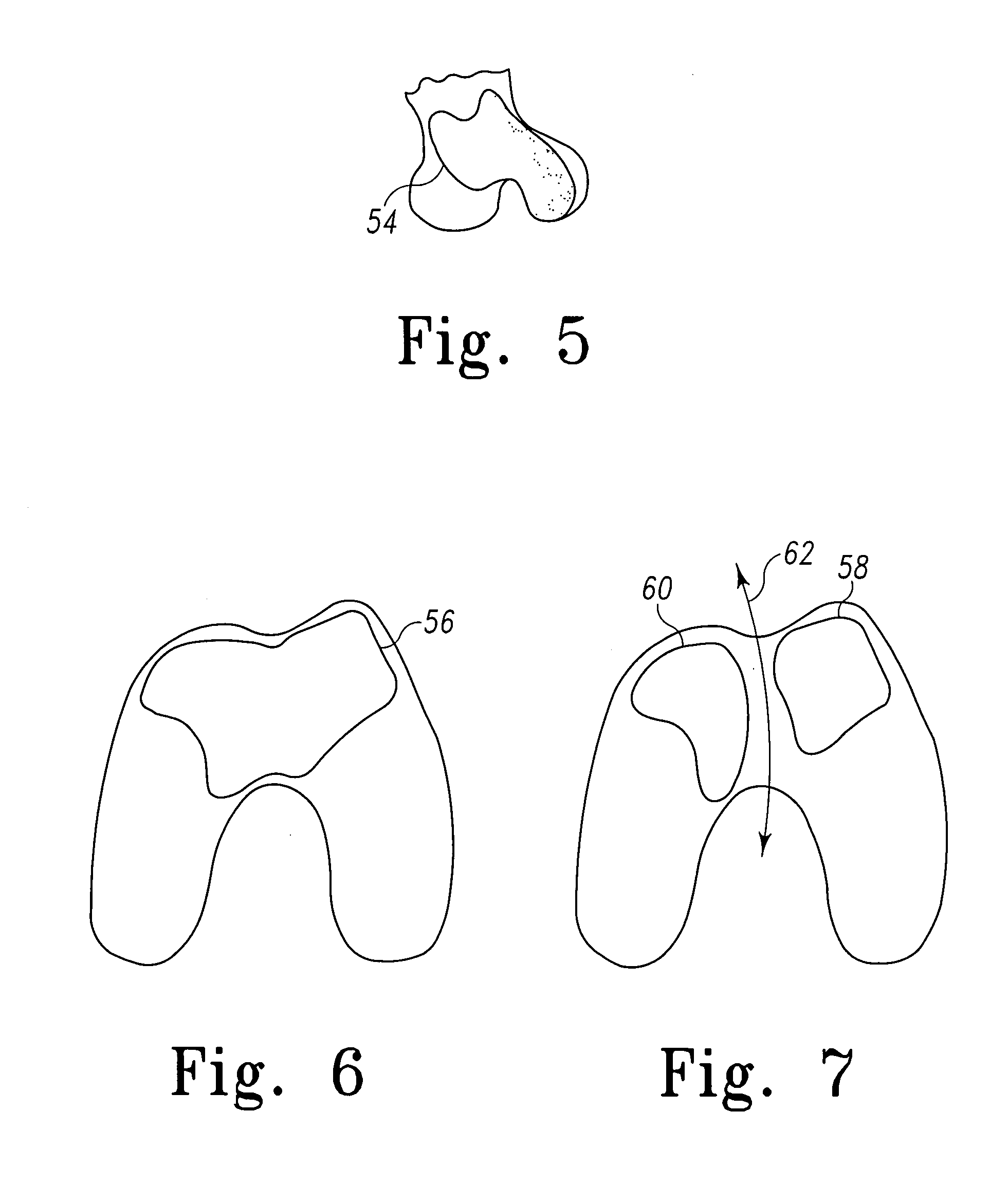
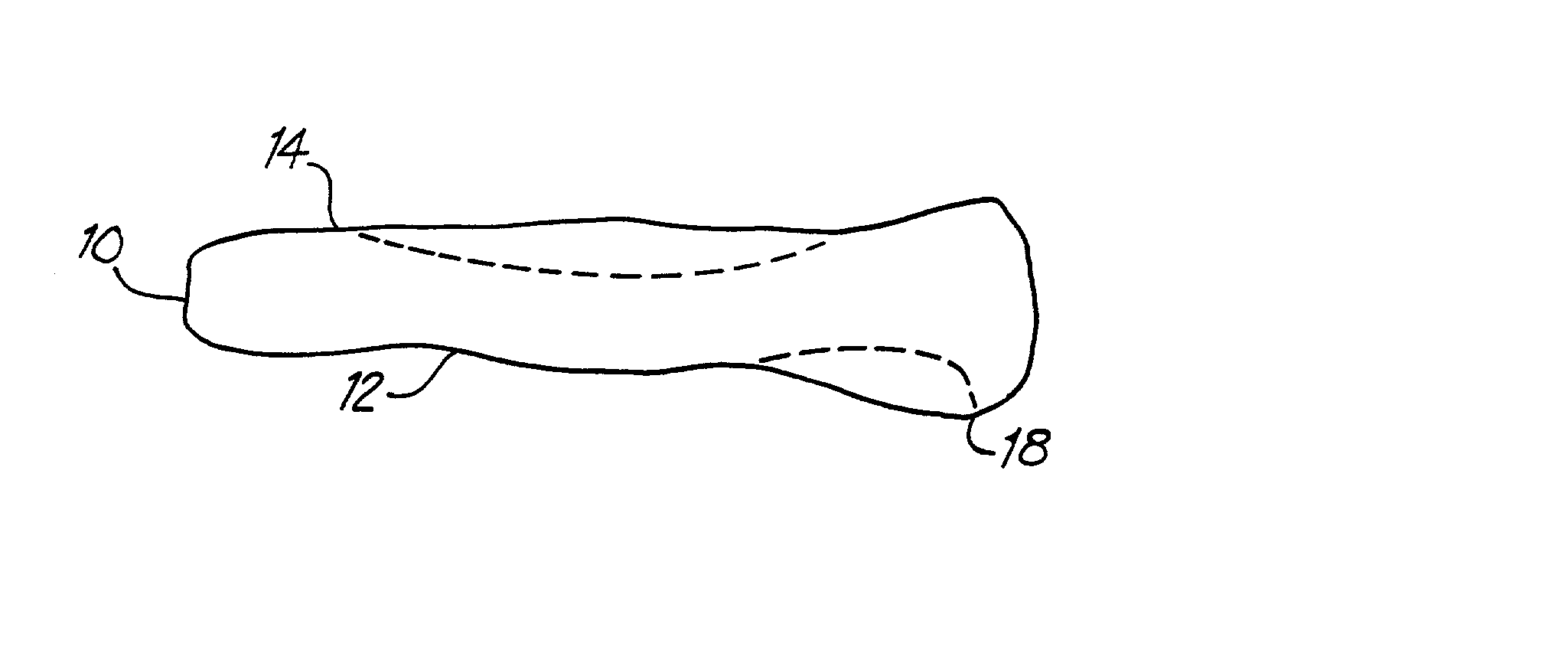
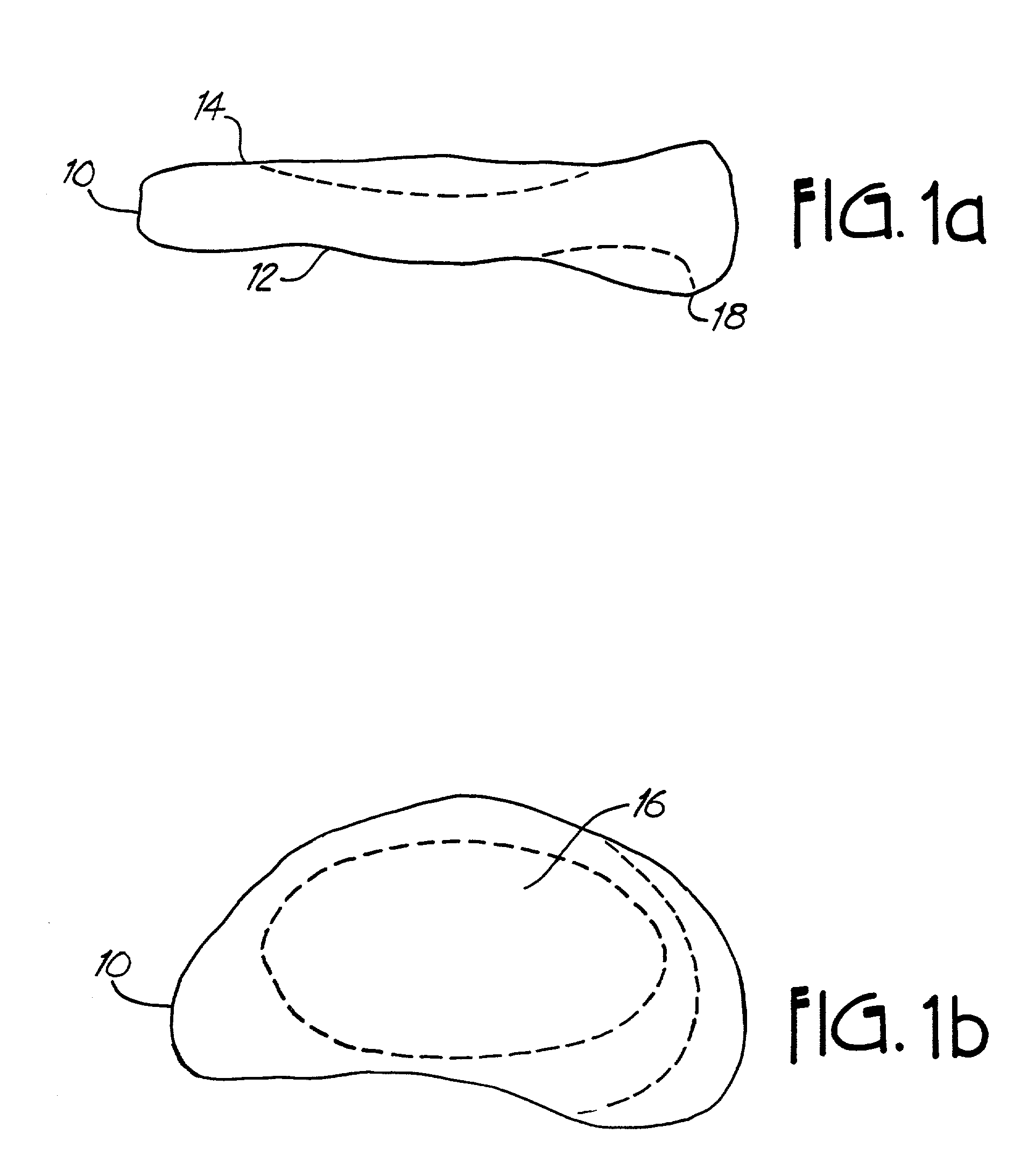
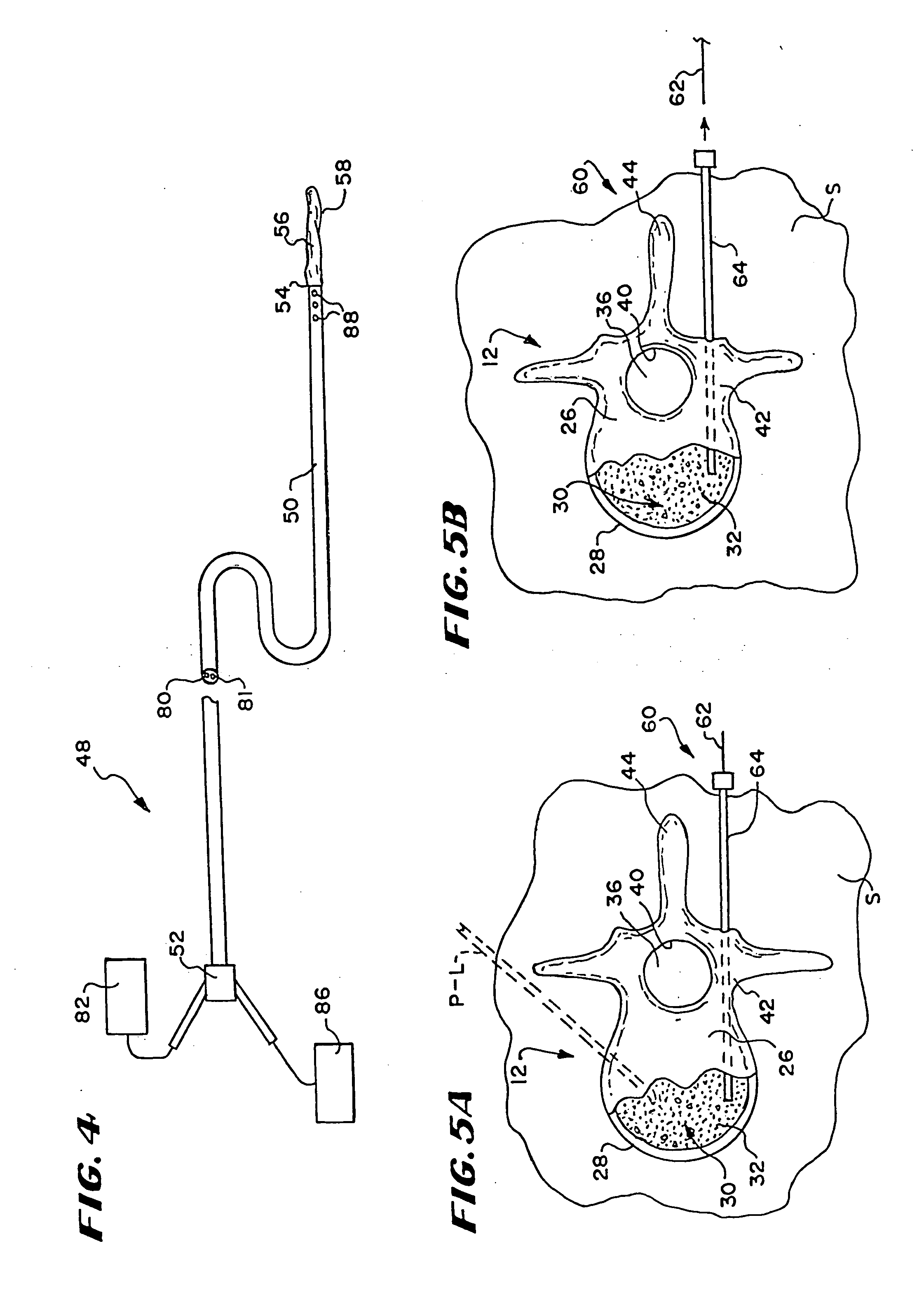
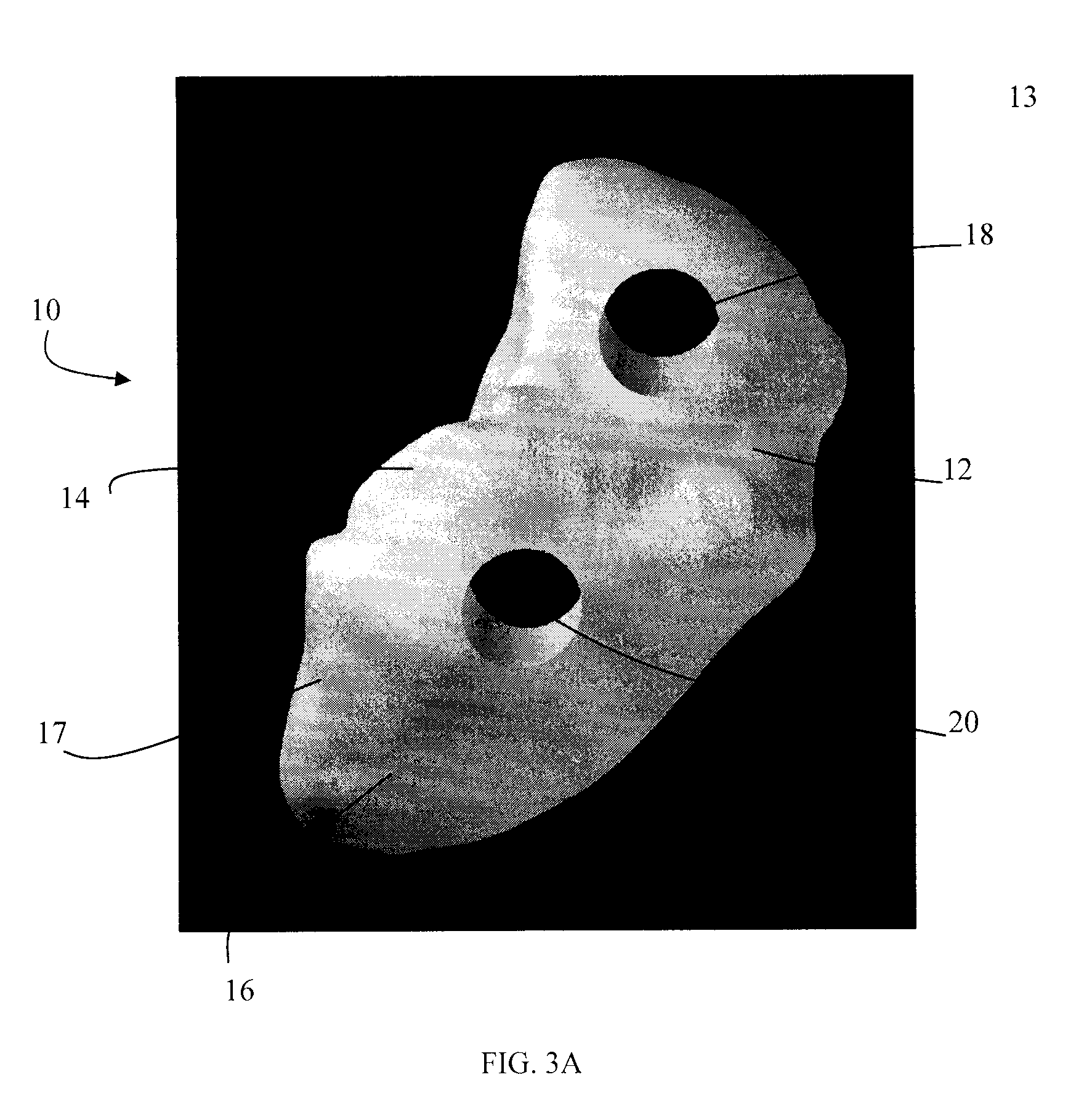
Minimally invasive joint implant with 3-dimensional geometry matching the articular surfaces
ActiveUS7799077B2Increase successFacilitating the integration of a wide variety of cartilageFinger jointsWrist jointsArticular surfacesArticular surface
This invention is directed to orthopedic implants and systems. The invention also relates to methods of implant design, manufacture, modeling and implantation as well as to surgical tools and kits used therewith. The implants are designed by analyzing the articular surface to be corrected and creating a device with an anatomic or near anatomic fit; or selecting a pre-designed implant having characteristics that give the implant the best fit to the existing defect.
Owner:CONFORMIS
Minimally Invasive Joint Implant with 3-Dimensional Geometry Matching the Articular Surfaces
InactiveUS20110066245A1Facilitating the integration of a wide variety of cartilageIncrease successFinger jointsWrist jointsArticular surfacesArticular surface
This invention is directed to orthopedic implants and systems. The invention also relates to methods of implant design, manufacture, modeling and implantation as well as to surgical tools and kits used therewith. The implants are designed by analyzing the articular surface to be corrected and creating a device with an anatomic or near anatomic fit; or selecting a pre-designed implant having characteristics that give the implant the best fit to the existing defect.
Owner:CONFORMIS
Diamond-surfaced cup for use in a prosthetic joint
InactiveUS6488715B1Improve wear resistanceReduce coefficient of frictionFinger jointsWrist jointsArticular surfacesSacroiliac joint
Prosthetic joints, components for prosthetic joints, superhard bearing and articulation surfaces, diamond bearing and articulation surfaces, substrate surface topographical features, materials for making joints, bearing and articulation surfaces, and methods for manufacturing and finishing the same, and related information are disclosed, including a diamond-surfaced cup for use in a prosthetic joint.
Owner:DIAMICRON
Methods and devices for utilizing thermal energy to bond, stake and/or remove implants
ActiveUS20090024161A1Short cycleSuture equipmentsUltrasonic/sonic/infrasonic diagnosticsThermal energyBody tissue
A fastener including material meltable at a temperature not likely to produce substantial tissue necrosis of neighboring body tissue, or “bondable material”, is caused to soften or melt by the application of vibratory energy, advantageously including ultrasonic vibratory energy. Vibratory energy is applied using a horn applied to the fastener, and tuned to generate vibratory motion proximate the horn, or at a point distal to the horn, for example at a point along the fastener body, or at the end of the fastener. Melted or softened material of the fastener bonds to a contacting surface, which may be body tissue or another implant. The contacting surface may also include bondable material, softenable or meltable through vibratory energy derived from contact with the fastener. To improve a bond, particularly where dissimilar materials are to be bonded, one or more contacting surfaces is provided with a roughened or porous surface, or a surface including one or more cavities or projections into or onto which softened or melted bondable material may form, bonding once the bondable material has cooled.
Owner:P TECH
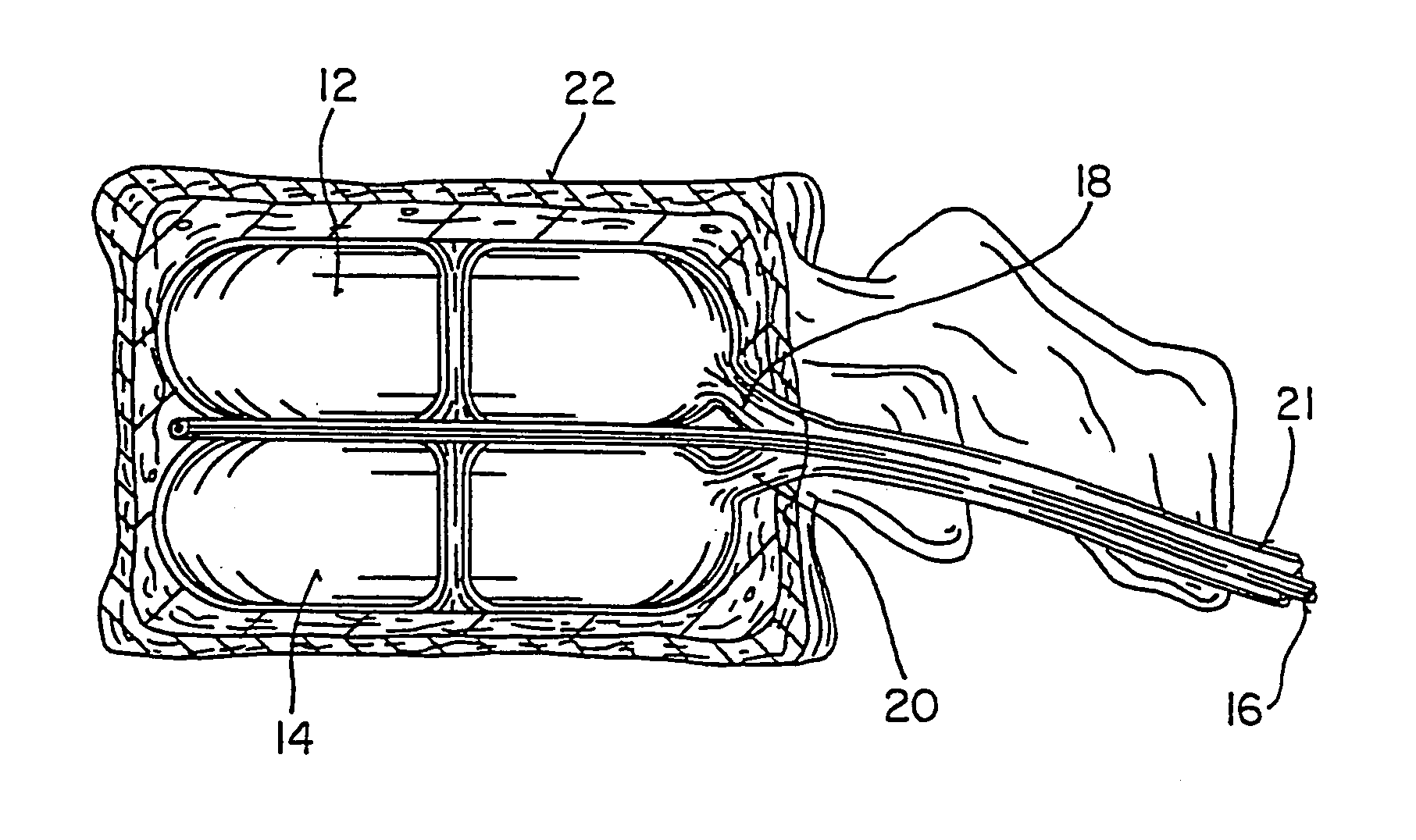
Devices and methods using an expandable body with internal restraint for compressing cancellous bone
Devices and methods compress cancellous bone. In one arrangement, the devices and methods make use of an expandable body that includes an internal restraint coupled to the body. The internal restraint directs expansion of the body. In one arrangement, a method for treating bone inserts the device having the internal restraint inside bone and causes directed expansion of the body in cancellous bone. Cancellous bone is compacted by the directed expansion.
Owner:ORTHOPHOENIX
Custom radiographically designed cutting guides and instruments for use in total ankle replacement surgery
ActiveUS8337503B2High precisionSimplify operating proceduresWrist jointsAnkle jointsTibiaSacroiliac joint
A system comprised of custom radiographically designed tibial and talar cutting guides, a tibial reaming guide and bit, and instrumentalities for use in total ankle replacement surgery and a computer-based system and method for making the custom radiographically designed tibial and talar cutting guides.
Owner:LIAN GEORGE JOHN
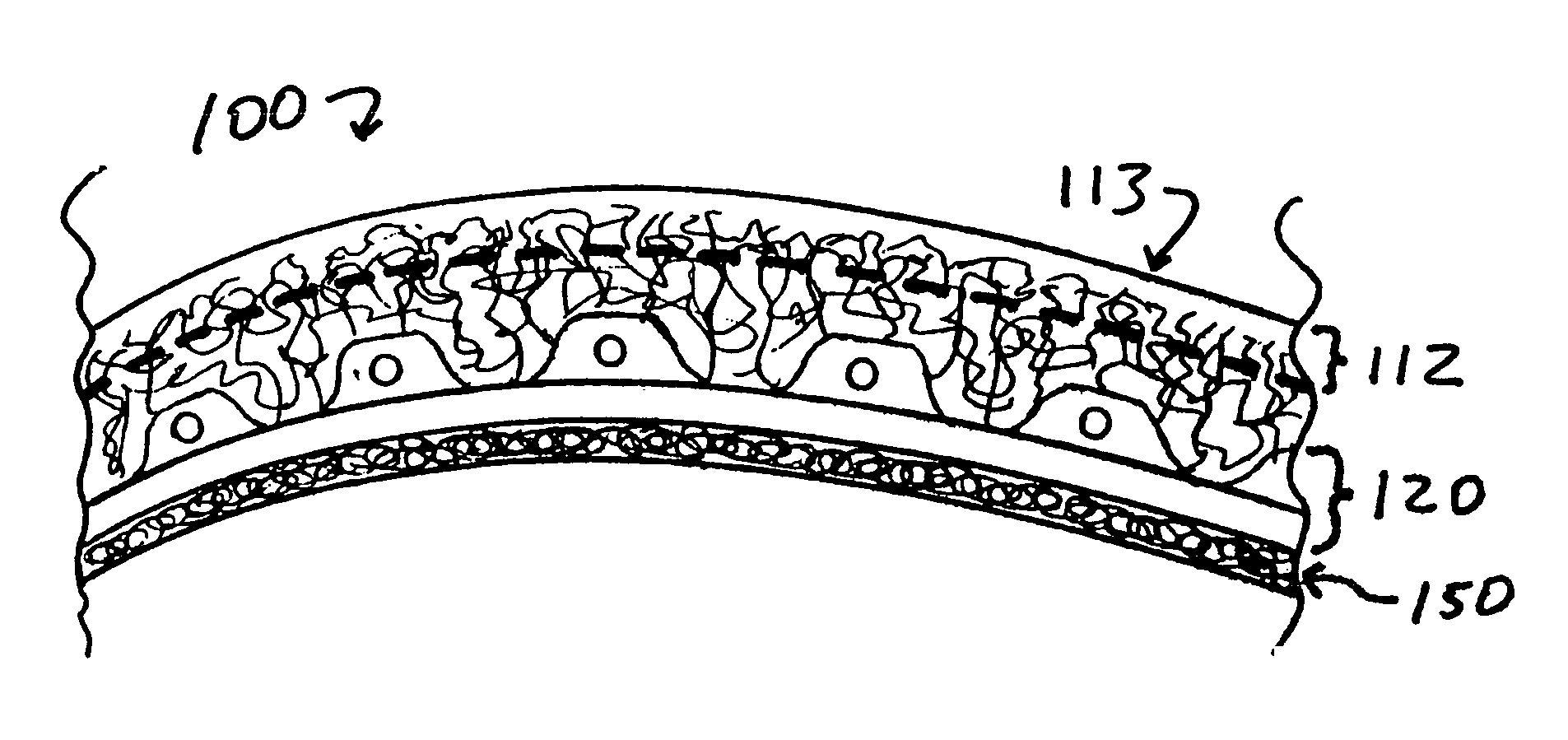
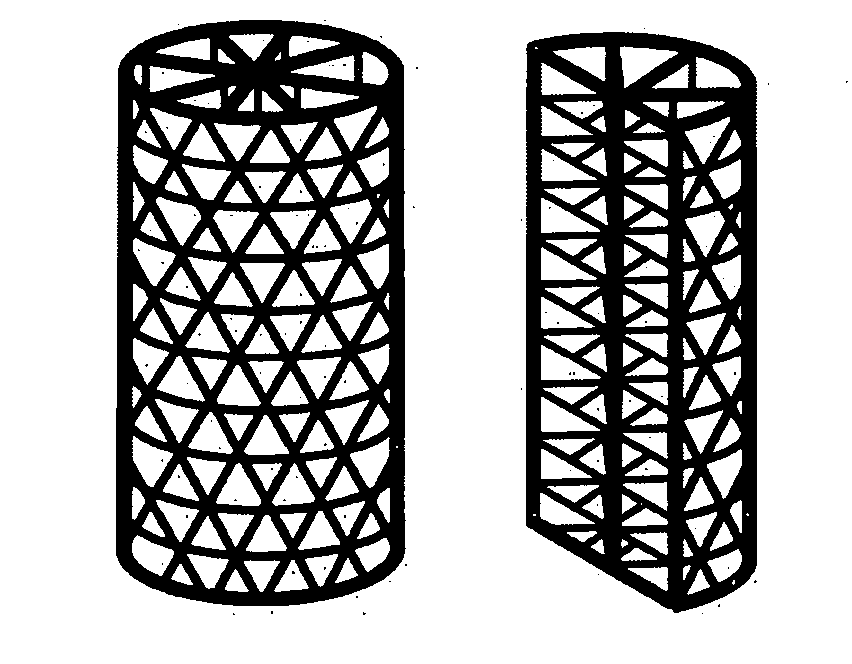
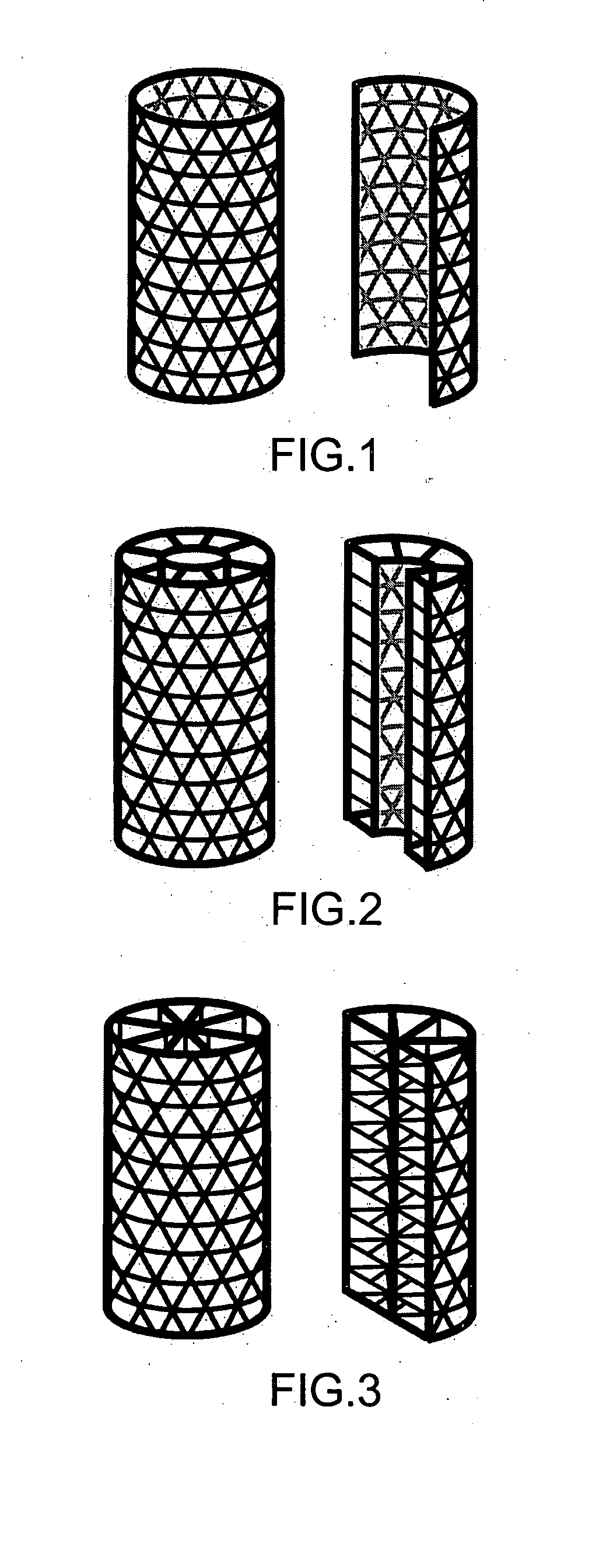
Tissue integration design for seamless implant fixation
The present invention relates to orthopaedic implants having a fenestrated hollow shell and a biologic core. These design features provide an improved interface between the implant and the surrounding tissue, aiding fixation, and provide a vehicle for applying new bone healing and enhancing modalities, such as gene therapy, tissue engineering, and growth factors.
Owner:BIEDERMANN TECH GMBH & CO KG
Knee joint prosthesis
InactiveUS20050043808A1Eliminate the effects ofImprove propertiesImpression capsAnkle jointsTissue repairProsthesis
A method, and related composition and apparatus for repairing a tissue site. The method involves the use of a curable polyurethane biomaterial composition having a plurality of parts adapted to be mixed at the time of use in order to provide a flowable composition and to initiate cure. The flowable composition can be delivered using minimally invasive means to a tissue site and there fully cured provide a permanent and biocompatible prosthesis for repair of the tissue site. Further provided are a mold apparatus, e.g., in the form of a balloon or tubular cavity, for receiving a biomaterial composition, and a method for delivering and filling the mold apparatus with a curable composition in situ to provide a prosthesis for tissue repair.
Owner:ADVANCED BIO SURFACE
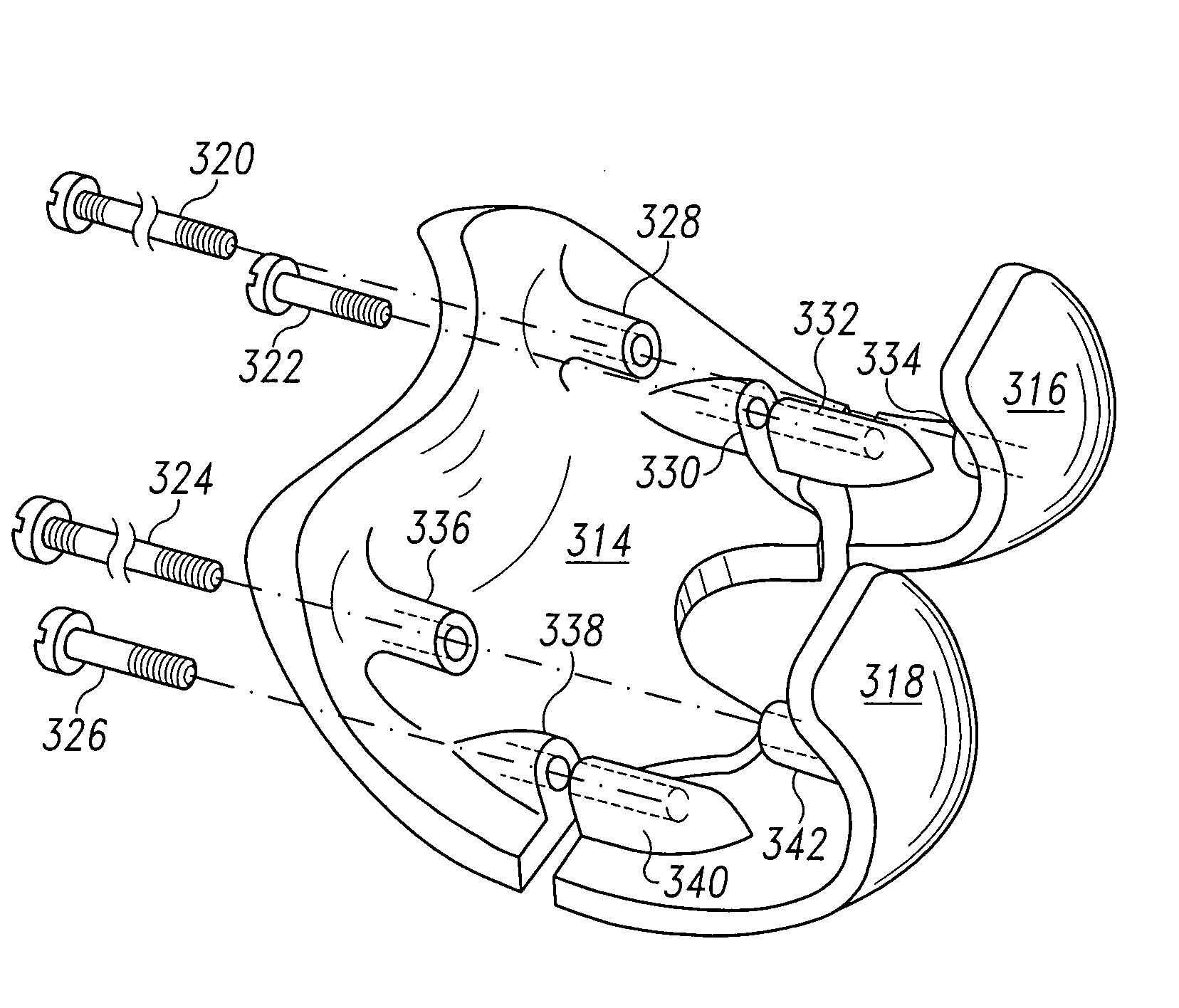
Systems and methods for compartmental replacement in a knee
A knee replacement system provides a knee implant that may be used to more accurately replicate the diameter of a natural knee. In one embodiment, a patellofemoral component is connected to the posterior portion of a condylar component by screws that pass through the femur allowing the patellofemoral component and the condylar component to be torqued against opposing sides of the femur. Two additional screws are used to connect the patellofemoral component to an anterior portion of the condylar component. A gap may be left between the patellofemoral component and the anterior portion of the condylar component if needed to provide precise replication of the diameter of the natural knee from the patellofemoral component to the condylar component.
Owner:DEPUY PROD INC
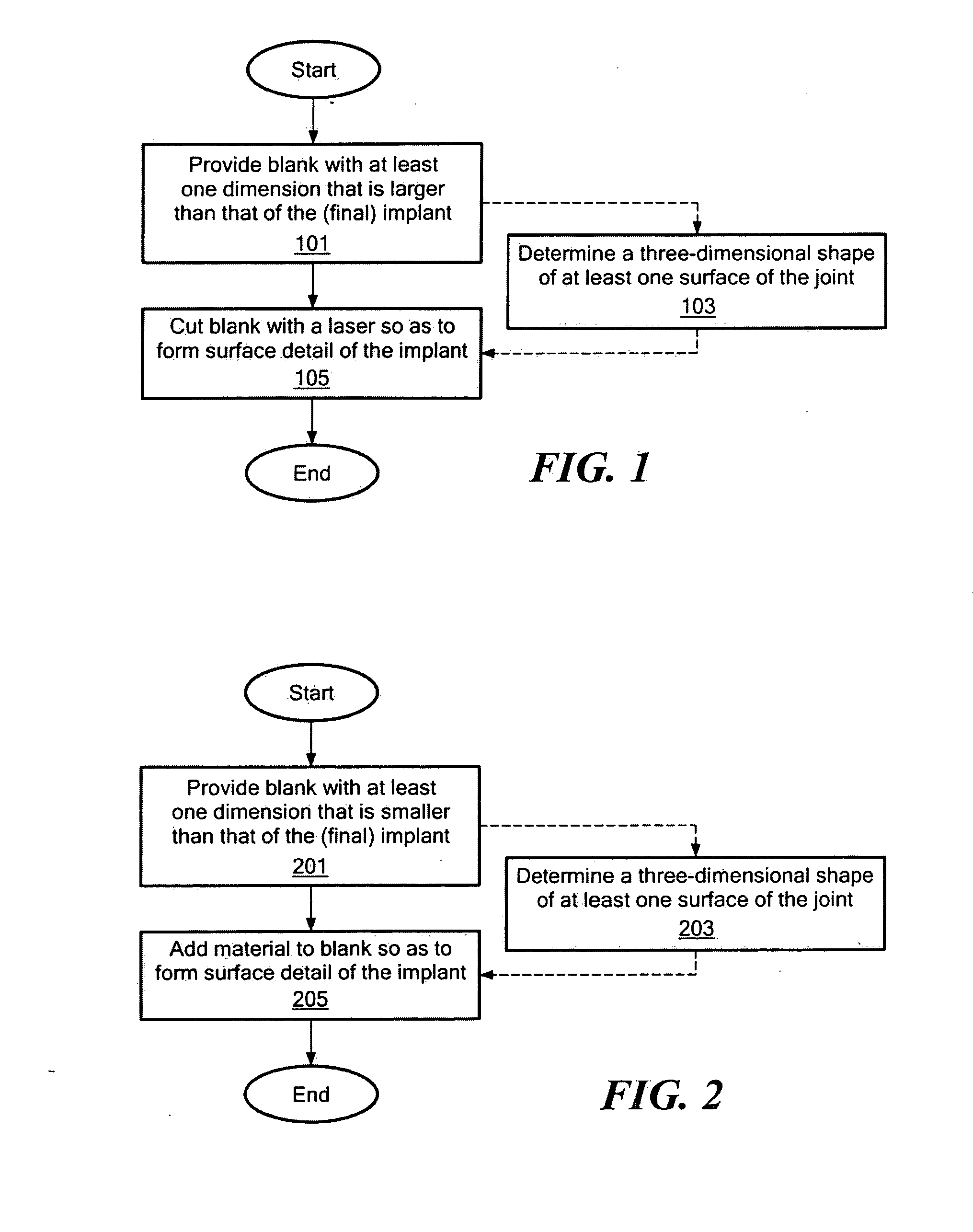
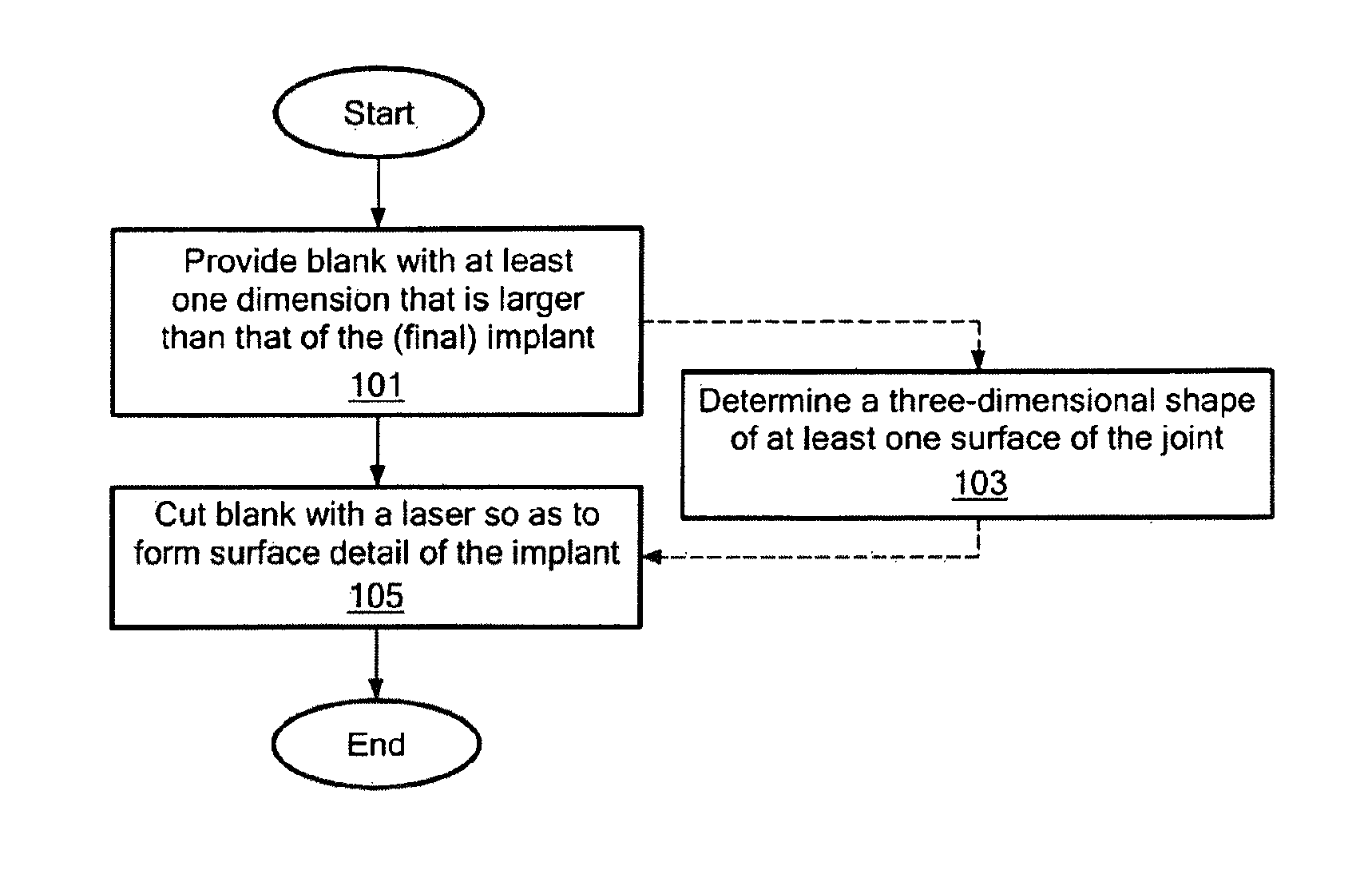
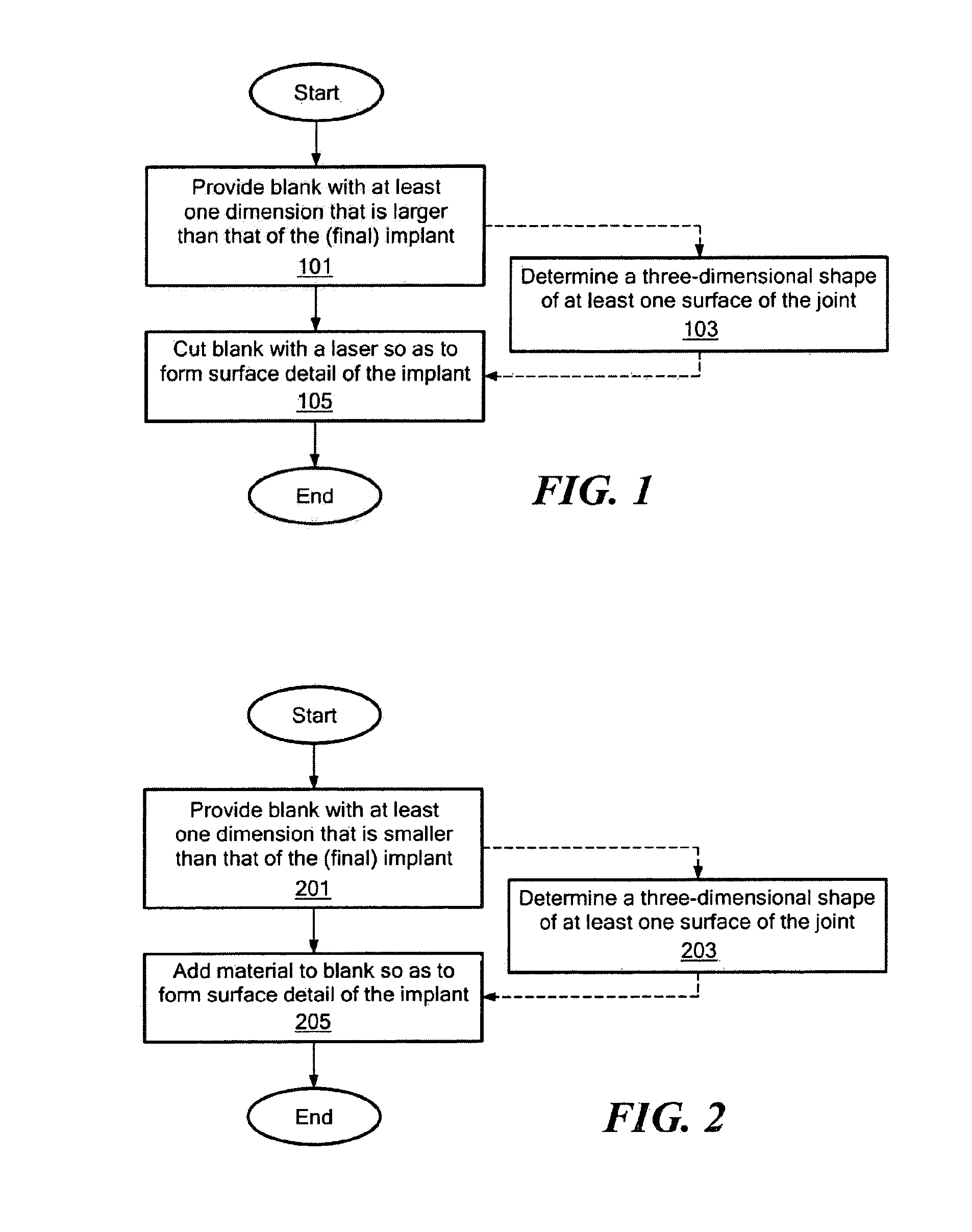
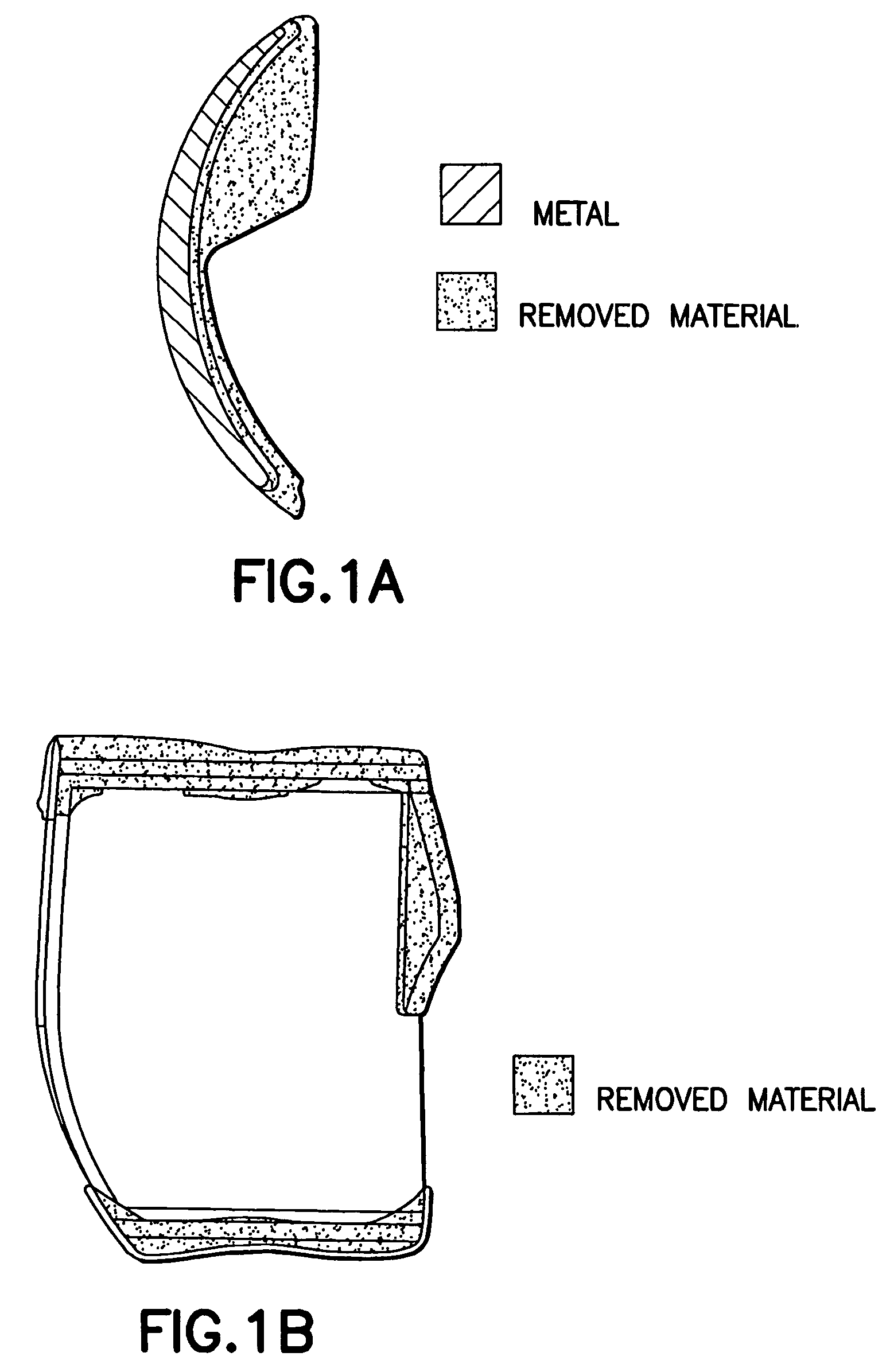
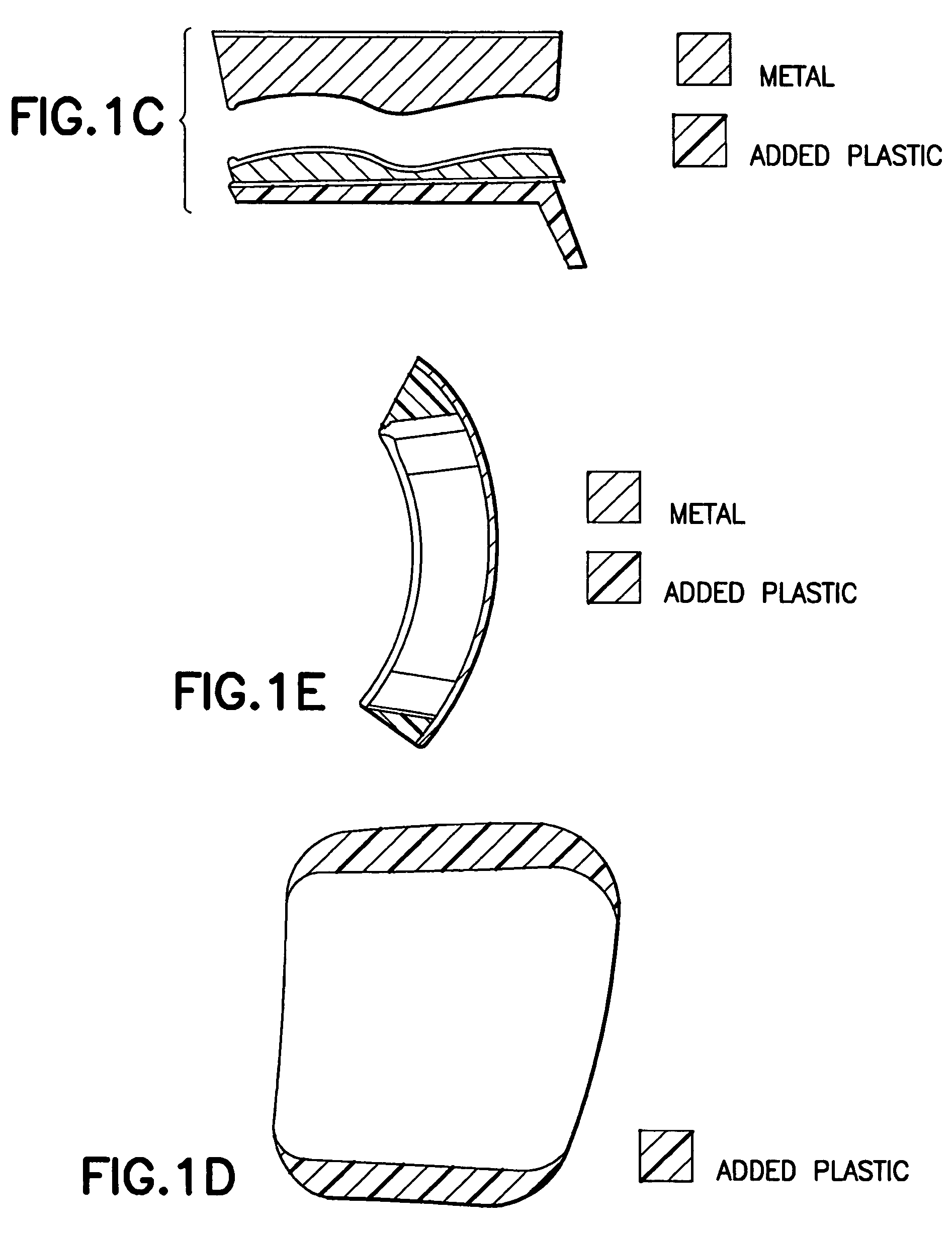
Implant device and method for manufacture
Disclosed are systems, devices and methods for optimizing the manufacture and / or production of patient-specific orthopedic implants. The methods include obtaining image data of a patient, selecting a blank implant to be optimized for the patient, and modifying the blank implant utilizing techniques disclosed herein to alter specific features of the implant to conform to the patient's anatomy.
Owner:CONFORMIS
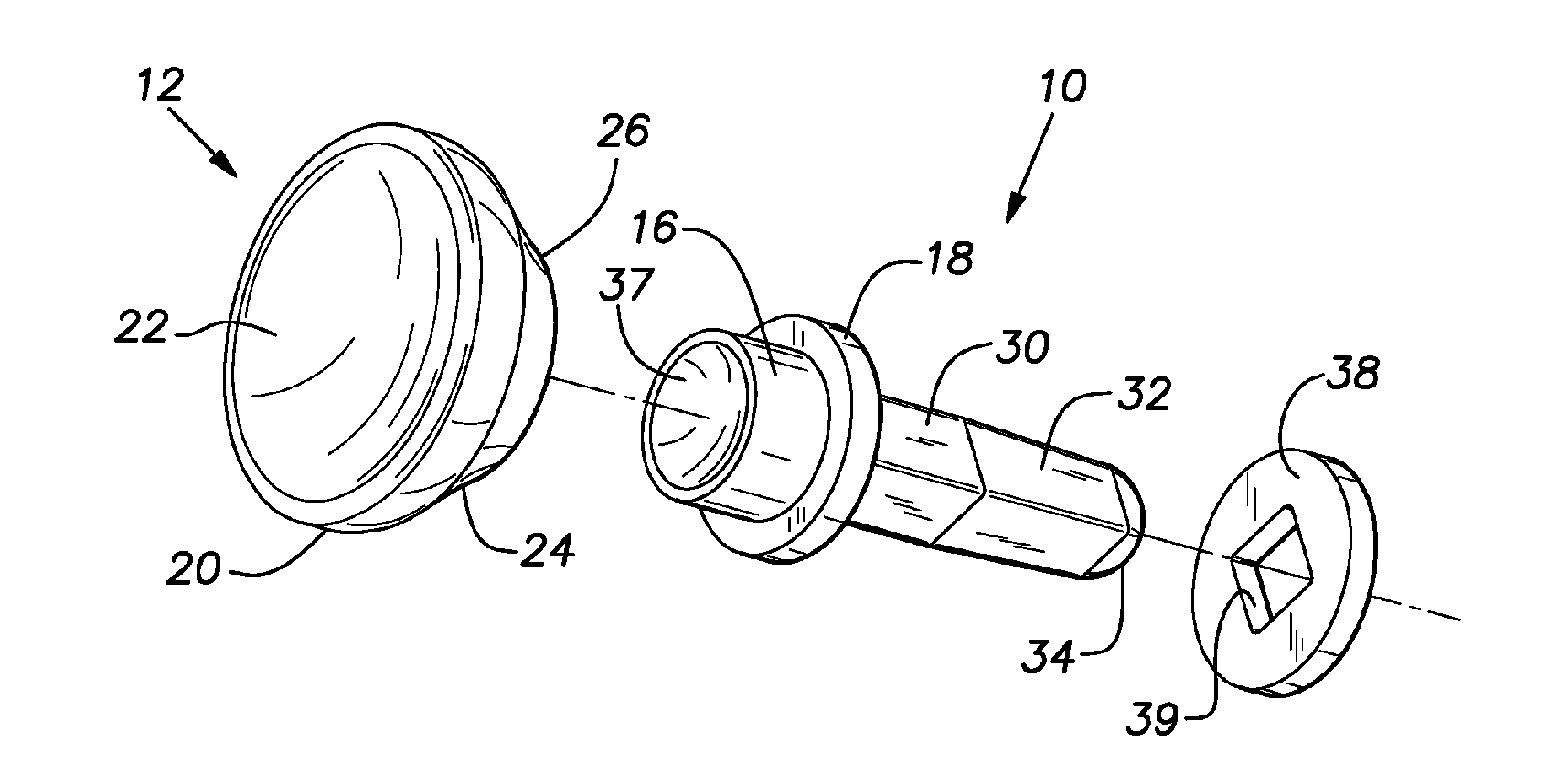
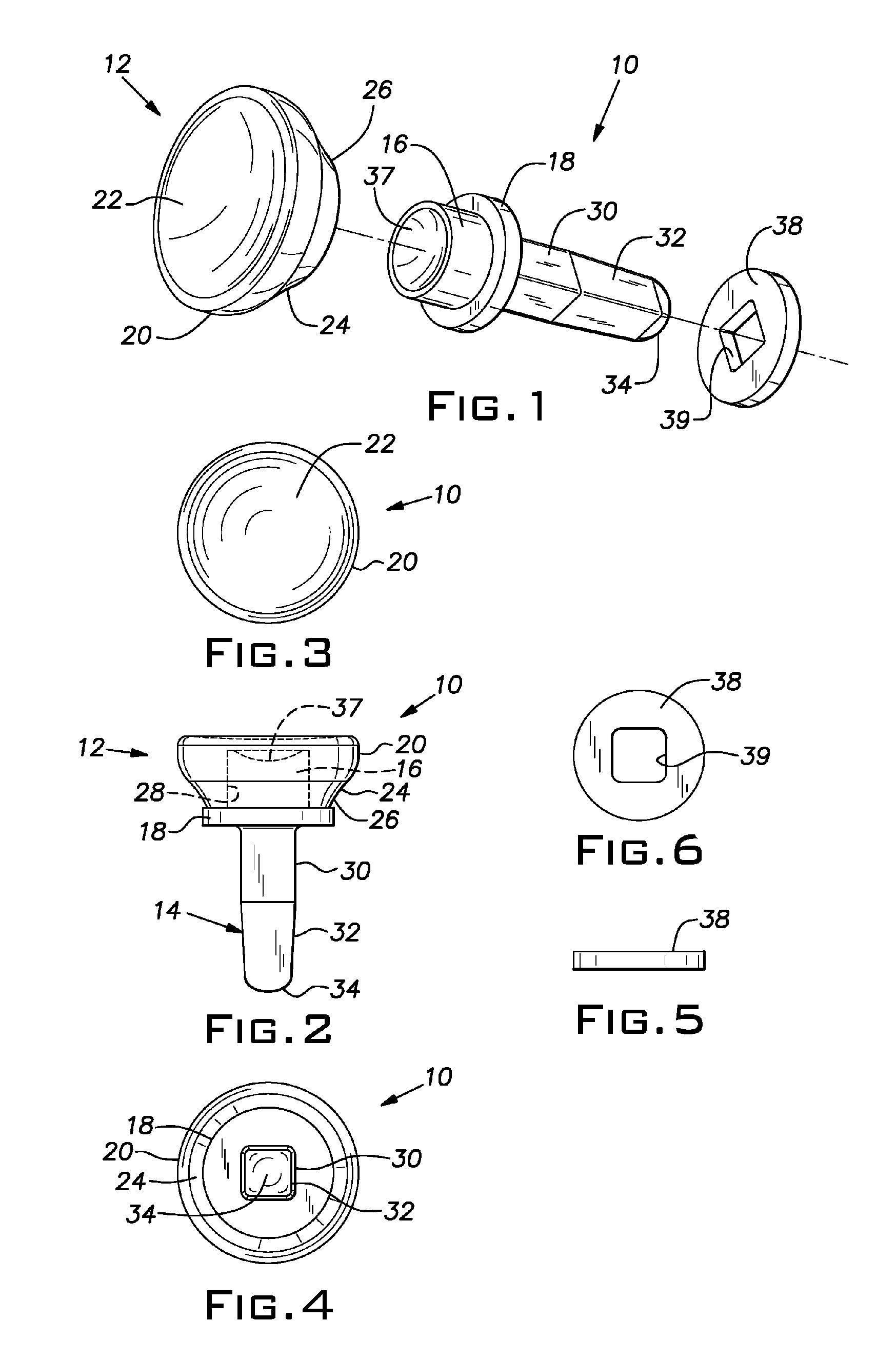
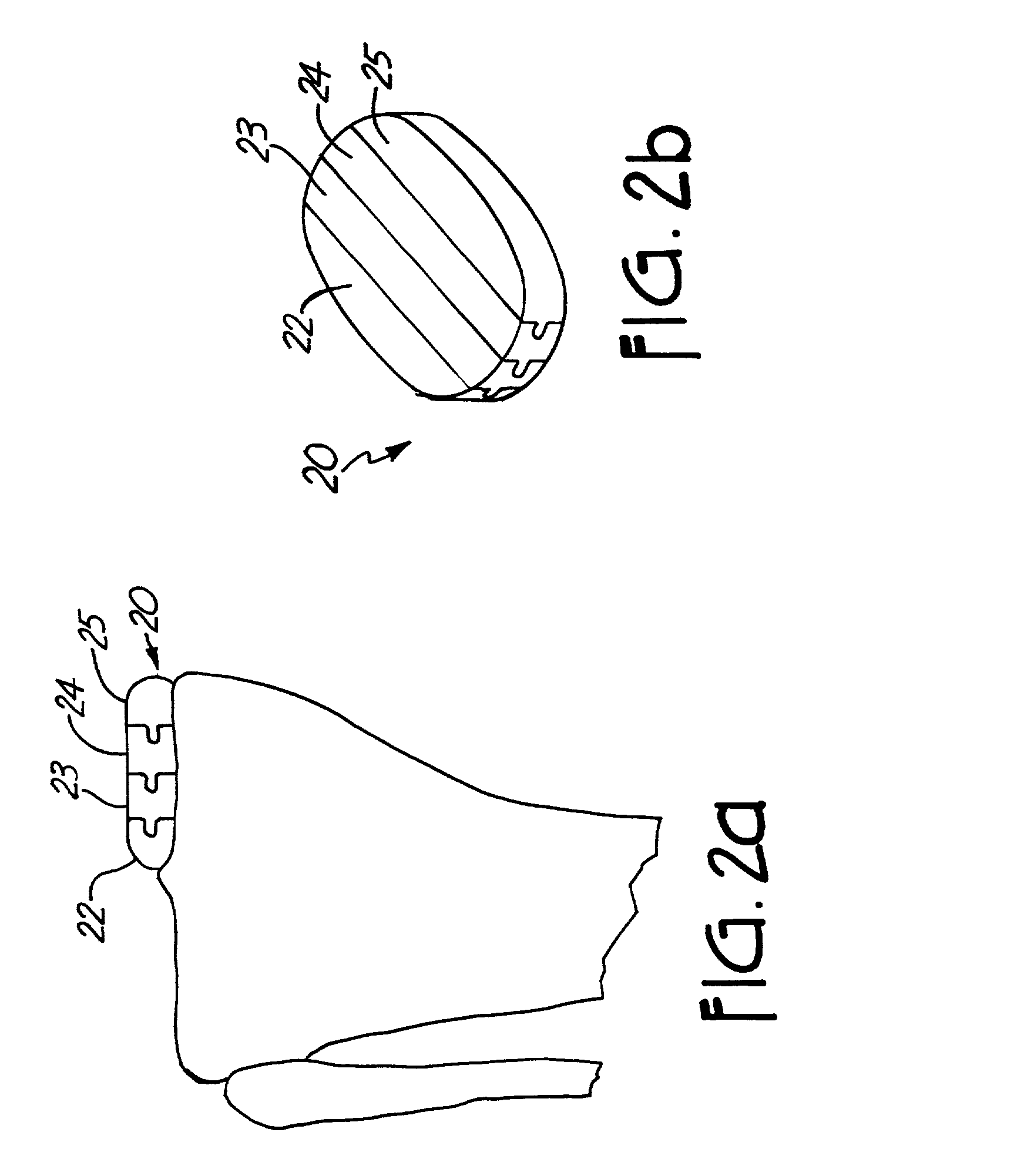
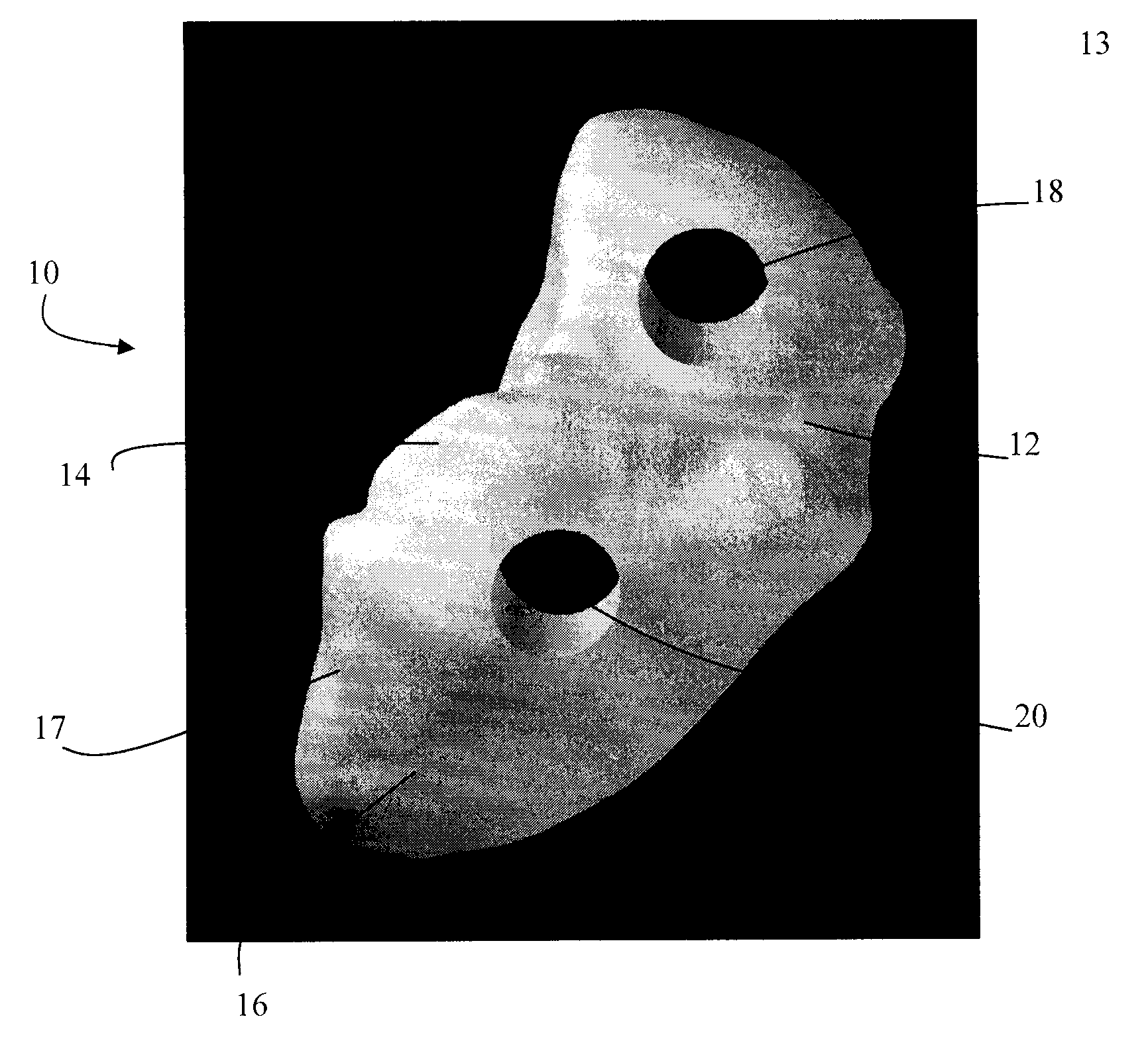
Small joint orthopedic implants and their manufacture
ActiveUS20060052725A1Simple processLarge inventoryFinger jointsWrist jointsBone CortexCancellous bone
A technique to manufacture small joint orthopedic implants includes the steps of taking standard radiographs of a pathologic joint and the corresponding non-pathologic joint. In order to provide an accurate frame of reference, a specialized marker is placed in the radiographic field. By inspection of the radiographs and by comparison with the marker, the dimensions of the cortical bone and the cancellous bone can be quickly and accurately determined. These dimensions can be used to manufacture a suitable implant and installation tool. Typically, the implant will include a stem from which a post projects. A radially extending collar is located at the intersection between the stem and the post. A mating head is attached to the post. The head closely approximates the size and shape of the natural head being replaced. The stem will be non-round in cross-section to prevent rotation of the stem in the bone. For many applications, the head will not be fixedly attached to the post, but will be rotatable about the longitudinal axis of the post. One or more spacers that fit about the stem also can be provided in order to adjust the distance that the head projects from the bone.
Owner:SEITZ JR WILLIAM H +1
Method and system for mammalian joint resurfacing
A method and system for the creation or modification of the wear surface of orthopedic joints, involving the preparation and use of one or more partially or fully preformed and procured components, adapted for insertion and placement into the body and at the joint site. In a preferred embodiment, component(s) can be partially cured and generally formed ex vivo and further and further formed in vivo at the joint site to enhance conformance and improve long term performance. In another embodiment, a preformed balloon or composite material can be inserted into the joint site and filled with a flowable biomaterial in situ to conform to the joint site. In yet another embodiment, the preformed component(s) can be fully cured and formed ex vivo and optionally further fitted and secured at the joint site. Preformed components can be sufficiently pliant to permit insertion through a minimally invasive portal, yet resilient enough to substantially assume, or tend towards, the desired form in vivo with additional forming there as needed.
Owner:ADVANCED BIO SURFACE
Ankle prosthesis
A fixed-bearing ankle prosthesis may include tibial and talar components whose articulating surfaces directly contact one another. The tibial component defines medial and lateral concave condylar facets separated by a convex central portion. The talar component includes medial and lateral convex condyles separated by a concave central portion. The condyles each have a single radius of curvature in a medial-lateral plane such that each condyle has a circular-arc cross-section continuously extending from the respective medial or lateral edge of the talar component to the concave central portion. The medial-lateral radii of the condyles are smaller than corresponding radii of the condylar facets.
Owner:UNIV OF IOWA RES FOUND
Systems and methods for treating fractured or diseased bone using expandable bodies
Systems and methods treat fractured or diseased bone by deploying more than a single therapeutic tool into the bone. In one arrangement, the systems and methods deploy an expandable body in association with a bone cement nozzle into the bone, such that both occupy the bone interior at the same time. In another arrangement, the systems and methods deploy multiple expandable bodies, which occupy the bone interior volume simultaneously. Expansion of the bodies form cavity or cavities in cancellous bone in the interior bone volume.
Owner:ORTHOPHOENIX
Orthopaedic implants
InactiveUS20110004317A1Reduce difficultyReduce disadvantagesAdditive manufacturing apparatusWrist jointsPlastic surgerySurgical department
A method for making an orthopaedic implant, the method comprising: characterizing at least a portion of a bone corresponding to the bone to be replaced, said corresponding bone being on the contralateral side of the patient; providing a model of the orthopaedic implant based on a mirror image of the contralateral bone; and forming the orthopaedic implant based on the model.
Owner:MCGILL UNIV
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com