Apparatus and method for performing spinal surgery
a spinal surgery and apparatus technology, applied in the field of spinal surgery, can solve the problems of loss of disc height and alteration of annulus fibrosis, loss of motion at the fused vertebral joint, and significant pain for individuals with damaged or degenerated discs
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
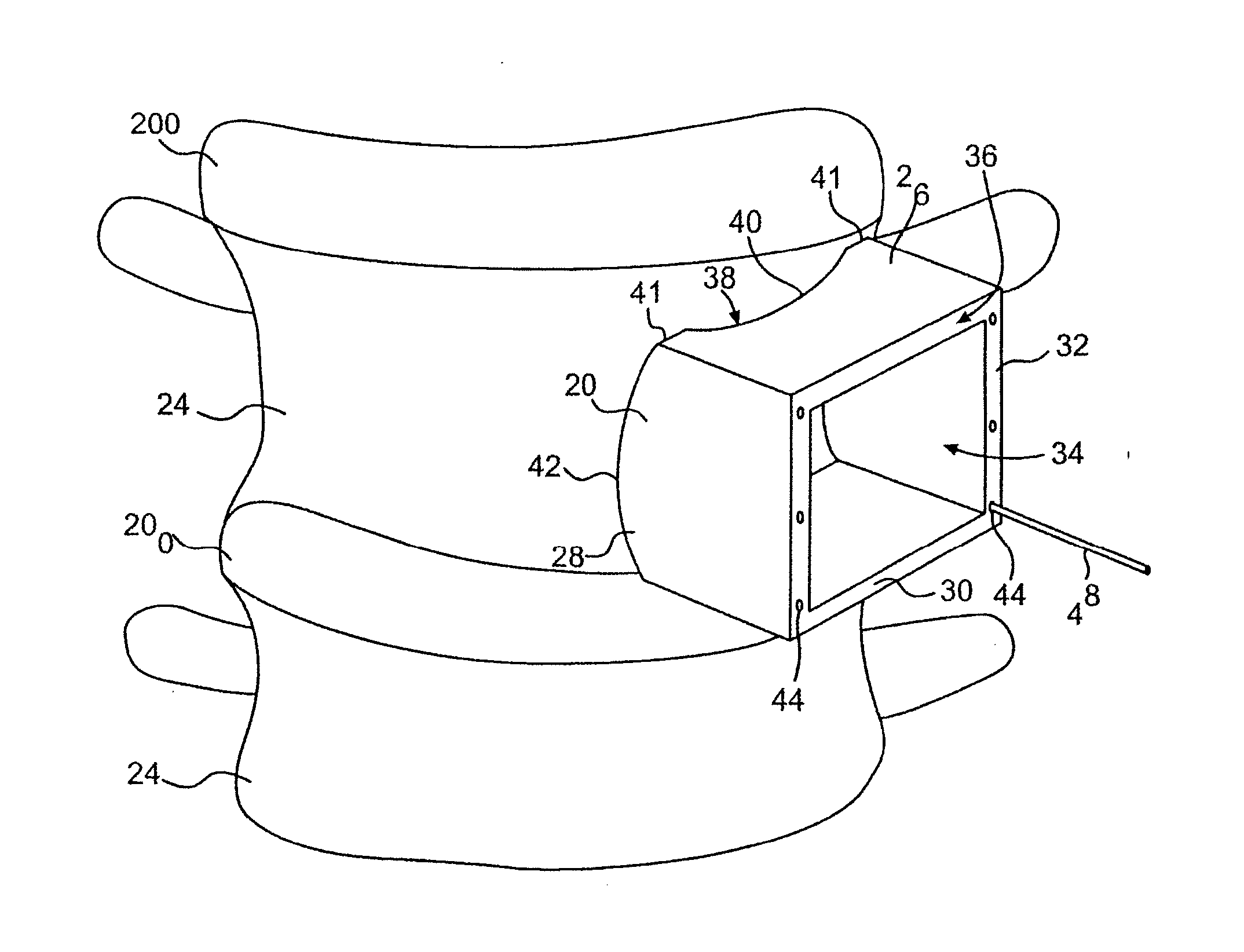
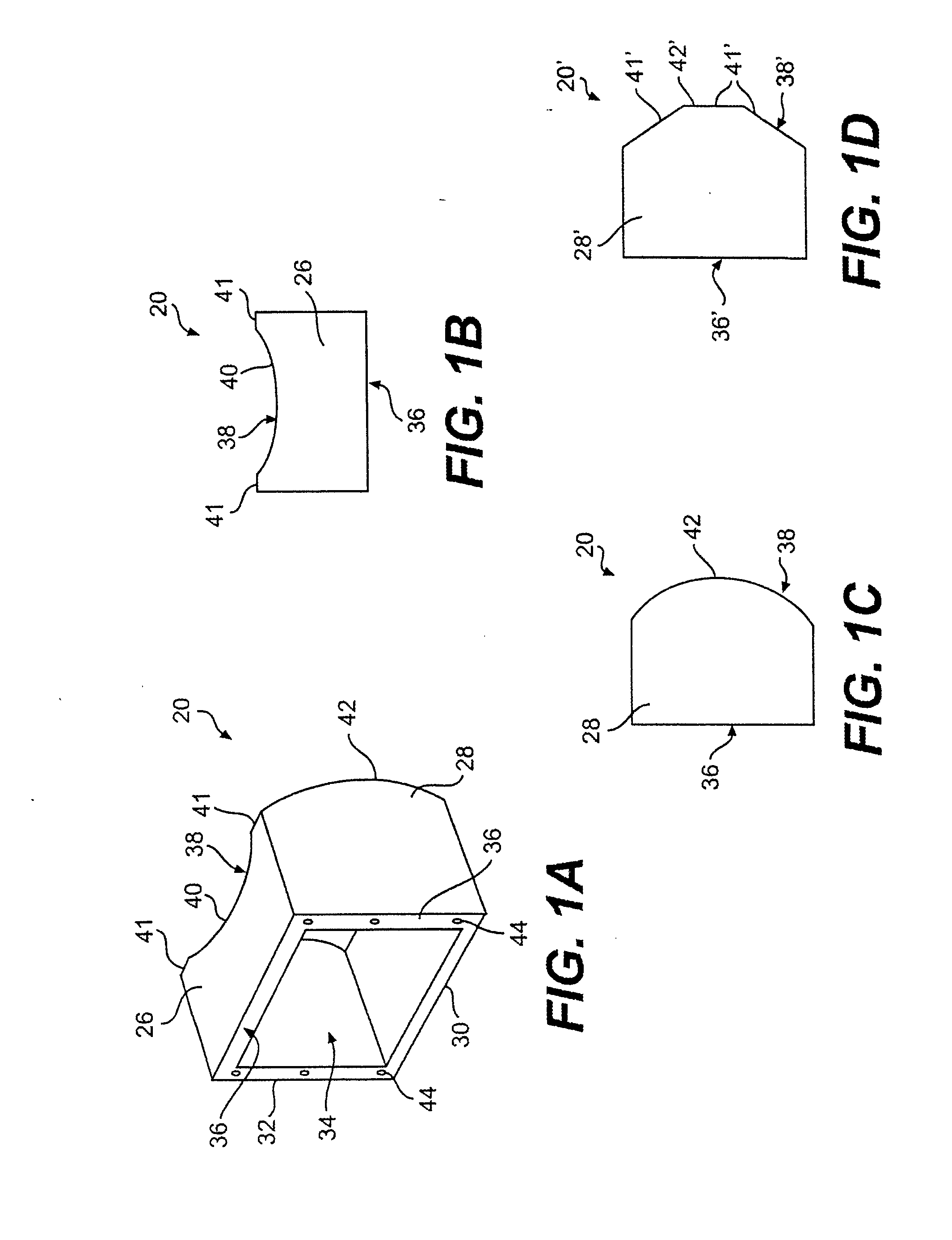
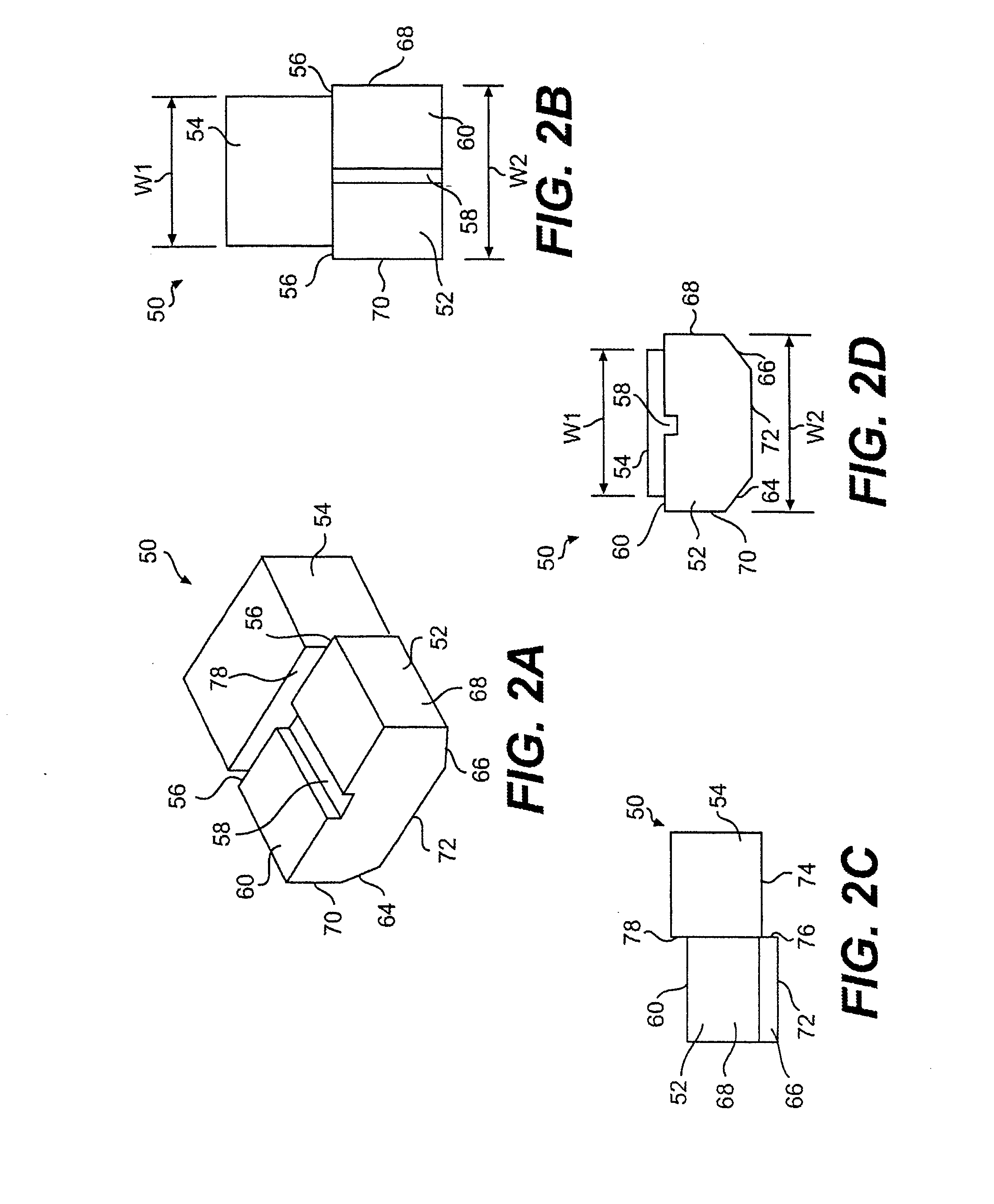
[0067] Referring now to the drawings, wherein like numerals indicate like parts, and initially to FIGS. 1A-1C and 8, there will be seen a cutting guide 20 for use in removing bone 22 from a vertebral body 24. The cutting guide is designed to be placed into contact with the outer surface of the vertebral body 24 to “guide” a surgical instrument as it cuts through the cortical bone of the vertebral body, as shown in FIGS. 8 and 9A-9B and as later described in more detail. In this regard, the cutting guide 20 has a sidewall that defines an internal cavity 34 extending through the cutting guide 20. The sidewall generally has four walls 26, 28, 30, 32 arranged to form a rectangular cross-section. Although the cavity 34 is preferably rectangular in cross section, the walls 26, 28, 30, 32 can be configured to define a cavity that is square in cross-section or any other suitable geometric shape.
[0068] The cutting guide 20 has a first edge 38 to face toward and to contact the vertebral body...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com