Systems and Methods For Placement of Valve Prosthesis System
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
)
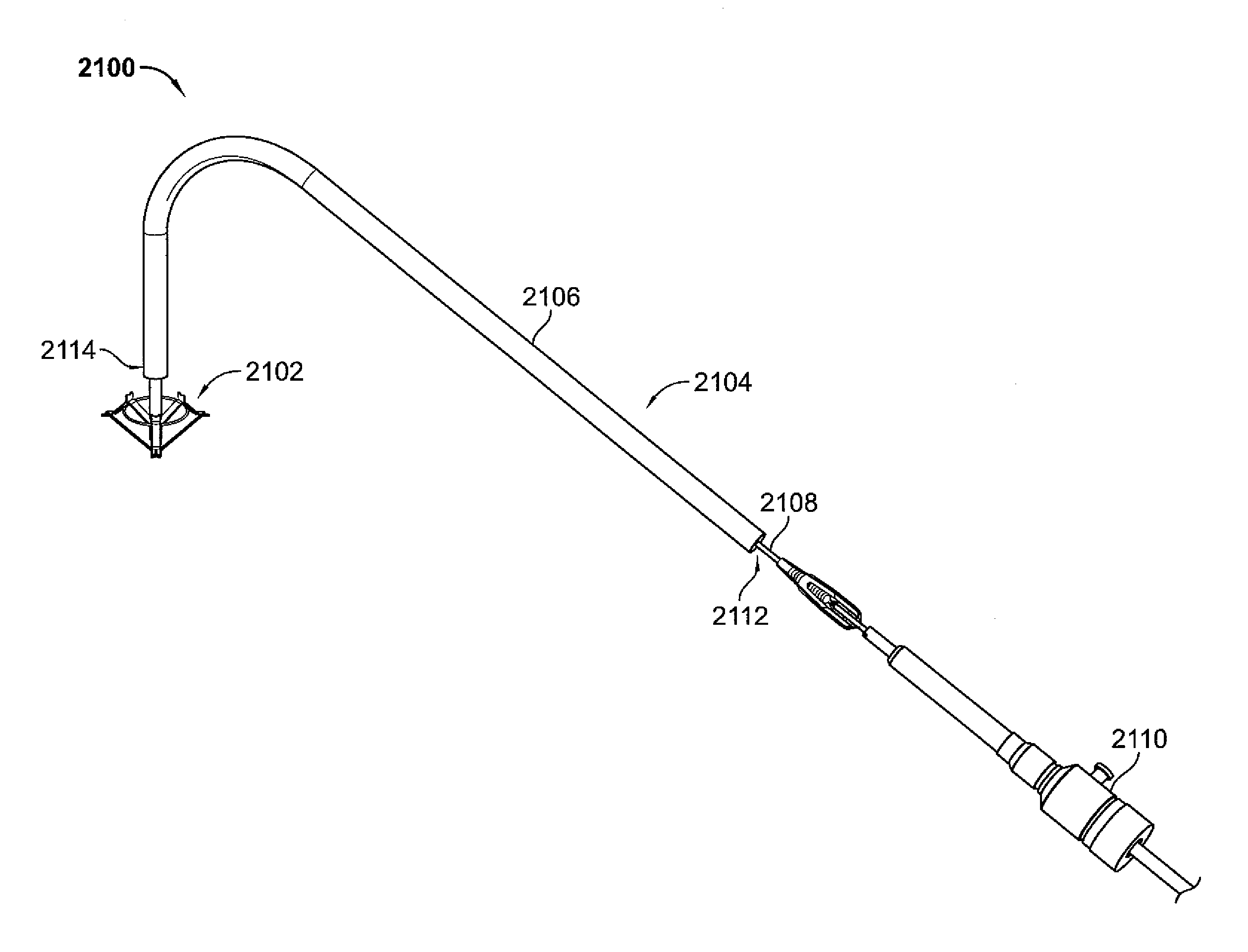
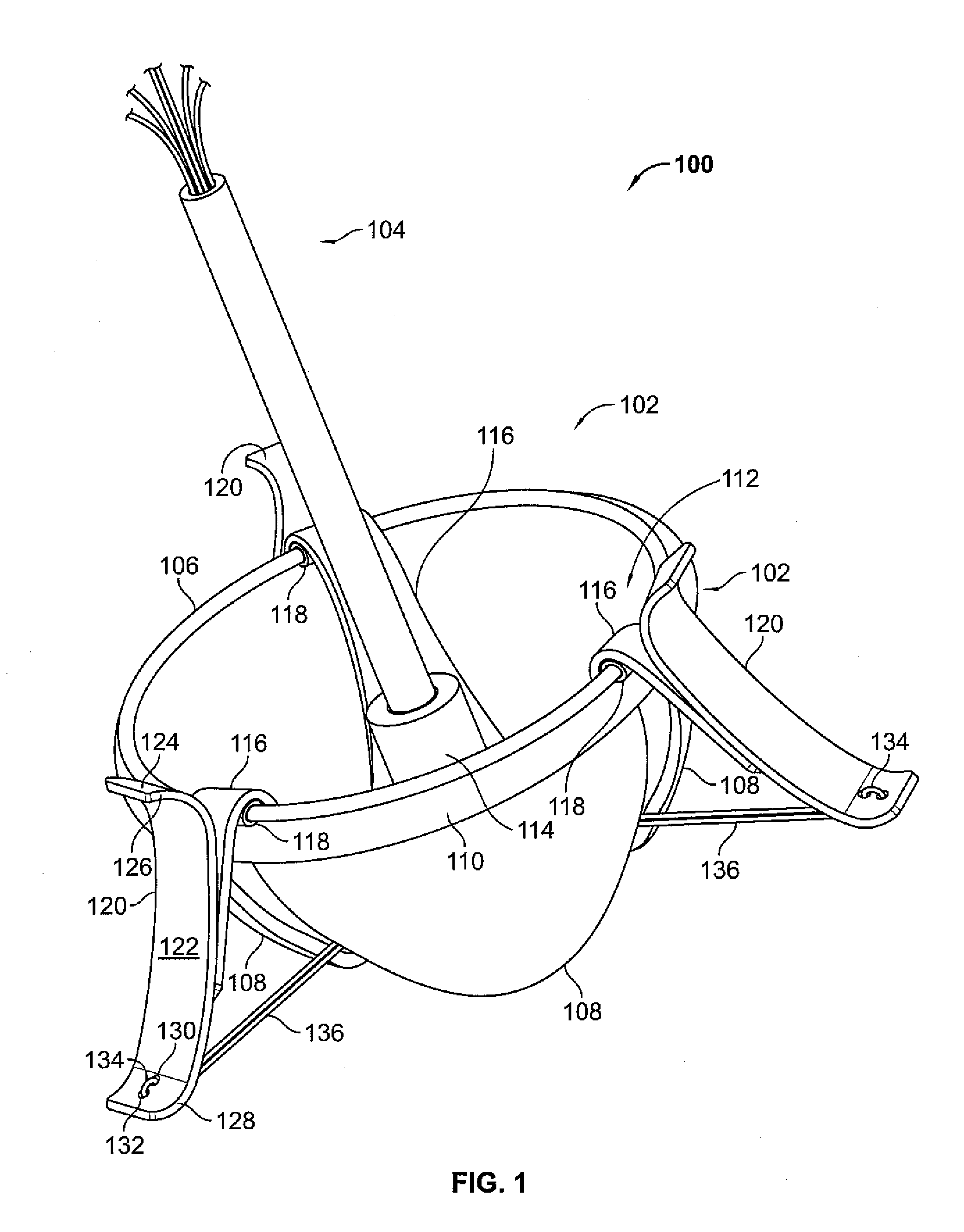
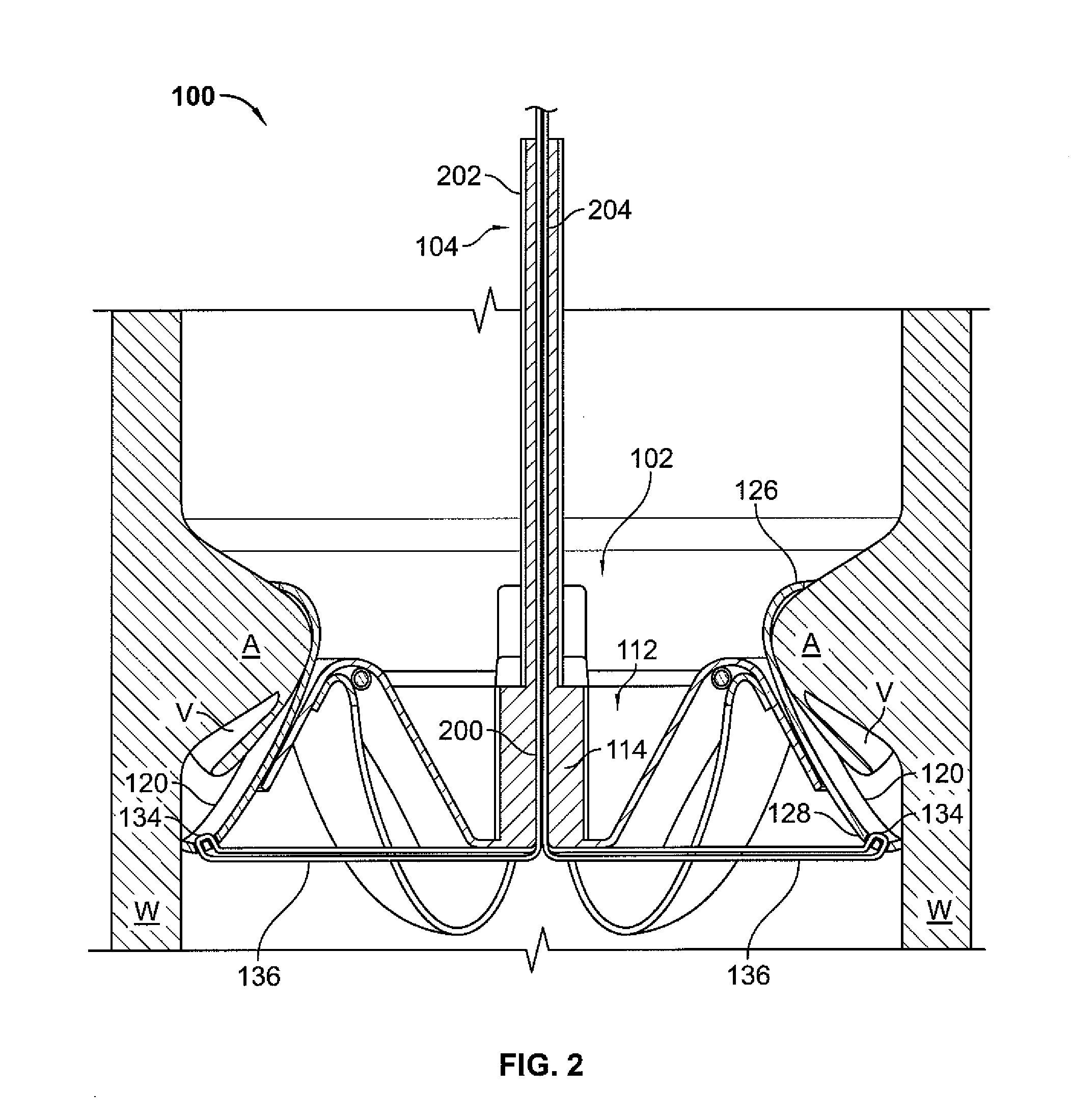
[0055]Advantageous valve prosthesis systems and deployment systems / methods are provided according to the present disclosure. The disclosed systems and methods permit surgeons / clinicians to improve heart valve function without invasive surgical intervention. Indeed, the disclosed valve prosthesis systems permit a heart valve prosthesis to be percutaneously delivered to a desired anatomical location. Once located in the desired anatomical region / locale, the disclosed valve prosthesis system facilitates secure and aligned placement of a heart valve prosthesis relative to a heart annulus. Percutaneous delivery of the disclosed heart valve prosthesis as disclosed herein provides for efficient and effective clinical placement of a heart valve prosthesis. The disclosed heart valve prosthesis and associated delivery techniques offer numerous clinical benefits, including enhanced valve function without the need to remove existing valve leaflets, an ability to effectively and efficiently del...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com