Levator for repair of perineal prolapse
a perineal prolapse and levator technology, applied in the field of urogenital surgery, can solve the problems of dragging feeling, increased importance of problems, and long-standing female genital prolapse, and achieve the effects of preventing or limiting the descent or lateral displacement of these muscles, facilitating and safe access, and enhancing repairs
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
[0031]Referring now to the drawings, wherein like reference numerals designate identical or corresponding parts throughout the several views. The following description is meant to be illustrative only, and not limiting other embodiments of this invention will be apparent to those of ordinary skill in the art in view of this description.
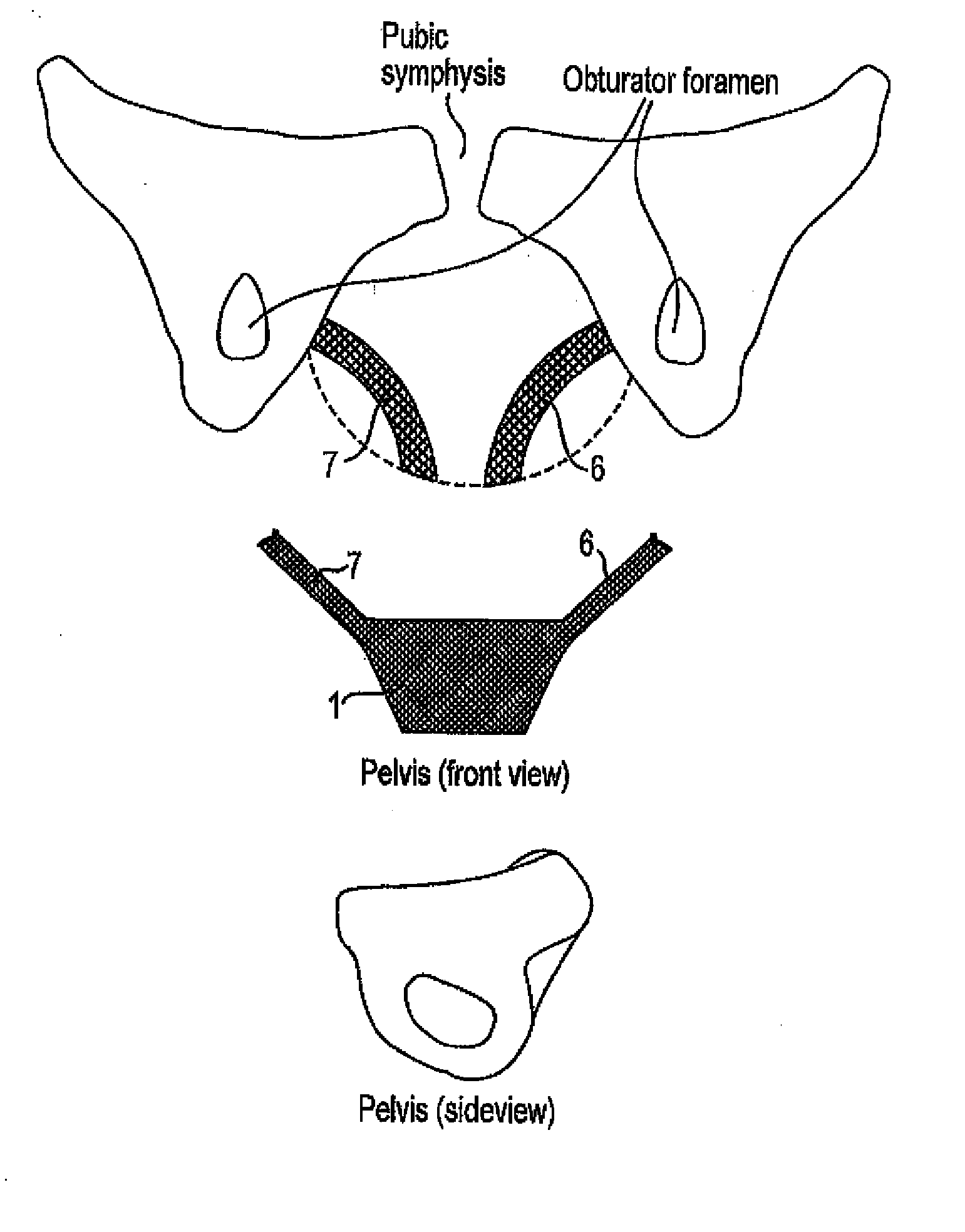
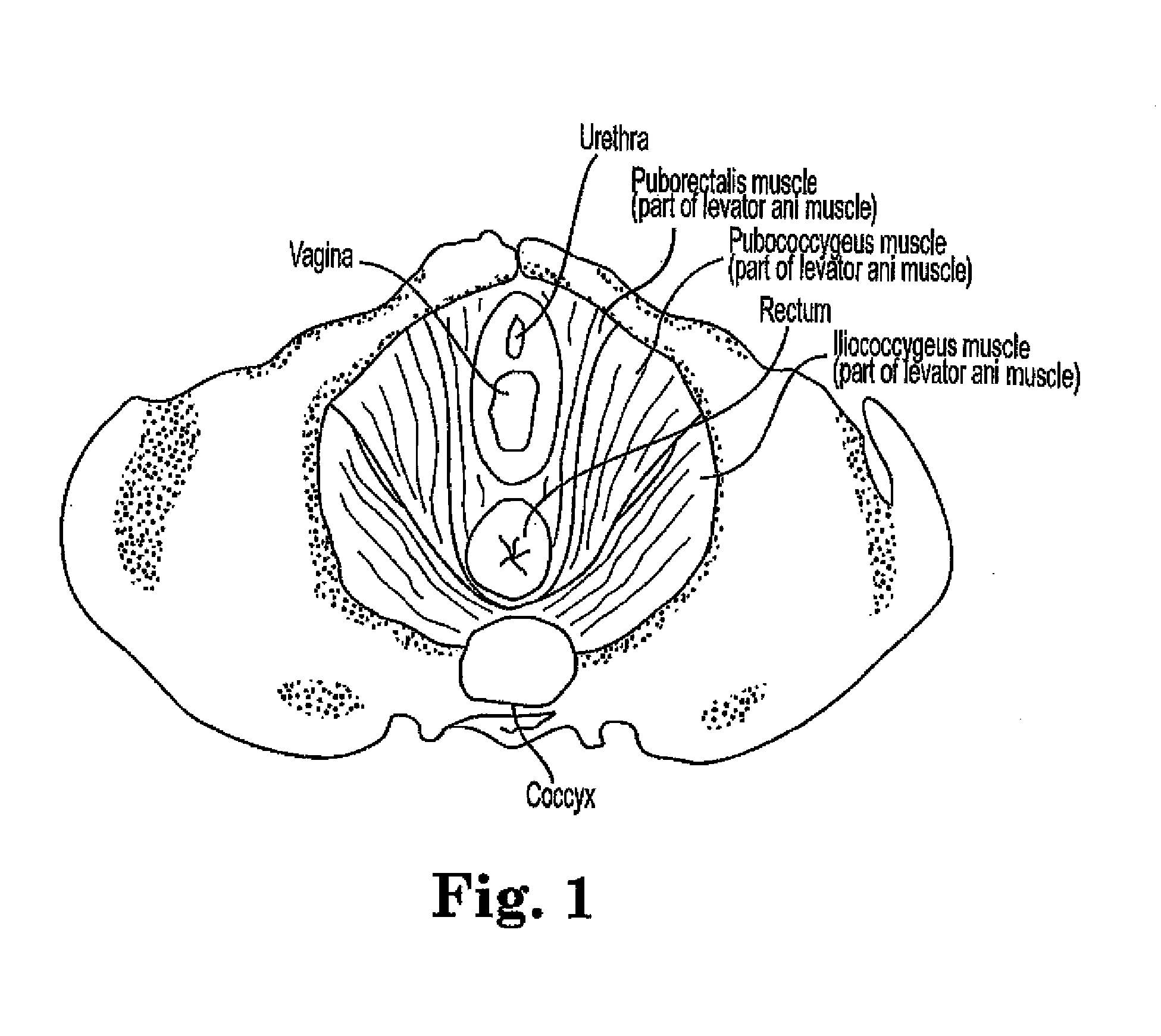
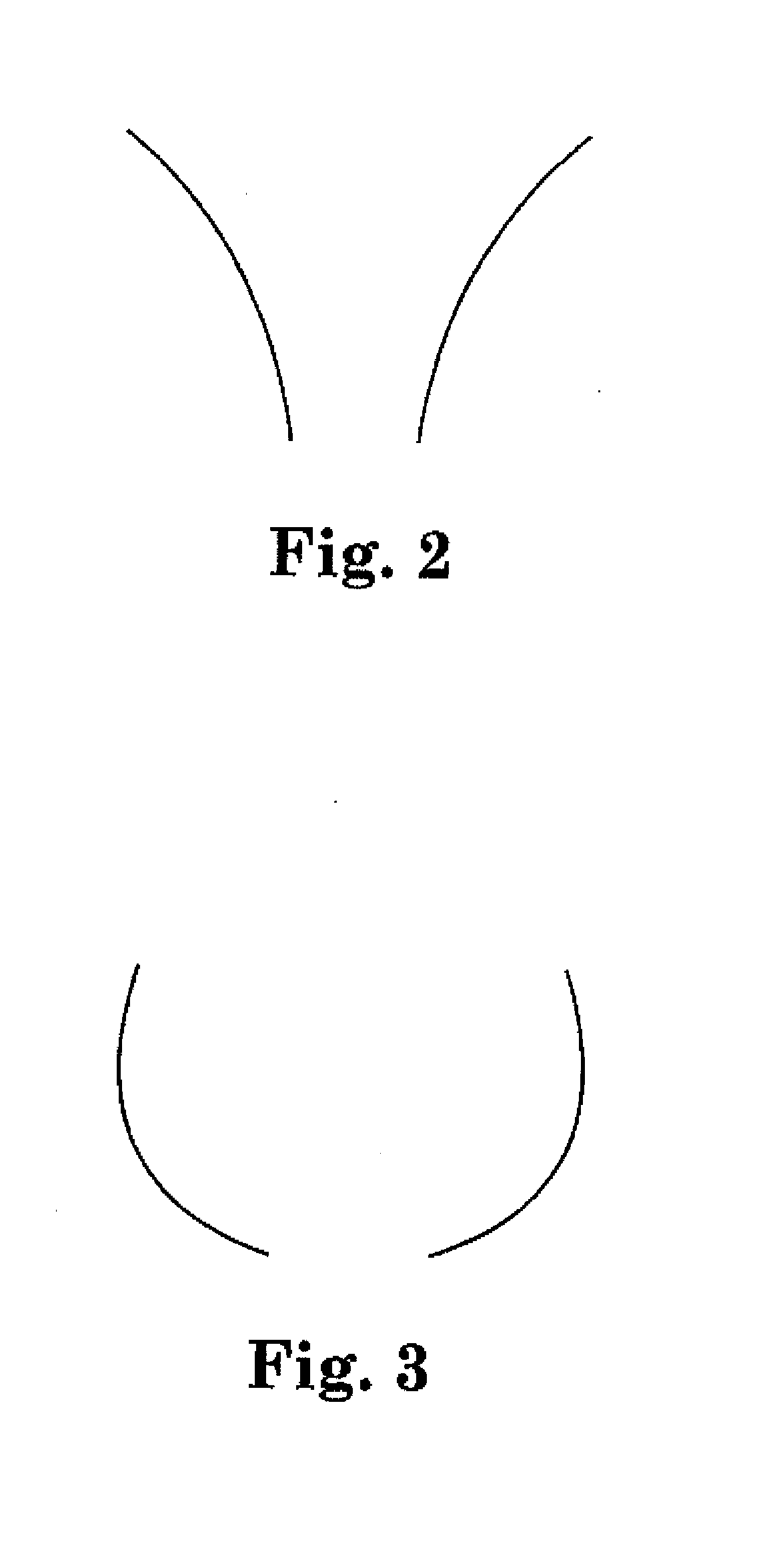
[0032]The relevant anatomy is illustrated in FIG. 1. As can be seen, the levator ani muscles, including the pubococcygeus and illiococcygeus muscles, are a significant portion of the pelvic floor and provide support for the pelvic viscera. FIGS. 1 and 2 show the normal condition of the levator muscles, while FIG. 3 shows the posture of levator muscles associated with prolapsed pelvic organs. As can be seen, such muscles offer less support for the pelvic viscera and may benefit from additional support as provided in the present invention. Further, laxity of such muscles is thought to result in an increased size of the normal opening in the muscles at t...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com