Asthma is a considerable problem, and peak flow meters play a role in the
asthma management strategies that physicians and medical institutions recommend.
Despite the recommendations of medical authorities, use of peak flow meters is far from ubiquitous.
While leading physicians and medical institutions are encouraging self-care through routine peak
airflow monitoring, they are not recommending that the entire burden of
asthma management fall on the shoulders of individual patients.
Furthermore, as threshold devices, they do not facilitate routine measurement in the manner that leading physicians and medical institutions now recommend.
While such mechanical peak flow meters are simple and relatively inexpensive, friction,
inertia, gravity, and other artifacts of mechanical implementation can compromise their accuracy.
Since mechanical peak flow meters typically only display the result of the most recent measurement trial, they do not facilitate presentation of multiple trial results simultaneously—much less the
visualization or exploration of trial data over a range of time scales.
Although electronic peak flow meters typically offer greater measurement accuracy than mechanical peak flow meters, this accuracy comes at a price.
Electronic peak flow meters tend to be significantly more expensive, and are also frequently less intuitive to use.
Significantly, electronic peak flow meters do little at present to capitalize on advantages that
software applications can provide within mobile contexts of use.
Electronic peak flow meters currently require batteries, and can run out of energy at inopportune moments—further eroding ease of use and reliability.
In comparison with alternatives, electronic peak flow meters are more complex to manufacture and more difficult to recycle.
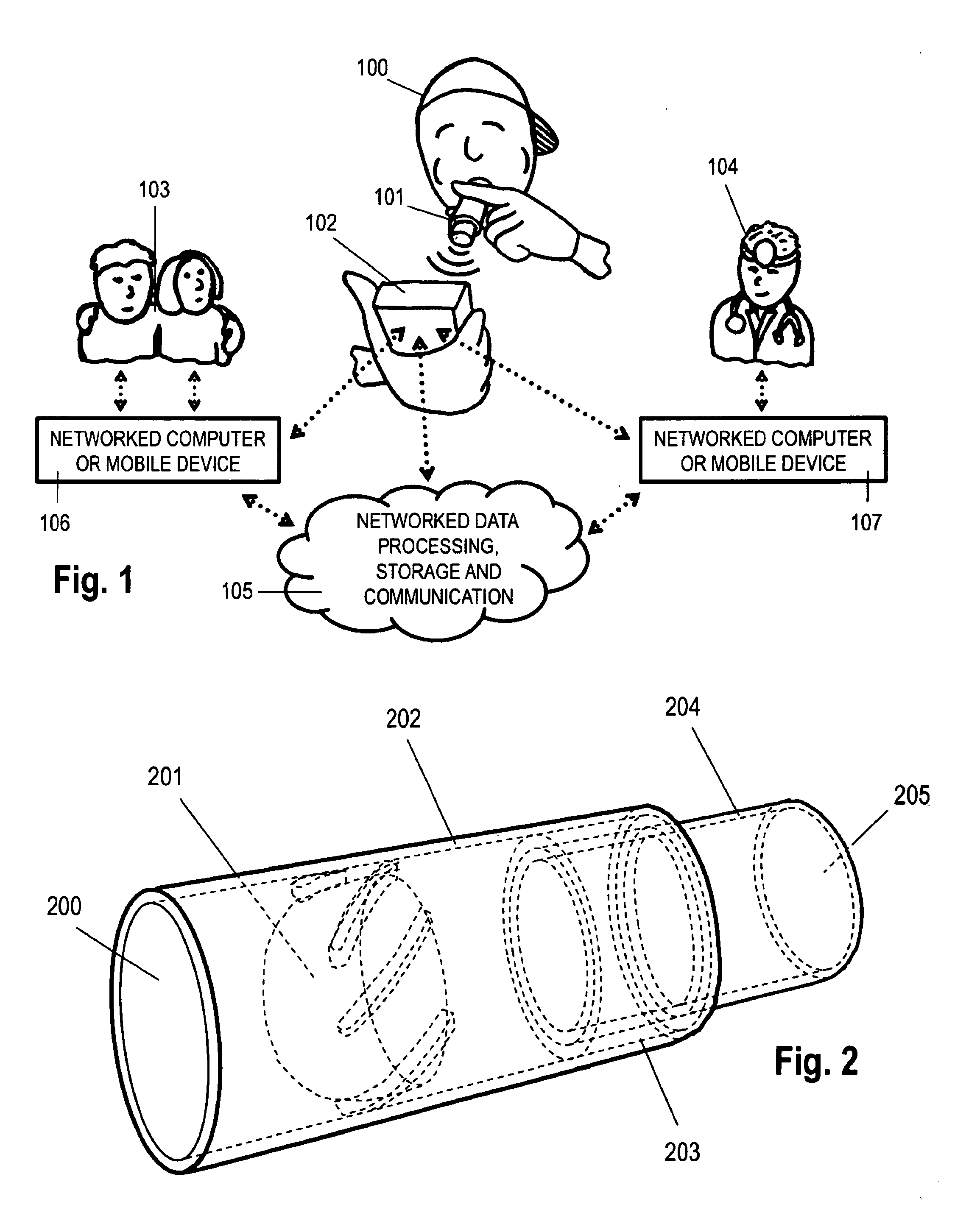
While this investigation introduced the use of a vortex whistle for measurement of expiratory
airflow rate, it did not address how the design of a vortex whistle could be refined for use within the context of a portable monitoring spirometry solution, nor did it consider or address mobile scenarios of use.
Because, however, these solutions employ fluidic oscillators as components within or attached to dedicated electronic peak flow measurement devices or systems, they suffer from many of the previously discussed limitations that are typical of electronic peak flow meters.
Furthermore, the solutions presented within these patents do not capitalize on
audio feedback as a means to reward a user for exhaling as forcefully as possible.
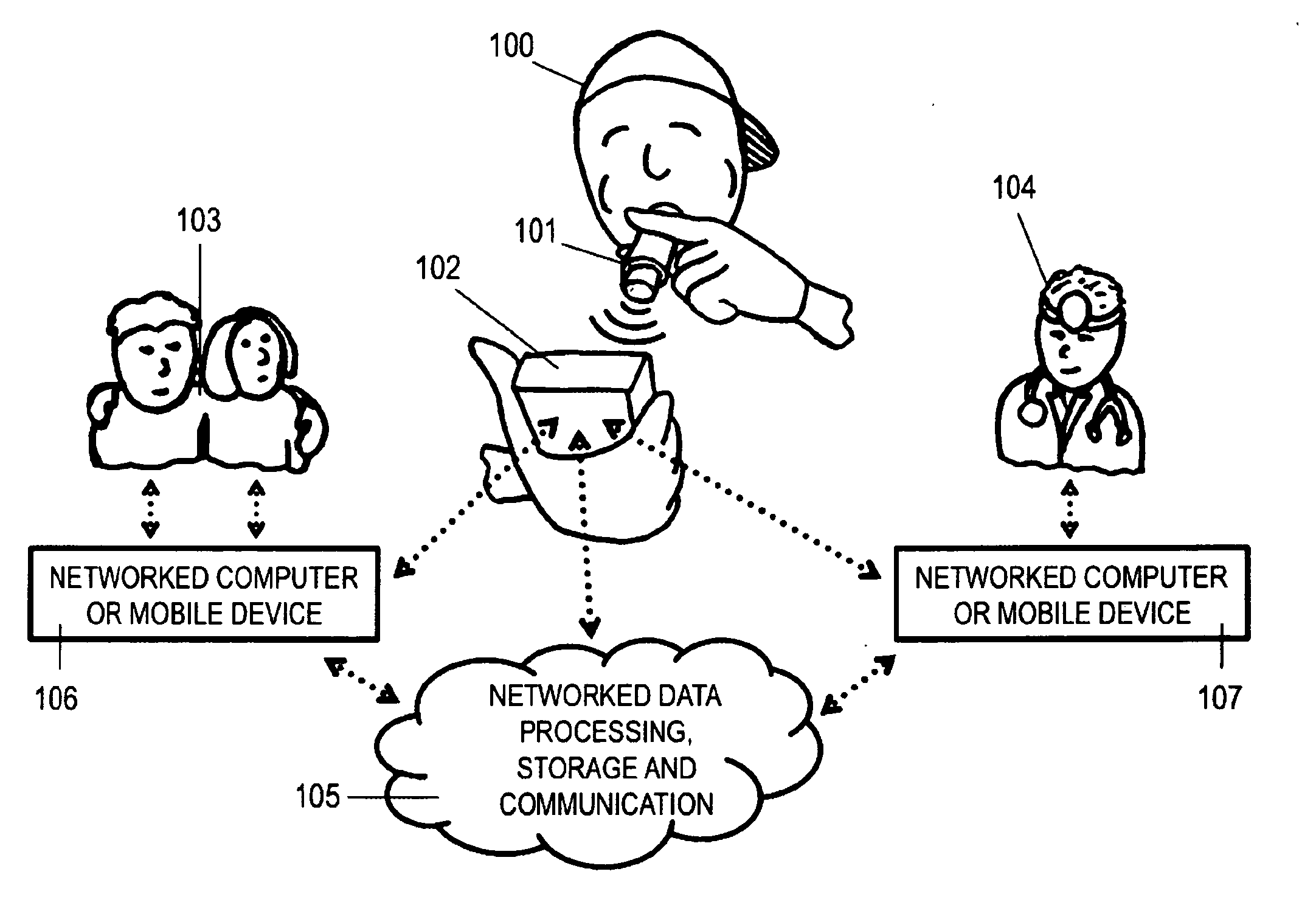
In an age when networked mobile information services are commonplace, the lack of convenient mobile
connectivity and structured channels of digital communication are notable shortcomings.
Visualization: Existing portable monitoring spirometry solutions frequently fail to provide concise graphical reports designed to facilitate quick, sound interpretation and effective
medical treatment decisions.
Furthermore, the user interfaces for existing portable monitoring solutions do little to support exploration of trends over multiple timescales.Ease of Use: Existing monitoring solutions currently fail to minimize the inconvenience of routine monitoring regimens—not only for patients, but also for family members and physicians.
Annotation: Existing peak flow monitoring devices for the most part do not assist patients to supplement automated quantitative measurement with self-reported contextual details.
If a patient does not routinely exhale as forcefully as they are able, the most precise of measurement solutions cannot ensure accurate results.
Contemporary solutions do little to reward the consistent effort required for routine expiratory
airflow measurement—nor do they frame the activity of measurement in ways that invite enjoyment.
Present solutions typically frame peak flow measurement as a task to be completed, when it could alternatively be framed as a game to be played, a competition to be won, or the price of admission for some other form of rewarding experience administered in periodic installments.Social Acceptability: The aesthetic /
industrial design of available peak flow monitoring devices is usually clinical and utilitarian; for the most part, available devices and systems cannot easily be construed as fun, cool, elegant or fashionable.
Existing portable peak flow monitoring solutions do little to help patients correlate their own
lung function with a range of potentially relevant environmental variables, such as local
pollen count and geographic location.
The ability to facilitate correlation could be beneficial not only for patients and their networks, but also for
public health and
medical research institutions in their efforts to understand asthma on a larger scale.Reminding: The vast majority of monitoring solutions do not provide patients with the option of configuring and activating automated reminders that could support the routine monitoring regimens that medical authorities recommend.Although the frequently-competing constraints of low cost, accuracy and reliability have been considered in the past, these constraints have not historically been balanced in ways that leverage the mobile technologies that a growing number of people carry on their persons.
 Login to View More
Login to View More  Login to View More
Login to View More