Bio-sensor
a biosensor and strip technology, applied in the field of biosensor strips, can solve the problems of pain and discomfort, pressure, friction, prior art methods of fine-tuning the shape of the socket to create a comfortable fit to the stump, laborious empirical and time-consuming, etc., to achieve the effect of reducing the number of iterations, reducing the amount of required, and improving the economic prosthesis fitting process
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
[0049]The invention will now be described on the basis of the drawings. It will be understood that the embodiments and aspects of the invention described herein are only examples and do not limit the protective scope of the claims in any way. The invention is defined by the claims and their equivalents. It will be understood that features of one aspect or embodiment of the invention can be combined with a feature of a different aspect or aspects and / or embodiments of the invention.
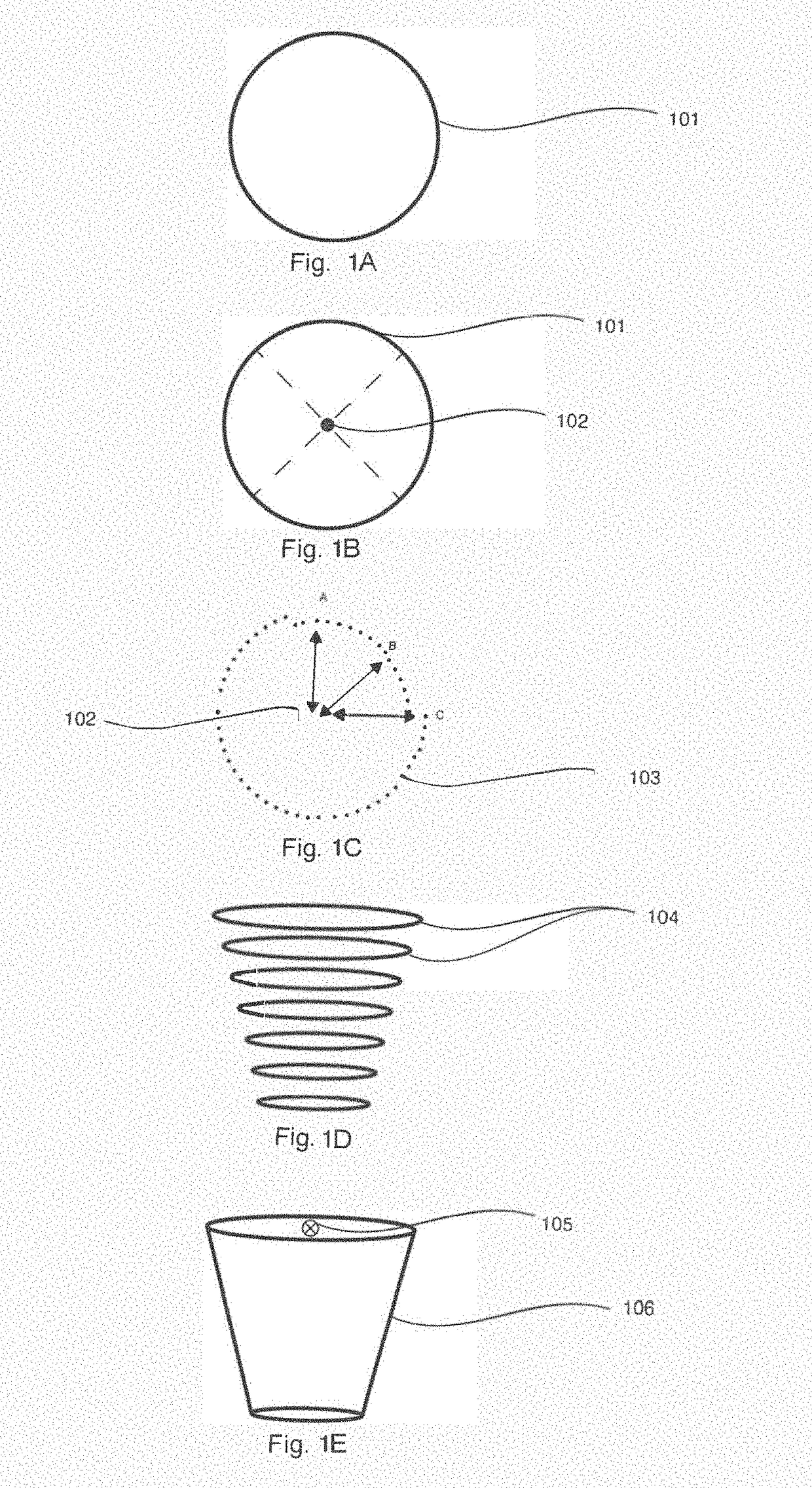
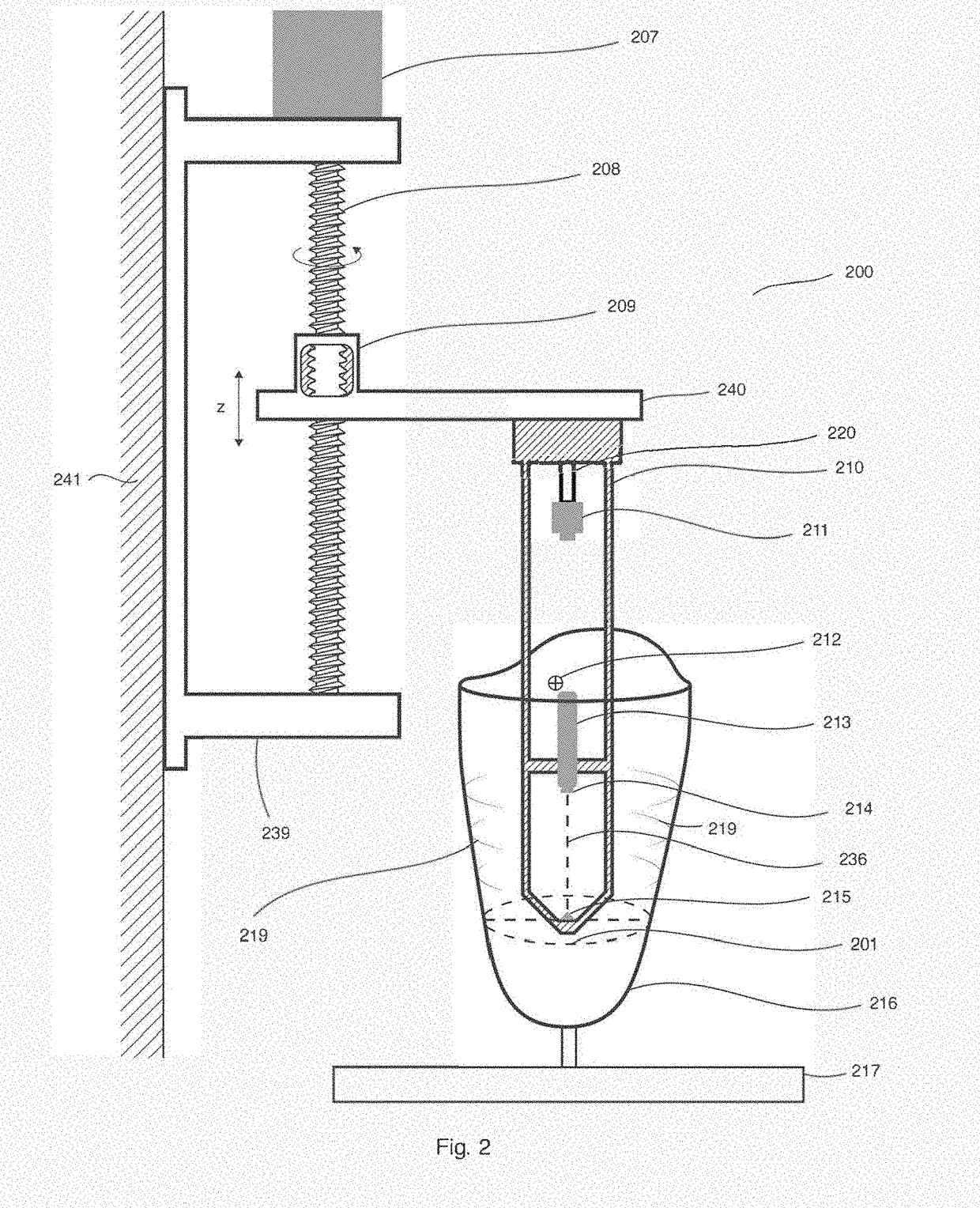
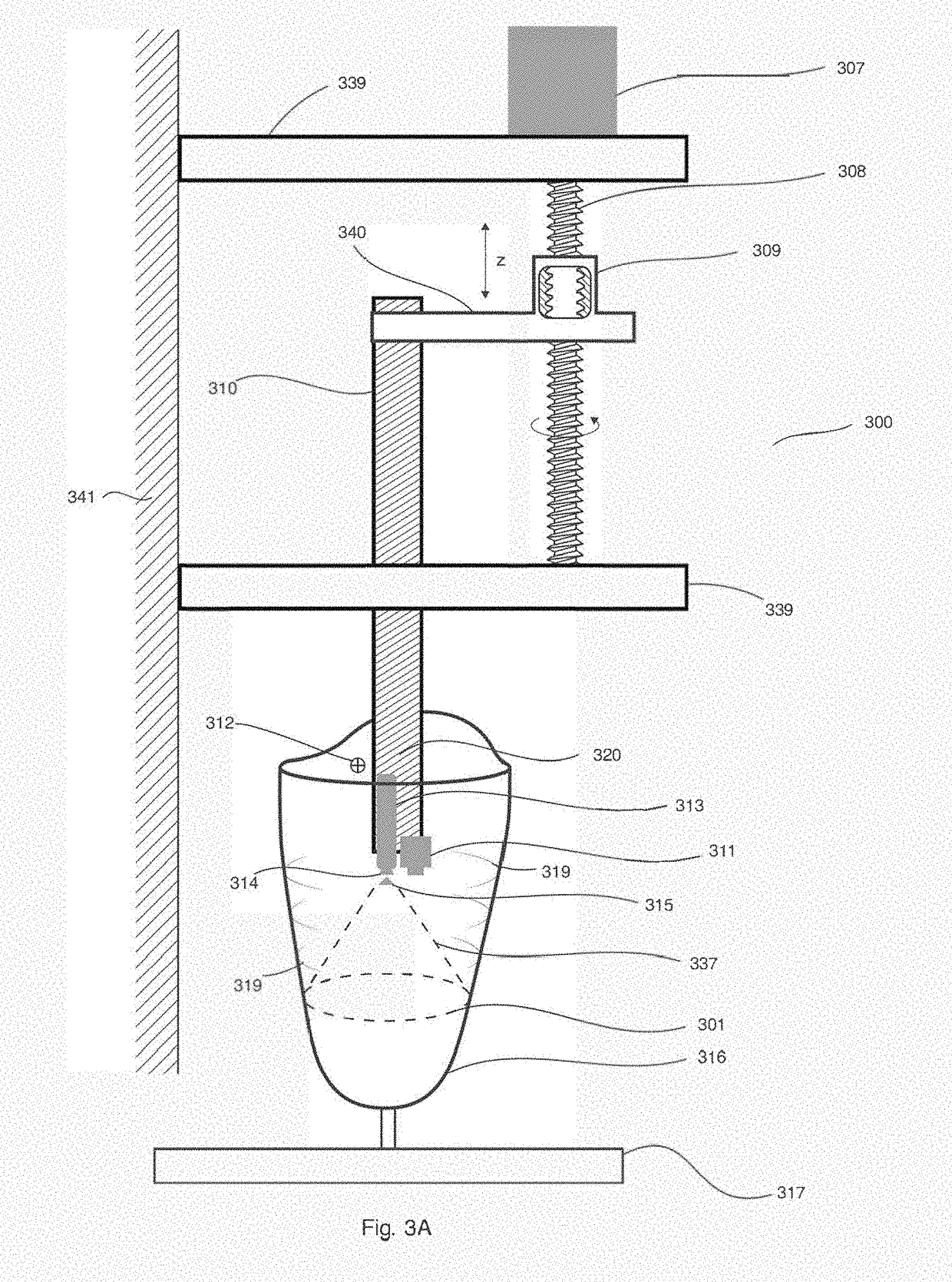
[0050]Referring first to FIGS. 1A to 1E, there is shown a summary of the steps involved in mapping and modelling in three dimensions of a socket for an artificial limb. Reference is also made to FIGS. 2 to 4 which shows the apparatus used for the mapping and modelling of the socket in three dimensions. The description below assumes that a laser is used as the radiation source, but it will be appreciated that other beams of light could be used to scan the socket of the artificial limb and this application i...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com