Injector
a technology of injectors and power injectors, which is applied in the field of injectors, can solve the problems of high cost, high price of many of these injectors, and inability to meet the needs of large-scale power injectors, and achieve the effects of reducing or eliminating the power connection of the injector, improving the power injector, and facilitating the attachment of the syring
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
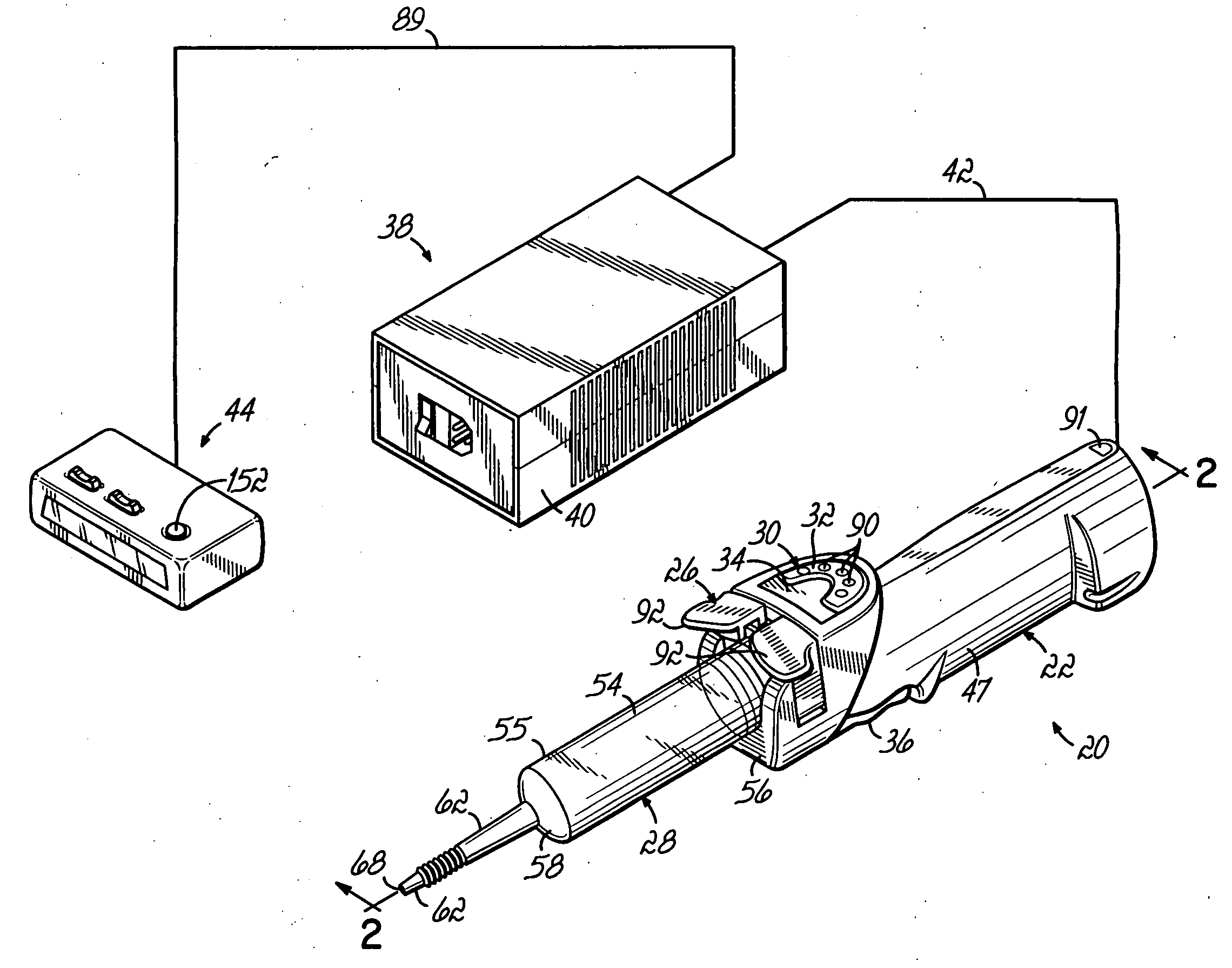
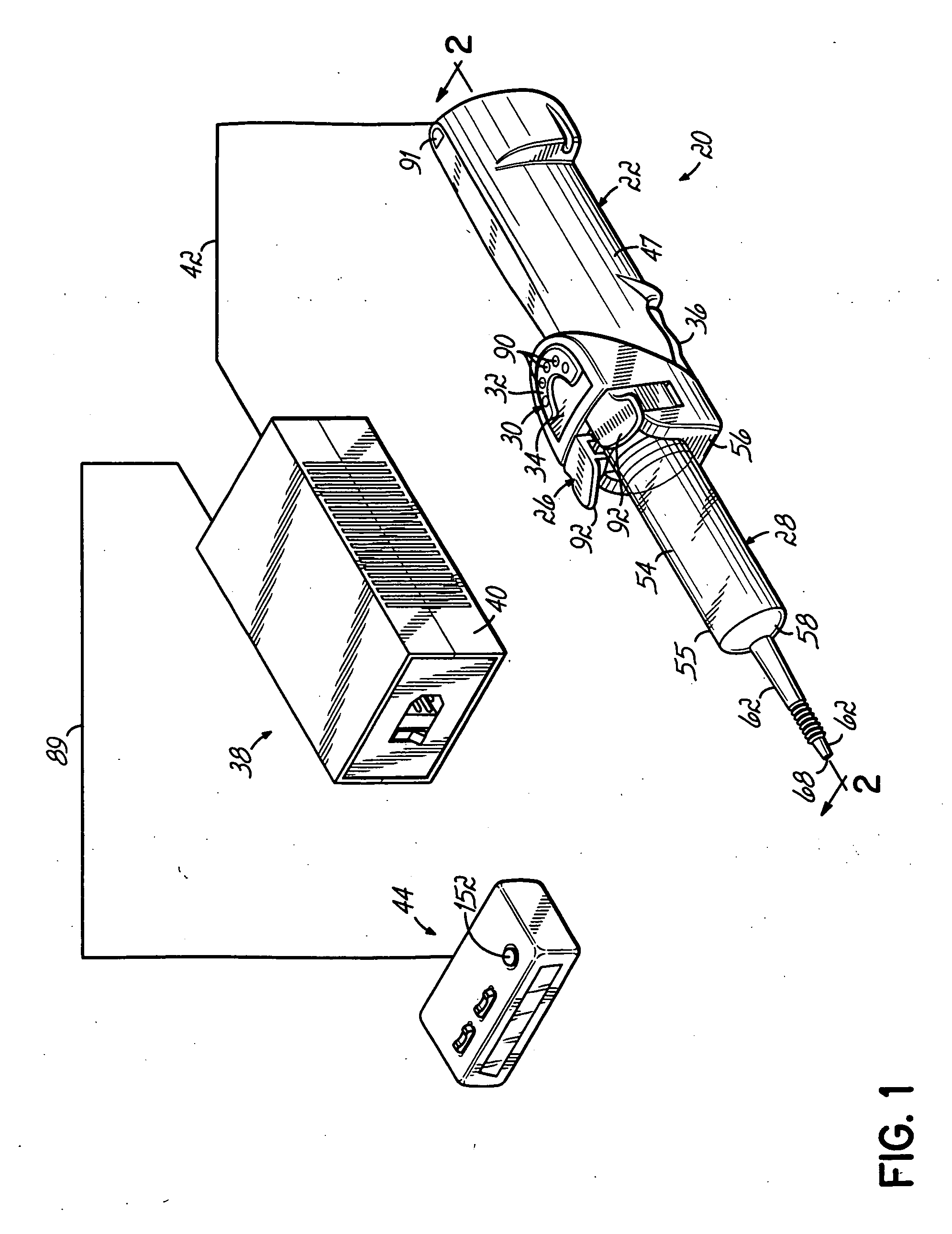
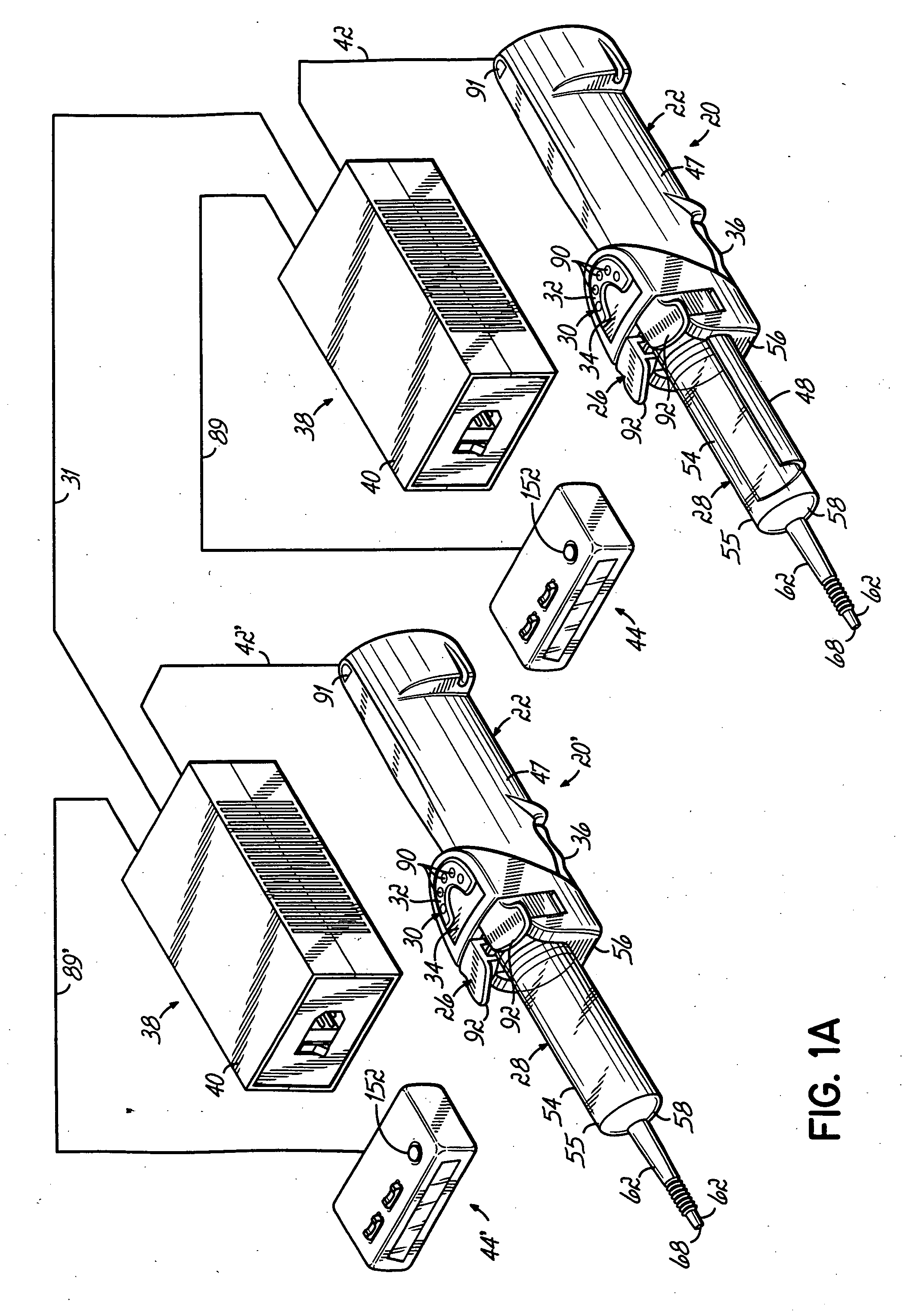
As described above in the summary of the invention, the present invention provides an injector which overcomes and eliminates the drawbacks of injectors as described above. With reference to the Figures, an injector 20 of the illustrated embodiment of the present invention may be provided in a “wand” shape in order to be hand held. The injector 20 of the present invention is designed to meet ordinary needs of the medical market and is therefore less expensive, smaller, and less complicated to operate. Features such as stored protocols, multi-phasic injections, high flow rate, and optional printer may be omitted in order to reduce costs and simplify the user-injector interface 30. With an optional injector-injector interface 31 (FIG. 1A), the injector 20 of the present invention may be joined with other compatible injectors in order to deliver greater volume injections, or a flushing solution (normally saline) in a similar manner as some other injection systems such as the Optistar ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com