Methods and apparatus for delivery of ocular implants
a technology of ocular implants and ocular arteries, which is applied in the field of methods and apparatus for delivering solid or semisolid materials into the eye, can solve the problems of inability to introduce drugs or therapeutic agents into the eye and maintain these drugs, increase the incidence of unacceptable side effects of drugs, and simple ocular instillation or application is not an acceptable alternative, so as to facilitate the inventive delivery method, facilitate the effect of delivering, and less invasive and traumati
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example 1
Effects of Needle Size and Technique on Vitreous Leakage
[0079] Different gauge needles together with various insertion techniques were pursued to determine the maximum size needle gauge and optimum insertion technique for mimimum vitreous leakage and “self-sealing” wounds.
[0080] Eight rabbits were anaesthetized with a Ketamine / Xylazine cocktail. Drops of a 0.5% Opthaine solution were delivered to each eye of the rabbit as a local anaesthetic. 16 g, 20 g, 23 g, 25 g needles (Beckton-Dickinson, Franklin Lakes, N.J.) were attached to syringes and inserted into the vitreous cavities of the rabbits' eyes, through the pars plana (2-3 mm from the limbus) according to varying techniques. For each needle size, the needles were inserted at either angles of 90° or 45° relative to the pars plana of the eye, or according to the following “tunnel” technique. In the “tunnel” technique, the needle is initially advanced into the first scleral layer of the eye tissue at a very shallow angle, almost...
example 2
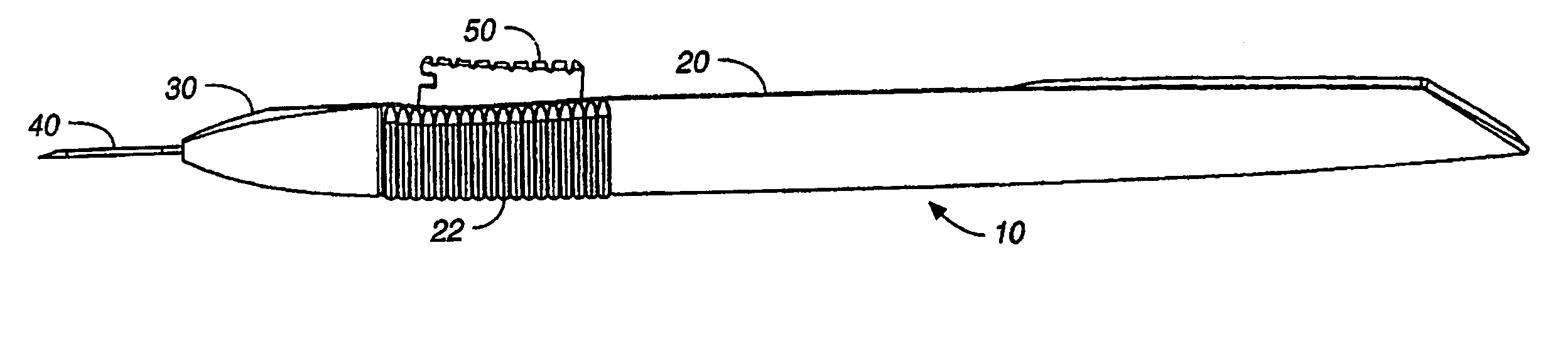
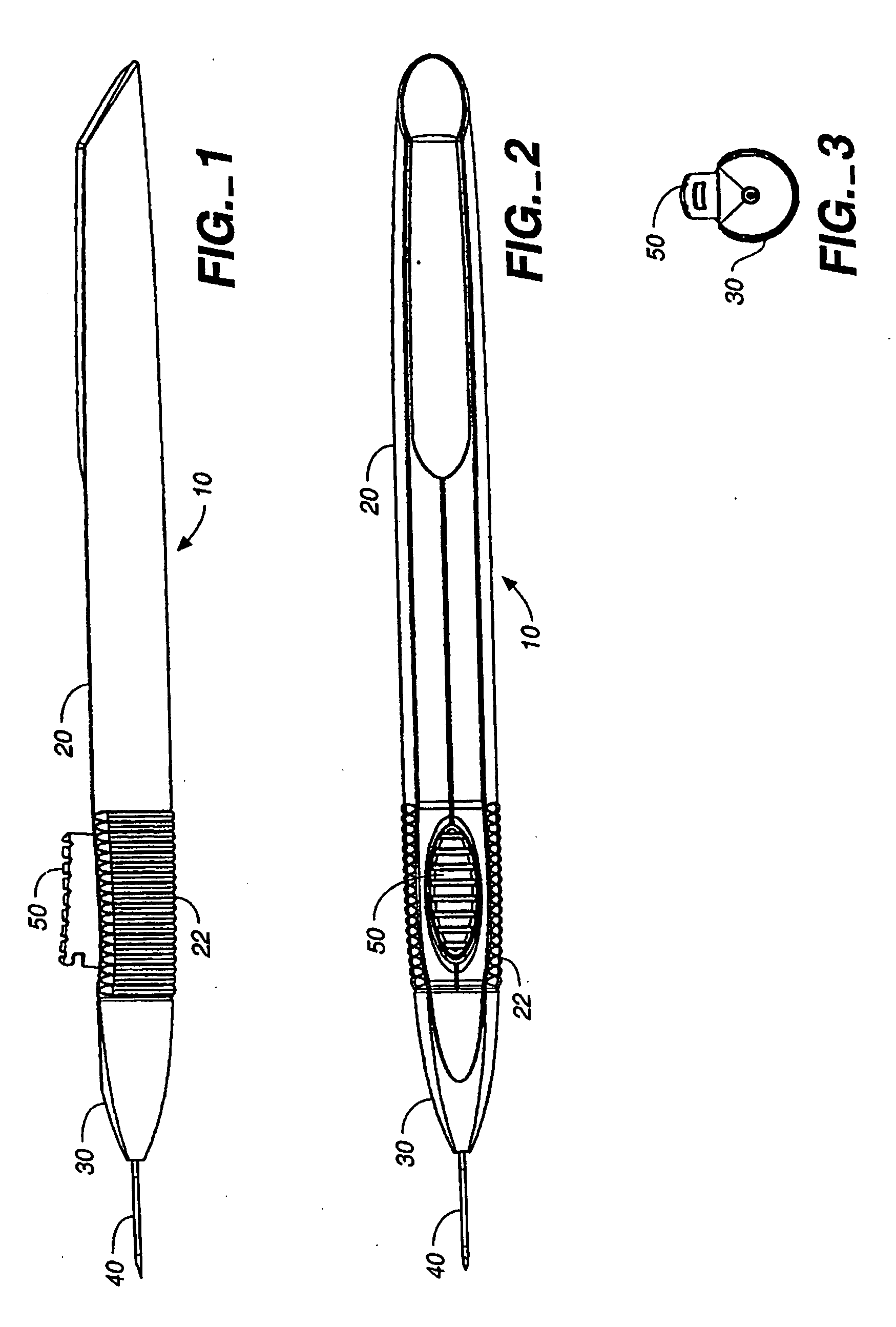
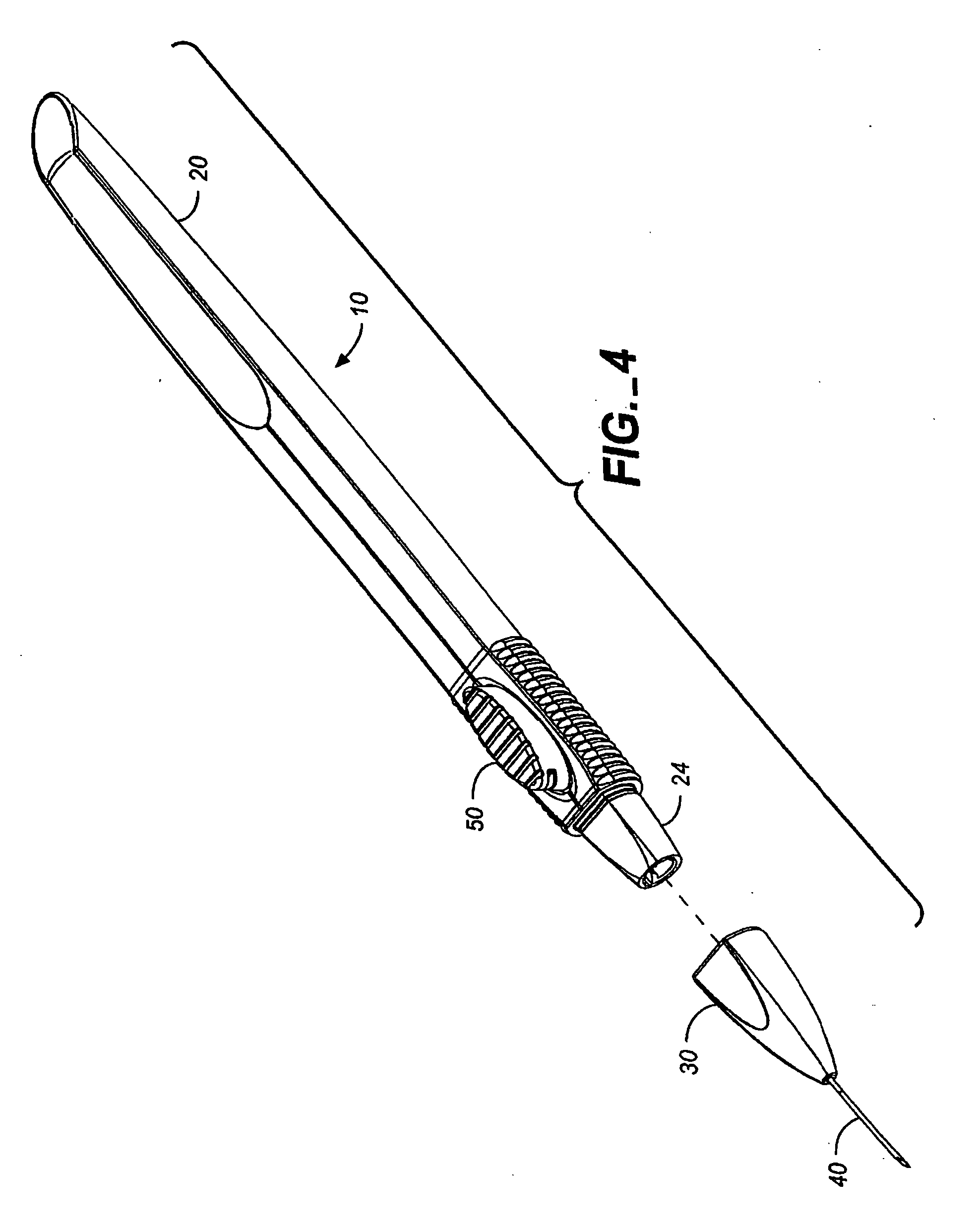
Delivery Of Microimplants
[0083] Cylindrical microimplants having dimensions of 0.015 inches diameter and 6 mm length were delivered into posterior segments of rabbits' eyes using a 23 gauge thin wall needle and according to insertion techniques described above in Example 1.
[0084] Four rabbits were anaesthetized as before with a Ketamine / Xylazine cocktail and with drops of a 0.5% Opthaine solution administered to each eye of the rabbit as a local anaesthetic. 23 g thin wall needles (BD, Franklin Lakes, N.J.) were attached to syringes and the needle cannulaes were loaded with the microimplants. The needles were inserted into the vitreous cavities of the rabbits' eyes, according to varying techniques detailed in Example 1 and as further described herein. Table 2A below details the needle gauge and insertion technique for each animal.
TABLE 2ASTUDY DESIGNBevel position,AnimalEyeorientation of needle1ODUp, 90°OSDown, 90°2ODUp, 45°OSDown, 45°3ODUp, 45°OSDown, 45°4ODTunnel techniqueOSTu...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com