Method and apparatus for tissue resection
a tissue resection and tissue technology, applied in the field of tissue resection devices and methods, can solve the problems of increasing the complexity, time and expense of the resection procedure, affecting the effect of hemostasis promotion, and severing the tissue, so as to prevent the polymerization of the hemostasis-promoting material
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
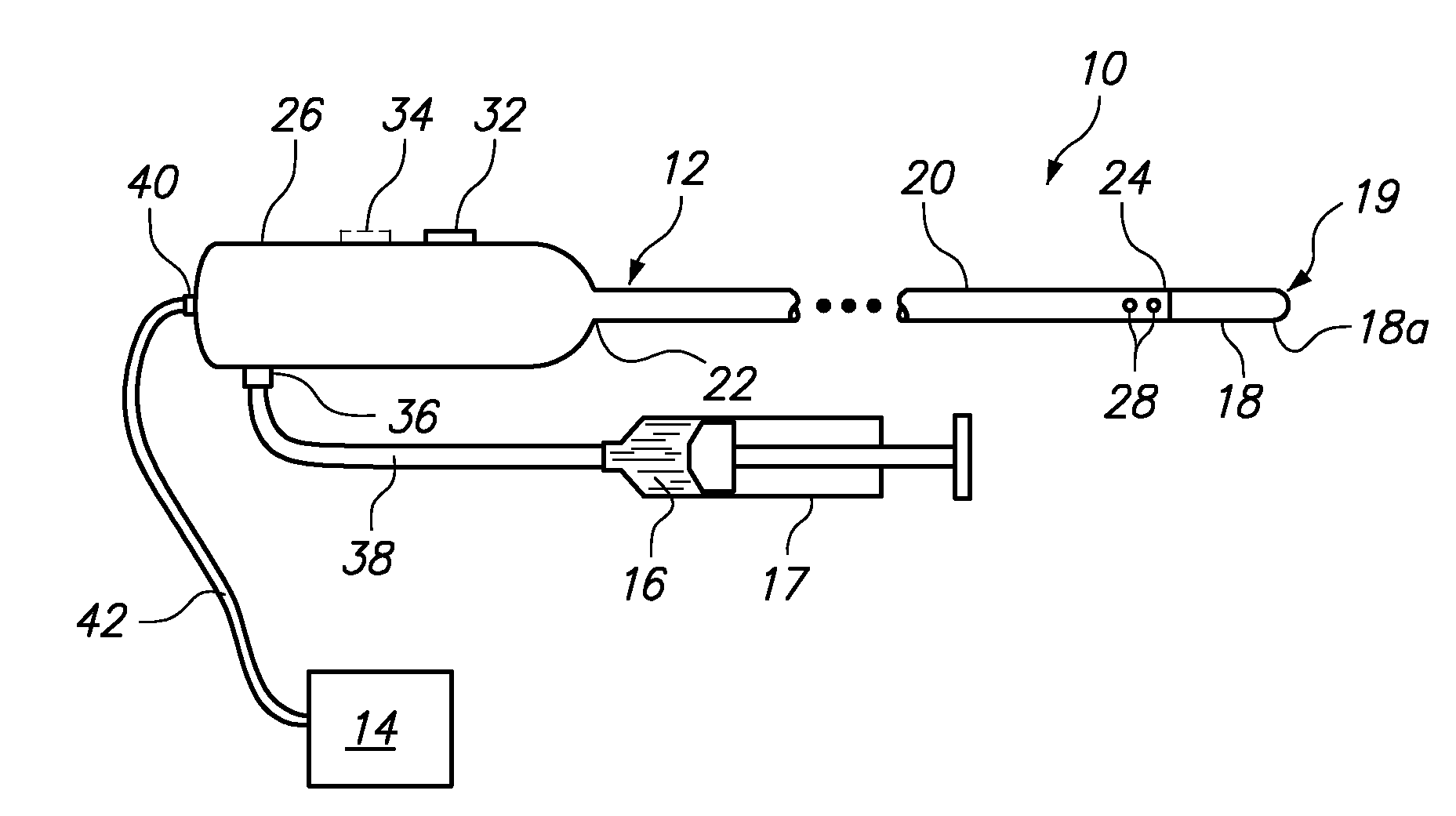
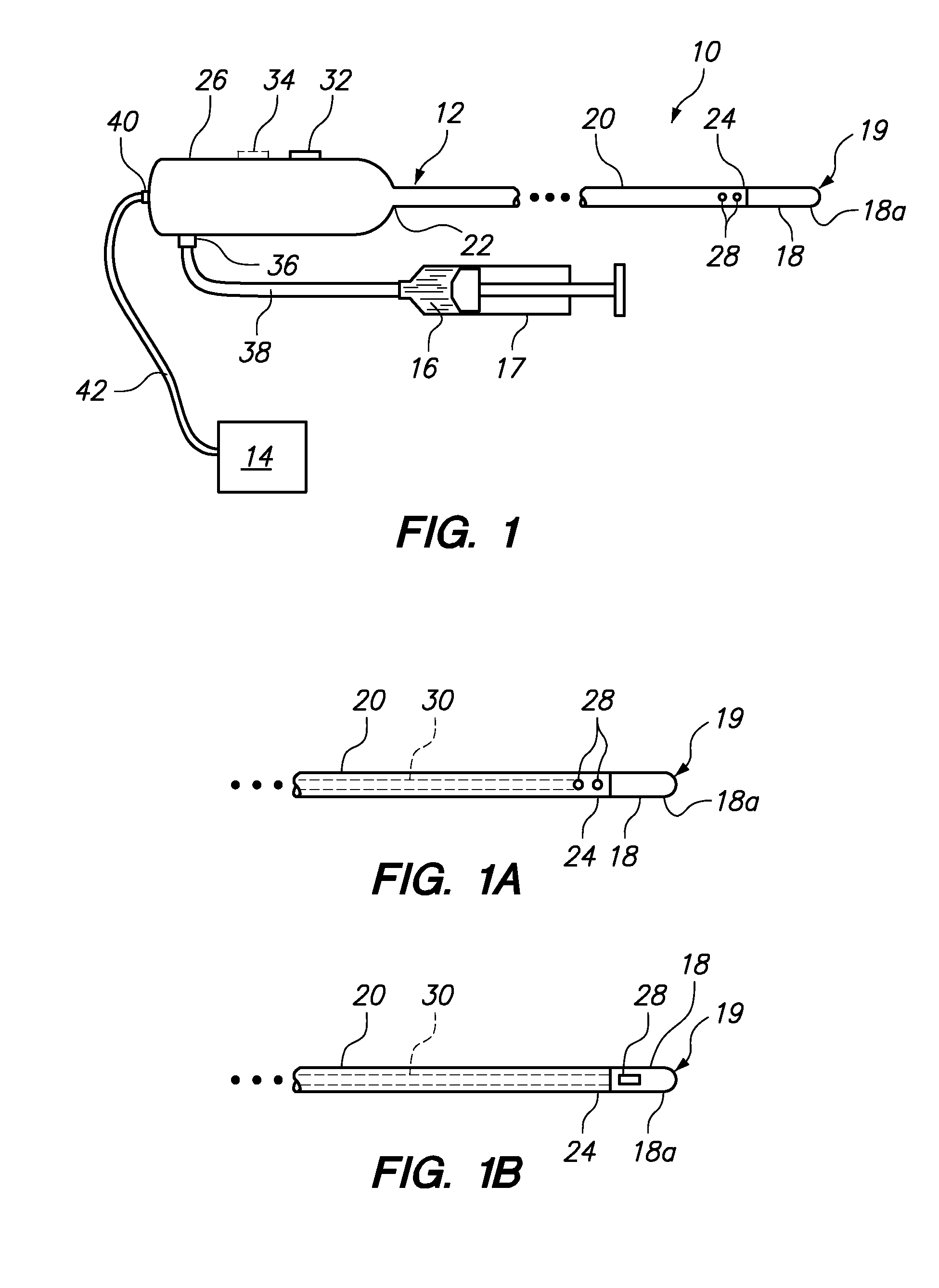
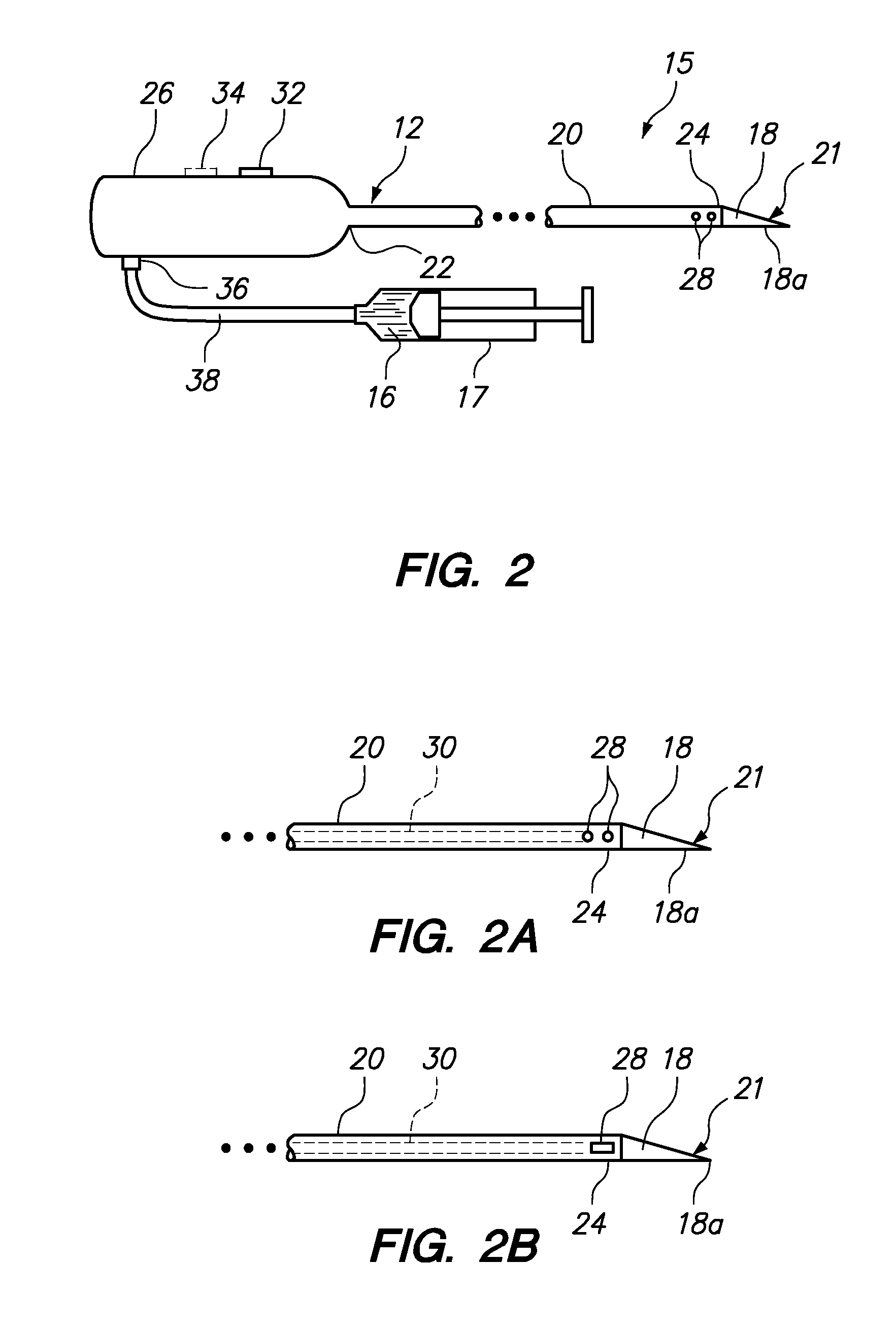
[0049]FIG. 1 illustrates a tissue resection device 10 constructed in accordance with one embodiment of the present invention. In this embodiment, the tissue resection device 10 generally includes a resection device or probe 12 configured for resecting and coagulating tissue and a syringe 17 or other pumping source configured for delivering a polymerizable hemostasis-promoting material 16 to the resection site. The resection probe 12 includes a tissue resection member 18 disposed on a distal end of the resection probe 12 that is configured for being placed into contact with tissue.
[0050]In the embodiment illustrated in FIG. 1, tissue resection member 18 is formed as a resection electrode 19. Accordingly, the device 10 further includes an ablation energy source, and in particular a radio frequency (RF) or microwave generator 14, configured for supplying RF energy or microwave energy to the resection electrode 19 in a controlled manner.
[0051]The resection probe 12 generally comprises a...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com