System and method for measuring force and torque applied to a catheter electrode tip
a technology of force and torque and catheter electrode tip, which is applied in the field of system and method for assessing force and torque, can solve the problems of catheter tip perforation or other damage to tissue, variety and even death, and ineffective lesions created
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
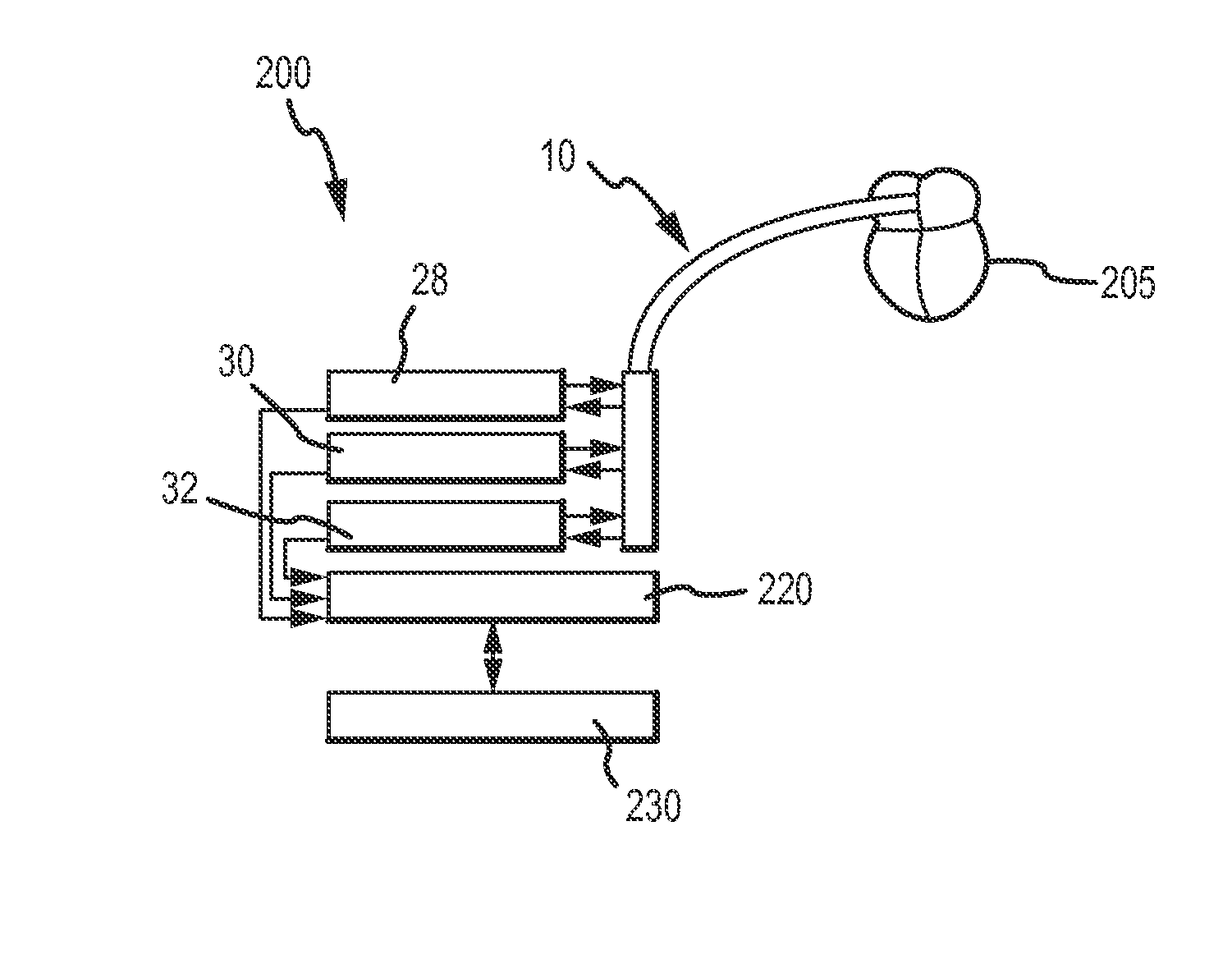
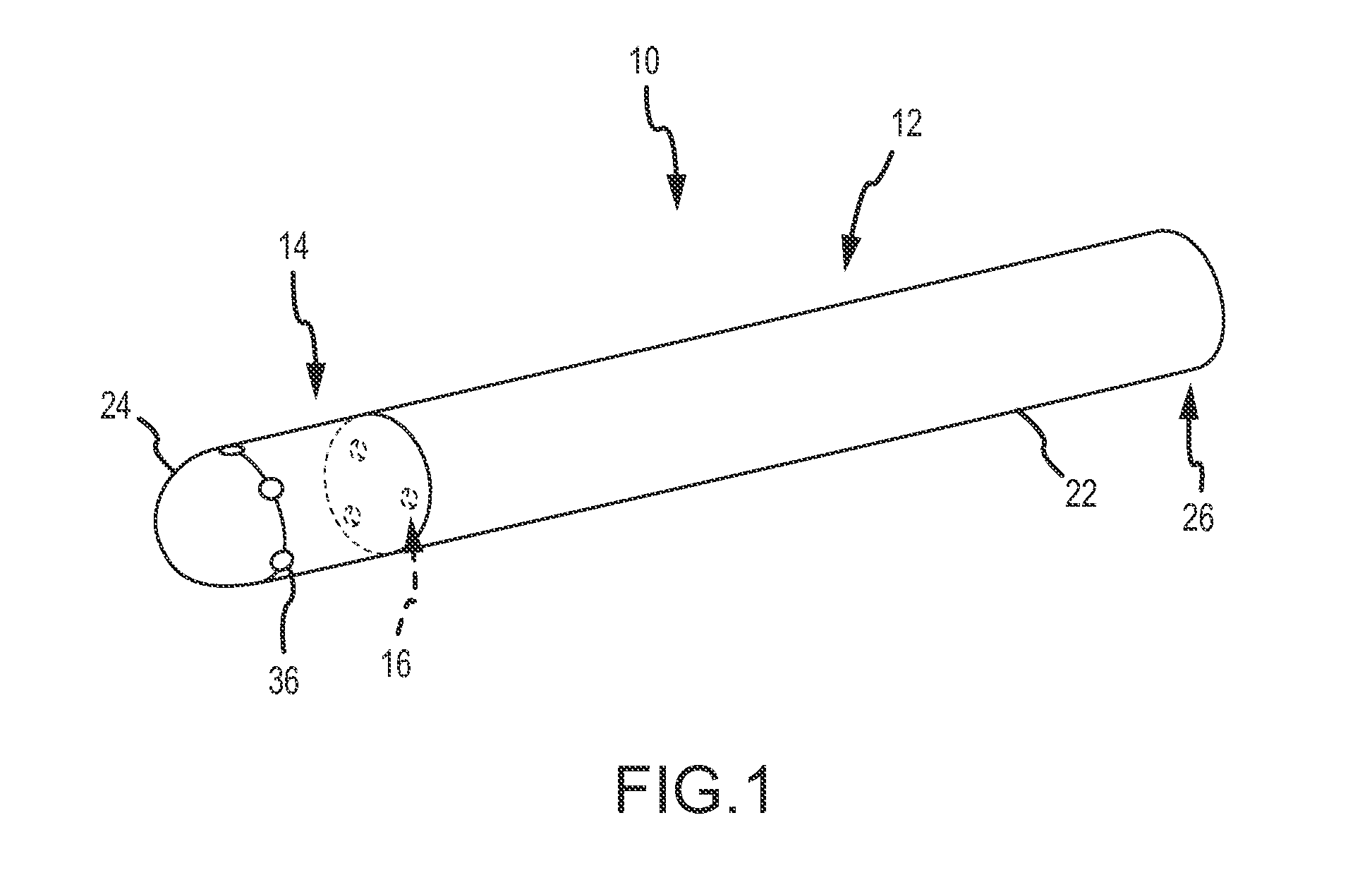
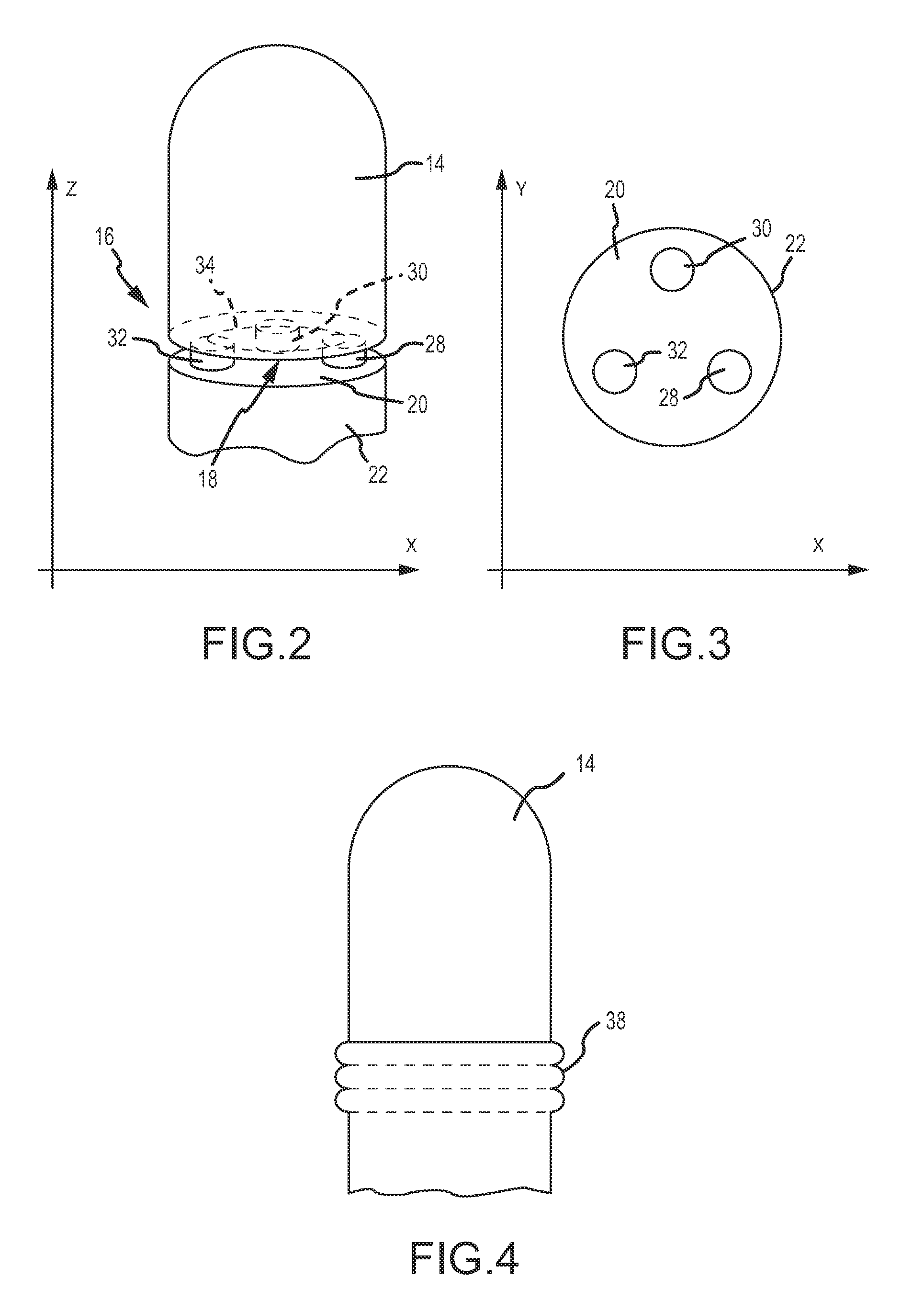
[0032]Referring now to the drawings wherein like reference numerals are used to identify like components in the various views, FIG. 1 illustrates an exemplary embodiment of a contact sensing assembly 10 as provided by the invention. In a general form, referring to FIGS. 1 and 2, contact sensing assembly 10 may include a catheter 12, an electrode 14 connected to the catheter, and a force and torque sensor 16 for interacting with base 18 of electrode 14 or alternatively with head 20 of catheter body 22 if sensor 16 is mounted on base 18. In another embodiment, contact sensing assembly 10 may include a first interactive component and a second interactive component. The contact sensing assembly may be used in the diagnosis, visualization, and / or treatment of tissue (such as endocardial tissue) in a body. Contact sensing assembly 10 may be used in a number of diagnostic and therapeutic applications, such as for example, the recording of electrograms in the heart, the performance of cardi...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com