Apparatus having stabilization members for percutaneously performing surgery and methods of use
a technology of stabilization members and implants, which is applied in the field of implants and methods for performing surgery on the interior wall of the hollow body organ, can solve the problems of significant trauma to the patient, inadequate blood flow to the myocardium, and ischemia of the hear
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
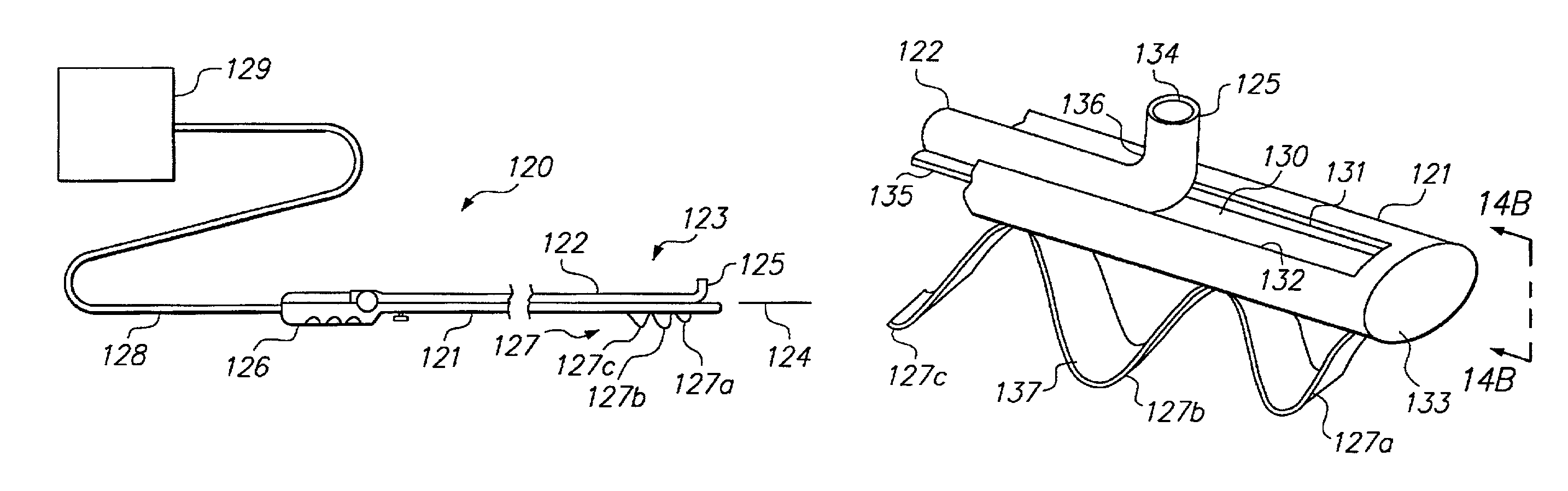
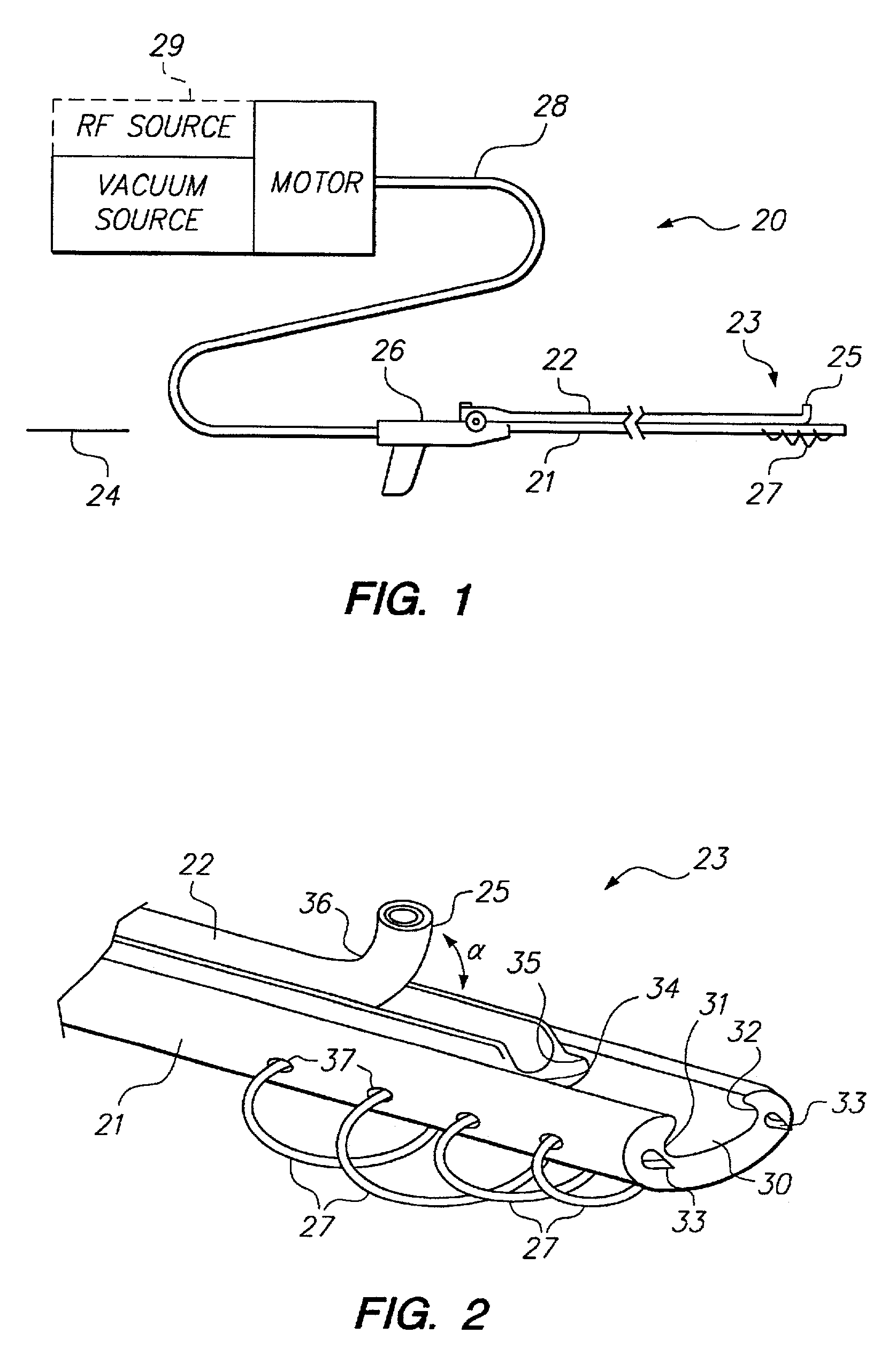
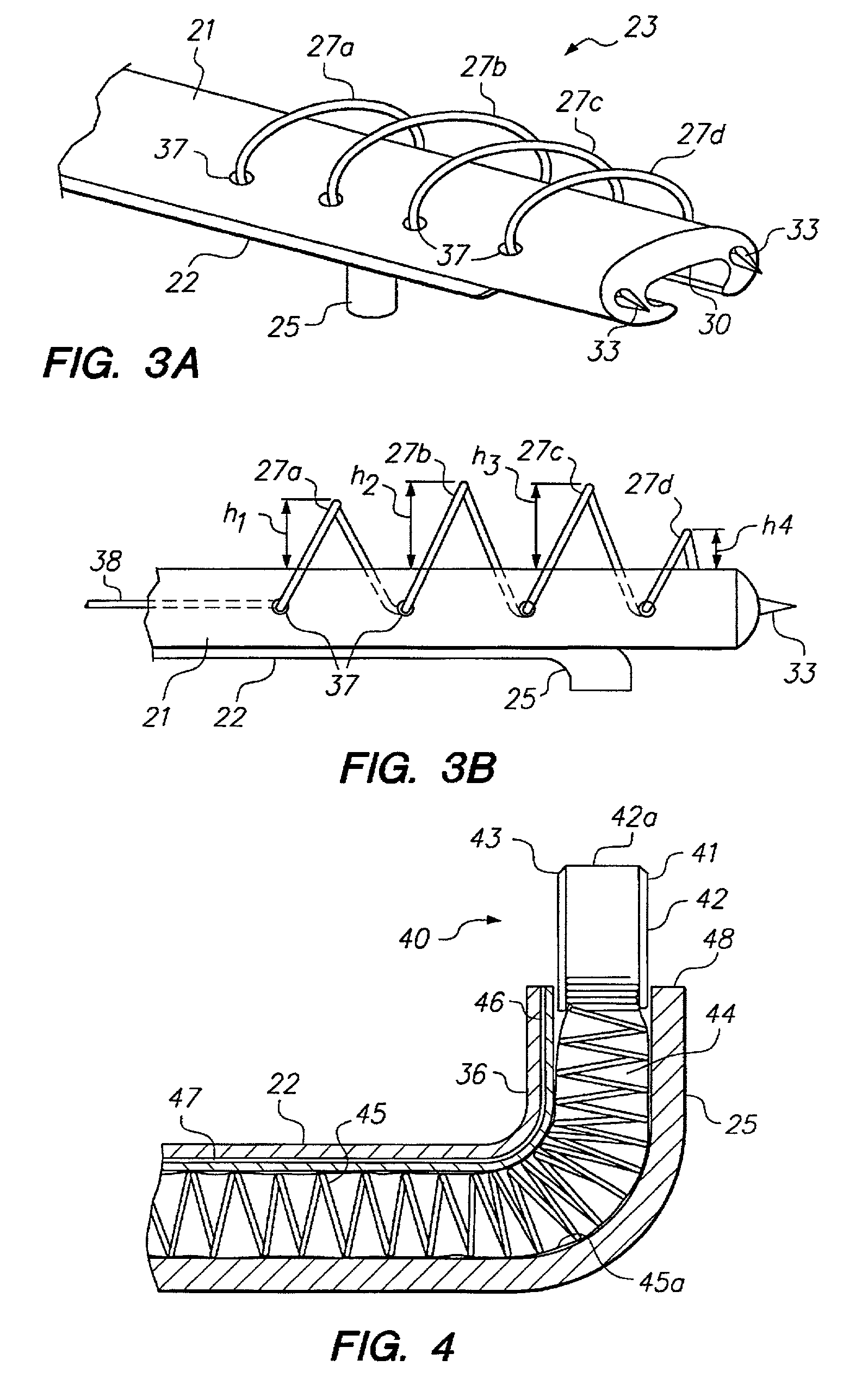
[0039]The present invention relates generally to apparatus and methods for percutaneously performing surgery within an organ or vessel. The apparatus of the present invention comprises a catheter including a stabilizing catheter shaft which percutaneously may be disposed within an organ. A guide member engaged with the catheter shaft includes an end region that may be selectively articulated to a position at an angle to a longitudinal axis of the catheter, including a position substantially orthogonal to the longitudinal axis. The end region carries an end effector (e.g., an ablative or mechanical cutting device) for treating tissue. Severed or ablated tissue may be aspirated through the catheter to its proximal end for disposal. The catheter shaft, either alone or in conjunction with stabilizing members, and the guide member, provides precise control over the location of the end region, and thus, the end effector.
[0040]The present invention therefore offers a device having a direct...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com