Method for cryopreserving tumor tissue
A tumor tissue, cryopreservation technology, applied in the preservation, application, animal husbandry and other directions of human or animal body, to achieve the effect of high tumor formation rate
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Problems solved by technology
Method used
Image
Examples
Embodiment 1
[0021] Example 1: Obtaining and Freezing of Patient Tumor Tissue Specimens
[0022] Fresh tumor tissue samples were obtained from a 40-year-old female patient with colon cancer and lymph node and liver metastases. The samples were obtained with the informed consent of the patient and the permission of the ethics committee of the institution. The patients had not received chemotherapy and other treatments before operation. The intraoperative specimens were cut into different sizes with sterilized surgical scissors and then frozen in the pre-prepared freezing solution of the present invention (first placed in a freezing box containing isopropanol at 4°C for about 1 hour; Then place the frozen storage box containing the specimen in a low-temperature refrigerator at -20°C overnight (24 hours); then place the frozen storage box containing the specimen at -80°C (24 hours); and remove the specimen from the freezing storage box Take it out and place it in liquid nitrogen (-196°C) for...
Embodiment 2
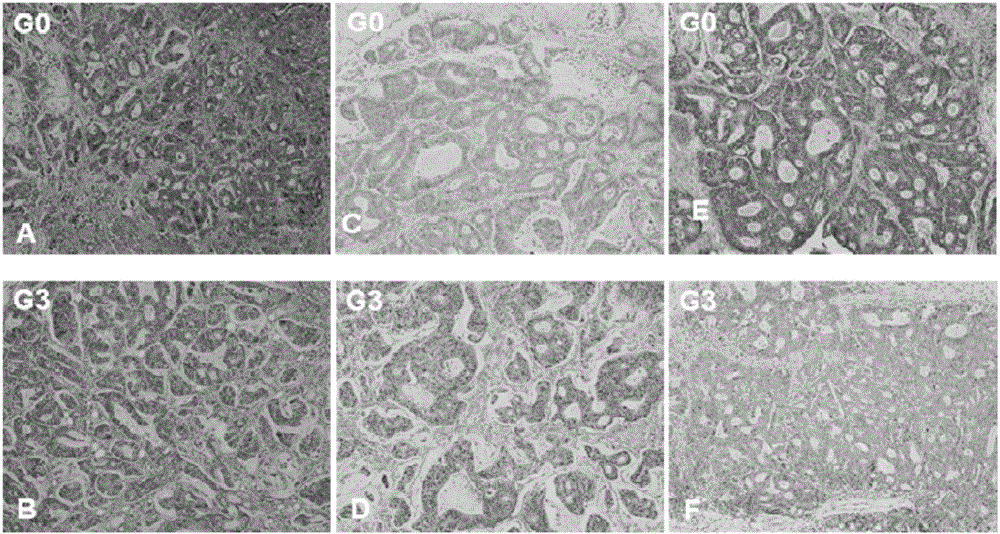
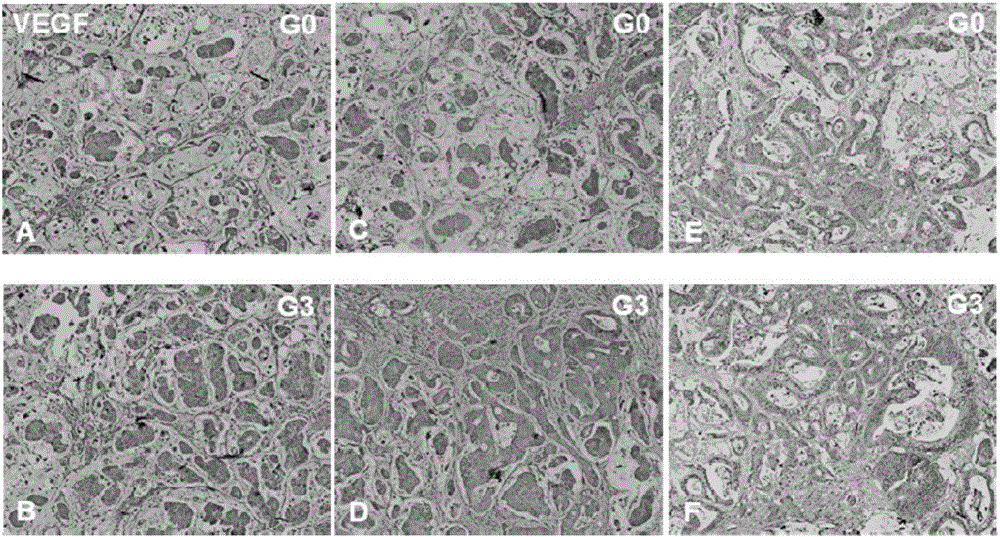
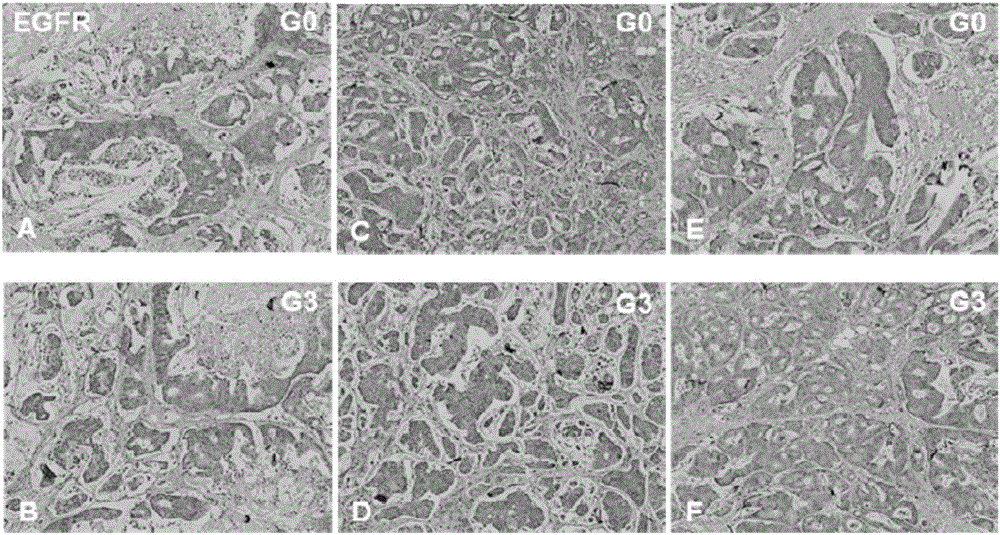
[0026] Example 2: Establishment of multi-focal PDTT xenograft model of colon cancer
[0027] 1) BALB / c nude mice aged 4-6 weeks were raised in an SPF barrier environment and allowed to adapt to the environment for more than three days;
[0028] 2) The tumor tissue specimens frozen in the cryopreservation solution of the present invention (the specimens have been cut into fragments of different sizes with sterilized surgical scissors before freezing) are recovered and transferred to the RPMI 1640 medium (containing 20% fetal bovine serum and 0.05% penicillin / streptomycin);
[0029] 3) Then wash three times with the above-mentioned RPMI 1640 medium;
[0030]4) After the animal is anesthetized with isoflurane, disinfect the skin on the back and abdomen of the nude mouse, wipe it dry with a sterile cotton ball, cut a small incision near the anterior armpit on one side of the nude mouse with a razor blade, and bluntly separate the skin and subcutaneous tissue with a 18-gauge punct...
Embodiment 3
[0035] Example 3: Effects of Different Freezing Time on the Tumor Formation Rate of Colon Cancer PDTT Transplanted Tumor Model
[0036] According to the method of Example 2, the PDTT xenograft tumor model was established according to the tumor tissue with the cut size of 1 mm×1 mm×3 mm frozen for 2-52 weeks according to Example 1, and the tumor formation rate is shown in Table 1.
[0037] Table 1: The effect of different cryopreservation time on the tumor formation rate of colon cancer PDTT xenograft model
[0038]
[0039]
[0040] Note: G3, passage to the third generation.
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com