Endovascular prosthesis
a prosthesis and endovascular technology, applied in the field of endovascular prosthesis, can solve the problems of stroke, paralysis or abnormal sensation, high risk for patients,
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
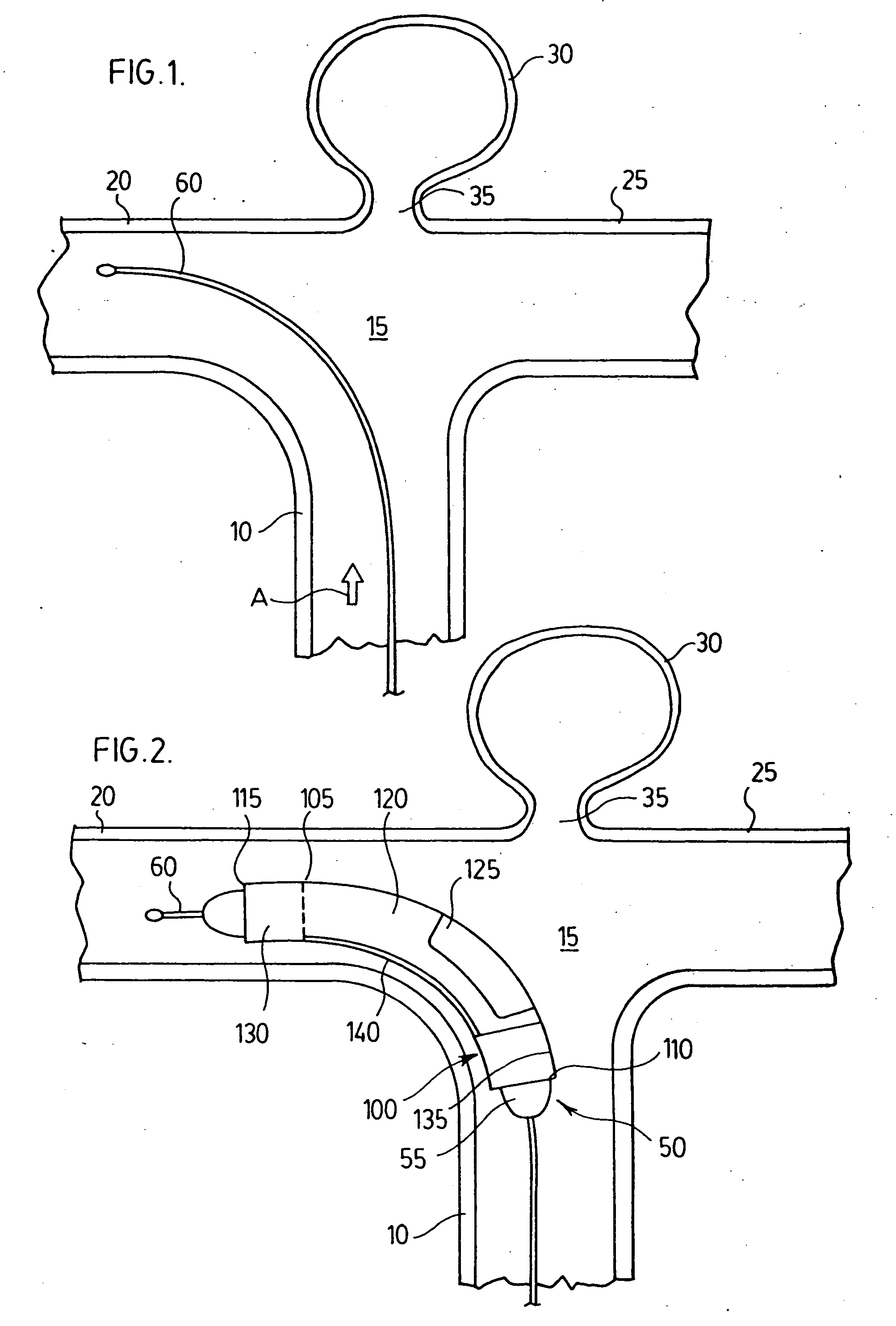
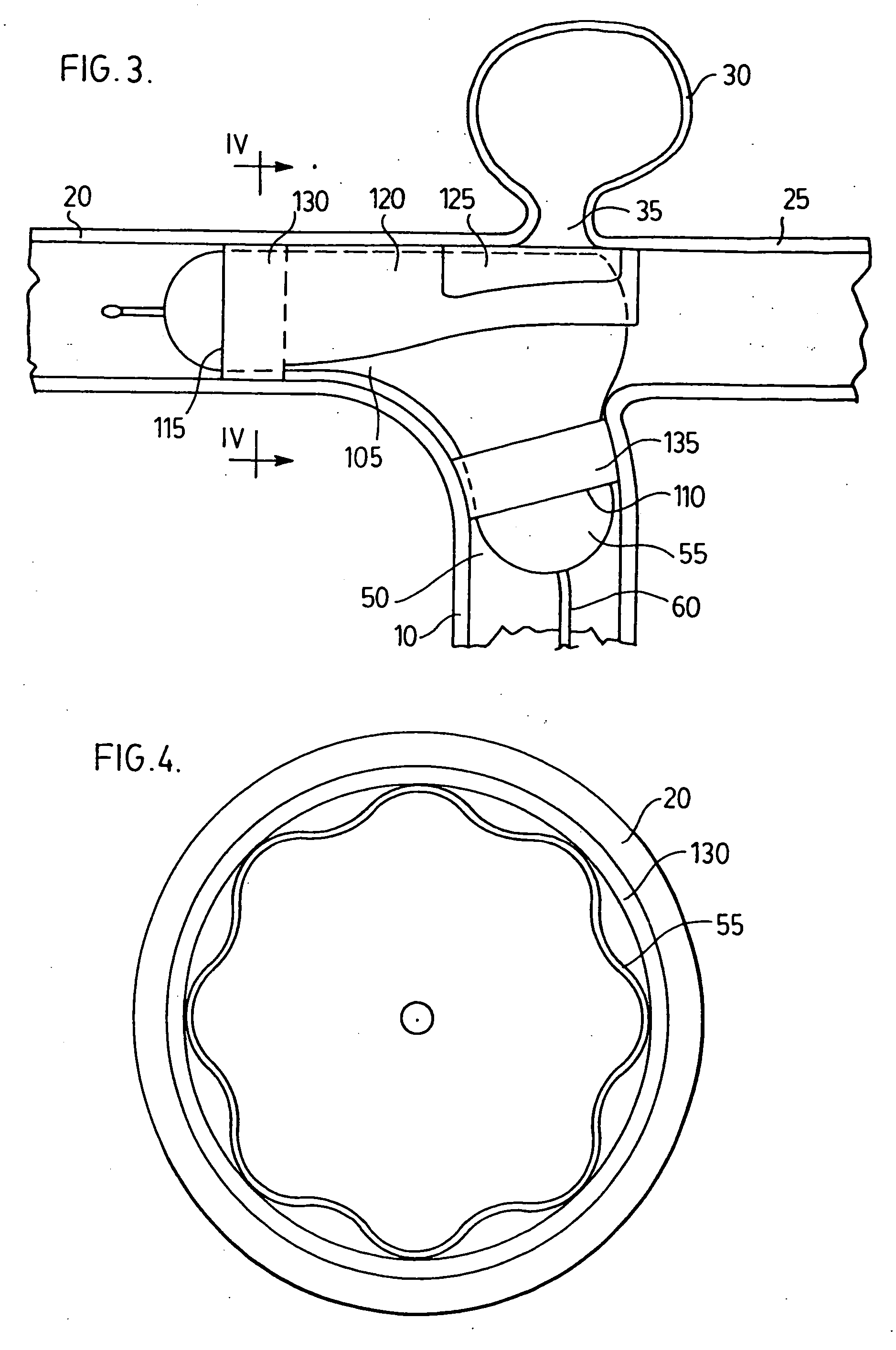
[0052] With reference to FIGS. 1-4, a first embodiment of the present endovascular prosthesis will be described with particular reference to implantation of same at the terminal bifurcation of the basilar artery.
[0053] Thus, there is illustrated a basilar artery 10 which terminates at a junction 15 which bifurcates into pair of secondary arteries 20,25. Located at junction 15 is an aneurysm 30. Aneurysm 30 has an opening 35 (shown enlarged for illustrative purposes only) through which blood enters and sustains aneurysm 30.
[0054] An endovascular prosthesis 100 is mounted on a catheter 50.
[0055] Catheter 50 comprises an inflatable balloon 55 and a guidewire 60. Catheter 50, inflatable balloon 55 and guidewire 60 are conventional. As is known in the art, inflatable balloon 55 is moveable along guidewire 60.
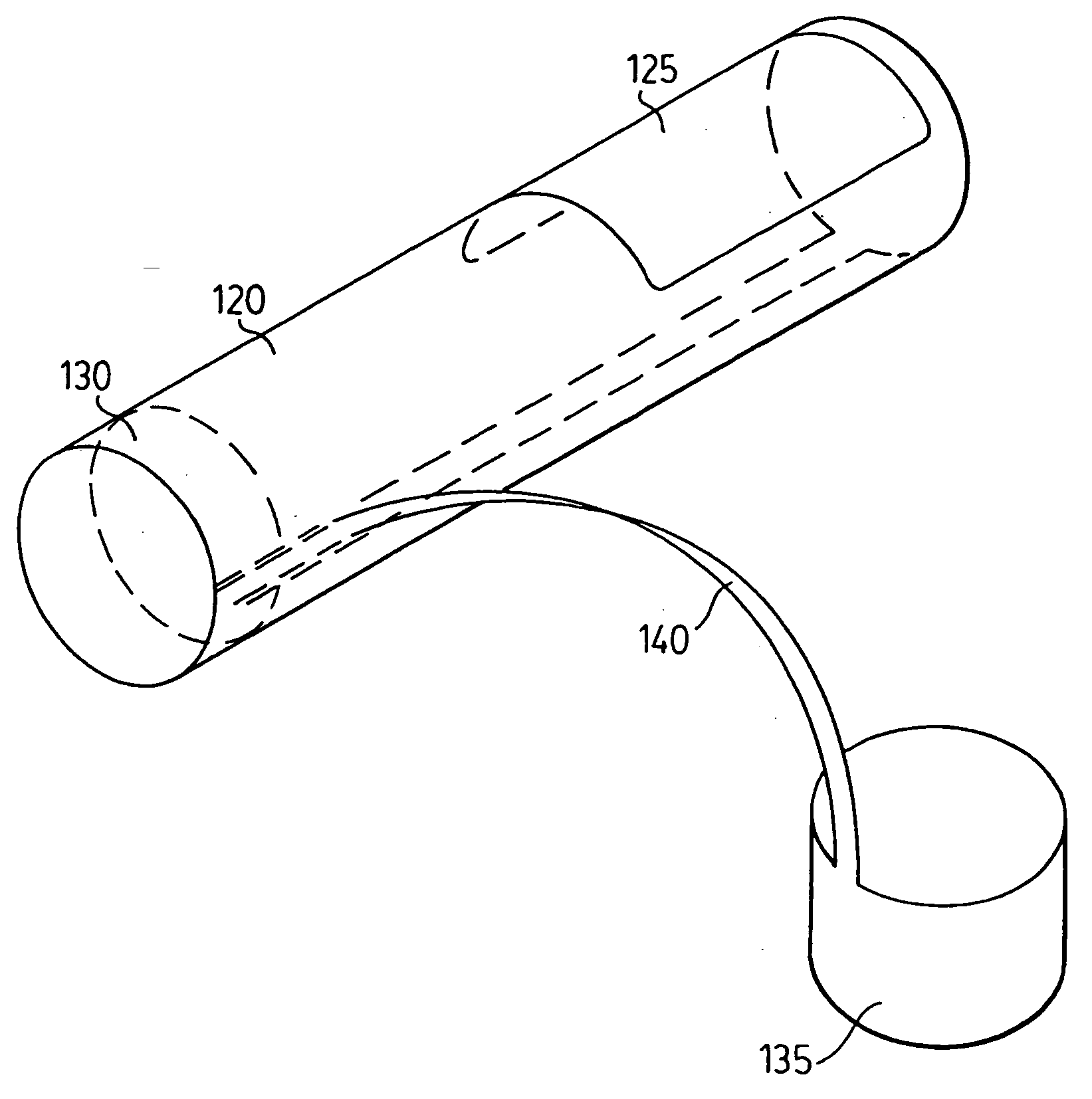
[0056] Endovascular prosthesis 100 is constructed of a body 105. Body 105 comprises a proximal end 110 and a distal end 115. Endovascular prosthesis 100 further comprises an expa...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com